Abstract
Higher blood pressure prior to pregnancy is associated with increased risk of placental abruption, hypertension and preeclampsia, preterm delivery and fetal growth restriction. These conditions are jointly termed placental syndromes as they are characterised by impaired placentation and early placental vascularization. Placental syndromes are associated with an increased maternal risk of progression to hypertension and cardiovascular disease (CVD) in later life. Women affected by both a clinical placental syndrome and with evidence of placental maternal vascular malperfusion (MVM) have a particularly high risk of hypertension and CVD. Yet whether placental impairment and clinical syndromes are causes or consequences of higher blood pressure in women remains unclear. In this review, we address the relationship between blood pressure and maternal health in pregnancy. We conclude that there is a pressing need for studies with a range of detailed measures of cardiac and vascular structure and function taken before, during and after pregnancy to solve the ‘chicken and egg’ puzzle of women’s blood pressure and pregnancy health, and to inform effective precision medicine prevention and treatment of both placental syndromes and chronic hypertension in women.
Similar content being viewed by others
Introduction
Maternal blood pressure decreases very early in the first trimester of pregnancy due to decreased systemic vascular resistance, reaching a nadir at mid-pregnancy after which blood pressure rises and returns to pre-pregnancy levels by term [1,2,3]. Women with hypertension prior to pregnancy are at increased risk of developing a placental syndrome. Placental syndromes include placental abruption, early and late-onset as well as super-imposed preeclampsia, fetal growth restriction, and preterm delivery, suggesting that pre-pregnancy blood pressure may contribute to all of these syndromes [4, 5].
The placenta provides essential nutrient and oxygen exchange to the growing fetus. Impaired placentation and early placental vascularization give rise to clinical placental syndromes; and each of these, in turn, is linked to a higher risk of hypertension after delivery [6,7,8,9]. In this review, we address the evidence as well as knowledge gaps about the links between pregnancy, placental syndromes, and maternal blood pressure, and why placental syndromes may be sex-specific markers of adverse life course blood pressure patterns.
The effect of pregnancy on blood pressure
Several studies have shown that maternal blood pressure falls following pregnancy [10,11,12,13]. Using repeated blood pressure measures from pre-conception up to 40 years post-conception, we have shown that maternal systolic blood pressure (SBP) was −3.32 mmHg (95%CI:−3.93, −2.71) lower and diastolic blood pressure (DBP) −1.98 mmHg (95%CI:−2.43, −1.53) lower after a first pregnancy, with subsequent pregnancies having more modest effects. SBP and DBP changes from pre- to post- second pregnancy were −0.68 (95%CI −1.30, −0.06) and −0.31 (95%CI: −0.75, 0.14), respectively. For the third pregnancy, the results were: −0.24 (95%CI: −1.00, 0.52) and −0.59 (95%CI: −1.13, −0.06). We also found that it takes approximately a decade for parous women to ‘return’ to their pre-pregnancy blood pressure and that the difference between parous and non-parous women lasts beyond the menopause [10].
Similarly, a recent study used firstborn sex as an instrumental variable (or proxy) for number of children, exploiting the preference for sons in India. This preference for male offspring means that on average, women with a first-born daughter have a greater number of children than women with a first-born son. Authors found that parous women (but not men) with a first-born daughter had a -1mmHg (95%CI −1.26, −0.74) lower SBP and a −0.35 mmHg (95%CI: −0.52, −0.17) lower DBP than those with a first-born son [14]. This suggests that a greater number of pregnancies results in lower maternal – but not paternal – blood pressure. Whilst sex-specific effects of child-rearing on blood pressure cannot be completely ruled out, it is more likely that the inverse effect of family size on maternal blood pressure reflects child-bearing, i.e., pregnancy, effects.
Clinical placental syndromes and blood pressure
Women with placental syndromes have approximately a two-fold risk of CVD and CVD-related mortality in later life [15,16,17] compared to women without a history of pregnancy complicated by a placental syndrome, and progression to chronic hypertension has been found to explain a large part of this increased risk. Indeed, European and U.S. preventive guidelines now recognize preeclampsia as a female-specific CVD risk factor [18,19,20]. A recent report using data from the US Nurses’ Health Study II, found that chronic hypertension explained 81% of the increased risk of CVD in women with a first pregnancy affected by gestational hypertension and 48% of the increased CVD risk associated with preeclampsia [15]. These findings are in line with previous reports using data from Norway [21] and the UK [22, 23].
There are three possible explanations for the increased risk of CVD associated with placental syndromes that is largely mediated by chronic hypertension as well as the drop in blood pressure seen post-pregnancy, and they are not mutually exclusive explanations. The first is that women with placental syndromes do not experience a drop in blood pressure after pregnancy like women without a placental syndrome either due to pre-pregnancy factors or as a consequence of the placental syndrome. The second is that women with placental syndromes do experience a comparable drop in blood pressure, but they have higher pre-pregnancy blood pressure. This would suggest that pregnancy is a natural ‘screening test’ that identifies women that have a more adverse cardiovascular health profile prior to pregnancy [24]. Finally, women with placental syndromes may experience a sharper rise in blood pressure in the post-partum years, which would suggest that placental syndromes causally affect blood pressure, through end-organ damage to vasculature or the kidneys, for example.
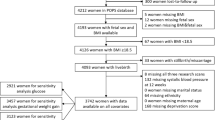
Evidence from a study using linked data from the population-based Norwegian HUNT study and the Medical Birth Registry of Norway shows a comparable drop in SBP following pregnancy in both women with and without hypertension in pregnancy. However, no equivalent drop in DBP in women with hypertension in pregnancy was observed. We also found that women who went on to develop hypertension in pregnancy had a 5 mmHg (95%CI: 3.2, 7.2) higher predicted SBP and a 3.5 mmHg (95%CI: 2.0, 5.0) higher predicted DBP at age 20, prior to pregnancy, compared with women who had a normotensive pregnancy [25]. Similarly, in a smaller preconception cohort study, women who developed preeclampsia or fetal growth restriction (n = 15) had lower cardiac output and cardiac index, and higher total peripheral resistance before pregnancy compared to women who did not have a placental syndrome (n = 205) [26]. Finally, in HUNT, the age-related increase in blood pressure was similar in women with and without hypertension in pregnancy so that by age 60 years, SBP was 9.0 mmHg (95%CI 6.2–11.8) higher and DBP was 2.8 mmHg (95% CI, 1.0–4.6) higher in women with preeclampsia. These findings are in line with the hypothesis that pregnancy is cardiometabolic stress test that identifies women with a greater propensity for CVD. Figure 1 (first published here [25]) shows the prevalence of hypertension in women with preeclampsia (the curve for women with gestational hypertension is virtually identical but not plotted for clarity) compared with women with a normotensive first pregnancy. By age 60 years, 78% and 79% of women with a first preeclamptic and hypertensive pregnancy respectively had hypertension, compared with 58% of women with a normotensive pregnancy.
Similarly, women with a first-born baby who was small-for-gestational-age (SGA) also had higher mean blood pressure across adulthood (from before to after pregnancy) than women with a first-born baby who was appropriate-for-gestational-age (AGA), despite having lower adiposity levels [27]. Interestingly, when we compared life-course trajectories of blood pressure and other cardiovascular risk factors in women with a first normotensive preterm pregnancy vs. term, there was no strong evidence that trajectories differed. This may be because normotensive pre-term delivery is a heterogeneous phenotype. Given that the placenta is a crucial organ of human pregnancy and its complications, it may reveal additional clues regarding the links between preterm delivery (and other placental syndromes) and maternal risk of hypertension and CVD, as discussed in the next section.
Placental pathology, clinical placental syndromes, and blood pressure
A common finding in preeclampsia is the failure of the maternal decidua to adapt to adequately perfuse the placenta to support fetal growth and development [7]. This decidual vasculopathy includes insufficient remodelling of the uterine spiral arteries into highly dilated conduits feeding the placenta and related spiral artery pathologies. Decidual vasculopathy and concomitant hypoxia/reperfusion lesions in the placenta are collectively termed maternal vascular malperfusion (MVM) [7]. MVM is most classically and consistently detected in early-onset preeclampsia, early-onset fetal growth restriction, and in preeclamptic pregnancies delivered preterm or with accompanying fetal growth restriction [7, 28], suggesting that sub-types of clinical placental syndromes (e.g., early versus late onset preeclampsia) may be affected by different forms of placental impairment. MVM lesions are also present in up to a third of spontaneous preterm births [6], and retroplacental haemorrhage, the placental evidence of abruption, is also a diagnostic feature of MVM [29].
The causes of MVM are not known and are likely to be numerous; immunological and inflammatory components have been proposed, particularly in relation to acute atherosis [30, 31]. Another possible cause is pre-existing maternal predisposition to microvascular dysfunction, which is unmasked by the cardiometabolic stress test of pregnancy and apparent in the placenta. Regardless of its causes, MVM can result in both a poorly perfused placenta and circulating endothelial microparticles which themselves induce or exacerbate systemic vessel injury, perhaps via oxidative stress damage [32,33,34]. Thus, this initial damage may extend both spatially outside the placenta, and temporally outside of the pregnancy event. For example, MVM is a risk factor for preeclampsia in subsequent pregnancies, even in women without prior preeclampsia [35]. Abnormalities of the maternal microvasculature in other beds have also been described in women with preeclampsia with or without MVM, including capillary rarefaction in the fingernail [36] and skin [37,38,39], reduced venular diameters in conjunctiva [36], increased microvascular reactivity in skin blood flow, and abnormal endothelial glycocalyx of sublingual micro-vessels [35, 39,40,41,42]. There is also evidence that there are changes in the microvascular structure of the retina assessed via optical coherence tomography angiography (OCTA) during pregnancies complicated by preeclampsia compared to normal pregnancy and the non-pregnant state [43].
We have reported that women with MVM in the placenta have higher DBP (2.56 mmHg; 95%CI: 0.39, 4.74) but not SBP ten years after delivery compared to women with no evidence of vascular pathology in the placenta [44]. These findings were independent of pregnancy outcomes and maternal BMI. Of note, both SBP and DBP were higher 10 years post-delivery as the severity of the placental MVM worsened. In addition, MVM-affected women compared to those with a healthy placental vasculature had evidence of microvascular rarefaction and a more atherogenic lipid profile [44]. It also appears that only the subset of women with idiopathic preterm birth and MVM lesions have an excess risk for higher blood pressure and atherogenic lipids after delivery, both of which contribute to subclinical atherosclerosis after delivery [44, 45].
Consistent with these data, there is evidence that seven months after delivery, women with preeclampsia with accompanying decidual vasculopathy (the most severe, chronic, and likely underlying precursor lesion to other MVM features) had higher DBP, lower left ventricular stroke volume, and higher total peripheral vascular resistance compared with women with preeclampsia but no decidual vasculopathy [46]. A large, prospective, community-based U.S. cohort has also reported that mural hyperplasia, a feature of decidual vasculopathy characterized by thickening of the smooth muscle wall of the spiral arteries, is associated with risk of hypertension a decade after delivery when accompanied by modest BP elevations in pregnancy [47].
While even modest pre-pregnancy blood pressure elevations are associated with excess risk of placental syndromes during pregnancy, as shown above, there are sparse data directly examining the association of pre-pregnancy blood pressure and MVM occurrence. We have reported that the expected drop in DBP from pre-conception to early pregnancy (10 weeks, on average) was blunted in women who delivered placentas with evidence of MVM (−1.35 vs. −5.66 mmHg in women with no MVM). These data further support the possibility that subtle pre-existing vascular dysfunction may contribute to failed placental vascularization detected in placenta syndromes that is a marker for excess hypertension risk later in life.
Preventative treatment following a placental syndrome
Studies assessing prevention and treatment options for placental syndromes during pregnancy understandably focus on short terms maternal and fetal outcomes and have recently been comprehensively reviewed by Magee et al. [48], with post-partum interventions and management strategies to mitigate CVD in women who experienced a placental syndrome also recently reviewed by Jowell et al. [49].
The SNAP-HT trial evaluated the feasibility of self-management of postpartum hypertension with automated medication reduction via telemonitoring in women requiring antihypertensive medication in the puerperium. Investigators reported improved blood pressure control and that DBP remained lower at six months post-partum in the intervention group compared to the control group (−5.4 mmHg; 95%CI: −8.1, −0.8). The difference in SBP between the two arms was more modest (−1.0 mmHg; −6.3, 4.4) [50, 51]. Results of the subsequent main trial (POP-HT) that is powered to detect differences in 24-hour average ambulatory diastolic blood pressure at 6–9 months post-partum, with secondary outcomes including multimodal cardiovascular assessments (CMR and echocardiography), parameters derived from multiorgan MRI including brain and kidneys, and peripheral macrovascular and microvascular measures are expected to be published in the near future [52].
Summary
Hypertension and higher blood pressure prior to pregnancy are associated with increased risk of clinical placental syndromes and MVM, and those in turn, are associated with an increased risk of progression to hypertension and CVD in later life. Women with both clinical placental syndrome and evidence of placental MVM have a particularly high risk of hypertension and CVD. Both SBP and DBP are higher prior to pregnancy in women who go on to develop a placental syndrome and MVM, supporting the hypothesis that placental lesions and clinical syndromes are indicative of a pre-existing propensity for hypertension and CVD. Limited evidence suggests that DBP (but not SBP) fails to normalise following a hypertensive pregnancy, that the early pregnancy drop in DBP (but not SBP) is blunted in women with MVM, and that DBP is more amenable than SBP to post-partum treatment. DBP—more so than SBP—reflects microvascular dysfunction in young women, it is therefore possible that the latter plays a role in the pathogenesis of placental syndromes. It is also possible that placental syndromes further damage women’s microvasculature, directly contributing to the increased risk of hypertension post-partum. Studies with detailed measures of cardiac and vascular structure and function, from before to after pregnancy are needed to solve the ‘chicken and egg’ puzzle of women’s blood pressure and pregnancy health. Postpartum Intervention trials among women with placental syndromes can also help disentangle this question, and consideration of DBP as a primary endpoint is warranted.
Change history
07 September 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41371-023-00860-8
References
Gabbe S. Obstetrics: Normal and problem pregnancies. Vol Sixth Edition. Philadelphia, PA: Elsevier/Saunders; 2012.
Clapp JF 3rd, Seaward BL, Sleamaker RH, Hiser J. Maternal physiologic adaptations to early human pregnancy. Am J Obstet Gynecol. 1988;159:1456–60.
Macdonald-Wallis C, Lawlor DA, Fraser A, May M, Nelson SM, Tilling K. Blood pressure change in normotensive, gestational hypertensive, preeclamptic, and essential hypertensive pregnancies. Hypertension 2012;59:1241–8.
Steer PJ, Little MP, Kold-Jensen T, Chapple J, Elliott P. Maternal blood pressure in pregnancy, birth weight, and perinatal mortality in first births: prospective study. BMJ 2004;329:1312.
Orbach H, Matok I, Gorodischer R, Sheiner E, Daniel S, Wiznitzer A, et al. Hypertension and antihypertensive drugs in pregnancy and perinatal outcomes. Am J Obstet Gynecol. 2013;208:301.e301–306.
Brosens I, Pijnenborg R, Vercruysse L, Romero R. The “Great Obstetrical Syndromes” are associated with disorders of deep placentation. Am J Obstet Gynecol. 2011;204:193–201.
Parks WT. Placental hypoxia: The lesions of maternal malperfusion. Semin Perinatol. 2015;39:9–19.
Lane-Cordova AD, Khan SS, Grobman WA, Greenland P, Shah SJ. Long-term cardiovascular risks associated with adverse pregnancy outcomes: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;73:2106–16.
Giorgione V, Ridder A, Kalafat E, Khalil A, Thilaganathan B. Incidence of postpartum hypertension within 2 years of a pregnancy complicated by pre-eclampsia: a systematic review and meta-analysis. BJOG: Int J Obstet Gynaecol. 2021;128:495–503.
Haug EB, Horn J, Markovitz AR, Fraser A, Macdonald-Wallis C, Tilling K, et al. The impact of parity on life course blood pressure trajectories: the HUNT study in Norway. Eur J Epidemiol. 2018;33:751–61.
Gunderson EP, Chiang V, Lewis CE, Catov J, Quesenberry CP, Sidney S, et al. Long-term blood pressure changes measured from before to after pregnancy relative to nonparous women. Obstet Gynecol. 2008;112:1294–302.
Clapp JF 3rd, Capeless E. Cardiovascular function before, during, and after the first and subsequent pregnancies. Am J Cardiol. 1997;80:1469–73.
Morris EA, Hale SA, Badger GJ, Magness RR, Bernstein IM. Pregnancy induces persistent changes in vascular compliance in primiparous women. Am J Obstet Gynecol. 2015;212:633.e631–636.
Teufel. The effect of bearing and rearing a child on blood pressure: A nationally representative instrumental variable analysis of 444 611 mothers in India. Int J Epidemiol. 2021;50:1671–83.
Rich-Edwards JW, Fraser A, Lawlor DA, Catov JM. Pregnancy characteristics and women’s future cardiovascular health: an underused opportunity to improve women’s health? Epidemiol Rev. 2014;36:57–70.
Grandi SM, Filion KB, Yoon S, Ayele HT, Doyle CM, Hutcheon JA, et al. Cardiovascular disease-related morbidity and mortality in women with a history of pregnancy complications. Circulation 2019;139:1069–79.
Stuart JJ, Tanz LJ, Rimm EB, Spiegelman D, Missmer SA, Mukamal KJ, et al. Cardiovascular risk factors mediate the long-term maternal risk associated with hypertensive disorders of pregnancy. J Am Coll Cardiol. 2022;79:1901–13.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315–81.
Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update. Circulation 2011;123:1243–62.
Brown HL, Warner JJ, Gianos E, Gulati M, Hill AJ, Hollier LM, et al. Promoting risk identification and reduction of cardiovascular disease in women through collaboration with obstetricians and gynecologists: a presidential advisory From the American Heart Association and the American College of Obstetricians and Gynecologists. Circulation 2018;137:e843–e852.
Haug EB, Horn J, Markovitz AR, Fraser A, Klykken B, Dalen H, et al. Association of conventional cardiovascular risk factors with cardiovascular disease after hypertensive disorders of pregnancy: analysis of the nord-trøndelag health study. JAMA Cardiol. 2019;4:628.
Leon LJ, McCarthy FP, Direk K, Gonzalez-Izquierdo A, Prieto-Merino D, Casas JP, et al. Preeclampsia and cardiovascular disease in a large UK Pregnancy Cohort of Linked Electronic Health Records. Circulation 2019;140:1050–60.
Honigberg MC, Zekavat SM, Aragam K, Klarin D, Bhatt DL, Scott NS, et al. Long-term cardiovascular risk in women with hypertension during pregnancy. J Am Coll Cardiol. 2019;74:2743–54.
Melchiorre K, Giorgione V, Thilaganathan B. The placenta and preeclampsia: villain or victim? Am J Obstet Gynecol. 2022;226:S954–s962.
Haug EB, Horn J, Markovitz AR, Fraser A, Vatten LJ, Macdonald-Wallis C, et al. Life course trajectories of cardiovascular risk factors in women with and without hypertensive disorders in first pregnancy: The HUNT study in Norway. J Am Heart Assoc. 2018;7:e009250.
Foo FL, Mahendru AA, Masini G, Fraser A, Cacciatore S, MacIntyre DA, et al. Association between prepregnancy cardiovascular function and subsequent preeclampsia or fetal growth restriction. Hypertension 2018;72:442–50.
Horn J, Haug EB, Markovitz AR, Fraser A, Vatten LJ, Romundstad PR, et al. Life course trajectories of maternal cardiovascular risk factors according to offspring birthweight: the HUNT Study. Sci Rep. 2020;10:10436.
Redman CW, Staff AC. Preeclampsia, biomarkers, syncytiotrophoblast stress, and placental capacity. Am J Obstet Gynecol. 2015;213:S9.e1. 4 SupplS9-11
Khong TY, Mooney EE, Ariel I, Balmus NCM, Boyd TK, Brundler MA, et al. Sampling and definitions of placental lesions: Amsterdam Placental Workshop Group Consensus Statement. Arch Pathol Lab Med. 2016;140:698–713.
Staff AC, Dechend R, Pijnenborg R. Learning from the placenta. Hypertension 2010;56:1026–34.
Staff AC, Johnsen GM, Dechend R, Redman CWG. Preeclampsia and uteroplacental acute atherosis: immune and inflammatory factors. J Reprod Immunol. 2014;101-102:120–6.
Das S, Halushka MK. Extracellular vesicle microRNA transfer in cardiovascular disease. Cardiovasc Pathol. 2015;24:199–206.
Gonzalez-Quintero VH, Smarkusky LP, Jimenez JJ, Mauro LM, Jy W, Hortsman LL, et al. Elevated plasma endothelial microparticles: Preeclampsia versus gestational hypertension. Am J Obstet Gynecol. 2004;191:1418–24.
Hecht JL, Zsengeller ZK, Spiel M, Karumanchi SA, Rosen S. Revisiting decidual vasculopathy. Placenta 2016;42:37–43.
Hauspurg A, Redman EK, Assibey-Mensah V, Tony Parks W, Jeyabalan A, Roberts JM, et al. Placental findings in non-hypertensive term pregnancies and association with future adverse pregnancy outcomes: a cohort study. Placenta 2018;74:14–19.
Houben AJ, de Leeuw PW, Peeters LL. Configuration of the microcirculation in pre-eclampsia: possible role of the venular system. J Hypertens. 2007;25:1665–70.
Cornette J, Herzog E, Dubekot JJ, Tibboel D, Buijs EA, Steegers EA. Microcirculation analysed by sidestream dark field imaging (SDF) technique in women with severe pre-eclampsia. Reprod Sci. 2011;18:197.
Hasan KM, Manyonda IT, Ng FS, Singer DR, Antonios TF. Skin capillary density changes in normal pregnancy and pre-eclampsia. J Hypertens. 2002;20:2439–43.
Gandley RE, Bregand-White J, Brands J, Tang G, Gorman L, James, et al. Sublingual microvascular density and glycocalyx barrier dynamics, during and after normal and preeclamptic pregnancy. Pregnancy Hypertens. 2018;13:S111.
Weissgerber TL, Garcia-Valencia O, Milic NM, Codsi E, Cubro H, Nath MC, et al. Early onset preeclampsia is associated with glycocalyx degradation and reduced microvascular perfusion. J Am Heart Assoc. 2019;8:e010647.
Brands J, Hauspurg A, Bregand-White J, Gorman L, Jeyabalan A, Roberts JM, et al. The microvascular endothelial glycocalyx: impaired barrier function in preeclampsia with small gestational age neonates. Pregnancy Hypertens. 2018;13:S99.
Brands J, Jeyabalan A, Hauspurg A, McGonigal SC, Gandley RE, Hubel CA. Reduced barrier function of the microvascular endothelial glycocalyx in women with a history of preeclampsia, one year after delivery. Pregnancy Hypertens. 2018;13:S99–S100.
Ciloglu E, Okcu NT, Dogan N. Optical coherence tomography angiography findings in preeclampsia. Eye. 2019;33:1946–51.
Catov JM, Muldoon MF, Gandley RE, Brands J, Hauspurg A, Hubel CA, et al. Maternal vascular lesions in the placenta predict vascular impairments a decade after delivery. Hypertension 2022;79:424–34.
Catov J, Muldoon M, Reis S, Ness R, Nguyen L, Yamal JM, et al. Preterm birth with placental evidence of malperfusion is associated with cardiovascular risk factors after pregnancy: a prospective cohort study. BJOG: Int J Obstet Gynaecol. 2018;125:1009–17.
Stevens DU, Al-Nasiry S, Fajta MM, Bulten J, van Dijk AP, van der Vlugt MJ, et al. Cardiovascular and thrombogenic risk of decidual vasculopathy in preeclampsia. Am J Obstet Gynecol. 2014;210:545.e541–545.e546.
Holzman CB, Senagore P, Xu J, Dunietz GL, Strutz KL, Tian Y, et al. Maternal risk of hypertension 7–15 years after pregnancy: clues from the placenta. Bjog 2020;128:827–36.
Magee LA, Nicolaides KH, von Dadelszen P. Preeclampsia. N. Engl J Med. 2022;386:1817–32.
Jowell AR, Sarma AA, Gulati M, Michos ED, Vaught AJ, Natarajan P, et al. Interventions to mitigate risk of cardiovascular disease after adverse pregnancy outcomes: a review. JAMA Cardiol. 2022;7:346–55.
Kitt JA, Fox RL, Cairns AE, Mollison J, Burchert HH, Kenworthy Y, et al. Short-term postpartum blood pressure self-management and long-term blood pressure control: a randomized controlled trial. Hypertension 2021;78:469–79.
Cairns AE, Tucker KL, Leeson P, Mackillop LH, Santos M, Velardo C, et al. Self-management of postnatal hypertension: The SNAP-HT trial. Hypertension 2018;72:425–32.
Kitt J, Frost A, Mollison J, Tucker KL, Suriano K, Kenworthy Y, et al. Postpartum blood pressure self-management following hypertensive pregnancy: protocol of the Physician Optimised Post-partum Hypertension Treatment (POP-HT) trial. BMJ Open. 2022;12:e051180.
Funding
This work was supported by the Medical Research Council [grant number MR/M009351/1].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In this article the ‘Funding’ statement was missing and should have been ‘This work was supported by the Medical Research Council [grant number MR/M009351/1]’.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fraser, A., Catov, J.M. Placental syndromes and long-term risk of hypertension. J Hum Hypertens 37, 671–674 (2023). https://doi.org/10.1038/s41371-023-00802-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-023-00802-4
This article is cited by
-
Postpartum and interpregnancy care of women with a history of hypertensive disorders of pregnancy
Hypertension Research (2024)
-
Journal of Human Hypertension special issue on sex and gender differences in hypertension
Journal of Human Hypertension (2023)