Abstract
Objective
To examine quality measures for moderate and late preterm (MLP) infants.
Study design
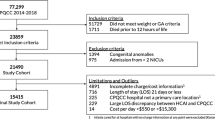
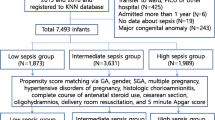
By prospectively analyzing Vermont Oxford Network’s all NICU admissions database, we adapted Baby-MONITOR, a composite quality measure for extremely/very preterm infants, for MLP infants. We examined correlations between the adapted MLP quality measure (MLP-QM) in MLP infants and Baby-MONITOR in extremely and very preterm infants.
Result
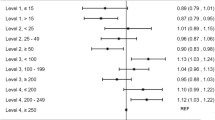
We studied 376,219 MLP (30–36 weeks GA) and 57,595 extremely/very preterm (25–29 weeks GA) infants from 465 U.S. hospitals born from 2016 to 2020. MLP-QM summary scores in MLP infants had weak correlation with Baby-MONITOR scores in extremely and very preterm infants (r = 0.47). There was weak correlation among survival (r = 0.19), no pneumothorax (r = 0.35), and no infection after 3 days (r = 0.45), but strong correlation among human milk at discharge (r = 0.79) and no hypothermia (r = 0.76).
Conclusion
Modest correlation among hospital care measures in two preterm populations suggests the need for MLP-specific care measures.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Please contact authors regarding code availability.
References
Shapiro-Mendoza CK, Lackritz EM. Epidemiology of late and moderate preterm birth. Semin Fetal Neonatal Med. 2012;17:120–5.
Teune MJ, Bakhuizen S, Bannerman CG, Opmeer BC, Van Kaam AH, Van Wassenaer AG, et al. A systematic review of severe morbidity in infants born late preterm. Am J Obstet Gynecol. 2011;205:374.e1–374.e9.
Stewart DL, Barfield WD. Updates on an at-risk population: Late-preterm and early-term infants. Pediatrics. 2019;144:e20192760.
Phibbs CS, Schmitt SK, Cooper M, Gould JB, Lee HC, Profit J, et al. Birth hospitalization costs and days of care for mothers and neonates in California, 2009–2011. J Pediatr. 2019;204:118–25.
McCormick MC, Escobar GJ, Zheng Z, Richardson DK. Place of birth and variations in management of late preterm (“near-term”) infants. Semin Perinatol. 2006;30:44–7.
Profit J, Gould JB, Zupancic J, Stark AR, Wall KM, Kowalkowski MA, et al. Formal selection of measures for a composite index of NICU quality of care: Baby-MONITOR. J Perinatol. 2011;31:702–10.
Profit J, Kowalkowski MA, Zupancic JA, Pietz K, Richardson P, Draper D, et al. Baby-MONITOR: a composite indicator of NICU quality. Pediatrics. 2014;134:X8–X8.
Profit J, Gould JB, Bennett M, Goldstein BA, Draper D, Phibbs CS, et al. The Association of Level of Care with NICU Quality. Pediatrics. 2016;137:e20144210.
Profit J, Gould JB, Bennett M, Goldstein BA, Draper D, Phibbs CS, et al. Racial/ethnic disparity in NICU quality of care delivery. Pediatrics. 2017;140:e20170918.
Horbar JD, Edwards EM, Greenberg LT, Profit J, Draper D, Helkey D, et al. Racial Segregation and Inequality in the Neonatal Intensive Care Unit for Very Low-Birth-Weight and Very Preterm Infants. JAMA Pediatr. 2019;173:455–61.
Edwards E, Greenberg L, Profit J, Draper D, Helkey D, Horbar J. Quality of Care in US NICUs by Race and Ethnicity. Pediatrics. 2021;148:e2020037622.
Sebastião YV, Womack LS, Castillo HL, Balakrishnan M, Bruder K, Alitz P, et al. Hospital Variations in Unexpected Complications Among Term Newborns. Pediatrics. 2017;139:e20162364.
Clapp MA, James KE, Bates SV, Kaimal AJ. Patient and hospital factors associated with unexpected newborn complications among term neonates in US hospitals. JAMA Netw Open. 2020;3:e19194–98.
Horbar JD, Edwards EM, Greenberg LT, Morrow KA, Soll RF, Buus-Frank ME, et al. Variation in Performance of Neonatal Intensive Care Units in the United States. JAMA Pediatr. 2017;171:e164396.
Vermont Oxford Network. Manual of operations: Part 1. Guidelines for database participation (Burlington; VT: Vermont Oxford Network; 2016).
Jensen E, Dysart K, Gantz M, McDonald S, Bamat N, Keszler M, et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. an evidence-based approach. Am J Respir Crit Care Med. 2019;200:751–9.
Patel AL, Engstrom JL, Meier PP, Kimura RE. Accuracy of methods for calculating postnatal growth velocity for extremely low birth weight infants. Pediatrics. 2005;116:1466–73.
Simon L, Hanf M, Frondas-Chauty A, Darmaun D, Rouger V, Gascoin G, et al. Neonatal growth velocity of preterm infants: The weight Z-score change versus Patel exponential model. PLoS One. 2019;14:e0218746.
Altman M, Vanpée M, Cnattingius S, Norman M. Moderately preterm infants and determinants of length of hospital stay. Arch Dis Child Fetal Neonatal Ed. 2009;94:414–8.
Escobar GJ, McCormick MC, Zupancic JAF, Coleman-Phox K, Armstrong MA, Greene JD, et al. Unstudied infants: outcomes of moderately premature infants in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2006;91:238–44.
Profit J, McCormick MC, Escobar GJ, Richardson DK, Zheng Z, Coleman-Phox K, et al. Neonatal intensive care unit census influences discharge of moderately preterm infants. Pediatrics. 2007;119:314–9.
Lee HC, Bennett MV, Schulman J, Gould JB, Profit J. Estimating length of stay by patient type in the neonatal intensive care unit. Am J Perinatol. 2016;33:751–7.
Seaton SE, Barker L, Draper ES, Abrams KR, Modi N, Manktelow BN. Estimating neonatal length of stay for babies born very preterm. Arch Dis Child Fetal Neonatal Ed. 2019;104:F182–6.
Bannwart DdeC, Rebello CM, Sadeck LS, Pontes MD, Ramos JL, Leone CR. Prediction of length of hospital stay in neonatal units for very low birth weight infants. J Perinatol. 1999;19:92–6.
Cegolon L, Mastrangelo G, Campbell OM, Giangreco M, Alberico S, Montasta L, et al. Length of stay following cesarean sections: A population based study in the Friuli Venezia Giulia region (North-Eastern Italy), 2005-15. PLoS One. 2019;14:e0210753.
Cegolon L, Campbell O, Alberico S, Montico M, Mastrangelo G, Monasta L, et al. Length of stay following vaginal deliveries: A population based study in the Friuli Venezia Giulia region (North-Eastern Italy), 2005-15. PLoS One. 2019;14:e0204919.
Draper D, Gittoes M. Statistical analysis of performance indicators in UK higher education. J R Stat Soc. 2004;167:449–74.
Britton J. Altitude, oxygen and the definition of bronchopulmonary dysplasia. J Perinatol. 2012;32:880–5.
Helkey D. DD. dghrank: construct Draper-Gittoes-Helkey institution rankings. [Internet]. 2018. [accessed 12 Dec 2018]. https://github.com/dhelkey/dghrank.
Dhurjati R, Sigurdson K, Profit J. Patient- and family-centered care as a dimension of quality. Am J Med Qual. 2019;34:307–8.
Aberson C. Applied power analysis for the behavioral sciences. (New York, NY: Taylor & Francis Group LLC; 2010).
Escobar GJ, Clark RH, Greene JD. Short-term outcomes of infants born at 35 and 36 weeks gestation: We need to ask more questions. Semin Perinatol. 2006;30:28–33.
Profit J, Typpo KV, Hysong SJ, Woodard LCD, Kallen MA, Petersen LA. Improving benchmarking by using an explicit framework for the development of composite indicators: an example using pediatric quality of care. Implement Sci. 2010;5:1–10.
Rosenthal G. Weak associations between hospital mortality rates for individual diagnoses: implications for profiling hospital quality. Am J Public Health. 1997;87:429–33.
National Quality Forum. Endorsement Summary: Cardiovascular Measures [Internet]. 2012 [accessed 9 Dec 2021]. https://www.qualityforum.org/News_And_Resources/Endorsement_Summaries/Endorsement_Summaries.aspx.
National Quality Forum. Endorsement summary: pulmonary and critical care measures [Internet]. 2012 [accessed 9 Dec 2021]. https://www.qualityforum.org/News_And_Resources/Endorsement_Summaries/Endorsement_Summaries.aspx.
National Quality Forum. Endorsement Summary: Neurology Measures [Internet]. 2013 [accessed 9 Dec 2021]. https://www.qualityforum.org/News_And_Resources/Endorsement_Summaries/Endorsement_Summaries.aspx.
National Quality Forum. Perinatal and Women’s Health, Spring 2020 Cycle, CDP Report. 2021.
Silber JH, Rosenbaum PR, Ross RN, Ludwig JM, Wang W, Niknam BA, et al. A hospital-specific template for benchmarking its cost and quality. Heal Serv Res. 2014;49:1475–97.
Silber J, Rosenbaum P, Ross R, Ludwig J, Wang W, Niknam B, et al. Indirect standardization matching: assessing specific advantage and risk synergy. Health Serv Res. 2016;51:2330–57.
Schulman J, Braun D, Lee HC, Profit J, Duenas G, Bennett MV, et al. Association between neonatal intensive care unit admission rates and illness acuity. JAMA Pediatr. 2018;172:17–23.
Edwards EMHJ. Variation in use by NICU types in the United States. Pediatrics 2018;142:e20180457.
Smazal A, Kavars A, Carlson S, Tolaizy T, Dagle J. Peripherally inserted central catheters optimize nutrient intake in moderately preterm infants. Pediatr Res. 2016;80:185–9.
Duong HH, Mirea L, Shah PS, Yang J, Lee SK, Sankaran K. Pneumothorax in neonates: trends, predictors and outcomes. J Neonatal Perinat Med. 2014;7:29–38.
Acknowledgements
We are indebted to our colleagues who submit data to VON on behalf of infants and their families. The list of centers contributing data to this study is in Supplementary Table 4.
Author information
Authors and Affiliations
Contributions
Elizabeth G Salazar conceptualized and designed the study, drafted the initial manuscript, reviewed and revised the manuscript. Sara C Handley conceptualized and designed the study, critically reviewed and revised the manuscript. Lucy T Greenberg carried out the analyses, critically reviewed and revised the manuscript. Scott A Lorch conceptualized and designed the study, critically reviewed and revised the manuscript. Erika M Edwards conceptualized and designed the study, carried out and oversaw the analyses, critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
Erika M Edwards receives salary support from Vermont Oxford Network. Lucy T Greenberg is an employee of Vermont Oxford Network. T32HL098054 (to EGS). There are no additional conflicts of interest to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Salazar, E.G., Handley, S.C., Greenberg, L.T. et al. Measuring quality of care in moderate and late preterm infants. J Perinatol 42, 1294–1300 (2022). https://doi.org/10.1038/s41372-022-01377-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01377-7
This article is cited by
-
The impact of volume and neonatal level of care on outcomes of moderate and late preterm infants
Journal of Perinatology (2024)