Abstract
Objective
We sought to determine if fetuses with prenatally diagnosed congenital heart disease (CHD) were more likely to undergo cesarean delivery in the setting of a non-reassuring fetal heart rate tracing (NRFHT) and to determine if those fetuses were more likely to have a fetal acidosis.
Study design
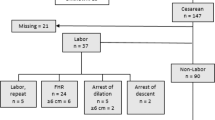
A retrospective cohort study of neonates prenatally diagnosed with CHD from August 2010 to July 2016. The control group consisted of gestational age matched controls without CHD.
Results
Each group consisted of 143 patients. The most common reason for cesarean delivery was a NRFHT (control 31% vs CHD 35%, p = 0.67). Fetal acidosis was a rare outcome occurring in only five controls (3.5%) and 11 cases (7.7%) (p = 0.12).
Conclusion
These findings demonstrate that with multidisciplinary care coordination, fetuses with a prenatal diagnosis of CHD have similar cesarean rates, labor and delivery management, and delivery room compromise as healthy fetuses.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
“Data and Statistics of Congential Heart Defects.” Congenital Heart Defects, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention. Accessed 2 Nov 2018. http://www.cdc.gov/ncbddd/heartdefects/data.html.
Donofrio MT. Predicting the future: delivery room planning of congenital heart disease diagnosed by fetal echocardiography. Am J Perinatol. 2018;35:549–52.
Sanapo L, Pruetz JD, Slodki M, Goens MB, Moon-Grady AJ, Donofrio MT. Fetal echocardiography for planning perinatal and delivery room care of neonates with congenital heart disease. Echocardiography. 2017;34:1804–21.
Cnota JF, Gupta R, Michelfelder EC, Ittenbach RF. Congenital heart disease infant death rates decrease as gestational age advances from 34 to 40 weeks. J Pediatr. 2011;159:761–5.
Landis BJ, Levey A, Levasseur SM, Glickstein JS, Kleinman CS, Simpson LL, et al. Prenatal diagnosis of congenital heart disease and birth outcomes. Pediatr Cardiol. 2013;34:597–605.
Trento LU, Pruetz JD, Chang RK, Detterich J, Sklansky MS. Prenatal diagnosis of congenital heart disease: Impact of mode of delivery on neonatal outcome. Prenat Diagn. 2012;32:1250–5.
Walsh CA, MacTiernan A, Farrell S, Mulcahy C, McMahon CJ, Franklin O, et al. Mode of delivery in pregnancies complicated by major fetal congenital heart disease: a retrospective cohort study. J Perinatol. 2014;34:901–5.
Peyvandi S, Nguyen TA, Almeida-Jones M, Boe N, Rhee L, Anton T, et al. Timing and mode of delivery in prenatally diagnosed congenital heart disease- an analysis of practices within the university of california fetal consortium (UCfC). Pediatr Cardiol. 2017;38:588–95.
Parikh LI, Grantz KL, Iqbal SN, Huang CC, Landy HJ, Fries MH, et al. Neonatal outcomes in fetuses with cardiac anomalies and the impact of delivery route. Am J Obstet Gynecol. 2017;217:469.e1–e12.
American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 106: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol. 2009;114:192–202.
Alfirevic Z, Devane D, Gyte GM, Cuthbert A. Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database Syst Rev. 2017;2:CD006066.
Ueda K, Ikeda T, Iwanaga N, Katsuragi S, Yamanaka K, Neki R, et al. Intrapartum fetal heart rate monitoring in cases of congenital heart disease. Am J Obstet Gynecol. 2009;201:64.e1–e6.
Donofrio MT, Levy RJ, Schuette JJ, Skurow-Todd K, Sten MB, Stallings C, et al. Specialized delivery room planning for fetuses with critical congenital heart disease. Am J Cardiol. 2013;111:737–47.
Donofrio MT, Moon-Grady AJ, Hornberger LK, Copel JA, Sklansky MS, Abuhamad A, et al. Diagnosis and treatment of fetal cardiac disease: a scientific statement from the american heart association. Circulation 2014;129:2183–242.
Donofrio MT, Skurow-Todd K, Berger JT, McCarter R, Fulgium A, Krishnan A, et al. Risk-stratified postnatal care of newborns with congenital heart disease determined by fetal echocardiography. J Am Soc Echocardiogr. 2015;28:1339–49.
American College of Obstetricians and Gynecologists. Practice bulletin no. 116: management of intrapartum fetal heart rate tracings. Obstet Gynecol. 2010;116:1232–40.
Nardozza LMM, Zamarian ACP, Araujo Junior E. New definition of fetal growth restriction: Consensus regarding a major obstetric complication. Rev Bras Ginecol Obstet. 2017;39:315–6.
“Updated National Birth Prevalence Estimates for Selected Birth Defects | CDC.” Birth Defects, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention. Accessed 1 Nov 2018. https://www.cdc.gov/ncbddd/birthdefects/features/birthdefects-keyfindings.html.
Perez-Delboy A, Simpson LL. Prenatal sonographic diagnosis of congenital heart disease and intrauterine growth restriction: a case-control study. J Clin Ultrasound. 2007;35:376–81.
Wallenstein MB, Harper LM, Odibo AO, Roehl KA, Longman RE, Macones GA, et al. Fetal congenital heart disease and intrauterine growth restriction: a retrospective cohort study. J Matern Fetal Neonatal Med. 2012;25:662–5.
Song MS, Hu A, Dyamenahalli U, Chitayat D, Winsor EJ, Ryan G, et al. Extracardiac lesions and chromosomal abnormalities associated with major fetal heart defects: Comparison of intrauterine, postnatal and postmortem diagnoses. Ultrasound Obstet Gynecol. 2009;33:552–9.
Randis TM, Rice MM, Myatt L, Tita ATN, Leveno KJ, Reddy UM, et al. Incidence of early-onset sepsis in infants born to women with clinical chorioamnionitis. J Perinat Med. 2018;46:926–33.
Hoppe KK, Schiff MA, Benedetti TJ, Delaney S. Duration of spontaneous active labor and perinatal outcomes using contemporary labor curves. Am J Perinatol. 2018;35:1186–91.
Faiz AS, Ananth CV. Etiology and risk factors for placenta previa: an overview and meta-analysis of observational studies. J Matern Fetal Neonatal Med. 2003;13:175–90.
Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol 1997;177:210–4.
American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. Obstetric care consensus no. 1: safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014;123:693–711.
Miyoshi T, Katsuragi S, Neki R, Kurosaki KI, Shiraishi I, Nakai M, et al. Cardiovascular profile score as a predictor of acute intrapartum non-reassuring fetal status in infants with congenital heart defects. J Matern Fetal Neonatal Med. 2017;30:2831–7.
Yeh P, Emary K, Impey L. The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: analysis of 51,519 consecutive validated samples. BJOG. 2012;119:824–31.
Victory R, Penava D, Da Silva O, Natale R, Richardson B. Umbilical cord pH and base excess values in relation to adverse outcome events for infants delivering at term. Am J Obstet Gynecol 2004;191:2021–8.
Committee on Obstetric Practice American Academy of Pediatrics - Committee on Fetus and Newborn. Committee opinion no. 644: the apgar score. Obstet Gynecol. 2015;126:e52–5.
Penfield CA, Hong C, Ibrahim Sel H, Kilpatrick SJ, Gregory KD. Easy as ABC: a system to stratify category II fetal heart rate tracings. Am J Perinatol. 2016;33:688–95.
Soncini E, Paganelli S, Vezzani C, Gargano G, Giovanni Battista LS. Intrapartum fetal heart rate monitoring: Evaluation of a standardized system of interpretation for prediction of metabolic acidosis at delivery and neonatal neurological morbidity. J Matern Fetal Neonatal Med. 2014;27:1465–9.
Dadlez NM, Brubaker SG, Simpson LL, Yilmaz B, Williams IA. Impact of change in delivery practice on neonatal and maternal outcomes in cases of significant congenital heart disease. Congenit Heart Dis. 2014;9:368–72.
Peterson AL, Quartermain MD, Ades A, Khalek N, Johnson MP, Rychik J. Impact of mode of delivery on markers of perinatal hemodynamics in infants with hypoplastic left heart syndrome. J Pediatr. 2011;159:64–9.
Acknowledgements
The authors would like to thank MedStar Health Research Institute for assistance with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Adams, A.D., Aggarwal, N., Fries, M.H. et al. Neonatal and maternal outcomes of pregnancies with a fetal diagnosis of congenital heart disease using a standardized delivery room management protocol. J Perinatol 40, 316–323 (2020). https://doi.org/10.1038/s41372-019-0528-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0528-1