Abstract
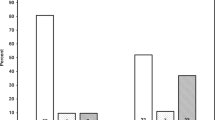
Failure to thrive (FTT) is an inadequate growth in young children. It can increase the risk of overweight or obesity later in life. Patients with renal tubulopathies can present FTT due to solute losses in the urine. We aimed to test our hypothesis that children with tubulopathies have an increased risk of overweight and obesity due to rebound following FTT that could complicate these conditions. We enrolled 26 patients with tubulopathies and evaluated for the first time within the first 12 months of life (mean age: 4.8 months ± 2.6 SDS). FTT was evident in 17 out of 26 patients (65.4%). The mean age at the last follow-up was 14.1 years ± 5.5 SDS. The mean age at overweight/obesity onset was 9.0 years ± 3.6 SDS. The prevalence of overweight/obesity was 73.1% (19/26). Among the patients with FTT, 15 (88.2%) developed overweight/obesity compared to 4 out of the 9 patients (44.4%) without FFT (p = 0.028). The presence of FTT determined an OR for obesity/overweight of 9.4 (95% CI: 1.3–67.6; p = 0.026). FTT continued to be significantly associated with obesity/overweight also after adjustment for preterm birth and birth weight <10th percentile (OR = 23.3; 95% CI: 1.95–279.4; p = 0.01). In conclusion, in our series, patients with tubulopathies presented an increased risk of overweight/obesity due to the FTT that can complicate these conditions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the presence of information that could compromise research participant privacy.
References
Kliegman RM, Stanton BMD, Geme J St., Schor NF, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia: Elsevier Inc; 2016.
Kim GJ, Furman LM. Obesity outcomes in children with a history of failure to thrive. Clin Pediatr. 2014;53:603–4.
Vijay Kiran B, Barman H, Iyengar A. Clinical profile and outcome of renal tubular disorders in children: a single center experience. Indian J Nephrol. 2014;24:362–6.
Mrad FCC, Soares SBM, de Menezes Silva LAW, dos Anjos Menezes PV, Simões-e-Silva AC. Bartter’s syndrome: clinical findings, genetic causes and therapeutic approach. World J Pediatr. 2021;17:31–9.
Alexander RT, Law L, Gil-Peña H, Greenbaum LA, Santos F. Hereditary distal renal tubular acidosis. In: Adam MP, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, editors. GeneReviews®. Seattle: University of Washington; 2019. https://www.ncbi.nlm.nih.gov/books/NBK547595/.
Leung T, Babbitt C, O’Brien K. Severe hypernatremia and failure to thrive. Clin Pediatr. 2016;55:1085–7.
La Scola C, Guarino S, Pasini A, Capalbo D, Liguori L, Di Sessa A, et al. Effect of body mass index on estimated glomerular filtration rate levels in children with congenital solitary kidney: a cross-sectional multicenter study. J Ren Nutr. 2020;30:261–7.
Indagine nazionale 2019: i dati nazionali. 2019. https://www.epicentro.iss.it/okkioallasalute/indagine-2019-dati.
Thoene JG. Cystinosis. J Inherit Metab Dis. 1995;18:380–6.
Becue C, Ceuleers B, den Brinker M, Somers I, Ledeganck KJ, Dotremont H, et al. Screening for an underlying tubulopathy in children with growth failure, simply maths? Front Pediatr. 2022;10:902252.
Kleta R, Bockenhauer D. Salt-losing tubulopathies in children: what’s new, what’s controversial? J Am Soc Nephrol. 2018;29:727.
Elmonem MA, Veys KR, Soliman NA, Van Dyck M, Van Den Heuvel LP, Levtchenko E. Cystinosis: a review. Orphanet J Rare Dis. 2016;11:47.
Blanchard A, Curis E, Guyon-Roger T, Kahila D, Treard C, Baudouin V, et al. Observations of a large Dent disease cohort. Kidney Int. 2016;90:430–9.
Al-Awqati Q. Basic research: salt wasting in distal renal tubular acidosis-new look, old problem. Nat Rev Nephrol. 2013;9:712–3.
Seyberth HW, Schlingmann KP. Bartter- and Gitelman-like syndromes: salt-losing tubulopathies with loop or DCT defects. Pediatr Nephrol. 2011;26:1789–802.
Liu C, Wu B, Lin N, Fang X. Insulin resistance and its association with catch-up growth in Chinese children born small for gestational age. Obesity. 2017;25:172–7.
Luther JM. Effects of aldosterone on insulin sensitivity and secretion. Steroids. 2014;91:54–60.
Hales CN, Barker DJP. The thrifty phenotype hypothesis. Br Med Bull. 2001;60:5–20.
Lopez-Garcia SC, Downie ML, Kim JS, Boyer O, Walsh SB, Nijenhuis T, et al. Treatment and long-term outcome in primary nephrogenic diabetes insipidus. Nephrol Dial Transplant. 2020;gfaa243. https://doi.org/10.1093/ndt/gfaa243.
Author information
Authors and Affiliations
Contributions
Conceptualization: CLS, PM; methodology: ADS, GR; software: CB, AP; validation: SG, PM; formal analysis: ADS, PM; investigation: AP, SG, CLS; data curation: PM, CLS; writing—original draft preparation: ADS, PM; writing—review and editing: CLS, PM, GR; supervision: PM. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This was a retrospective study; however, each patient or their parents signed a generic consent to use anonymous data deriving from their clinical charts.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
La Scola, C., Rivetti, G., Bertulli, C. et al. Failure to thrive in children with tubulopathies increases the risk of overweight later in life. Int J Obes 48, 127–129 (2024). https://doi.org/10.1038/s41366-023-01386-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01386-2