Abstract
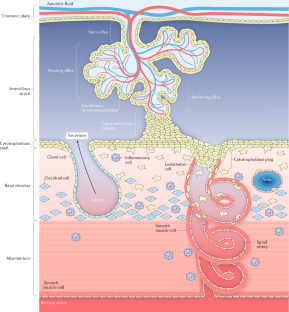
Pre-eclampsia and fetal growth restriction arise from disorders of placental development and have some shared mechanistic features. Initiation is often rooted in the maldevelopment of a maternal–placental blood supply capable of providing for the growth requirements of the fetus in later pregnancy, without exerting undue stress on maternal body systems. Here, we review normal development of a placental bed with a safe and adequate blood supply and a villous placenta–blood interface from which nutrients and oxygen can be extracted for the growing fetus. We consider disease mechanisms that are intrinsic to the maternal environment, the placenta or the interaction between the two. Systemic signalling from the endocrine placenta targets the maternal endothelium and multiple organs to adjust metabolism for an optimal pregnancy and later lactation. This signalling capacity is skewed when placental damage occurs and can deliver a dangerous pathogenic stimulus. We discuss the placental secretome including glycoproteins, microRNAs and extracellular vesicles as potential biomarkers of disease. Angiomodulatory mediators, currently the only effective biomarkers, are discussed alongside non-invasive imaging approaches to the prediction of disease risk. Identifying the signs of impending pathology early enough to intervene and ameliorate disease in later pregnancy remains a complex and challenging objective.
Key points
-
In the first trimester, uterine secretions support embryonic development; remodelling of the maternal vascular supply to the placental site enables increased volume supply of substrates at low pressure as fetal demand increases.
-
Placental growth and branching of the villous tree yield an increasing surface area for substrate transport, which is coordinated with the elaboration of a fetoplacental vascular network.
-
Fetal growth restriction arises when the supply of nutrients and oxygen to the fetus is insufficient because of maternal vascular malperfusion and/or inefficient extraction of substrates by the placenta.
-
Pre-eclampsia is caused by reaction of the placenta to stress, which triggers the release of factors that induce systemic vascular pathology or suppresses factors that stabilize vascular and immune interfaces.
-
An angiomodulatory imbalance is present in a large proportion of pregnancies with one or more of the clinical features of either pre-eclampsia or fetal growth restriction.
-
Data on many of the potential biomarkers of disease in pregnancy are conflicting, with reports of unchanged, lower or higher levels in the maternal circulation in complicated versus control pregnancies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Tobi, E. W. et al. Selective survival of embryos can explain DNA methylation signatures of adverse prenatal environments. Cell Rep. 25, 2660–2667.e4 (2018).
Constancia, M. et al. Adaptation of nutrient supply to fetal demand in the mouse involves interaction between the Igf2 gene and placental transporter systems. Proc. Natl Acad. Sci. USA 102, 19219–19224 (2005).
Lane-Cordova, A. D., Khan, S. S., Grobman, W. A., Greenland, P. & Shah, S. J. Long-term cardiovascular risks associated with adverse pregnancy outcomes: JACC review topic of the week. J. Am. Coll. Cardiol. 73, 2106–2116 (2019).
Kesavan, K. & Devaskar, S. U. Intrauterine growth restriction: postnatal monitoring and outcomes. Pediatr. Clin. North. Am. 66, 403–423 (2019).
Ruane, P. T. et al. Apposition to endometrial epithelial cells activates mouse blastocysts for implantation. Mol. Hum. Reprod. 23, 617–627 (2017).
Burton, G. J., Watson, A. L., Hempstock, J., Skepper, J. N. & Jauniaux, E. Uterine glands provide histiotrophic nutrition for the human fetus during the first trimester of pregnancy. J. Clin. Endocrinol. Metab. 87, 2954–2959 (2002).
Jones, C. J., Choudhury, R. H. & Aplin, J. D. Tracking nutrient transfer at the human maternofetal interface from 4 weeks to term. Placenta 36, 372–380 (2015).
Guo, H. et al. The DNA methylation landscape of human early embryos. Nature 511, 606–610 (2014).
Aplin, J. D. & Jones, C. J. in The Endometrium Ch. 29 (eds Aplin J. D., Fazleabas A. T., Glasser S. R., & Giudice L. C.) 441–453 (Informa Healthcare, 2008).
Aplin, J. D. & Ruane, P. T. Embryo-epithelium interactions during implantation at a glance. J. Cell Sci. 130, 15–22 (2017).
Aplin, J. D., Lewis, R. M. & Jones, C. J. in Reference Module in Biomedical Sciences https://doi.org/10.1016/B978-0-12-801238-3.99857-X (Elsevier, 2018).
Cheong, M. L. et al. A positive feedback loop between glial cells missing 1 and human chorionic gonadotropin (hCG) regulates placental hCGbeta expression and cell differentiation. Mol. Cell Biol. 36, 197–209 (2016).
Gerbaud, P. et al. Mesenchymal activin-A overcomes defective human trisomy 21 trophoblast fusion. Endocrinology 152, 5017–5028 (2011).
Jones, C. J., Harris, L. K., Whittingham, J., Aplin, J. D. & Mayhew, T. M. A re-appraisal of the morphophenotype and basal lamina coverage of cytotrophoblasts in human term placenta. Placenta 29, 215–219 (2008).
Kar, M., Ghosh, D. & Sengupta, J. Histochemical and morphological examination of proliferation and apoptosis in human first trimester villous trophoblast. Hum. Reprod. 22, 2814–2823 (2007).
Mayhew, T. M. Recent applications of the new stereology have thrown fresh light on how the human placenta grows and develops its form. J. Microsc. 186, 153–163 (1997).
Mayhew, T. M. Villous trophoblast of human placenta: a coherent view of its turnover, repair and contributions to villous development and maturation. Histol. Histopathol. 16, 1213–1224 (2001).
Lu, X. et al. Fine-tuned and cell-cycle-restricted expression of fusogenic protein syncytin-2 maintains functional placental syncytia. Cell Rep. 21, 1150–1159 (2017).
Lin, C., Lin, M. & Chen, H. Biochemical characterization of the human placental transcription factor GCMa/1. Biochem. Cell Biol. 83, 188–195 (2005).
Liang, C. Y. et al. GCM1 regulation of the expression of syncytin 2 and its cognate receptor MFSD2A in human placenta. Biol. Reprod. 83, 387–395 (2010).
Karolczak-Bayatti, M. et al. IGF signalling and endocytosis in the human villous placenta in early pregnancy as revealed by comparing quantum dot conjugates with a soluble ligand. Nanoscale 11, 12285–12295 (2019).
Sibley, C. P., Brownbill, P., Glazier, J. D. & Greenwood, S. L. Knowledge needed about the exchange physiology of the placenta. Placenta 64, S9–S15 (2018).
Aplin, J. D., Haigh, T., Jones, C. J., Church, H. J. & Vicovac, L. Development of cytotrophoblast columns from explanted first-trimester human placental villi: role of fibronectin and integrin alpha5beta1. Biol. Reprod. 60, 828–838 (1999).
Aplin, J. D., Haigh, T., Vicovac, L., Church, H. J. & Jones, C. J. Anchorage in the developing placenta: an overlooked determinant of pregnancy outcome? Hum. Fertil. 1, 75–79 (1998).
Vento-Tormo, R. et al. Single-cell reconstruction of the early maternal-fetal interface in humans. Nature 563, 347–353 (2018).
Velicky, P. et al. Genome amplification and cellular senescence are hallmarks of human placenta development. PLoS Genet. 14, e1007698 (2018).
al-Lamki, R. S., Skepper, J. N. & Burton, G. J. Are human placental bed giant cells merely aggregates of small mononuclear trophoblast cells? An ultrastructural and immunocytochemical study. Hum. Reprod. 14, 496–504 (1999).
Aplin, J. D. in Encyclopedia of Reproduction 2nd edn. Vol. 2 (ed. Skinner M. K.) 326–332 (Elsevier, 2018).
Kajihara, T. et al. Differential expression of FOXO1 and FOXO3a confers resistance to oxidative cell death upon endometrial decidualization. Mol. Endocrinol. 20, 2444–2455 (2006).
Yoshino, O. et al. Endometrial stromal cells undergoing decidualization down-regulate their properties to produce proinflammatory cytokines in response to interleukin-1 beta via reduced p38 mitogen-activated protein kinase phosphorylation. J. Clin. Endocrinol. Metab. 88, 2236–2241 (2003).
Leitao, B. et al. Silencing of the JNK pathway maintains progesterone receptor activity in decidualizing human endometrial stromal cells exposed to oxidative stress signals. FASEB J. 24, 1541–1551 (2010).
Berkhout, R. P. et al. High-quality human preimplantation embryos actively influence endometrial stromal cell migration. J. Assist. Reprod. Genet. 35, 659–667 (2018).
Weimar, C. H. et al. Endometrial stromal cells of women with recurrent miscarriage fail to discriminate between high- and low-quality human embryos. PLoS ONE 7, e41424 (2012).
Tapia-Pizarro, A., Argandona, F., Palomino, W. A. & Devoto, L. Human chorionic gonadotropin (hCG) modulation of TIMP1 secretion by human endometrial stromal cells facilitates extravillous trophoblast invasion in vitro. Hum. Reprod. 28, 2215–2227 (2013).
Meinhardt, G. et al. Wingless ligand 5a is a critical regulator of placental growth and survival. Sci. Rep. 6, 28127 (2016).
Murakami, K. et al. Deficiency in clonogenic endometrial mesenchymal stem cells in obese women with reproductive failure — a pilot study. PLoS ONE 8, e82582 (2013).
Masuda, H., Anwar, S. S., Buhring, H. J., Rao, J. R. & Gargett, C. E. A novel marker of human endometrial mesenchymal stem-like cells. Cell Transpl. 21, 2201–2214 (2012).
Barragan, F. et al. Human endometrial fibroblasts derived from mesenchymal progenitors inherit progesterone resistance and acquire an inflammatory phenotype in the endometrial niche in endometriosis. Biol. Reprod. 94, 118 (2016).
Garrido-Gomez, T. et al. Defective decidualization during and after severe preeclampsia reveals a possible maternal contribution to the etiology. Proc. Natl Acad. Sci. USA 114, E8468–E8477 (2017).
Lucas, E. S. et al. Loss of endometrial plasticity in recurrent pregnancy loss. Stem Cells 34, 346–356 (2016).
Brighton, P. J. et al. Clearance of senescent decidual cells by uterine natural killer cells in cycling human endometrium. eLife 6, e31274 (2017).
Brosens, J. J. et al. Uterine selection of human embryos at implantation. Sci. Rep. 4, 3894 (2014).
Teklenburg, G. et al. Natural selection of human embryos: decidualizing endometrial stromal cells serve as sensors of embryo quality upon implantation. PLoS ONE 5, e10258 (2010).
Nadkarni, S. et al. Neutrophils induce proangiogenic T cells with a regulatory phenotype in pregnancy. Proc. Natl Acad. Sci. USA 113, E8415–E8424 (2016).
Amsalem, H. et al. Identification of a novel neutrophil population: proangiogenic granulocytes in second-trimester human decidua. J. Immunol. 193, 3070–3079 (2014).
Robertson, S. A. et al. Therapeutic potential of regulatory T cells in preeclampsia — opportunities and challenges. Front. Immunol. 10, 478 (2019).
Kelleher, A. M., DeMayo, F. J. & Spencer, T. E. Uterine glands: developmental biology and functional roles in pregnancy. Endocr. Rev. 40, 1424–1445 (2019).
Burton, G. J. & Jauniaux, E. The cytotrophoblastic shell and complications of pregnancy. Placenta 60, 134–139 (2017).
Moser, G., Weiss, G., Gauster, M., Sundl, M. & Huppertz, B. Evidence from the very beginning: endoglandular trophoblasts penetrate and replace uterine glands in situ and in vitro. Hum. Reprod. 30, 2747–2757 (2015).
Pijnenborg, R., Vercruysse, L. & Hanssens, M. The uterine spiral arteries in human pregnancy: facts and controversies. Placenta 27, 939–958 (2006).
Weiss, G., Sundl, M., Glasner, A., Huppertz, B. & Moser, G. The trophoblast plug during early pregnancy: a deeper insight. Histochem. Cell Biol. 146, 749–756 (2016).
Rodesch, F., Simon, P., Donner, C. & Jauniaux, E. Oxygen measurements in endometrial and trophoblastic tissues during early pregnancy. Obstet. Gynecol. 80, 283–285 (1992).
Burton, G. J., Jauniaux, E. & Murray, A. J. Oxygen and placental development; parallels and differences with tumour biology. Placenta 56, 14–18 (2017).
Foidart, J. M., Hustin, J., Dubois, M. & Schaaps, J. P. The human placenta becomes haemochorial at the 13th week of pregnancy. Int. J. Dev. Biol. 36, 451–453 (1992).
Okae, H. et al. Derivation of human trophoblast stem cells. Cell Stem Cell 22, 50–63.e6 (2018).
Haider, S. et al. Self-renewing trophoblast organoids recapitulate the developmental program of the early human placenta. Stem Cell Rep. 11, 537–551 (2018).
Turco, M. Y. et al. Trophoblast organoids as a model for maternal-fetal interactions during human placentation. Nature 564, 263–267 (2018).
Sheridan, M. A. et al. Early onset preeclampsia in a model for human placental trophoblast. Proc. Natl Acad. Sci. USA 116, 4336–4345 (2019).
Moser, G. et al. Extravillous trophoblasts invade more than uterine arteries: evidence for the invasion of uterine veins. Histochem. Cell Biol. 147, 353–366 (2017).
Rai, A. & Cross, J. C. Development of the hemochorial maternal vascular spaces in the placenta through endothelial and vasculogenic mimicry. Dev. Biol. 387, 131–141 (2014).
Pollheimer, J., Vondra, S., Baltayeva, J., Beristain, A. G. & Knofler, M. Regulation of placental extravillous trophoblasts by the maternal uterine environment. Front. Immunol. 9, 2597 (2018).
Paparini, D. E. et al. Vasoactive intestinal peptide shapes first-trimester placenta trophoblast, vascular, and immune cell cooperation. Br. J. Pharmacol. 176, 964–980 (2019).
Lacey, H., Haigh, T., Westwood, M. & Aplin, J. D. Mesenchymally-derived insulin-like growth factor 1 provides a paracrine stimulus for trophoblast migration. BMC Dev. Biol. 2, 5 (2002).
Smith, S. D., Dunk, C. E., Aplin, J. D., Harris, L. K. & Jones, R. L. Evidence for immune cell involvement in decidual spiral arteriole remodeling in early human pregnancy. Am. J. Pathol. 174, 1959–1971 (2009).
Choudhury, R. H. et al. Extravillous trophoblast and endothelial cell crosstalk mediates leukocyte infiltration to the early remodeling decidual spiral arteriole wall. J. Immunol. 198, 4115–4128 (2017).
Smith, S. D. et al. Changes in vascular extracellular matrix composition during decidual spiral arteriole remodeling in early human pregnancy. Histol. Histopathol. 31, 557–571 (2016).
Choudhury, R. H. et al. Decidual leucocytes infiltrating human spiral arterioles are rich source of matrix metalloproteinases and degrade extracellular matrix in vitro and in situ. Am. J. Reprod. Immunol. 81, e13054 (2019).
Harris, L. K. et al. Trophoblast- and vascular smooth muscle cell-derived MMP-12 mediates elastolysis during uterine spiral artery remodeling. Am. J. Pathol. 177, 2103–2115 (2010).
Harris, L. K. et al. Invasive trophoblasts stimulate vascular smooth muscle cell apoptosis by a fas ligand-dependent mechanism. Am. J. Pathol. 169, 1863–1874 (2006).
Keogh, R. J. et al. Fetal-derived trophoblast use the apoptotic cytokine tumor necrosis factor-alpha-related apoptosis-inducing ligand to induce smooth muscle cell death. Circ. Res. 100, 834–841 (2007).
Dickey, R. P. & Hower, J. F. Ultrasonographic features of uterine blood flow during the first 16 weeks of pregnancy. Hum. Reprod. 10, 2448–2452 (1995).
Roberts, V. H. J. et al. Early first trimester uteroplacental flow and the progressive disintegration of spiral artery plugs: new insights from contrast-enhanced ultrasound and tissue histopathology. Hum. Reprod. 32, 2382–2393 (2017).
Hempstock, J. et al. Intralobular differences in antioxidant enzyme expression and activity reflect the pattern of maternal arterial blood flow within the human placenta. Placenta 24, 517–523 (2003).
Jauniaux, E., Hempstock, J., Greenwold, N. & Burton, G. J. Trophoblastic oxidative stress in relation to temporal and regional differences in maternal placental blood flow in normal and abnormal early pregnancies. Am. J. Pathol. 162, 115–125 (2003).
Konje, J. C., Kaufmann, P., Bell, S. C. & Taylor, D. J. A longitudinal study of quantitative uterine blood flow with the use of color power angiography in appropriate for gestational age pregnancies. Am. J. Obstet. Gynecol. 185, 608–613 (2001).
Collins, S. L., Grant, D., Black, R. S., Vellayan, M. & Impey, L. Abdominal pregnancy: a perfusion confusion? Placenta 32, 793–795 (2011).
Burke, S. D. et al. Spiral arterial remodeling is not essential for normal blood pressure regulation in pregnant mice. Hypertension 55, 729–737 (2010).
Small, H. Y. et al. Abnormal uterine artery remodelling in the stroke prone spontaneously hypertensive rat. Placenta 37, 34–44 (2016).
Small, H. Y. et al. Role of tumor necrosis factor-alpha and natural killer cells in uterine artery function and pregnancy outcome in the stroke-prone spontaneously hypertensive rat. Hypertension 68, 1298–1307 (2016).
Care, A. S. et al. Reduction in regulatory T cells in early pregnancy causes uterine artery dysfunction in mice. Hypertension 72, 177–187 (2018).
Ellery, P. M., Cindrova-Davies, T., Jauniaux, E., Ferguson-Smith, A. C. & Burton, G. J. Evidence for transcriptional activity in the syncytiotrophoblast of the human placenta. Placenta 30, 329–334 (2009).
Chan, K. C. et al. Second generation noninvasive fetal genome analysis reveals de novo mutations, single-base parental inheritance, and preferred DNA ends. Proc. Natl Acad. Sci. USA 113, E8159–E8168 (2016).
Aplin, J. D. et al. Hemangioblastic foci in human first trimester placenta: distribution and gestational profile. Placenta 36, 1069–1077 (2015).
Burton, G. J. & Jauniaux, E. Development of the human placenta and fetal heart: synergic or independent? Front. Physiol. 9, 373 (2018).
Burton, G. J., Charnock-Jones, D. S. & Jauniaux, E. Regulation of vascular growth and function in the human placenta. Reproduction 138, 895–902 (2009).
Brosens, I., Pijnenborg, R., Vercruysse, L. & Romero, R. The “great obstetrical syndromes” are associated with disorders of deep placentation. Am. J. Obstet. Gynecol. 204, 193–201 (2011).
Burton, G. J. & Jauniaux, E. Pathophysiology of placental-derived fetal growth restriction. Am. J. Obstet. Gynecol. 218, S745–S761 (2018).
Brosens, J. J., Pijnenborg, R. & Brosens, I. A. The myometrial junctional zone spiral arteries in normal and abnormal pregnancies: a review of the literature. Am. J. Obstet. Gynecol. 187, 1416–1423 (2002).
Jauniaux, E., Collins, S. & Burton, G. J. Placenta accreta spectrum: pathophysiology and evidence-based anatomy for prenatal ultrasound imaging. Am. J. Obstet. Gynecol. 218, 75–87 (2018).
Verburg, P. E. et al. Peripheral maternal haemodynamics across pregnancy in hypertensive disorders of pregnancy. Pregnancy Hypertens. 16, 89–96 (2019).
Chaiworapongsa, T., Chaemsaithong, P., Yeo, L. & Romero, R. Pre-eclampsia part 1: current understanding of its pathophysiology. Nat. Rev. Nephrol. 10, 466–480 (2014).
Crovetto, F. et al. First-trimester screening for early and late small-for-gestational-age neonates using maternal serum biochemistry, blood pressure and uterine artery Doppler. Ultrasound Obstet. Gynecol. 43, 34–40 (2014).
Bartsch, E., Medcalf, K. E., Park, A. L., Ray, J. G. & High Risk of Pre-eclampsia Identification Group. Clinical risk factors for pre-eclampsia determined in early pregnancy: systematic review and meta-analysis of large cohort studies. BMJ 353, i1753 (2016).
Redline, R. W. & Patterson, P. Pre-eclampsia is associated with an excess of proliferative immature intermediate trophoblast. Hum. Pathol. 26, 594–600 (1995).
Oudejans, C. B. et al. Susceptibility allele-specific loss of miR-1324-mediated silencing of the INO80B chromatin-assembly complex gene in pre-eclampsia. Hum. Mol. Genet. 24, 118–127 (2015).
Visser, A., Beijer, M., Oudejans, C. B. M. & van Dijk, M. The effect of maternal NODAL on STOX1 expression in extravillous trophoblasts is mediated by IGF1. PLoS ONE 13, e0202190 (2018).
Rolfo, A. et al. Abnormalities in oxygen sensing define early and late onset preeclampsia as distinct pathologies. PLoS ONE 5, e13288 (2010).
Lv, S. et al. Impaired decidualization caused by downregulation of circadian clock gene BMAL1 contributes to human recurrent miscarriage. Biol. Reprod. 101, 138–147 (2019).
Dunk, C. et al. Failure of decidualization and maternal immune tolerance underlies uterovascular resistance in intra uterine growth restriction. Front. Endocrinol. 10, 160 (2019).
Zhou, Y. et al. Reversal of gene dysregulation in cultured cytotrophoblasts reveals possible causes of preeclampsia. J. Clin. Invest. 123, 2862–2872 (2013).
Moffett, A., Chazara, O., Colucci, F. & Johnson, M. H. Variation of maternal KIR and fetal HLA-C genes in reproductive failure: too early for clinical intervention. Reprod. Biomed. Online 33, 763–769 (2016).
Roth, C. J. et al. Dynamic modeling of uteroplacental blood flow in IUGR indicates vortices and elevated pressure in the intervillous space — a pilot study. Sci. Rep. 7, 40771 (2017).
Burton, G. J., Jauniaux, E. & Charnock-Jones, D. S. The influence of the intrauterine environment on human placental development. Int. J. Dev. Biol. 54, 303–312 (2010).
Burton, G. J., Yung, H. W. & Murray, A. J. Mitochondrial–endoplasmic reticulum interactions in the trophoblast: stress and senescence. Placenta 52, 146–155 (2017).
Sultana, Z., Maiti, K., Dedman, L. & Smith, R. Is there a role for placental senescence in the genesis of obstetric complications and fetal growth restriction? Am. J. Obstet. Gynecol. 218, S762–S773 (2018).
Hutchinson, E. S. et al. Utero-placental haemodynamics in the pathogenesis of pre-eclampsia. Placenta 30, 634–641 (2009).
Robinson, N. J., Baker, P. N., Jones, C. J. & Aplin, J. D. A role for tissue transglutaminase in stabilization of membrane-cytoskeletal particles shed from the human placenta. Biol. Reprod. 77, 648–657 (2007).
Kaya, B. et al. Proliferation of trophoblasts and Ki67 expression in preeclampsia. Arch. Gynecol. Obstet. 291, 1041–1046 (2015).
McGinnis, R. et al. Variants in the fetal genome near FLT1 are associated with risk of preeclampsia. Nat. Genet. 49, 1255–1260 (2017).
Roberts, J. M. & Escudero, C. The placenta in preeclampsia. Pregnancy Hypertens. 2, 72–83 (2012).
Redline, R. W. Placental pathology: a systematic approach with clinical correlations. Placenta 29, S86–91 (2008).
Leavey, K., Cox, B. J., Cargill, Y. & Grynspan, D. Recurrent placental transcriptional profile with a different histological and clinical presentation: a case report. Pediatr. Dev. Pathol. 22, 584–589 (2019).
Robertson, W. B., Brosens, I. & Dixon, G. Uteroplacental vascular pathology. Eur. J. Obstet. Gynecol. Reprod. Biol. 5, 47–65 (1975).
Kuzmina, I. Y., Hubina-Vakulik, G. I. & Burton, G. J. Placental morphometry and Doppler flow velocimetry in cases of chronic human fetal hypoxia. Eur. J. Obstet. Gynecol. Reprod. Biol. 120, 139–145 (2005).
Ong, S. S., Baker, P. N., Mayhew, T. M. & Dunn, W. R. Remodeling of myometrial radial arteries in preeclampsia. Am. J. Obstet. Gynecol. 192, 572–579 (2005).
Leavey, K. et al. Unsupervised placental gene expression profiling identifies clinically relevant subclasses of human preeclampsia. Hypertension 68, 137–147 (2016).
Kingdom, J. C., Audette, M. C., Hobson, S. R., Windrim, R. C. & Morgen, E. A placenta clinic approach to the diagnosis and management of fetal growth restriction. Am. J. Obstet. Gynecol. 218, S803–S817 (2018).
Gibbs, I. et al. Placental transcriptional and histologic subtypes of normotensive fetal growth restriction are comparable to preeclampsia. Am. J. Obstet. Gynecol. 220, 110.e1–110.e21 (2018).
Myers, J. E., Green, M. & Chappell, L. C. Why is the search for pre-eclampsia prevention so elusive? BMJ 362, k3536 (2018).
Rolnik, D. L. et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N. Engl. J. Med. 377, 613–622 (2017).
Sibley, C. P. Treating the dysfunctional placenta. J. Endocrinol. 234, R81–R97 (2017).
Winterhager, E. & Gellhaus, A. Transplacental nutrient transport mechanisms of intrauterine growth restriction in rodent models and humans. Front. Physiol. 8, 951 (2017).
Kingdom, J. C. & Kaufmann, P. Oxygen and placental villous development: origins of fetal hypoxia. Placenta 18, 613–621 (1997).
Junaid, T. O., Bradley, R. S., Lewis, R. M., Aplin, J. D. & Johnstone, E. D. Whole organ vascular casting and microCT examination of the human placental vascular tree reveals novel alterations associated with pregnancy disease. Sci. Rep. 7, 4144 (2017).
Chen, C. P., Bajoria, R. & Aplin, J. D. Decreased vascularization and cell proliferation in placentas of intrauterine growth-restricted fetuses with abnormal umbilical artery flow velocity waveforms. Am. J. Obstet. Gynecol. 187, 764–769 (2002).
Junaid, T. O., Brownbill, P., Chalmers, N., Johnstone, E. D. & Aplin, J. D. Fetoplacental vascular alterations associated with fetal growth restriction. Placenta 35, 808–815 (2014).
Hayward, C. E. et al. Placental adaptation: what can we learn from birthweight:placental weight ratio? Front. Physiol. 7, 28 (2016).
Glazier, J. D. et al. Association between the activity of the system A amino acid transporter in the microvillous plasma membrane of the human placenta and severity of fetal compromise in intrauterine growth restriction. Pediatr. Res. 42, 514–519 (1997).
Mayhew, T. M. Fetoplacental angiogenesis during gestation is biphasic, longitudinal and occurs by proliferation and remodelling of vascular endothelial cells. Placenta 23, 742–750 (2002).
Krebs, C. et al. Intrauterine growth restriction with absent end-diastolic flow velocity in the umbilical artery is associated with maldevelopment of the placental terminal villous tree. Am. J. Obstet. Gynecol. 175, 1534–1542 (1996).
Mills, T. A., Wareing, M., Bugg, G. J., Greenwood, S. L. & Baker, P. N. Chorionic plate artery function and Doppler indices in normal pregnancy and intrauterine growth restriction. Eur. J. Clin. Invest. 35, 758–764 (2005).
Lu, L., Kingdom, J., Burton, G. J. & Cindrova-Davies, T. Placental stem villus arterial remodeling associated with reduced hydrogen sulfide synthesis contributes to human fetal growth restriction. Am. J. Pathol. 187, 908–920 (2017).
Cindrova-Davies, T. et al. Reduced cystathionine gamma-lyase and increased miR-21 expression are associated with increased vascular resistance in growth-restricted pregnancies: hydrogen sulfide as a placental vasodilator. Am. J. Pathol. 182, 1448–1458 (2013).
Khalil, A. & Thilaganathan, B. Role of uteroplacental and fetal Doppler in identifying fetal growth restriction at term. Best Pract. Res. Clin. Obstet. Gynaecol. 38, 38–47 (2017).
Gordijn, S. J. et al. Consensus definition of fetal growth restriction: a Delphi procedure. Ultrasound Obstet. Gynecol. 48, 333–339 (2016).
Simcox, L. E., Myers, J. E., Cole, T. J. & Johnstone, E. D. Fractional fetal thigh volume in the prediction of normal and abnormal fetal growth during the third trimester of pregnancy. Am. J. Obstet. Gynecol. 217, 453 e451–453.e12 (2017).
Zhu, M. Y. et al. The hemodynamics of late-onset intrauterine growth restriction by MRI. Am. J. Obstet. Gynecol. 214, 367.e1–367.e17 (2016).
Ingram, E., Morris, D., Naish, J., Myers, J. & Johnstone, E. MR imaging measurements of altered placental oxygenation in pregnancies complicated by fetal growth restriction. Radiology 285, 953–960 (2017).
Nye, G. A. et al. Human placental oxygenation in late gestation: experimental and theoretical approaches. J. Physiol. 596, 5523–5534 (2018).
Zamudio, S. et al. Hypoglycemia and the origin of hypoxia-induced reduction in human fetal growth. PLoS ONE 5, e8551 (2010).
Monkley, S. J., Delaney, S. J., Pennisi, D. J., Christiansen, J. H. & Wainwright, B. J. Targeted disruption of the Wnt2 gene results in placentation defects. Development 122, 3343–3353 (1996).
Cureton, N. et al. Selective targeting of a novel vasodilator to the uterine vasculature to treat impaired uteroplacental perfusion in pregnancy. Theranostics 7, 3715–3731 (2017).
Redline, R. W. Classification of placental lesions. Am. J. Obstet. Gynecol. 213, S21–S28 (2015).
Metzger, R. J., Klein, O. D., Martin, G. R. & Krasnow, M. A. The branching programme of mouse lung development. Nature 453, 745–750 (2008).
Gaccioli, F., Aye, I., Sovio, U., Charnock-Jones, D. S. & Smith, G. C. S. Screening for fetal growth restriction using fetal biometry combined with maternal biomarkers. Am. J. Obstet. Gynecol. 218, S725–S737 (2018).
Ilekis, J. V. et al. Placental origins of adverse pregnancy outcomes: potential molecular targets: an executive workshop summary of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Am. J. Obstet. Gynecol. 215, S1–S46 (2016).
Sahraravand, M., Jarvela, I. Y., Laitinen, P., Tekay, A. H. & Ryynanen, M. The secretion of PAPP-A, ADAM12, and PP13 correlates with the size of the placenta for the first month of pregnancy. Placenta 32, 999–1003 (2011).
Morris, R. K. et al. Serum screening with Down’s syndrome markers to predict pre-eclampsia and small for gestational age: systematic review and meta-analysis. BMC Pregnancy Childbirth 8, 33 (2008).
Hui, D. et al. Combinations of maternal serum markers to predict preeclampsia, small for gestational age, and stillbirth: a systematic review. J. Obstet. Gynaecol. Can. 34, 142–153 (2012).
Townsend, R. et al. Prediction of pre-eclampsia: review of reviews. Ultrasound Obstet. Gynecol. 54, 16–27 (2018).
Wu, P. et al. Early pregnancy biomarkers in pre-eclampsia: a systematic review and meta-analysis. Int. J. Mol. Sci. 16, 23035–23056 (2015).
Giguere, Y. et al. Combining biochemical and ultrasonographic markers in predicting preeclampsia: a systematic review. Clin. Chem. 56, 361–375 (2010).
Zhu, X. L., Wang, J., Jiang, R. Z. & Teng, Y. C. Pulsatility index in combination with biomarkers or mean arterial pressure for the prediction of pre-eclampsia: systematic literature review and meta-analysis. Ann. Med. 47, 414–422 (2015).
Kuc, S. et al. Evaluation of 7 serum biomarkers and uterine artery Doppler ultrasound for first-trimester prediction of preeclampsia: a systematic review. Obstet. Gynecol. Surv. 66, 225–239 (2011).
Ray, J. G., Huang, T., Meschino, W. S., Cohen, E. & Park, A. L. Prenatal biochemical screening and long term risk of maternal cardiovascular disease: population based cohort study. BMJ 362, k2739 (2018).
Ormesher, L. et al. A clinical evaluation of placental growth factor in routine practice in high-risk women presenting with suspected pre-eclampsia and/or fetal growth restriction. Pregnancy Hypertens. 14, 234–239 (2018).
Birdir, C. et al. Predictive value of sFlt-1, PlGF, sFlt-1/PlGF ratio and PAPP-A for late-onset preeclampsia and IUGR between 32 and 37weeks of pregnancy. Pregnancy Hypertens. 12, 124–128 (2018).
Zhou, Y. et al. Vascular endothelial growth factor ligands and receptors that regulate human cytotrophoblast survival are dysregulated in severe preeclampsia and hemolysis, elevated liver enzymes, and low platelets syndrome. Am. J. Pathol. 160, 1405–1423 (2002).
Bushway, M. E. et al. Morphological and phenotypic analyses of the human placenta using whole mount immunofluorescence. Biol. Reprod. 90, 110 (2014).
De Falco, S. The discovery of placenta growth factor and its biological activity. Exp. Mol. Med. 44, 1–9 (2012).
Carmeliet, P. et al. Synergism between vascular endothelial growth factor and placental growth factor contributes to angiogenesis and plasma extravasation in pathological conditions. Nat. Med. 7, 575–583 (2001).
Luna, R. L. et al. Placental growth factor deficiency is associated with impaired cerebral vascular development in mice. Mol. Hum. Reprod. 22, 130–142 (2016).
Matsui, M. et al. Placental growth factor as a predictor of cardiovascular events in patients with CKD from the NARA-CKD Study. J. Am. Soc. Nephrol. 26, 2871–2881 (2015).
Dewerchin, M. & Carmeliet, P. Placental growth factor in cancer. Expert. Opin. Ther. Targets 18, 1339–1354 (2014).
Maynard, S. E. et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J. Clin. Invest. 111, 649–658 (2003).
Kendall, R. L., Wang, G. & Thomas, K. A. Identification of a natural soluble form of the vascular endothelial growth factor receptor, FLT-1, and its heterodimerization with KDR. Biochem. Biophys. Res. Commun. 226, 324–328 (1996).
Sela, S. et al. A novel human-specific soluble vascular endothelial growth factor receptor 1: cell-type-specific splicing and implications to vascular endothelial growth factor homeostasis and preeclampsia. Circ. Res. 102, 1566–1574 (2008).
Cebe-Suarez, S., Zehnder-Fjallman, A. & Ballmer-Hofer, K. The role of VEGF receptors in angiogenesis; complex partnerships. Cell Mol. Life Sci. 63, 601–615 (2006).
Rana, S. et al. Angiogenic factors and the risk of adverse outcomes in women with suspected preeclampsia. Circulation 125, 911–919 (2012).
Levine, R. J. et al. Circulating angiogenic factors and the risk of preeclampsia. N. Engl. J. Med. 350, 672–683 (2004).
Kumasawa, K. et al. Pravastatin induces placental growth factor (PGF) and ameliorates preeclampsia in a mouse model. Proc. Natl Acad. Sci. USA 108, 1451–1455 (2011).
Lu, F. et al. The effect of over-expression of sFlt-1 on blood pressure and the occurrence of other manifestations of preeclampsia in unrestrained conscious pregnant mice. Am. J. Obstet. Gynecol. 196, 396.e1–396.e7 (2007).
Sugimoto, H. et al. Neutralization of circulating vascular endothelial growth factor (VEGF) by anti-VEGF antibodies and soluble VEGF receptor 1 (sFlt-1) induces proteinuria. J. Biol. Chem. 278, 12605–12608 (2003).
Bergmann, A. et al. Reduction of circulating soluble Flt-1 alleviates preeclampsia-like symptoms in a mouse model. J. Cell Mol. Med. 14, 1857–1867 (2010).
Vogtmann, R. et al. Human sFLT1 leads to severe changes in placental differentiation and vascularization in a transgenic hsFLT1/rtTA FGR mouse model. Front. Endocrinol. 10, 165 (2019).
Gilbert, J. S. et al. Recombinant vascular endothelial growth factor 121 infusion lowers blood pressure and improves renal function in rats with placental ischemia-induced hypertension. Hypertension 55, 380–385 (2010).
Li, Z. et al. Recombinant vascular endothelial growth factor 121 attenuates hypertension and improves kidney damage in a rat model of preeclampsia. Hypertension 50, 686–692 (2007).
Thadhani, R. et al. Removal of soluble Fms-like tyrosine kinase-1 by dextran sulfate apheresis in preeclampsia. J. Am. Soc. Nephrol. 27, 903–913 (2016).
Thadhani, R. et al. Pilot study of extracorporeal removal of soluble fms-like tyrosine kinase 1 in preeclampsia. Circulation 124, 940–950 (2011).
Karumanchi, S. A. Angiogenic factors in preeclampsia: from diagnosis to therapy. Hypertension 67, 1072–1079 (2016).
Zeisler, H. et al. Predictive value of the sFlt-1:PlGF ratio in women with suspected preeclampsia. N. Engl. J. Med. 374, 13–22 (2016).
Chappell, L. C. et al. Diagnostic accuracy of placental growth factor in women with suspected preeclampsia: a prospective multicenter study. Circulation 128, 2121–2131 (2013).
National Institute for Health and Care Excellence. PlGF-based testing to help diagnose suspected pre-eclampsia (Triage PlGF test, Elecsys immunoassay sFlt-1/PlGF ratio, DELFIA Xpress PlGF 1-2-3 test, and BRAHMS sFlt-1 Kryptor/BRAHMS PlGF plus Kryptor PE ratio) (NICE, 2016).
Benton, S. J. et al. Can placental growth factor in maternal circulation identify fetuses with placental intrauterine growth restriction? Am. J. Obstet. Gynecol. 206, 163.e1–163.e7 (2012).
Hoeller, A. et al. Placental expression of sFlt-1 and PlGF in early preeclampsia vs. early IUGR vs. age-matched healthy pregnancies. Hypertens. Pregnancy 36, 151–160 (2017).
Ehrlich, L. et al. Increased placental sFlt-1 but unchanged PlGF expression in late-onset preeclampsia. Hypertens. Pregnancy 36, 175–185 (2017).
Powers, R. W. et al. Low placental growth factor across pregnancy identifies a subset of women with preterm preeclampsia: type 1 versus type 2 preeclampsia? Hypertension 60, 239–246 (2012).
Redman, C. W. & Staff, A. C. Preeclampsia, biomarkers, syncytiotrophoblast stress, and placental capacity. Am. J. Obstet. Gynecol. 213, S9.e1–S9.e4 (2015).
Griffin, M. et al. Predicting delivery of a small-for-gestational-age infant and adverse perinatal outcome in women with suspected pre-eclampsia. Ultrasound Obstet. Gynecol. 51, 387–395 (2018).
Rana, S. et al. Circulating angiogenic factors and risk of adverse maternal and perinatal outcomes in twin pregnancies with suspected preeclampsia. Hypertension 60, 451–458 (2012).
Palomaki, G. E. et al. Modeling risk for severe adverse outcomes using angiogenic factor measurements in women with suspected preterm preeclampsia. Prenat. Diagn. 35, 386–393 (2015).
Duhig, K. E. et al. Placental growth factor testing to assess women with suspected pre-eclampsia: a multicentre, pragmatic, stepped-wedge cluster-randomised controlled trial. Lancet 393, 1807–1818 (2019).
Colombo, M., Raposo, G. & Thery, C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu. Rev. Cell Dev. Biol. 30, 255–289 (2014).
Giacomini, E. et al. Secretome of in vitro cultured human embryos contains extracellular vesicles that are uptaken by the maternal side. Sci. Rep. 7, 5210 (2017).
Holder, B. et al. Macrophage exosomes induce placental inflammatory cytokines: a novel mode of maternal-placental messaging. Traffic 17, 168–178 (2016).
Gemmell, C. H., Sefton, M. V. & Yeo, E. L. Platelet-derived microparticle formation involves glycoprotein IIb-IIIa. Inhibition by RGDS and a Glanzmann’s thrombasthenia defect. J. Biol. Chem. 268, 14586–14589 (1993).
Endzelins, E. et al. Detection of circulating miRNAs: comparative analysis of extracellular vesicle-incorporated miRNAs and cell-free miRNAs in whole plasma of prostate cancer patients. BMC Cancer 17, 730 (2017).
Théry, C. et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles 8, 1535750 (2019).
Hromadnikova, I., Kotlabova, K., Ivankova, K. & Krofta, L. First trimester screening of circulating C19MC microRNAs and the evaluation of their potential to predict the onset of preeclampsia and IUGR. PLoS ONE 12, e0171756 (2017).
Ura, B. et al. Potential role of circulating microRNAs as early markers of preeclampsia. Taiwan. J. Obstet. Gynecol. 53, 232–234 (2014).
Salomon, C. et al. Placental exosomes as early biomarker of preeclampsia: potential role of exosomal microRNAs across gestation. J. Clin. Endocrinol. Metab. 102, 3182–3194 (2017).
Truong, G. et al. Oxygen tension regulates the miRNA profile and bioactivity of exosomes released from extravillous trophoblast cells — liquid biopsies for monitoring complications of pregnancy. PLoS ONE 12, e0174514 (2017).
Wu, L. et al. Circulating microRNAs are elevated in plasma from severe preeclamptic pregnancies. Reproduction 143, 389–397 (2012).
Qin, W., Tang, Y., Yang, N., Wei, X. & Wu, J. Potential role of circulating microRNAs as a biomarker for unexplained recurrent spontaneous abortion. Fertil. Steril. 105, 1247–1254.e3 (2016).
Pillay, P., Maharaj, N., Moodley, J. & Mackraj, I. Placental exosomes and pre-eclampsia: maternal circulating levels in normal pregnancies and, early and late onset pre-eclamptic pregnancies. Placenta 46, 18–25 (2016).
Miranda, J. et al. Placental exosomes profile in maternal and fetal circulation in intrauterine growth restriction — liquid biopsies to monitoring fetal growth. Placenta 64, 34–43 (2018).
Gonzalez-Quintero, V. H. et al. Elevated plasma endothelial microparticles: preeclampsia versus gestational hypertension. Am. J. Obstet. Gynecol. 191, 1418–1424 (2004).
Tong, M., Chen, Q., James, J. L., Stone, P. R. & Chamley, L. W. Micro- and nano-vesicles from first trimester human placentae carry Flt-1 and levels are increased in severe preeclampsia. Front. Endocrinol. 8, 174 (2017).
Li, H. et al. Differential proteomic analysis of syncytiotrophoblast extracellular vesicles from early-onset severe preeclampsia, using 8-Plex iTRAQ labeling coupled with 2D nano LC-MS/MS. Cell Physiol. Biochem. 36, 1116–1130 (2015).
Biro, O. et al. Various levels of circulating exosomal total-miRNA and miR-210 hypoxamiR in different forms of pregnancy hypertension. Pregnancy Hypertens. 10, 207–212 (2017).
Holder, B. S., Tower, C. L., Jones, C. J., Aplin, J. D. & Abrahams, V. M. Heightened pro-inflammatory effect of preeclamptic placental microvesicles on peripheral blood immune cells in humans. Biol. Reprod. 86, 103 (2012).
Tannetta, D., Collett, G., Vatish, M., Redman, C. & Sargent, I. Syncytiotrophoblast extracellular vesicles — circulating biopsies reflecting placental health. Placenta 52, 134–138 (2016).
Shomer, E. et al. Microvesicles of women with gestational hypertension and preeclampsia affect human trophoblast fate and endothelial function. Hypertension 62, 893–898 (2013).
Chen, Y., Huang, Y., Jiang, R. & Teng, Y. Syncytiotrophoblast-derived microparticle shedding in early-onset and late-onset severe pre-eclampsia. Int. J. Gynaecol. Obstet. 119, 234–238 (2012).
Tarca, A. L. et al. The prediction of early preeclampsia: results from a longitudinal proteomics study. PLoS ONE 14, e0217273 (2019).
King, A. et al. Tumor-homing peptides as tools for targeted delivery of payloads to the placenta. Sci. Adv. 2, e1600349 (2016).
Stephenson, J. et al. Before the beginning: nutrition and lifestyle in the preconception period and its importance for future health. Lancet 391, 1830–1841 (2018).
Qin, J., Liu, X., Sheng, X., Wang, H. & Gao, S. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Fertil. Steril. 105, 73–85.e856 (2016).
[No authors listed]. ACOG Practice Bulletin No. 202: gestational hypertension and preeclampsia. Obstet. Gynecol. 133, e1–e25 (2019).
National Institute for Health and Care Excellence. Hypertension in pregnancy: diagnosis and management (NICE, 2019).
Acknowledgements
We thank the co-workers in our own groups who have added to our understanding of this field. In summarizing placental development and the evidence for incomplete spiral artery remodelling in disease (especially) we regret being unable to fit in citations to the primary work of many researchers whose contributions were significant.
Author information
Authors and Affiliations
Contributions
J.D.A. made substantial contributions to discussion of content. J.D.A., J.E.M., K.T. and M.W. researched data for the article, wrote the article and carried out review/editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Endocrinology thanks B. Huppertz, S. Karumanchi and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related link
The Centre for Trophoblast Research: https://www.trophoblast.cam.ac.uk/Resources/enders
Supplementary information
Glossary
- Imprinting
-
Covalent epigenetic modifications to the genome that cause genes to be expressed in a parent-of-origin-specific pattern.
- Placental villi
-
Tree-like projections that form the placental exchange surface, and that are the basic functional unit of the placenta, comprising an outer syncytiotrophoblast layer, inner cytotrophoblast layer and a mesenchymal core.
- Decidualization
-
Transformation of endometrial stromal cells that occurs in early pregnancy
- Peri-implantation
-
The developmental time period between early attachment and gastrulation, or the secondary villous stage in the placenta; it approximates the second week of pregnancy.
- Chorionic plate
-
The disc-shaped, highly vascularized, fetal aspect of the placenta.
- Haemochorial
-
The maternal–fetal interface, where maternal blood passes directly over the outer layer of fetal cells in the placenta.
- Junctional zone
-
The tissue layer at the interface between the basal endometrium and the inner myometrium.
- Luteal–placental shift
-
The placenta takes over from the corpus luteum as the major source of oestrogens and progesterone at about 8–9 weeks of pregnancy.
Rights and permissions
About this article
Cite this article
Aplin, J.D., Myers, J.E., Timms, K. et al. Tracking placental development in health and disease. Nat Rev Endocrinol 16, 479–494 (2020). https://doi.org/10.1038/s41574-020-0372-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-020-0372-6
This article is cited by
-
The influence of placenta microbiota of normal term pregnant women on immune regulation during pregnancy
BMC Pregnancy and Childbirth (2024)
-
Single-nucleus multi-omic profiling of human placental syncytiotrophoblasts identifies cellular trajectories during pregnancy
Nature Genetics (2024)
-
Placental transfer and hazards of silver nanoparticles exposure during pregnancy: a review
Environmental Chemistry Letters (2024)
-
27-Hydroxycholesterol inhibits trophoblast fusion during placenta development by activating PI3K/AKT/mTOR signaling pathway
Archives of Toxicology (2024)
-
Proteomic studies of VEGFR2 in human placentas reveal protein associations with preeclampsia, diabetes, gravidity, and labor
Cell Communication and Signaling (2024)



