Abstract
Objective
To describe high/low daily blood pressures (BP) and variability in BP management with vasoactive infusions (VI) and/or hydrocortisone (HC) in extremely preterm infants.
Study design
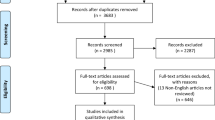
Analysis of data from 24–27 weeks’ gestation infants in the Preterm Erythropoietin Neuroprotection (PENUT) Trial. Daily high/low BPs, the use of VI and/or HC, and adverse outcomes were compared descriptively and using regression models.
Results
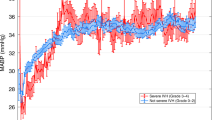
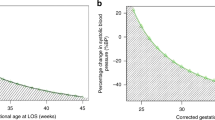
936 infants were included; 64% untreated, 20% VI, 3% HC, and 13% VI + HC. BP ranges are described for the 602 untreated infants. Considerable inter- and intra-center variability was demonstrated in the rate of VI and/or HC use and the lowest BP on the day of VI or HC initiation.
Conclusions
Despite published expert opinion guidance regarding BP management in extremely preterm infants, our results suggest a continued lack of consensus result in both inter- and intra-center variability in practice. Well-designed studies in the field are urgently needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Batton B, Li L, Newman NS, Das A, Watterberg KL, Yoder BA, et al. Use of antihypotensive therapies in extremely preterm infants. Pediatrics. 2013;131:e1865–73.
Dempsey EM. Challenges in treating low blood pressure in preterm infants. Child (Basel, Switz). 2015;2:272–88.
Zubrow AB, Hulman S, Kushner H, Falkner B. Determinants of blood pressure in infants admitted to neonatal intensive care units: a prospective multicenter study. Philadelphia Neonatal Blood Pressure Study Group. J Perinatol Off J Calif Perinat Assoc. 1995;15:470.
Watkins AM, West CR, Cooke RW. Blood pressure and cerebral haemorrhage and ischaemia in very low birthweight infants. Early Hum Dev. 1989;19:103–10.
Versmold HT, Kitterman JA, Phibbs RH, Gregory GA, Tooley WH. Aortic blood pressure during the first 12 h of life in infants with birth weight 610 to 4,220 grams. Pediatrics. 1981;67:607–13.
Hegyi T, Carbone MT, Anwar M, Ostfeld B, Hiatt M, Koons A, et al. Blood pressure ranges in premature infants. I. The first hours of life. J Pediatr. 1994;124:627–33.
Demarini S, Dollberg S, Hoath SB, Ho M, Donovan EF. Effects of antenatal corticosteroids on blood pressure in very low birth weight infants during the first 24 h of life. J Perinatol. 1999;19:419–25.
Stark MJ, Hodyl NA, Andersen CC. Effects of antenatal magnesium sulfate treatment for neonatal neuro-protection on cerebral oxygen kinetics. Pediatr Res. 2015;78:310–4.
Moise AA, Wearden ME, Kozinetz CA, Gest AL, Welty SE, Hansen TN. Antenatal steroids are associated with less need for blood pressure support in extremely premature infants. Pediatrics 1995;95:845–50.
Batton B, Li L, Newman NS, Das A, Watterberg KL, Yoder BA, et al. Evolving blood pressure dynamics for extremely preterm infants. J perinatology: Off J Calif Perinat Assoc. 2014;34:301–5.
Vesoulis ZA, El Ters NM, Wallendorf M, Mathur AM. Empirical estimation of the normative blood pressure in infants <28 weeks gestation using a massive data approach. J perinatology: Off J Calif Perinat Assoc. 2016;36:291–5.
Ahn SY, Kim ES, Kim JK, Shin JH, Sung SI, Jung JM, et al. Permissive hypotension in extremely low birth weight infants (≤1000 gm). Yonsei Med J. 2012;53:765–71.
Cunningham S, Symon AG, Elton RA, Zhu C, McIntosh N. Intra-arterial blood pressure reference ranges, death and morbidity in very low birthweight infants during the first seven days of life. Early Hum Dev. 1999;56:151–65.
Lee J, Rajadurai VS, Tan KW. Blood pressure standards for very low birthweight infants during the first day of life. Arch Dis Child Fetal neonatal Ed. 1999;81:F168–70.
Cordero L, Timan CJ, Waters HH, Sachs LA. Mean arterial pressures during the first 24 h of life in < or = 600-gram birth weight infants. J perinatology: Off J Calif Perinat Assoc. 2002;22:348–53.
LeFlore JL, Engle WD, Rosenfeld CR. Determinants of blood pressure in very low birth weight neonates: lack of effect of antenatal steroids. Early Hum Dev. 2000;59:37–50.
Batton B, Batton D, Riggs T. Blood pressure during the first 7 days in premature infants born at postmenstrual age 23 to 25 weeks. Am J Perinatol. 2007;24:107–15.
Development of audit measures and guidelines for good practice in the management of neonatal respiratory distress syndrome. Report of a Joint Working Group of the British Association of Perinatal Medicine and the Research Unit of the Royal College of Physicians. Arch Dis Child. 1992;67:1221–7.
Logan JW, O’Shea TM, Allred EN, Laughon MM, Bose CL, Dammann O, et al. Early postnatal hypotension and developmental delay at 24 months of age among extremely low gestational age newborns. Arch Dis Child Fetal Neonatal Ed. 2011;96:F321–8.
Logan JW, O’Shea TM, Allred EN, Laughon MM, Bose CL, Dammann O, et al. Early postnatal hypotension is not associated with indicators of white matter damage or cerebral palsy in extremely low gestational age newborns. J Perinatol. 2011;31:524–34.
Alderliesten T, Lemmers PM, van Haastert IC, de Vries LS, Bonestroo HJ, Baerts W, et al. Hypotension in preterm neonates: low blood pressure alone does not affect neurodevelopmental outcome. J Pediatr. 2014;164:986–91.
Helbock HJ, Insoft RM, Conte FA. Glucocorticoid-responsive hypotension in extremely low birth weight newborns. Pediatrics 1993;92:715–7.
Seri I, Tan R, Evans J. Cardiovascular effects of hydrocortisone in preterm infants with pressor-resistant hypotension. Pediatrics 2001;107:1070–4.
Rios DR, Moffett BS, Kaiser JR. Trends in pharmacotherapy for neonatal hypotension. J Pediatr. 2014;165:697–701.
Fanaroff JM, Wilson-Costello DE, Newman NS, Montpetite MM, Fanaroff AA. Treated hypotension is associated with neonatal morbidity and hearing loss in extremely low birth weight infants. Pediatrics 2006;117:1131–5.
Limperopoulos C, Bassan H, Kalish LA, Ringer SA, Eichenwald EC, Walter G, et al. Current definitions of hypotension do not predict abnormal cranial ultrasound findings in preterm infants. Pediatrics 2007;120:966–77.
Halliday HL, Ehrenkranz RA, Doyle LW. Early (<8 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst Rev. 2010;1:CD001146.
Zhang R, Bo T, Shen L, Luo S, Li J. Effect of dexamethasone on intelligence and hearing in preterm infants: a meta-analysis. Neural Regen Res. 2014;9:637–45.
Ramanathan R, Siassi B, deLemos RA. Severe retinopathy of prematurity in extremely low birth weight infants after short-term dexamethasone therapy. J perinatology: Off J Calif Perinat Assoc. 1995;15:178–82. quiz 83-4
Juul SE, Mayock DE, Comstock BA, Heagerty PJ. Neuroprotective potential of erythropoietin in neonates; design of a randomized trial. Matern health, Neonatol Perinatol. 2015;1:27.
Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika 1986;73:13–22.
Stuart EA, King G, Imai K, Ho D MatchIt: nonparametric preprocessing for parametric causal inference. Journal of statistical software. 2011.
Seri I Hemodynamics and Cardiology: Neonatology Questions and Controversies: Elsevier Health Sciences; 2018.
Munro MJ, Walker AM, Barfield CP. Hypotensive extremely low birth weight infants have reduced cerebral blood flow. Pediatrics 2004;114:1591–6.
Miall-Allen VM, de Vries LS, Whitelaw AG. Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child. 1987;62:1068–9.
Laughon M, Bose C, Allred E, O’Shea TM, Van Marter LJ, Bednarek F, et al. Factors associated with treatment for hypotension in extremely low gestational age newborns during the first postnatal week. Pediatrics 2007;119:273–80.
Batton B. Neonatal Blood Pressure Standards: What Is “Normal”? Clin Perinatol. 2020;47:469–85.
Kluckow M, Evans N. Low superior vena cava flow and intraventricular haemorrhage in preterm infants. Arch Dis Child Fetal neonatal Ed. 2000;82:F188–94.
Batton B, Li L, Newman NS, Das A, Watterberg KL, Yoder BA, et al. Early blood pressure, antihypotensive therapy and outcomes at 18-22 months’ corrected age in extremely preterm infants. Arch Dis Child Fetal Neonatal Ed. 2016;101:F201–6.
Durrmeyer X, Marchand-Martin L, Porcher R, Gascoin G, Roze J-C, Storme L, et al. Abstention or intervention for isolated hypotension in the first 3 days of life in extremely preterm infants: association with short-term outcomes in the EPIPAGE 2 cohort study. Arch Dis Child - Fetal Neonatal Ed. 2017;102:490–6.
Dempsey EM, Barrington KJ, Marlow N, O’Donnell CPF, Miletin J, Naulaers G, et al. Hypotension in Preterm Infants (HIP) randomised trial. Arch Dis Child-Fetal Neonatal Ed. 2021;106:398–403.
Vesoulis ZA, Ters NE, Foster A, Trivedi SB, Liao SM, Mathur AM. Response to dopamine in prematurity: a biomarker for brain injury? J perinatology: Off J Calif Perinat Assoc. 2016;36:453–8.
Abdul Aziz AN, Thomas S, Murthy P, Rabi Y, Soraisham A, Stritzke A, et al. Early inotropes use is associated with higher risk of death and/or severe brain injury in extremely premature infants. J Matern-Fetal Neonatal Med. 2020;33:2751–8.
Solanki NS, Hoffman SB. Association between dopamine and cerebral autoregulation in preterm neonates. Pediatr Res. 2020;88:618–22.
Eriksen VR, Hahn GH, Greisen G. Dopamine therapy is associated with impaired cerebral autoregulation in preterm infants. Acta Paediatrica. 2014;103:1221–6.
Mizoguchi MB, Chu TG, Murphy FM, Willits N, Morse LS. Dopamine use is an indicator for the development of threshold retinopathy of prematurity. Br J Ophthalmol. 1999;83:425–8.
Baud O, Maury L, Lebail F, Ramful D, El Moussawi F, Nicaise C, et al. Effect of early low-dose hydrocortisone on survival without bronchopulmonary dysplasia in extremely preterm infants (PREMILOC): a double-blind, placebo-controlled, multicentre, randomised trial. Lancet. 2016;387:1827–36.
Watterberg KL, Gerdes JS, Cole CH, Aucott SW, Thilo EH, Mammel MC, et al. Prophylaxis of early adrenal insufficiency to prevent bronchopulmonary dysplasia: a multicenter trial. Pediatrics 2004;114:1649–57.
Peeples ES. An evaluation of hydrocortisone dosing for neonatal refractory hypotension. J Perinatol. 2017;37:943–6.
Vesoulis ZA, Flower AA, Zanelli S, Rambhia A, Abubakar M, Whitehead HV, et al. Blood pressure extremes and severe IVH in preterm infants. Pediatr Res. 2020;87:69.
Funding
This project was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under award numbers U01NS077953 and U01NS077955.
Author information
Authors and Affiliations
Consortia
Contributions
ESP and BAC contributed to the design, analysis, and interpretation of the data, drafted the initial manuscript, and reviewed and critically revised the manuscript. PJH and SEJ contributed to the design, analysis, collection, and interpretation of the data, and reviewed and critically revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Peeples, E.S., Comstock, B.A., Heagerty, P.J. et al. Blood pressure values and hypotension management in extremely preterm infants: a multi-center study. J Perinatol 42, 1169–1175 (2022). https://doi.org/10.1038/s41372-022-01425-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01425-2