Abstract
Introduction
Absent risk stratification, variable physiology of ductal-dependent congenital heart disease (DD-CHD) imparts risk of over-medicalization and unnecessary exclusion from early parental bonding.
Methods
Single-center retrospective cohort study of term infants with isolated prenatally diagnosed DD-CHD expected to require immediate advanced resuscitation/intervention (2005–2017). Standardized documentation (2015 onward) included diagnosis, expected saturations, and allowability of postnatal parental bonding.
Results
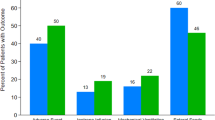
The study cohort (n = 386) included 289 patients in the pre-standardized documentation era and 97 in the post-era; the groups had similar characteristics. Fewer infants were born by cesarean in the later era (32% vs. 22%; p = 0.049). Decrease in any respiratory intervention (38–26%; p = 0.03) followed standardized documentation. More patients had any bonding time (22–74%; p < 0.0001), without increase in CPAP or intubation in the first two hours of life (6.9% vs. 7.2%; p = 0.92).
Conclusion
Standardized predelivery documentation for neonates with DD-CHD decreased unnecessary respiratory intervention and increased parental bonding.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
van der Linde D, Konings EE, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJ, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;58:2241–7.
Botto LD, Correa A, Erickson JD. Racial and temporal variations in the prevalence of heart defects. Pediatrics. 2001;107:E32.
Oster ME, Lee KA, Honein MA, Riehle-Colarusso T, Shin M, Correa A. Temporal trends in survival among infants with critical congenital heart defects. Pediatrics. 2013;131:e1502–8.
Donofrio MT. Predicting the future: delivery room planning of congenital heart disease diagnosed by Fetal Echocardiography. Am J Perinatol. 2018;35:549–52.
Donofrio MT, Skurow-Todd K, Berger JT, McCarter R, Fulgium A, Krishnan A, et al. Risk-stratified postnatal care of newborns with congenital heart disease determined by fetal echocardiography. J Am Soc Echocardiogr. 2015;28:1339–49.
Slodki M, Respondek-Liberska M, Pruetz JD, Donofrio MT. Fetal cardiology: changing the definition of critical heart disease in the newborn. J Perinatol. 2016;36:575–80.
Popat H, Kluckow M. Noninvasive assessment of the early transitional circulation in healthy term infants. Neonatology. 2012;101:166–71.
Schultz AH, Localio AR, Clark BJ, Ravishankar C, Videon N, Kimmel SE. Epidemiologic features of the presentation of critical congenital heart disease: implications for screening. Pediatrics. 2008;121:751–7.
Shiraishi H, Yanagisawa M. Bidirectional flow through the ductus arteriosus in normal newborns: evaluation by Doppler color flow imaging. Pediatr Cardiol. 1991;12:201–5.
Aghdas K, Talat K, Sepideh B. Effect of immediate and continuous mother-infant skin-to-skin contact on breastfeeding self-efficacy of primiparous women: a randomised control trial. Women Birth. 2014;27:37–40.
Beiranvand S, Valizadeh F, Hosseinabadi R, Pournia Y. The effects of skin-to-skin contact on temperature and breastfeeding successfulness in full-term newborns after cesarean delivery. Int J Pediatr. 2014;2014:846486.
Bystrova K, Widstrom AM, Matthiesen AS, Ransjo-Arvidson AB, Welles-Nystrom B, Wassberg C, et al. Skin-to-skin contact may reduce negative consequences of “the stress of being born”: a study on temperature in newborn infants, subjected to different ward routines in St. Petersburg. Acta Paediatr. 2003;92:320–6.
Handlin L, Jonas W, Petersson M, Ejdeback M, Ransjo-Arvidson AB, Nissen E, et al. Effects of sucking and skin-to-skin contact on maternal ACTH and cortisol levels during the second day postpartum-influence of epidural analgesia and oxytocin in the perinatal period. Breastfeed Med. 2009;4:207–20.
Moore ER, Bergman N, Anderson GC, Medley N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2016;11:CD003519.
Bystrova K, Ivanova V, Edhborg M, Matthiesen AS, Ransjo-Arvidson AB, Mukhamedrakhimov R, et al. Early contact versus separation: effects on mother-infant interaction one year later. Birth. 2009;36:97–109.
Feldman R, Rosenthal Z, Eidelman AI. Maternal-preterm skin-to-skin contact enhances child physiologic organization and cognitive control across the first 10 years of life. Biol Psychiatry 2014;75:56–64.
O’Higgins M, Roberts IS, Glover V, Taylor A. Mother-child bonding at 1 year; associations with symptoms of postnatal depression and bonding in the first few weeks. Arch Women’s Ment Health. 2013;16:381–9.
Barker PCA, Tatum GH, Campbell MJ, Camitta MGW, Milazzo AS, Hornik CP, et al. Improving maternal-infant bonding after prenatal diagnosis of CHD. Cardiol Young. 2018;28:1306–15.
Stevens J, Schmied V, Burns E, Dahlen H. Immediate or early skin-to-skin contact after a Caesarean section: a review of the literature. Matern Child Nutr. 2014;10:456–73.
Ashmeade TL, Haubner L, Collins S, Miladinovic B, Fugate K. Outcomes of a neonatal golden hour implementation project. Am J Med Qual. 2016;31:73–80.
Reynolds RD, Pilcher J, Ring A, Johnson R, McKinley P. The Golden Hour: care of the LBW infant during the first hour of life one unit’s experience. Neonatal Netw. 2009;28:211–9. quiz 55-8
Zecca E, de Luca D, Costa S, Marras M, de Turris P, Romagnoli C. Delivery room strategies and outcomes in preterm infants with gestational age 24-28 weeks. J Matern Fetal Neonatal Med. 2006;19:569–74.
Edwards MO, Kotecha SJ, Kotecha S. Respiratory distress of the term newborn infant. Paediatr Respir Rev. 2013;14:29–36. quiz -7
Saugstad OD. Oxidative stress in the newborn-a 30-year perspective. Biol Neonate. 2005;88:228–36.
Tan A, Schulze AA, O’Donnell CPF, Davis PG. Air versus oxygen for resuscitation of infants at birth. Cochrane Database Syst Rev. 2005. https://doi.org/10.1002/14651858.CD002273.
Walsh BK, Smallwood CD. Pediatric oxygen therapy: a review and update. Respir Care. 2017;62:645–61.
Naumburg E, Bellocco R, Cnattingius S, Jonzon A, Ekbom A. Supplementary oxygen and risk of childhood lymphatic leukaemia. Acta Paediatr. 2002;91:1328–33.
Spector LG, Klebanoff MA, Feusner JH, Georgieff MK, Ross JA. Childhood cancer following neonatal oxygen supplementation. J Pediatr. 2005;147:27–31.
Keebler JR, Lazzara EH, Patzer BS, Palmer EM, Plummer JP, Smith DC, et al. Meta-analyses of the effects of standardized handoff protocols on patient, provider, and organizational outcomes. Hum Factors. 2016;58:1187–205.
Rychik J, Donaghue DD, Levy S, Fajardo C, Combs J, Zhang X, et al. Maternal psychological stress after prenatal diagnosis of congenital heart disease. J Pediatr. 2013;162:302–7 e1.
Sklansky M, Tang A, Levy D, Grossfeld P, Kashani I, Shaughnessy R, et al. Maternal psychological impact of fetal echocardiography. J Am Soc Echocardiogr. 2002;15:159–66.
Kapadia VS, Chalak LF, Sparks JE, Allen JR, Savani RC, Wyckoff MH. Resuscitation of preterm neonates with limited versus high oxygen strategy. Pediatrics. 2013;132:e1488–96.
Newnam KM. Oxygen saturation limits and evidence supporting the targets. Adv Neonatal Care. 2014;14:403–9.
Perlman JM, Wyllie J, Kattwinkel J, Wyckoff MH, Aziz K, Guinsburg R, et al. Part 7: neonatal resuscitation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132(16 Suppl 1):S204–41.
Vaucher YE, Peralta-Carcelen M, Finer NN, Carlo WA, Gantz MG, Walsh MC, et al. Neurodevelopmental outcomes in the early CPAP and pulse oximetry trial. N Engl J Med. 2012;367:2495–504.
Wyckoff MH, Aziz K, Escobedo MB, Kapadia VS, Kattwinkel J, Perlman JM, et al. Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S543–60.
Author information
Authors and Affiliations
Contributions
IT conceptualized and designed the study, collected data, drafted the initial paper and reviewed and revised the paper. SG conceptualized and designed the study, supervised data collection, and reviewed and revised the paper. NTL conceptualized and designed the study and reviewed and revised the paper. SY carried out the statistical analysis and reviewed and revised the paper. RL designed the data collection instruments, supervised data collection and carried out parts of the analysis. All authors approved the final paper as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Thomas, I., Laventhal, N.T., Yu, S. et al. Impact of standardized prenatal documentation among newborns with ductal-dependent heart disease. J Perinatol 40, 1531–1536 (2020). https://doi.org/10.1038/s41372-020-0674-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0674-5