Abstract
Background
The objective of this study was to investigate the association between systolic, diastolic, and mean blood pressures (SBP, DBP, and MBP) and adverse outcomes in preterm neonates with late-onset sepsis (LOS).
Methods
This is a two-center retrospective study over 6 years. Neonates <35 weeks gestational age (GA) with blood ± cerebrospinal fluid culture positive for organisms other than coagulase-negative Staphylococcus at >72 h age were included. Outcome measures were organ dysfunction (ODF) using the predefined criteria and post-ODF mortality (≤7 days from LOS onset). The lowest noninvasive blood pressures (BPs) recorded at baseline (24–48 h pre-LOS) and 0–12, 13–24, 25–36, and 37–48 h post LOS were analyzed.
Results
Of 147 neonates, ODF occurred in 70 (48%), of which 20 (29%) died. ODF was associated with a drop in all BP components, starting 0–12 h post-LOS onset (p < 0.01 for all); BPs remained unchanged in the non-ODF group. Mortality was associated with a greater reduction in SBP [−13 (−19, −8) vs. −4 (−8, 0); p < 0.01] and MBP [−9 (−13, −5) vs. +1 (−1, +4); p = 0.03] 0–12 h post-LOS onset. SBP had a higher area under the curve for mortality than MBP and DBP (0.83, 0.81, and 0.78, respectively). An inverse relation may exist between corrected GA and percentage reduction in SBP from baseline for equivalent risk of death.
Conclusions
Reduction in BPs early in illness may identify preterm neonates at the highest risk of ODF and mortality from LOS.
Impact
-
Drop in BPs from baseline starting in the immediate post-illness onset period may identify preterm neonates at the highest risk of developing ODF and mortality in LOS.
-
Lowest systolic followed by mean BP measured during the first 12 h of illness provided the highest discriminating ability for LOS-related mortality.
-
Absolute BPs recorded during the first 12 h of illness performed better than relative change from baseline for identifying neonates at risk of LOS-related mortality.
-
The specific BP thresholds identified in this study may inform future therapeutic trials.
Similar content being viewed by others
Introduction
Globally, the incidence of neonatal sepsis is 2.2 per 100 live births, with mortality rates ranging between 11 and 19%.1 Premature neonates in neonatal intensive care units (NICUs) are particularly vulnerable to late-onset sepsis (LOS), with its incidence inversely related to gestational age (GA).2 Up to 36% of neonates born <28 weeks GA may experience LOS, with mortality rates as high as 13–40%.3,4,5,6 Physiologically, sepsis is frequently associated with acute alterations in blood pressures (BPs) and organ dysfunction (ODF); the latter referring to a state of compromised function of major organ systems such as cardiovascular, respiratory, renal, and neurological.7,8 The relationship between BPs and ODF and associated mortality during sepsis is well known for older patients, resulting in the inclusion of well-defined BP targets for clinical practice for adult patients in the Surviving Sepsis Campaign guidelines.8,9,10,11,12,13,14 The specific association between BPs and adverse outcomes following LOS remains unknown for premature neonates.
Hence, our primary objective was to examine the relationship between different components of BP (systolic [SBP], mean [MBP], and diastolic [DBP], absolute post-illness values, change from baseline, and relative change from baseline) with the development of ODF during LOS in premature neonates. The secondary objectives were: (1) to examine the associations between these BP-related variables, early in illness (within 12 h after LOS), and LOS-related mortality in neonates with ODF, and (2) to examine the interaction between corrected GA (cGA) and BP threshold, as relevant, in identifying infants at highest risk of mortality after LOS. We hypothesized that premature neonates who develop ODF and mortality after ODF will have lower BPs in comparison to those without these adverse outcomes.
Methods
Design
We conducted a retrospective cohort study in 2018 at the tertiary NICUs of Mount Sinai Hospital (MSH) and Sunnybrook Health Sciences Center (SHSC), University of Toronto, Canada, including data from a 6-year period, between January 2011 and December 2016. The study received approval from both Institutional Research Ethics Boards.
Key definitions
-
i.
Late-onset sepsis: for this study, LOS was defined as positive blood or cerebrospinal fluid (CSF) culture obtained after 72 h of age for organisms other than coagulase-negative Staphylococcus (CoNS). We elected to exclude CoNS from this study as it is known to be associated with a low frequency of adverse outcomes.15 In addition, our center-specific practices such as obtaining only one blood culture sample as part of the LOS workup instead of the recommended two samples,16 and continuation of broad-spectrum antibiotic in CoNS cases demonstrating higher illness severity made it challenging to distinguish true CoNS LOS from contaminants. Excluding CoNS from our study made our study population more reliable.
-
ii.
LOS onset: this was defined by the timing of the first investigation related to the evaluation for the LOS episode.
-
iii.
Organ dysfunction: currently there is no validated definition of ODF in preterm neonates. For this study, informed by the pediatric sepsis literature and typical normal values acceptable for premature neonates, a definition of ODF was adapted a priori to identify likely significant alteration.17 Our intent for developing the criteria for ODF was to identify patients who develop any organ function-related complication from LOS to allow examination of their BP profiles in comparison to those who remain relatively unaffected. The criteria included the occurrence of any of the following: (1) base excess <−8 mEq/L. This cut-off was selected as the “normal” range for preterm neonates during the first 28 days of life is suggested to be ±5 mEq/L.18 (2) Renal dysfunction, defined as urine output (UO) < 1 mL/kg/h over any 8-h period or serum creatinine ≥100 μmol/L.19 (3) Severe hypoxic respiratory failure, defined as FiO2 1.0 for ≥2 consecutive hours despite invasive mechanical ventilation, and (4) sudden cardiac arrest. We did not include serum lactate values in our definition of ODF as it was not routinely measured at our centers during the study period. Only the first criteria that were met by the patients to be classified as ODF was recorded as part of this study.
-
iv.
LOS-related mortality was defined as death ≤7 days from LOS onset.
Patient selection
All neonates born at <35 weeks GA who had LOS as per study definition during the study period were eligible for inclusion. Health records of eligible patients, identified from each unit’s electronic database, were reviewed for the following exclusion criteria: (1) known chromosomal or congenital anomaly, (2) positive culture considered as a contaminant, defined by discontinuation of antibiotic therapy <5 days, (3) necrotizing enterocolitis ≥Bell’s stage 2A diagnosed on the same day as LOS onset, and (4) transfer to another tertiary facility <7 days from LOS onset, as it was not feasible to ascertain study outcomes. Only the first episode of LOS for each patient was included for analysis.
Blood pressure measurements
Only noninvasive blood pressure (NIBP) measurements were extracted for analysis due to the following considerations: (1) among preterm neonates invasive BP monitoring is typically initiated in high acuity cases, introducing a selection bias in the study population. (2) Peripheral arterial line insertion and its maintenance to ensure reliable readings over long periods can be technically challenging in this population, often resulting in intermittent data availability. The use of NIBPs not only ensured the inclusion of all eligible patients and generalizability of study findings but also allowed us to investigate the relevance of change in BPs from baseline values that are typically only available as NIBP.
Data collection
In addition to the demographic and perinatal characteristics, specific LOS-related data extracted included pre-existing morbidities, type of organism (gram positive or gram negative), presence of meningitis, occurrence of adverse outcomes (ODF, mortality), and their timing. ODF diagnosed within 2 h of LOS onset was considered as “ODF at presentation.” All BPs (SBP, DBP, and MBP) were recorded over the 24-h period between 24 and 48 h preceding LOS onset (baseline period), and for 48 h after LOS onset were extracted. For this study, the lowest BPs recorded during the baseline period and each of the four 12-h periods after LOS onset (0–12, 13–24, 25–36, and 37–48 h) were considered for analysis.
Study setting
The study NICUs are high-volume inborn centers primarily caring for high-risk premature neonates. Like a typical tertiary NICU, the evaluation of patients for LOS was based on the clinical team’s interpretation of patient’s symptoms and included starting empirical treatment with broad-spectrum antibiotics after obtaining a minimal set of laboratory investigations (blood, urine, and CSF samples for culture and sensitivities, and blood sample for complete blood count and capillary or arterial blood gas). Additional and subsequent investigations were at the attending team’s discretion and often informed by patient’s illness severity. As per routine care, all physiological parameters, including details of respiratory support, were documented hourly and UO, which was measured from the weighted diapers, was calculated every 8 h. The practice regarding NIBP measurements was also typical for tertiary NICUs. These were routinely measured for all patients, by the bedside nurse, at a minimum frequency of 6–12 h at baseline. Routine NIBP measurements were also taken in those with indwelling arterial catheters. Measurements were obtained using the oscillometric method (DINAMBP Pro; GE Healthcare, Tampa, FL) from one of the limbs using a standard technique, with preference given to the right arm.20 Typically, in study units, if NIBP is unexpectedly abnormal, the bedside nurse would repeat the measurement at least once to confirm its reliability. If repeat measurements differ significantly, the reading closest to the normal range for the neonate is recorded, unless directed otherwise by the medical team.
Outcomes
The primary outcome was the occurrence of ODF, as defined above, ≤7 days from LOS onset. The secondary outcome was death ≤7 days from LOS onset.
Statistics
Data are presented as number (frequency), mean (±standard deviation), or median (interquartile range), as appropriate. Intergroup comparison was performed between neonates with and without ODF, using χ2 or Fisher’s exact test, and Student’s t test or Wilcoxon’s rank-sum test, as appropriate. For our primary objective, the lowest absolute BP and change from baseline (both absolute change and percentage change) during each of the four 12-h periods after LOS onset were compared between groups using mixed-effect models for repeated measures. SBP, DBP, and MBP were analyzed individually. The results were also presented after adjusting for potential confounders identified on univariate analysis. For the secondary objective, within the ODF group, BP-related variables were compared between those who died ≤7 days vs. those who survived >7 days after LOS onset. The ability of relevant BP parameters to identify infants who met the adverse outcome was examined by calculating the area under the curve (AUC) using receiver-operating characteristic (ROC) curve analysis. For ODF, only BPs within 12 h immediately preceding ODF occurrence were used and patients who had ODF at the presentation itself were not included. For LOS-related mortality, the lowest BPs during the first 12 h after LOS onset were examined, as early identification would be clinically most meaningful. AUCs were also calculated after adjusting for cGA. Further, to examine the interaction between cGA and relevant BP thresholds, logistic regression analysis was conducted, where, in addition to the lowest BPs during the first 12 h of illness, cGA and the interaction term between BP and cGA were included in the model [logit(prob(Y = 1|BP,cGA)) = a0 + a1 × BP + a2 × cGA + a3BP × cGA…]. The regression equation was computed, as relevant, incorporating cGA to derive BP thresholds, which may identify neonates at the highest risk of mortality following LOS, and respective sensitivity and specificity were reported based on the best cut-off determined by the Youden’s index, which maximizes the sum of sensitivity and specificity.21 Analyses were performed using SAS 9.4 (SAS Inc., Cary NC, USA). Two-sided p value < 0.05 was considered statistically significant.
Results
Of the 195 potentially eligible neonates, 147 were included for analyses. The reasons for exclusion were NEC at LOS onset (n = 18), transferred to another tertiary center (n = 12), incomplete documentation (n = 16), and positive culture from contaminants (n = 2). The mean GA and weight at birth and at LOS were 25.9 ± 1.9 and 829 ± 258 and 29.2 ± 3.6 weeks and 1045 ± 529 g, respectively. Only two neonates were >34 weeks and the remaining were <32 weeks GA. The distribution of cGA at illness was as follows: 65 infants (44.2%) <28 weeks, 61 (41.5%) 28–32 weeks, 19 (12.9%), 32–40 weeks, and 2 (1.4%) >40 weeks. The distribution of organisms included gram positive (n = 63), gram negative (n = 71), both gram positive and negative (n = 7), and Candida species (n = 6).
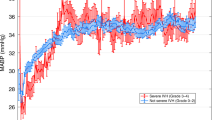
Blood pressures and ODF
Overall, 70 (48%) neonates fulfilled the predecided criteria for ODF. The first criteria that were met in the majority were base deficit >8 mEq/L (62.9%), followed by renal dysfunction (27.1%), hypoxic respiratory failure (8.6%), and sudden cardiac arrest (1.4%). The median (interquartile range [IQR]) time to ODF from LOS onset was 3.4 (0.8, 9.5) h; 28 had ODF at presentation. ODF was more frequently associated with gram-negative bacteremia and meningitis, while other baseline characteristics were similar between groups (Table 1). While baseline BPs were similar between groups, the ODF group demonstrated significantly lower SBP, MBP, and DBP, starting within the first 12-h period after LOS onset (Supplemental Fig. S1). The BPs in the non-ODF group remained unchanged. Both absolute post-LOS BPs and greater change from baseline were associated with ODF, even after accounting for the type of organism and meningitis (Table 2). On ROC analysis, after excluding patients with ODF at presentation, the predictive ability of SBP, DBP, and MBP for ODF was low (AUCs 0.63, 0.63, and 0.65, respectively).
Blood pressures and mortality after ODF
The analysis for mortality was restricted to the ODF subgroup as the outcome of LOS-related mortality was largely restricted to this cohort [20/70 (28.6%) vs. 2/77 (2.6%); p < 0.01]. There was no significant difference in the baseline characteristics between ODF neonates who survived vs. died following LOS (Supplemental Table S1) There was also no significant difference in the median (IQR) BP readings recorded over the 48-h period between those who died vs. those who survived [12.5 (5.5–16.0) vs. 11.0 (7.0–26.0; p = 0.65)]. Mortality was associated with lower BPs and a greater drop from baseline, with the greatest decline observed in SBP and MBP (Table 3). Among the various BP variables, the lowest absolute BPs recorded in the first 12 h performed better at identifying neonates who died (AUCs ranging from 0.78 to 0.83) compared with ΔBP (AUCs 0.60–0.71) and percentage change in BP (0.62–0.73). Among the BP components, the absolute lowest SBP in the first 12 h performed better in comparison to MBP and DBP (AUC 0.83 vs. 0.81 vs. 0.78, respectively). While SBP cut-offs demonstrated the highest individual sensitivity (95%, cut-off 51 mm Hg) and specificity (91%, cut-off 36 mm Hg), the best combination was seen with MBP [sensitivity 80%, specificity 77% for cut-off of 31 mm Hg].
Interaction between cGA and BP thresholds
Whilst both GA at birth and cGA correlated with baseline BPs, the correlation coefficients were greater for cGA compared to GA (with SBP r = 0.48 vs. 0.35, DBP r = 0.45 vs. 0.34, MBP r = 0.48 vs. 0.37, for cGA and GA, respectively). Hence, cGA was used in subsequent analysis. Despite adjusting for cGA, the AUCs for the lowest absolute BPs during the first 12 h of illness (AUCs ranging from 0.80 to 0.83) remained higher than those for ΔBPs (AUCs 0.70–0.77) and percentage change in BPs (AUCs 0.71– 0.79). Similarly, SBP in the first 12 h continued to perform better than MBP and DBP (AUC 0.83 vs. 0.81 vs. 0.80, respectively, after adjusting for cGA). The following regression equations were identified, incorporating cGA and SBP variables in the first 12 h of illness, to derive thresholds to identify neonates at risk of death after LOS across the range of cGA from 23 to 46 weeks:
For absolute post-illness SBP: SBP ≤ (5.23–0.34 × cGA)/(0.185–0.0105 × cGA), provides a sensitivity of 0.70 and specificity of 0.87.
For percentage change in SBP from baseline: %SBP ≤ (−7.68 + 0.297 × cGA)/(0.0766–0.0042 × cGA), provides a sensitivity and specificity of 0.75 and 0.74, respectively.
The equation demonstrated an inverse relationship between derived cut-offs and increasing cGA. The neonates at lower cGA at illness demonstrated an equivalent risk of death at a relatively higher SBP threshold and a lower percentage change in BP from baseline compared to neonates with higher cGA at illness (Fig. 1a, b).
a Absolute systolic blood pressure (SBP) and b percentage change in SBP from baseline (%BP) thresholds identifying neonates at risk of death after late-onset sepsis (LOS) in relation to corrected gestational age (cGA) across the range of cGA from 23 to 46 weeks. The lowest SBP in the first 12 h post LOS onset was used for the analysis. There is an inverse relationship between cut-offs and increasing cGA. Neonates at lower cGA demonstrate an equivalent risk of death at a relatively higher SBP threshold and a lower percentage change in BP from baseline compared to those with higher cGA at illness. X-axis: cGA at LOS. Y-axis: a SBP and b %BP. LOS late-onset sepsis.
Discussion
The maintenance of BP to sustain adequate organ performance during critical illness is a key hemodynamic goal in critical care medicine.22 A number of studies have reported adverse outcomes in association with the use of inotropes; however, to our knowledge, no previous study has specifically examined the BP components and their association with adverse outcomes in preterm neonates with LOS. Similar studies from adult patients, however, demonstrated the association between low MBP and risk of mortality, and acute renal and myocardial injury.23,24 Based on these and subsequent investigations, Surviving Sepsis Campaign guidelines have prescribed an MBP target of at least 65 mm Hg for the management of sepsis in adults.25 Although interventions to support BP during LOS are frequently undertaken in NICUs, there is limited data to guide practice. Typically, in neonatal practice MBP equivalent to cGA is targeted to guide interventions.26,27 This stems from studies and practices surrounding transitional hypotension in preterm neonates, and its extrapolation to acquired acute illnesses such as LOS cannot be recommended.28
In this large cohort study of premature neonates with LOS, we demonstrate that a drop in BPs from baseline may distinguish patients who are at the highest risk of developing ODF and mortality after ODF, starting in the immediate period after LOS onset. Although, in comparison to baseline BP, the majority of post-illness BP variables remained significantly low throughout the 48 h time period in infants with adverse outcomes, the magnitude of difference reduced over time, particularly after 24–36 h of illness onset. This may be reflective of the effect of interventions or disease process improving over time. During the time period, the interpretation and management of BPs were variable and at the discretion of the attending team. The absence of a standard approach did not allow us to investigate the effect of the response to interventions. For these reasons, we limited our time period to the first 12 h post LOS in mortality analysis, where the impact of these factors will be expected to be the lowest. Future studies should examine the role of interventions on the relationship between BPs and adverse outcomes in LOS in neonates, ideally in the context of a standardized management protocol. Further, our intention by creating a composite definition of ODF was to facilitate the identification of neonates who develop organ function-related complications after LOS vs. those who remained relatively unaffected, to allow the examination of their BP profiles. We do not suggest that the individual categories of ODF are equivalent in nature and nor was our aim to determine their individual relationships with BP and LOS-related mortality. This will have to be examined in the future. Nevertheless, our study highlights the need for increased vigilance for monitoring BP changes in premature neonates with suspected LOS, and perhaps a lower threshold to initiate continuous invasive monitoring in identified at-risk patients. Our data suggest that, similar to studies from adult patients, clinically relevant specific BP thresholds may also exist for LOS in premature neonates.
Another observation of our study was the inverse interaction between increasing cGA and BP thresholds to identify infants at the highest risk of death. Neonates with lower cGA at illness demonstrated an equivalent risk of death at a higher BP threshold and lower percentage change in BP from baseline compared to those with more advanced cGA. These results are counterintuitive to the typical clinical practice, where lower cGA patients would have lower BP thresholds for initiating treatment. We propose that our findings reflect the physiological protective effect of increasing maturity on death from an acute illness such as LOS. Host tolerance to cardiovascular insufficiency associated with LOS may increase with cGA. Whilst these thresholds may aid in risk stratification and selecting patients for enhanced monitoring, we do not recommend targeting these thresholds for treatment decisions until further validation and testing in future therapeutic trials. Our study, however, provides the necessary background and rationale for designing such trials and for future quality improvement work aimed at improving outcomes for this vulnerable patient population.
The predominant hemodynamic phenotype in sepsis, and consequently the ability of BP to reflect circulatory sufficiency, depends on the balance between vasoconstrictor (cold shock) and vasodilatory (warm shock) mediators, and maybe developmentally regulated. For instance, the predominant presentation in adults with sepsis is that of warm shock resulting in significant hypotension,29,30 while the typical sepsis phenotype in older children associated with mortality is that of cold shock, which may result in near-normal BP despite insufficient circulation.31 Data from physiological studies show that, similar to adult patients, premature neonates primarily demonstrate a warm shock physiology during LOS.32,33 This may explain the clinical relevance of BPs in this population as noted in our study. However, due to the lack of data we are unable to confirm and stratify our findings based on the type of shock. While we anticipate the majority of LOS-associated shock in premature neonates to be vasodilatory in nature, we would recommend careful appraisal at the bedside. It is likely that our results may not be applicable to the patients presenting with a vasoconstrictive response to LOS.
We found the predictive ability was better for SBP than MBP, albeit by a small margin, and SBP cut-offs provided superior sensitivity and specificity. Although typical NICU practices and most of the previous research in this field are focused on MBP, the clinical relevance of SBP is increasingly being recognized. In extremely preterm neonates, lower SBP on admission is associated with early mortality and severe brain injury.34 In a previous echocardiographic study, our group noted that SBP, but not MBP or DBP, correlated positively with left ventricular output (LVO), a surrogate marker of systemic blood flow.35 Neonates with low LVO demonstrated lower SBP than those with normal or high LVO (58 ± 18 vs. 64 ± 14 mm Hg, p < 0.01). It is thus possible that higher SBP during LOS may reflect better hemodynamic compensation to a vasodilatory state, providing for relatively preserved circulation supporting organ performance. Further physiological studies are needed to examine the relationship between BP components and makers of circulatory sufficiency, ideally using noninvasive means such as echocardiography, near-infrared spectroscopy, or noninvasive continuous cardiac output monitoring. Interestingly, our findings echo those in the geriatric population where SBP has shown to have an inverse relationship with in-hospital mortality during sepsis.36
In addition to the retrospective design, our findings should be interpreted in the context of important limitations. Although this is a large cohort of premature neonates with LOS, our findings are based on fewer neonates meeting the outcome of mortality, as it is a relatively infrequent outcome. Second, although CoNS LOS is a common finding in NICUs, we have excluded this in our study for the reasons stated above. However, we anticipate that the results would remain applicable for CoNS LOS, but the exact cut-off BP values may vary and need to be confirmed. Third, there is no validated definition of ODF in this population, needing us to develop an a priori definition based on consensus. However, our definition was able to identify those at the highest risk of mortality. Fourth, given the study design, we are unable to verify the rigor followed for obtaining BP measurements, which may affect the exact threshold identified in our study. Although we found an association between BP and ODF, the predictive ability was relatively poor. This may be due to a significant number of neonates who had to be excluded from this analysis as they had “ODF at presentation,” which may have tempered our results. Lastly, during the study period, there was no standardized policy on the frequency of BP monitoring in cases of suspected LOS in our units. While it is expected that in clinical practice patients perceived to be sick may receive a higher frequency of monitoring, we found no difference in the overall number of readings recorded between infants who died after LOS vs. survivors. We are not able to comment on the applicability of our findings for invasive BP readings.
Conclusion
Reduction in BPs from baseline, starting early in the illness, is associated with ODF in premature neonates with LOS, with greater reduction occurring in those with the highest risk of mortality after ODF. Among BP variables during the first 12 h of illness, SBP, both for absolute post-illness values and percentage change from baseline, performed better than MBP and DBP for identifying patients at the highest risk of LOS-related mortality. Patients with lower cGA may demonstrate an equivalent risk of death at a relatively higher post-illness BP and lower percentage change from baseline compared to neonates with higher cGA. These results may aid in risk stratification, identify patients for enhanced monitoring, and inform future interventional studies in this population.
References
Fleischmann-Struzek, C. et al. The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir. Med. 6, 223–230 (2018).
Stoll, B. J. et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126, 443–456 (2010).
Cohen-Wolkowiez, M. et al. Early and late onset sepsis in late preterm infants. Pediatr. Infect. Dis. J. 28, 1052–1056 (2009).
Stoll, B. J. et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 110, 285–291 (2002).
El Manouni El Hassani, S. et al. Risk factors for late-onset sepsis in preterm infants: a multicenter case-control study. Neonatology 116, 42–51 (2019).
Dong, Y. & Speer, C. P. Late-onset neonatal sepsis: recent developments. Arch. Dis. Child. Fetal Neonatal Ed. 100, F257–F263 (2015).
Jones, A. E., Trzeciak, S. & Kline, J. A. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit. Care Med. 37, 1649–1654 (2009).
Schlapbach, L. J., Straney, L., Bellomo, R., MacLaren, G. & Pilcher, D. Prognostic accuracy of age-adapted SOFA, SIRS, PELOD-2, and qSOFA for in-hospital mortality among children with suspected infection admitted to the intensive care unit. Intens. Care Med. 44, 179–188 (2018).
Weiss, S. L. et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intens. Care Med. 46, 10–67 (2020).
Bestati, N. et al. Differences in organ dysfunctions between neonates and older children: a prospective, observational, multicenter study. Crit. Care 14, R202 (2010).
Wynn, J. L. & Polin, R. A. A neonatal sequential organ failure assessment score predicts mortality to late-onset sepsis in preterm very low birth weight infants. Pediatr. Res. 88, 85–90 (2020).
Marik, P. E. & Taeb, A. M. SIRS, qSOFA and new sepsis definition. J. Thorac. Dis. 9, 943–945 (2017).
Seymour, C. W. et al. Assessment of clinical criteria for sepsis: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315, 762–774 (2016).
Rhodes, A. et al. Surviving sepsis campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intens. Care Med. 43, 304–377 (2017).
Lim, W. H. et al. Prevalence and pathogen distribution of neonatal sepsis among very-low-birth-weight infants. Pediatr. Neonatol. 53, 228–234 (2012).
Horan, T. C., Andrus, M. & Dudeck, M. A. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am. J. Infect. Control 36, 309–332 (2008).
Goldstein, B., Giroir, B. & Randolph, A., International Consensus Conference on Pediatric, S. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr. Crit. Care Med. 6, 2–8 (2005).
Rennie, J. M. & Roberton, N. C. Rennie and Roberton’s Textbook of Neonatology (Churchill Livingston, 2012).
Kellum, J. A., Lameire, N. & Group, K. A. G. W. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit. Care 17, 204 (2013).
Dionne, J. M. et al. Method of blood pressure measurement in neonates and infants: a systematic review and analysis. J. Pediatr. 221, 23–31.e25 (2020).
Youden, W. J. Index for rating diagnostic tests. Cancer 3, 32–35 (1950).
Rivers, E. et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N. Engl. J. Med. 345, 1368–1377 (2001).
Asfar, P. et al. High versus low blood-pressure target in patients with septic shock. N. Engl. J. Med. 370, 1583–1593 (2014).
Dunser, M. W. et al. Arterial blood pressure during early sepsis and outcome. Intens. Care Med. 35, 1225–1233 (2009).
Rhodes, A. et al. Surviving sepsis campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit. Care Med. 45, 486–552 (2017).
Seri, I. & Noori, S. Diagnosis and treatment of neonatal hypotension outside the transitional period. Early Hum. Dev. 81, 405–411 (2005).
Development of audit measures and guidelines for good practice in the management of neonatal respiratory distress syndrome. Report of a Joint Working Group of the British Association of Perinatal Medicine and the Research Unit of the Royal College of Physicians. Arch. Dis. Child. 67, 1221–1227 (1992).
Bada, H. S. et al. Mean arterial blood pressure changes in premature infants and those at risk for intraventricular hemorrhage. J. Pediatr. 117, 607–614 (1990).
Parker, M. M. et al. Profound but reversible myocardial depression in patients with septic shock. Ann. Intern. Med. 100, 483–490 (1984).
Parker, M. M., Shelhamer, J. H., Natanson, C., Alling, D. W. & Parrillo, J. E. Serial cardiovascular variables in survivors and nonsurvivors of human septic shock: heart rate as an early predictor of prognosis. Crit. Care Med. 15, 923–929 (1987).
Davis, A. L. et al. American College of Critical Care Medicine Clinical Practice Parameters for Hemodynamic Support of Pediatric and Neonatal Septic Shock. Crit. Care Med. 45, 1061–1093 (2017).
Saini, S. S., Kumar, P. & Kumar, R. M. Hemodynamic changes in preterm neonates with septic shock: a prospective observational study*. Pediatr. Crit. Care Med. 15, 443–450 (2014).
de Waal, K. & Evans, N. Hemodynamics in preterm infants with late-onset sepsis. J. Pediatr. 156, 918–922.e911 (2010).
Lyu, Y. et al. Admission systolic blood pressure and outcomes in preterm infants of </= 26 weeks’ gestation. Am. J. Perinatol. 34, 1271–1278 (2017).
Kharrat, A. et al. The relationship between blood pressure parameters and left ventricular output in neonates. J. Perinatol. 39, 619–625 (2019).
Warmerdam, M. et al. The association between systolic blood pressure and in-hospital mortality in older emergency department patients who are hospitalised with a suspected infection. Emerg. Med. J. 35, 619–622 (2018).
Funding
No specific funding was secured for this study.
Author information
Authors and Affiliations
Contributions
F.Z. participated in the initial study design, made substantial contributions to data acquisition, and produced the first draft of the manuscript. M.B. and A.K. reviewed the study protocol, made substantial contributions to data acquisition, reviewed the manuscript, and provided critical feedback. X.Y.Y. performed all statistical analysis for the study, reviewed the manuscript, and provided critical feedback. D.W. reviewed the study protocol and made significant intellectual contributions to the study design and completion of this project, reviewed the manuscript, and provided crucial critical feedback. A.J. conceived the research question, conceptualized the initial study design and data collection forms. and revised the final draft of the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work in ensuring that questions related to its accuracy or integrity are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Patient consent was not required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhu, F., Baczynski, M., Kharrat, A. et al. Blood pressure, organ dysfunction, and mortality in preterm neonates with late-onset sepsis. Pediatr Res 92, 498–504 (2022). https://doi.org/10.1038/s41390-021-01768-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01768-0
This article is cited by
-
Early Blood Pressure Changes in Neonatal Sepsis and the Risk of Mortality
Indian Journal of Pediatrics (2023)