Abstract
Objective
To compare neurodevelopmental outcomes in linear growth-restricted (LGR) infants born <29 weeks with and without weight gain out of proportion to linear growth.
Study design
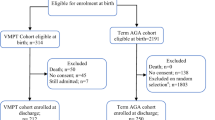
We compared 2-year neurodevelopmental outcomes between infants with and without LGR and between LGR infants with and without weight gain out of proportion to linear growth. The outcomes were Bayley-III cognitive, motor, and language scores, cerebral palsy, Gross Motor Function Classification System (GMFCS) level ≥ 2, and neurodevelopmental impairment.
Result
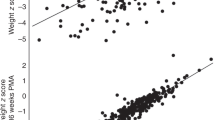
In total, 1227 infants were analyzed. LGR infants were smaller and less mature at birth, had higher BMI, and had lower Bayley-III language scores (82.3 vs. 85.0, p < 0.05). Among infants with LGR, infants with high BMI had lower language scores compared with those with low-to-normal BMI (80.8 vs. 83.3, p < 0.05), and were more likely to have GMFCS level ≥2 and neurodevelopmental impairment.
Conclusion
Among infants with LGR, weight gain out of proportion to linear growth was associated with poorer neurodevelopmental outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Belfort MB, Rifas-Shiman SL, Sullivan T, Collins CT, McPhee AJ, Ryan P, et al. Infant growth before and after term: effects on neurodevelopment in preterm infants. Pediatrics. 2011;128:e899–906.
Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006;117:1253–61.
Kan E, Roberts G, Anderson PJ, Doyle LW. Victorian Infant Collaborative Study G. The association of growth impairment with neurodevelopmental outcome at eight years of age in very preterm children. Early Hum Dev. 2008;84:409–16.
Latal-Hajnal B, von Siebenthal K, Kovari H, Bucher HU, Largo RH. Postnatal growth in VLBW infants: significant association with neurodevelopmental outcome. J Pediatr. 2003;143:163–70.
Modi M, Saluja S, Kler N, Batra A, Kaur A, Garg P, et al. Growth and neurodevelopmental outcome of VLBW infants at 1 year corrected age. Indian Pediatr. 2013;50:573–7.
Ramel SE, Demerath EW, Gray HL, Younge N, Boys C, Georgieff MK. The relationship of poor linear growth velocity with neonatal illness and two-year neurodevelopment in preterm infants. Neonatology. 2012;102:19–24.
Belfort MB, Gillman MW, Buka SL, Casey PH, McCormick MC. Preterm infant linear growth and adiposity gain: trade-offs for later weight status and intelligence quotient. J Pediatr. 2013;163:1564–9 e1562.
Forbes GB. Relation of lean body mass to height in children and adolescents. Pediatr Res. 1972;6:32–37.
Meyers JM, Bann CM, Stoll BJ, D’Angio CT, Bell EF, Duncan AF, et al. Neurodevelopmental outcomes in postnatal growth-restricted preterm infants with postnatal head-sparing. J Perinatol. 2016;36:1116–21.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Olsen IE, Lawson ML, Ferguson AN, Cantrell R, Grabich SC, Zemel BS, et al. BMI curves for preterm infants. Pediatrics. 2015;135:e572–581.
Newman JE, Bann CM, Vohr BR, Dusick AM, Higgins RD, Follow-Up Study Group of Eunice Kennedy Shriver National Institute of Child H. et al. Improving the Neonatal Research Network annual certification for neurologic examination of the 18-22 month child. J Pediatr. 2012;161:1041–6.
Bayley N. Bayley scales of infant and toddler development. San Antonio, TX: Harcourt Assessment; 2006.
Palisano RJ, Hanna SE, Rosenbaum PL, Russell DJ, Walter SD, Wood EP, et al. Validation of a model of gross motor function for children with cerebral palsy. Phys Ther. 2000;80:974–85.
Stevens TP, Shields E, Campbell D, Combs A, Horgan M, La Gamma EF, et al. Variation in enteral feeding practices and growth outcomes among very premature infants: a report from the New York state perinatal quality collaborative. Am J Perinatol. 2016;33:9–19.
Stefanescu BM, Gillam-Krakauer M, Stefanescu AR, Markham M, Kosinski JL. Very low birth weight infant care: adherence to a new nutrition protocol improves growth outcomes and reduces infectious risk. Early Hum Dev. 2016;94:25–30.
Cooke RW. Are there critical periods for brain growth in children born preterm? Arch Dis Child Fetal Neonatal Ed. 2006;91:F17–20.
Fugelstad ARR, Georgieff M. The Role of Nutrition in Cognitive Development. Handbook in Developmental Cognitive Neuroscience, 2nd edn. Cambridge, MA: MIT Press; 2008.
Georgieff MK. Nutrition and the developing brain: nutrient priorities and measurement. Am J Clin Nutr. 2007;85:614S–20.
Lang CH, Frost RA. Glucocorticoids and TNFalpha interact cooperatively to mediate sepsis-induced leucine resistance in skeletal muscle. Mol Med. 2006;12:291–9.
Lang CH, Frost RA. Sepsis-induced suppression of skeletal muscle translation initiation mediated by tumor necrosis factor alpha. Metabolism. 2007;56:49–57.
Ahmad I, Zaldivar F, Iwanaga K, Koeppel R, Grochow D, Nemet D, et al. Inflammatory and growth mediators in growing preterm infants. J Pediatr Endocrinol Metab. 2007;20:387–96.
Eliakim A, Nemet D, Ahmad I, Zaldivar F, Koppel R, Grochow D, et al. Growth factors, inflammatory cytokines and postnatal bone strength in preterm infants. J Pediatr Endocrinol Metab. 2009;22:733–40.
Karagianni P, Tsakalidis C, Kyriakidou M, Mitsiakos G, Chatziioanidis H, Porpodi M, et al. Neuromotor outcomes in infants with bronchopulmonary dysplasia. Pediatr Neurol. 2011;44:40–6.
Synnes A, Luu TM, Moddemann D, Church P, Lee D, Vincer M, et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch Dis Child Fetal Neonatal Ed. 2017;102:F235–4.
Brumbaugh JE, Colaizy TT, Patel NM, Klein JM. The changing relationship between bronchopulmonary dysplasia and cognition in very preterm infants. Acta Paediatr. 2018;107:1339–44.
Laughon M, O’Shea MT, Allred EN, Bose C, Kuban K, Van Marter LJ, et al. Chronic lung disease and developmental delay at 2 years of age in children born before 28 weeks’ gestation. Pediatrics. 2009;124:637–48.
Wood AJ, Raynes-Greenow CH, Carberry AE, Jeffery HE. Neonatal length inaccuracies in clinical practice and related percentile discrepancies detected by a simple length-board. J Paediatr Child Health. 2013;49:199–203.
Acknowledgements
The National Institutes of Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), and the National Center for Advancing Translational Sciences (NCATS) provided grant support for the Neonatal Research Network’s Generic Database and Follow-up Studies. NICHD staff provided input into the study design, conduct, analysis, and manuscript drafting; NCATS cooperative agreements provided infrastructure support to the NRN. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Data collected at participating sites of the NICHD Neonatal Research Network (NRN) were transmitted to RTI International, the data coordinating center (DCC) for the network, which stored, managed, and analyzed the data included in this study. On behalf of the NRN, Dr. Abhik Das (DCC Principal Investigator) and Sylvia Tan (DCC Statistician) had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
We are indebted to our medical and nursing colleagues and the infants and their parents who agreed to take part in this study. The following investigators, in addition to those listed as authors, participated in this study:
NRN Steering Committee Chair: Michael S. Caplan, MD, University of Chicago, Pritzker School of Medicine.
Alpert Medical School of Brown University and Women & Infants Hospital of Rhode Island (UG1 HD27904)—Abbot R. Laptook, MD; Martin Keszler, MD; Betty R. Vohr, MD; Angelita M. Hensman, MS RNC-NIC; Elisa Vieira, RN BSN; Emilee Little, RN BSN; Barbara Alksninis, PNP; Mary Lenore Keszler, MD; Andrea M. Knoll; Theresa M. Leach, MEd CAES; Elisabeth C. McGowan, MD; Victoria E. Watson, MS CAS.
Case Western Reserve University, Rainbow Babies & Children’s Hospital (UG1 HD21364)—Michele C. Walsh, MD MS; Avroy A. Fanaroff, MD; Anna Maria Hibbs, MD MSCE; Nancy S. Newman, BA RN; Allison H. Payne, MD MS; Deanne E. Wilson-Costello, MD; Bonnie S. Siner, RN; Monika Bhola, MD; Gulgun Yalcinkaya, MD; Harriet G. Friedman, MA.
Children’s Mercy Hospital, University of Missouri Kansas City School of Medicine (UG1 HD68284)—William E. Truog, MD; Eugenia K. Pallotto, MD MSCE; Howard W. Kilbride MD; Cheri Gauldin, RN BS CCRC; Anne Holmes RN MSN MBA-HCM CCRC; Kathy Johnson RN, CCRC; Allison Knutson, BSN RNC-NIC.
Cincinnati Children’s Hospital Medical Center, University Hospital, and Good Samaritan Hospital (UG1 HD27853)—Brenda B. Poindexter, MD MS; Kurt Schibler, MD; Barbara Alexander, RN; Cathy Grisby, BSN CCRC; Teresa L. Gratton, PA; Lenora Jackson, CRC; Kristin Kirker, CRC; Greg Muthig, BS; Stacey Tepe, BS; Kimberly Yolton, PhD.
Duke University School of Medicine, University Hospital, University of North Carolina, and Duke Regional Hospital (UG1 HD40492, UL1 TR1117, UL1 TR1111)—Ronald N. Goldberg, MD; C. Michael Cotten, MD MHS; Ricki F. Goldstein, MD; William F. Malcolm, MD; Patricia L. Ashley, MD PHD; Kimberley A. Fisher, PhD FNP-BC IBCLC; Joanne Finkle, RN JD; Kathryn E. Gustafson, PhD; Matthew M. Laughon, MD MPH; Carl L. Bose, MD; Janice Bernhardt, MS RN; Gennie Bose, RN; Janice Wereszczak CPNP-AC/PC.
Emory University, Children’s Healthcare of Atlanta, Grady Memorial Hospital, and Emory University Hospital Midtown (UG1 HD27851)—David P. Carlton, MD; Ellen C. Hale, RN BS CCRC; Ira Adams-Chapman, MD; Yvonne Loggins, RN; Sheena L. Carter, PhD; Maureen Mulligan LaRossa, RN; Lynn C. Wineski, RN MS; Diane I. Bottcher, RN MSN; Colleen Mackie, BS RRT.
Eunice Kennedy Shriver National Institute of Child Health and Human Development—Rosemary D. Higgins, MD; Stephanie Wilson Archer, MA.
Indiana University, University Hospital, Methodist Hospital, Riley Hospital for Children, and Wishard Health Services (UG1 HD27856)—Gregory M. Sokol, MD; Brenda B. Poindexter, MD MS; Lu-Ann Papile, MD; Heidi M. Harmon, MD MS; Abbey C. Hines, PsyD; Leslie Dawn Wilson, BSN CCRC; Dianne E. Herron, RN CCRC; Susan Gunn, NNP CCRC; Lucy Smiley CCRC.
McGovern Medical School at the University of Texas Health Science Center at Houston, Children’s Memorial Hermann Hospital, and Memorial Hermann Southwest (UG1 HD87229, U10 HD21373)—Kathleen A. Kennedy, MD MPH; Jon E. Tyson, MD MPH; Elizabeth Allain, MS; Julie Arldt-McAlister, RN BSN; Allison G. Dempsey, PhD; Carmen Garcia, RN CCRP; Janice John, CPNP; Patrick M. Jones, MD; Layne M. Lillie, RN BSN; Karen Martin, RN; Sara C. Martin, RN; Georgia E. McDavid, RN; Shawna Rodgers, RN; Saba Siddiki, MD; Daniel Sperry, RN; Sharon L. Wright, MT (ASCP).
Nationwide Children’s Hospital and the Ohio State University Medical Center (UG1 HD68278)—Pablo J. Sánchez, MD; Leif D. Nelin, MD; Sudarshan R. Jadcherla, MD; Christine A. Fortney, PhD RN; Patricia Luzader, RN; Gail E. Besner; Nehal A. Parikh, MD.
RTI International (U10 HD36790)—Abhik Das PhD; Dennis Wallace, PhD; Jamie E. Newman, PhD MPH; Jeanette O’Donnell Auman, BS; Margaret Crawford, BS; Jenna Gabrio, BS CCRP; Marie G. Gantz, PhD; Carolyn M. Petrie Huitema, MS; Kristin M. Zaterka-Baxter, RN BSN.
Stanford University and Lucile Packard Children’s Hospital (UG1 HD27880, UL1 TR93)—Krisa P. Van Meurs, MD; David K. Stevenson, MD; Susan R. Hintz, MD MS Epi; M. Bethany Ball, BSc CCRC; Melinda S. Proud, RCP; Barbara Bentley, PsychD MSEd; Maria Elena DeAnda, PhD; Anne M. DeBattista, RN PNP PhD; Beth Earhart, PhD; Lynne C. Huffman, MD; Casey E. Krueger, PhD; Ryan Lucash, PhD; Hali E. Weiss, MD.
University of Alabama at Birmingham Health System and Children’s Hospital of Alabama (UG1 HD34216, M01 RR32)—Waldemar A. Carlo, MD; Namasivayam Ambalavanan, MD; Myriam Peralta-Carcelen, MD MPH; Monica V. Collins, RN BSN MaEd; Shirley S. Cosby, RN BSN; Fred J. Biasini, PhD; Kristen C. Johnston, MSN CRNP; Cryshelle S. Patterson, PhD; Vivien A. Phillips, RN BSN; Sally Whitley, MA OTR-L FAOTA.
University of California—Los Angeles, Mattel Children’s Hospital, Santa Monica Hospital, Los Robles Hospital and Medical Center, and Olive View Medical Center (UG1 HD68270) – Uday Devaskar, MD; Meena Garg, MD; Isabell B. Purdy, PhD CPNP; Teresa Chanlaw, MPH; Rachel Geller, RN BSN.
University of Iowa and Mercy Medical Center (UG1 HD53109)—Tarah T. Colaizy, MD MPH; Jane E. Brumbaugh, MD; Dan L. Ellsbury, MD; Karen J. Johnson, RN BSN; Jacky R. Walker, RN; Donia B. Campbell, RNC-NIC; Diane L. Eastman, RN CPNP MA.
University of New Mexico Health Sciences Center (UG1 HD53089, UL1 TR41)—Kristi L. Watterberg, MD; Jean R. Lowe, PhD; Janell F. Fuller, MD; Robin K. Ohls, MD; Conra Backstrom Lacy, RN; Andrea F. Duncan, MD; Tara Dupont, MD; Elizabeth Kuan, RN BSN; Sandra Sundquist Beauman, MSN RNC-NIC.
University of Pennsylvania, Hospital of the University of Pennsylvania, Pennsylvania Hospital, and Children’s Hospital of Philadelphia (UG1 HD68244)—Barbara Schmidt, MD MSc; Haresh Kirpalani, MB MSc; Sara B. DeMauro, MD MSCE; Aasma S. Chaudhary, BS RRT; Soraya Abbasi, MD; Toni Mancini, RN BSN CCRC; Judy C. Bernbaum, MD; Marsha Gerdes, PhD; Hallam Hurt, MD; Noah Cook, MD; Dara M. Cucinotta, RN.
University of Rochester Medical Center, Golisano Children’s Hospital, and the University of Buffalo Women’s and Children’s Hospital of Buffalo (UG1 HD68263, UL1 TR42)—Satyan Lakshminrusimha, MD; Anne Marie Reynolds, MD MPH; Rosemary L. Jensen; Joan Merzbach, LMSW; Gary J. Myers, MD; Ashley Williams, MSEd; Kelley Yost, PhD; William Zorn, PhD; Karen Wynn, RN; Deanna Maffett, RN; Diane Prinzing; Julianne Hunn, BS; Stephanie Guilford, BS; Farooq Osman, MD; Mary Rowan, RN; Michael G. Sacilowski, BS; Holly I.M. Wadkins, MA; Melissa Bowman, MSN; Cait Fallone, MA; Kyle Binion, BS; Constance Orme; Ann Marie Scorsone, MS CCRC; Michelle Andrews-Hartley, MD.
University of Texas Southwestern Medical Center, Parkland Health & Hospital System, and Children’s Medical Center Dallas (UG1 HD40689)—Myra H. Wyckoff, MD; Pablo J. Sánchez, MD; Luc P. Brion, MD; Diana M. Vasil, MSN BSN; Lijun Chen, PhD RN; Roy J. Heyne, MD; Sally S. Adams, MS RN CPNP; Elizabeth Heyne, PsyD PA-C; Alicia Guzman; Lizette E. Lee, RN; Catherine Twell Boatman, MS CIMI.
Wayne State University, Hutzel Women’s Hospital and Children’s Hospital of Michigan (UG1 HD21385)—Seetha Shankaran MD; Athina Pappas, MD; Girija Natarajan, MD; Sanjay Chawla, MD; Monika Bajaj, MD; Melissa February, MD; Prashant Agarwal, MD; Kirsten Childs, RN BSN; Eunice Woldt, RN MSN; Rebecca Bara, RN BSN; Laura A. Goldston, MA; John Barks MD; Mary Christensen, RT; Stephanie Wiggins, MS; Diane White, RT.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Meyers, J.M., Tan, S., Bell, E.F. et al. Neurodevelopmental outcomes among extremely premature infants with linear growth restriction. J Perinatol 39, 193–202 (2019). https://doi.org/10.1038/s41372-018-0259-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0259-8
This article is cited by
-
A review and guide to nutritional care of the infant with established bronchopulmonary dysplasia
Journal of Perinatology (2023)
-
Correlation of NICU anthropometry in extremely preterm infants with brain development and language scores at early school age
Scientific Reports (2023)
-
The Optimal State Scoring Tool: guidance for interdisciplinary care of infants with severe bronchopulmonary dysplasia and its relation to linear growth
Journal of Perinatology (2023)
-
Effects of early intake of amino acid on the neurodevelopmental outcomes in very low birth weight infants at correct age of 20 months and school age
Irish Journal of Medical Science (1971 -) (2022)
-
Cord Blood Proteomic Biomarkers for Predicting Adverse Neurodevelopmental Outcomes in Monoamniotic Twins
Reproductive Sciences (2022)