Abstract
Background
Infants born very preterm (≤32 weeks gestational age, GA) and very-low birth weight (≤1500 g; PT-VLBW) demonstrate high systolic blood pressure (SBP), renal dysfunction, and obesity at 6 months–3 years and in early adulthood. Their parallel measurement and progression during childhood is unclear.
Methods
We reenrolled 62/120 patients originally seen at 1–3 years at 10–13 years and remeasured anthropometric indices, SBP, and serum creatinine (Cr) and cystatin C (cysC) to determine estimated glomerular filtration rate (eGFR). We selected Term-matched Controls at 10–13 years from the 2015–2016 NHANES database at a ratio of 2 Controls:1 Case (124:62).
Results
Reenrolled patients were predominantly Hispanic, birth weight 1073 ± 251 g, and GA at birth 28 ± 2 weeks. At 10–13 years, 45% were classified overweight/obese, 48% had SBP ≥ 90th centile (77% considered hypertensive), and 34% had low eGFR (<90 mL min−1 [1.73 m2]−1). Notably, 57% of reenrolled PT-VLBW Cases had low eGFRcysC at both 1–3 and 10–13 years, P < 0.03. Compared to Controls, Cases had four times the adjusted odds for having an elevated SBP and low eGFRCr despite similar proportions with overweight/obesity among Cases and Controls.
Conclusions
PT-VLBW infants seen at 1–3 years exhibit obesity, elevated SBP, and low eGFR in infancy and 10–13 years. Although the small sample size may limit conclusions, pediatricians should consider serial evaluations of PT-VLBW throughout childhood.
Impact
-
The association between preterm birth and elevated blood pressure, renal dysfunction, and obesity in young adults begins as early as 1 year and persists at 10–13 years of age.
-
This is the first study reporting serial measurements of blood pressure, renal function, and obesity from infancy to preadolescence in children born very preterm.
-
Fifty-seven percent of preterm 1–3 year olds have persistent low estimated glomerular filtration rate associated with hypertension at 10–13 years.
-
Clinicians should consider serial evaluations of blood pressure, renal function, and obesity throughout infancy and childhood in all preterm births.
Similar content being viewed by others
Introduction
Infants born low birth weight at term gestation are at increased risk for “adult onset” adiposity, hypertension, and renal dysfunction.1,2 This may be due to intrauterine stresses associated with nutrient deficiency that modify developmental programming and contribute to the occurrence of chronic disease states in adulthood.3,4,5 Preterm birth also has been associated with the occurrence of obesity, hypertension, and renal disease in young adults6,7,8,9,10,11,12 and the incidence of each increases with decreasing gestational age (GA) at birth.13,14,15,16,17 Duncan et al.18 reported that infants born very preterm (≤32 weeks GA) and very low birth weight (≤1500 g; PT-VLBW) had elevated weight-for-length ratios and systolic blood pressure (SBP) as early as 6 months to 1 year corrected age. Frankfurt et al.19 observed that the disproportionate growth and elevated SBP in this population were associated with evidence of renal dysfunction; however, the relationships between obesity, elevated SBP, and renal dysfunction were unclear. Notably, excessive weight gain and the velocity of weight gain in preterm and term infants in the first 3 years of life is also associated with later elevations in SBP.13,20,21,22,23 While it is clear that preterm birth is associated with subsequent obesity and hypertension in young adults, the time course in childhood remains unclear and requires further study.
Low birth weight in term infants and intrauterine growth restriction in term fetal sheep are also associated with decreased nephrogenesis and subsequent hyperfiltration, glomerulosclerosis, and chronic renal disease with hypertension.23,24,25,26 Similar observations have been reported in adolescents and young adults born preterm.27,28,29,30 Birth <35 weeks GA is associated with incomplete nephrogenesis, and it has been suggested that this also results in subsequent hyperfiltration, glomerulosclerosis, and chronic renal disease with hypertension.31,32 This is supported by autopsy data that revealed morphologically abnormal glomeruli in preterm neonates.33 Frankfurt et al.19 reported loss of renal autoregulation and increased perfusion in 1-year-old PT-VLBW infants and low estimated glomerular filtration rates (eGFR) in a cohort of 3 year olds born PT-VLBW. Thus, birth <32 weeks GA is associated with incomplete nephrogenesis, increased risk for hyperfiltration in infancy and renal dysfunction, and elevations in SBP later in childhood. However, there are no serial measurements examining renal function and blood pressure from infancy to preadolescence in PT-VLBW.
In the present study, PT-VLBW infants originally seen at 1, 2, or 3 years of age and consented for follow-up were reenrolled 10 years later in order to determine (1) whether the obesity, high SBP, and renal dysfunction observed at 1–3 years of age persists at preadolescence18,19 and (2) whether the occurrence of obesity, high SBP, and renal dysfunction in the reenrolled PT-VLBW Cases differs from Term-matched Controls identified in the National Health and Nutrition Examination Survey (NHANES) dataset for 2015–2016.34
Methods
Study population and recruitment
PT-VLBW infants initially seen and recruited between May and September 2007 in a prospective cohort study and consented to subsequent follow-up were contacted in 2017 in order to conduct a 10-year follow-up.18,19 These PT-VLBW Cases were born at Parkland Memorial Hospital after January 1, 2004, had a GA ≤ 32 weeks, birth weight ≤1500 g, and received primary care in the Low Birth Weight Clinic at Children’s Medical Center, Dallas, TX at 1, 2, or 3 years corrected age. Race/ethnicity was verbally obtained at the initial recruitment and is self-reported. We excluded infants with congenital anomalies or discharged before 35 weeks postmenstrual age. We identified all of the PT-VLBW Cases (n = 120) in the electronic health records of Children’s Health and/or Parkland Health and Hospital System and successfully contacted 86 (72%) by telephone; 68 agreed to a clinic visit and 62 (52%) were seen, consented, and reenrolled at 10–13 years of age. A health survey was completed by V.B. for all enrolled patients to examine medications and health care.
Blood pressure measurements
We obtained standardized blood pressure measurements from consented PT-VLBW Cases during the clinic visit.35 After the patient rested at least 5 min while seated, upright and feet flat on the floor, two manual blood pressure measurements, 5 min apart, were obtained by one investigator (V.B.) from the right upper arm using an appropriately sized cuff and a 9002 digital ADC® e-sphygTM 2 sphygmomanometer (American Diagnostic Corp., Hauppauge, NY). The cuff had a bladder length 80–100% of arm circumference and width at least 40%. If the two sequential blood pressure measurements were within the range of error for the sphygmomanometer, ±3 mmHg, and <90th centile for age using the 2004 guidelines available at that time for the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents,36 we used the average value for subsequent analyses. If either SBP was ≥90th centile, we obtained a third measurement before concluding the visit and used the average of the two lowest measurements for analyses. Parents of children with multiple high blood pressure measurements received a letter from V.B. to give their primary care physician for follow-up assessment. The updated 2017 AAP Clinical Practice Guidelines for blood pressure diagnosis and management were subsequently used to reclassify and analyze SBP in PT-VLBW Cases at 1–3 years, 10–13 years of age, and in Term-matched Controls.37 Measurements of SBP were categorized as normal (<90th centile), elevated (90–95th centile), and hypertensive (>95th centile). None of the study patients was receiving an antihypertensive medication.
Anthropometric measurements
One investigator (V.B.) measured weight (g) and height (cm) twice, weight on a digital scale (accurate to the nearest 100 g) and length by stadiometer (accurate to the nearest millimeter). We used the average of the two measurements for each analysis. Body mass index (BMI) was calculated as weight (kg)/height (m)2 and classified using the sex-specific reference ranges from the Centers for Disease Control and Prevention.38 We categorized values as normal (<85th centile), overweight (85–95th centile), or obese (>95th centile).
Blood samples
We collected 3.0 mL of blood from all consented Cases, n = 62. Samples were allowed to clot, centrifuged at 10,000 rpm for 10 min, and serum divided into three aliquots that were stored at −80 °C until analysis. Serum creatinine (Cr) was measured using the modified Jaffe method and cystatin C (cysC) using the particle enhanced turbidimetric immunoassay. All samples (n = 62) were measured in a single assay at the Children’s Medical Center Dallas laboratory. We calculated eGFR using currently recommended equations by the National Kidney Foundation for children aged 10–13 years: the bedside Schwartz for creatinine (eGFRCr = 0.413 × L (cm)/Cr (mg/dL)) and the equation for cystatin C (eGFRcysC = 70.69 × [cystatin C (mg/L)]−0.931.39
Control population
Term-matched Controls were selected from the 2015–2016 NHANES dataset and matched two Controls for each PT-VLBW Case using age at reenrollment or date of birth if available, sex, and race/ethnicity.34 Since GA at birth was unavailable, we used birth weight >2000 g as a proxy for term birth. This cutoff allowed us to consider a larger control population that might have had a serum Cr measured and still exclude fetal growth restriction. Serum Cr measurements were only available in a subset of 12–13-year-old Controls; thus, we matched them with a corresponding age-matched subset of Cases in order to compare eGFRCr; serum Cr was not available in three of the 12–13-year-old matched Controls. A sample size of 124 Controls matched to 62 Cases achieved a 90% power to detect a 0.25 between-group difference in proportions with SBP ≥ 90th centile, assuming the proportion in the Cases with elevated SBP was 0.25 under the null hypothesis and 0.50 under the alternative hypothesis. We targeted a significance level of 0.05.
Height (cm) and weight (Kg) were measured using the NHANES mobile examination center protocol.34 In this cohort, blood pressure was measured using the American Heart Association guidelines: after resting 5 min, three measurements were manually obtained with a Baumanometer® in the right upper arm with an appropriately sized cuff.37 A fourth measurement was obtained if any of the first three were interrupted or incomplete. We used the average of the three SBP measurements for analyses.
Statistical analyses
Demographic characteristics, e.g., ethnicity, birth weight, and GA, were matched and compared in PT-VLBW Cases at 1, 2, and 3 years and at 10, 11, 12, and 13 years. We also compared demographics between PT-VLBW Cases and Term-matched Controls at 10–13 years. We analyzed categorical variables (e.g., race, obesity) by χ2 analysis and continuous variables (e.g., birth weight, GA, eGFR) by t test or Mann–Whitney U-test dependent on data distribution. The alpha level was 0.05 for all statistical tests. We used linear regression analysis to determine correlations between continuous variables, e.g., GA and eGFR at 12–13 years. Analysis of variance (ANOVA) for multiple groups followed by the correct post hoc test and pair-wise analysis, e.g., Bonferroni correction, were used to compare multiple groups. Data are means ± SD or medians with 25th and 75th centiles unless noted otherwise. We also performed exploratory analyses using multivariate logistic regression to determine which clinical variables are associated with development of an elevated SBP at 10–13 years in the Cases and Controls compared to a normotensive group in the Cases and Controls. Data are the adjusted odds ratio (aOR) of each variable in the model with the 95th confidence limits.
The study was approved by the Institutional Review Boards of the University of Texas Southwestern Medical Center, Children’s Medical Center Dallas, and Parkland Health and Hospital Systems. Informed consent was obtained from parents or guardians of study patients at the clinic visit by V.B. and assent was obtained from all study patients >10 years. PT-VLBW Cases were also consented for later follow-up.
Results
Description of PT-VLBW cases
Sixty two (52%) of 120 patients originally studied at 1, 2, or 3 years were reenrolled at 10–13 years of age. They were evenly distributed between the three original cohorts (18/40, 21/40, and 23/40, respectively) and only differed from the overall original cohort due to fewer Black non-Hispanics (P < 0.03, Table 1). This difference also existed between reenrolled and nonenrolled Cases as well as 1 week lower GA at birth (P ≤ 0.03, Table 1). There is no significant difference between groups in exposure to maternal antenatal steroids (ANS) or postnatal therapeutic indomethacin. We also assessed the demographics of the reenrolled Cases as separate cohorts originally seen at 1, 2, and 3 year of age. The only significant differences are a lower GA (27 vs. 28.6 and 28.4 weeks) and birth weight (970 g vs. 1165 and 1106 g) in Cases originally in cohort 3 vs. cohorts 1 and 2, respectively (P < 0.05, ANOVA).
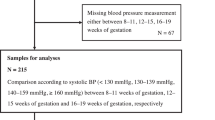
When the characteristics of the Cases reenrolled (n = 62) are examined as a single cohort at 10–13 years (Table 2), the average age at reenrollment is 11 years and 86% are Hispanic, reflecting the delivery population at Parkland Hospital. Notably, the mean weight Z-score at 10–13 years exceeds 0 while the height Z-score is <0; thus, 45% of Cases at 10–13 years exhibit disproportionate weight-for-length growth and are classified as overweight or obese with a BMI Z-score ≥85th centile.38 This is similar within all three cohorts (P > 0.1, ANOVA; data not shown). There is no difference in the velocity of weight gain from birth to 10–13 years between Cases from different cohorts (P > 0.1; data not shown); thus, these data are expressed as the mean value for all reenrolled Cases (Table 2). Although the mean SBP at 10–13 years is 115 ± 11 mmHg, classification of blood pressure measurements using the 2017 AAP Guidelines37 reveals that 48% (30/62) have a SBP ≥ 90th centile and 77% of these have a SBP > 95th centile and are considered hypertensive (Table 2). Four had Stage 2 hypertension. When we compare SBP classification at 1–3 years and 10–13 years using 2017 AAP Guidelines (Fig. 1), the number of Cases <90th centile decreases 36% between 1–3 and 10–13 years while the number ≥90th centile increases 2.5-fold. Notably, the Cases >95th centile increases from 6 to 23 (P = 0.07), while 17/50 Cases originally <90th centile have a SBP > 95th centile at 10–13 years (P = 0.9, χ2 analysis).
Values within bars are number of patients. Blood pressure is classified using the 2017 AAP Guidelines:37 Normal is <90th centile (white), elevated is 90th–95th centile (light gray), and hypertensive >95th centile (dark gray). P = 0.07 by Fisher exact test comparing patients >95th centile at 1–3 years and 10–13 years.
We measured serum Cr and cysC in each of the PT-VLBW Cases at 10–13 years and assessed renal function in the total cohort. The overall mean serum Cr concentration is 0.65 ± 0.16 mg/dL (n = 62; Table 2) and the overall mean eGFRCr is considered normal. However, classification of eGFRCr revealed that 34% are <90 mL min−1 [1.73 m2]−1 and considered low (Table 2). Since differences may exist between eGFRCr and eGFRcysC as well as between females and males, we examined both (Table 3). The analysis of paired values for eGFRCr and eGFRcysC show no significant difference in the overall mean eGFR, 96.2 ± 13 vs. 99.7 ± 21 mg/dL, respectively (P = 0.1, paired t test). There also are no differences in the mean eGFR or classification of eGFR between females and males using either estimate of GFR (P ≥ 0.5, Table 3). However, a third of all Cases at 10–13 years have an eGFRCr or eGFRcysC < 90 mL min−1 [1.73 m2]−1. Birth weight and GA are linearly related to both eGFRCr and eGFRcysC (Fig. 2), but the relationship is significantly greater for birth weight than GA (P < 0.01) and best defined by eGFRcysC (R = 0.30 and P = 0.02 vs. R = 0.49 and P < 0.01, respectively). The correlation between eGFR and GA is also best defined using eGFRcysC (eGFRcysC: R = 0.49 and P < 0.01 vs. eGFRCr: R = 0.11 and P = 0.4, respectively). When we examine the relationship between prenatal ANS exposure and the subsequent occurrence of an abnormal eGFR,40 there is no correlation with either eGFRCr or eGFRcysC at 10–13 years (P = 0.9). However, birth weight in Cases exposed to ANS remains highly correlated to subsequent eGFR at 10–13 years, P = 0.002.
Comparison of PT-VLBW Cases at 10–13 years and Term-matched Control
To determine whether there were differences in blood pressure and renal function between preterm and term births, we matched 10–13-year-old PT-VLBW Cases with Controls (62:124) selected from the 2015–2016 NHANES dataset.34 Clinical characteristics do not differ between groups except for birth weight (Table 2). Notably, the proportion with a BMI Z-score classified overweight or obese is similar in Cases and Controls, 45% and 48%, respectively, as is the mean velocity of weight gain from birth to preadolescence. There is, however, a higher overall SBP in PT-VLBW Cases (P < 0.01), who are sevenfold more likely to be classified as hypertensive with a SBP > 95th centile (P < 0.01). We also examined the relationship between SBP at 10–13 years with the velocity of weight gain from birth to 10–13 years in Cases and Controls (Fig. 3). While both demonstrate significant positive linear relationships (R = 0.74, P < 0.001 vs. R = 0.41, P < 0.001, respectively), the slopes and intercepts differ (P < 0.001) and Cases have a greater rise in SBP with increasing velocity of growth.
Relationships between systolic blood pressure (mmHg) at 10–13 years and the velocity of weight gain (g month−1) from birth to 10–13 years in PT-VLBW Cases (○; R = 0.74, n = 62, P < 0.001) and Term-matched Controls (●; R = 0.41, n = 124, P < 0.001). The slopes and intercepts are significantly different, P < 0.001.
We19 previously reported abnormalities of renal function at 1–3 years in PT-VLBW Cases; thus, we compared renal function in Cases (n = 62) with matched Controls at 12–13 years (n = 53) using serum Cr measurements to calculate eGFRCr (Table 2). Serum Cr is significantly higher in Cases vs. Controls and overall eGFRCr lower (P < 0.01). Moreover, Cases are fivefold more likely to have an eGFRCr < 90 mL min−1 [1.73 m2]−1, whereas Controls are ~3.5-fold more likely to have an eGFRCr > 140 mL min−1 [1.73 m2]−1 (P = 0.03, χ2 test). Since there may be sex-specific differences in renal function, we compared sex-related characteristics and eGFRCr in Cases and matched Controls (Table 4). There are no sex-related differences in race/ethnicity, weight, height, or distribution of BMI Z-score across groups. However, serum Cr is ~24% higher in male Cases vs. all Controls and male eGFRCr is four times more likely to be <90 mL min−1 [1.73 m2]−1 than either male or female Term-matched Controls (P < 0.01). No PT-VLBW Cases have an eGFRCr > 140 mL min−1 [1.73 m2]−1.
Prediction of SBP and eGFR at 10–13 years
We performed exploratory analyses using multivariate logistic regression to determine which clinical variables might be associated with development of an elevated SBP at 10–13 years. The clinical variables included in the SBP classification model are race/ethnicity, birth weight, overweight, obesity, eGFR classification (<90 and ≥140 mL min−1 [1.73 m2]−1), and Case (PT-VLBW) vs. Control (Term). Race/ethnicity, birth weight, eGFR classification, and Case vs. Control are not statistically significant in the SBP classification model. However, overweight and obesity are significant variables with an aOR 4.1 and 5.9, respectively (P ≤ 0.04). Notably, the aOR increases further when we use a SBP > 95th centile, 9.8 (P = 0.003) and 11.2 (P = 0.001), respectively. These observations are exploratory and require further investigation.
We performed a similar multivariate logistic regression to evaluate which clinical variables are associated with eGFR classification at 10–13 years with Cases and Controls in the model. There is no significant variable detected when race/ethnicity, birth weight, overweight, obesity, SBP classification, and Cases (PT-VLBW) vs. Controls are in the model. When we use neonatal characteristics in a model restricted to Cases (n = 62) to assess the roles of birth weight, GA, and ANS, birth weight is significant, P < 0.015, and a 1.0 g rise in birth weight is associated with a 0.56 rise in eGFRcysC. Importantly, 57% of PT-VLBW Cases with a low eGFRcysC at 1–3 years have a persistent low eGFRcysC at 10–13 years, P = 0.03 (Supplementary Table 1).
Discussion
Infants born PT-VLBW are at increased risk for elevated SBP in childhood, adolescence, and early adulthood.6,9,11,41,42,43,44,45,46 These observations are derived from population-based cohort studies that generally do not include parallel serial measurements of blood pressure and/or renal function beginning in infancy and continuing to preadolescence, which might improve our understanding of the presentation, progression, and pathogenesis of disease. To address this, we restudied children at 10–13 years who were born PT-VLBW and originally seen at 1, 2, or 3 years of age.18,19,47 At 10–13 years, nearly half are overweight or obese and have an elevated SBP, three quarters of whom are hypertensive. Moreover, a third have a reduced eGFR that persisted from infancy, while nearly 20% not only have an elevated SBP but also a reduced eGFR. When compared with Term-matched Controls, their BMI Z-score and prevalence of overweight/obesity do not differ; however, the PT-VLBW Cases are more likely to have an elevated SBP with hypertension and low eGFR. Thus, the occurrence of an elevated SBP and low renal function early in infancy in PT-VLBW infants persists at 10–13 years of age, demonstrating the need to not only study this population more intensely across childhood but also provide improved screening for blood pressure, renal function, and obesity starting early in infancy.
We reenrolled and consented 52% of the original PT-VLBW 10 years after their initial enrollment. Due to the relatively small study population, we sought to insure there is no bias. There are no substantive differences within the population studied other than minor differences in race/ethnicity and GA. Moreover, there are no significant differences in other neonatal variables between reenrolled and not reenrolled Cases. Furthermore, we reenrolled approximately 50% of each of the three cohorts originally seen at 1–3 years and observed no differences in neonatal characteristics between these cohorts at 10–13 years. Thus, we believe the reenrolled Cases are representative of the initial 120 infants studied.
A primary objective of our study was to determine whether there was persistence or progression of an abnormal SBP during the first 10–13 years of life in PT-VLBW neonates. Several investigators using variable sized population cohorts have reported an increase prevalence of an elevated SBP during childhood, including adolescence, but only a few included serial measurements within the same population.22,23,44 In our earlier study, SBP and SBP Z-scores at 1–3 years of age exceeded that expected for age and ~20% were ≥90th centile.18 The number with a normal SBP at 1–3 years decreased ~50% at preadolescence while those subsequently classified hypertensive rose fourfold. This redistribution, however, is not significant, likely reflecting the relatively small number of patients studied and/or the fact that only 52% of the original cohort was reenrolled. Furthermore, we excluded SBP measurements at 1–3 years in three reenrolled Cases since they were obtained while the infant was in an unstable state, which falsely elevates the SBP;48 their SBP is normal at 10–13 years. Thus, the prevalence of an elevated SBP increases between infancy and preadolescence and is associated with an increase in the occurrence of hypertension. This should be examined further in larger population-based studies that include serial measurements.
Infants born PT-VLBW exhibit disproportionate weight-for-length growth at neonatal intensive care unit (NICU) discharge and at 6 months and 1–2 years corrected age, which is associated with elevations in SBP at follow-up.18,19,49 At 3 years, the indices of overweight/obesity and an elevated SBP Z-scores were no longer evident, suggesting a relationship between being overweight and having an elevated SBP in infancy.18 At 10–13 years, nearly half of our Cases are overweight/obese; surprisingly, this does not differ from Term-matched Controls. In addition, the overall mean velocity of weight gain from birth to preadolescence does not differ. Nonetheless, the Cases are more likely to have an elevated SBP and be hypertensive. Vohr et al.23 also observed no difference in overall BMI between preterm and term born adolescents at 16 years, yet SBP was higher in the preterm. Of note, in comparison with Vohr’s adolescent population, the incidence of a BMI ≥ 85th centile in our preadolescent population was 40% greater and the incidence of a SBP ≥ 90th centile was three times greater, i.e., 48 vs. 17.6%. This may reflect differences in race/ethnicity, i.e., Vohr’s population is described as being 75% White non-Hispanic and 8% Hispanic as compared to 0% White non-Hispanic and 86% White Hispanic in the present study. This suggests involvement of unique ethnic and/or environmental influences on weight gain, e.g., diet, and the risk of an elevated SBP after preterm birth. This novel observation illustrates the problem of making broad conclusions about the outcomes of preterm births without detailed consideration of racial/ethnic makeup. Nonetheless, the present study confirms that preterm birth plus being overweight or obese (BMI ≥ 85th centile) at preadolescence contributes to an increased likelihood of having an elevated SBP and hypertension and this is more likely in Hispanic children born PT-VLBW.
Comparing serial measurements of blood pressure within the PT-VLBW Cases revealed a nearly fourfold rise in values ≥95th centile between 1–3 years and 10–13 years. When we examined potential factors associated with this change, SBP significantly correlated with the velocity of weight gain from birth to adolescence, suggesting that catch-up growth might contribute. Multivariate regression analysis revealed that only overweight and/or obesity contribute to a SBP > 90th centile. When we assessed SBP ≥ 95th centile at preadolescence, the aOR for a BMI > 85th centile doubled. Notably, neither birth weight nor GA contributed, consistent with a recent analysis of nine cohort studies assessing young adults born VLBW.11 In a retrospective cohort study of extremely preterm low-birth-weight infants followed 7–10 years, Mhanna et al.22 also observed an association between obesity and hypertension and reported that BMI and weight gain velocity from birth to 3 years (P = 0.008) predicted an elevated SBP. Edstedt-Bonamy et al.42 observed similar relationships in a Swedish population-based cohort of extremely preterm infants compared to term-matched controls at 6 years. Vohr et al.44 also examined weight gain velocity in a population of extremely preterm infants between 18 months and school age and noted that it predicted an elevated SBP at 6–7 years with a relative risk 1.36. In addition, in a retrospective review of 160 children born preterm and with at least three blood pressure measurements between 10 and 15 years, the odds of having a SBP ≥95th percentile was 1.6 times greater for every one standard deviation increase in BMI.50 The current study is consistent with these reports but differs due to ethnic/racial differences noted earlier. Moreover, it supports the conclusion that preterm children who are overweight and/or obese in early childhood are at increased risk for elevated blood pressure in preadolescence.
Renal dysfunction in the PT-VLBW population is related to the occurrence of chronic renal disease in adolescence and adults.27,28,29,30,31,32,33,46,51,52,53,54 However, few investigators have examined the age of onset and none obtained serial measurements of renal function between early infancy and later childhood.55 We19 previously reported that renal autoregulation appeared dysfunctional in PT-VLBW at 1 year corrected age, suggesting hyperfiltration. In addition, the 3-year-old cohort had a decreased eGFRcysC, which correlated with decreasing birth weight and GA. We now report that these PT-VLBW Cases have a greater prevalence of low eGFR at 10–13 years than Term-matched Controls and again observe that eGFRcysC decreases with decreasing birth weight and GA; however, the correlation with birth weight is greater than GA. This is consistent with other reports, but it is surprising since GA is generally considered a better marker for organ development than birth weight.32 This observation could reflect the contribution of adverse events occurring before and/or after birth, e.g., intrauterine nutritional deficiency, which occurred in 20% of our cohort, or adverse postnatal events, such as acute kidney injury.31,32 It is notable that none of the PT-VLBW Cases have an eGFRcysC > 140 mL min−1 [1.73 m2]−1 and evidence of hyperperfusion, whereas 17% of Term-matched Controls exhibit hyperperfusion at preadolescence, which is consistent with recent observations.56 It is possible that the development of obesity after birth and its consequences may contribute, suggesting that the low renal function may be due several variables. Future studies should consider modifying the disproportionate weight gain that frequently occurs in the NICU and after discharge as well as the rate of weight gain in childhood. Nonetheless, it appears that decreases in eGFR in PT-VLBW infants persist from infancy to preadolescence, but the pathophysiology and age it evolves into chronic renal disease remain unclear.
Limitations to this study include small sample size, predominant Hispanic population, and lack of concurrently collected data from a term-born control population. We addressed the latter by using the most recent NHANES dataset to match term-delivered controls 2:1. Furthermore, a subset of the Control population at 12 years had serum Cr measurements, which allowed us to compare eGFRCr at 12–13 years. We believe there was no selection bias during recruitment, which also could alter conclusions. A strength of this study is the ability to identify all of the earlier participants within our health care system and the recruitment of >50% 10 years later. Moreover, we collected blood samples from 100% and studied renal function between infancy and preadolescence. It is obvious that a more diverse PT-VLBW population should be studied in the future.
Conclusions
We have shown in this prospective cohort study of PT-VLBW infants originally seen at 1–3 years and again at 10–13 years that overweight/obesity, elevated SBP, and low renal function occur as early as 6 months corrected age and persist at 10–13 years of age. Moreover, while the occurrence of overweight/obesity is similar in Term-matched controls with a similar ethnicity at 10–13 years, the occurrence of an elevated SBP, hypertension, and low eGFR are significantly greater in the PT-VLBW population. Furthermore, nearly 20% of Cases have an elevated SBP plus low eGFR. How this will progress during adolescence and in early adulthood requires further follow-up. It also remains unclear whether measurements at 1–3 years and/or 10–13 years will predict the severity and/or occurrence of adult disease. Nonetheless, it is important that PT-VLBW neonates receive improved comprehensive long-term care that includes serial assessment of renal function, blood pressure, and obesity, which might permit early recognition of renal disease and hypertension and the institution of appropriate therapies.57,58
Data availability
The nonidentified datasets generated and/or analyzed during the current study may be available from the corresponding author on reasonable request.
References
Barker, D. J. & Martyn, C. N. The maternal and fetal origins of cardiovascular disease. J. Epidemiol. Community Health 46, 8–11 (1992).
Barker, D. J. The intrauterine origins of cardiovascular disease. Acta Paediatr. 391, 93–99 (1993).
Luyckx, V. A. et al. Effect of fetal and child health on kidney development and long-term risk of hypertension and kidney disease. Lancet 382, 273–283 (2013).
Sutherland, M., Ryan, D., Black, M. J. & Kent, A. L. Long-term renal consequences of preterm birth. Clin. Perinatol. 41, 561–573 (2014).
Chehade, H., Simeoni, U., Guignard, J. P. & Boubred, F. Preterm birth: long term cardiovascular and renal consequences. Curr. Pediatr. Rev. 14, 219–226 (2018).
de Jong, F., Monuteaux, M. C., van Elburg, R. M., Gillman, M. W. & Belfort, M. B. Systematic review and meta-analysis of preterm birth and later systolic blood pressure. Hypertension 59, 226–234 (2012).
Parkinson, J. R., Hyde, M. J., Gale, C., Santhakumaran, S. & Modi, N. Preterm birth and the metabolic syndrome in adult life: a systematic review and meta-analysis. Pediatrics 131, e1240–e1263 (2013).
Paquette, K. et al. Kidney size, renal function, Ang (angiotensin) peptides, and blood pressure in young adults born preterm. Hypertension 72, 18–928 (2018).
Keijzer-Veen, M. G., Dulger, A., Dekker, F. W., Nauta, J. & van der Heijden, B. J. Very preterm birth is a risk factor for increased systolic blood pressure at a young adult age. Pediatr. Nephrol. 25, 509–516 (2010).
Keijzer-Veen, M. G. et al. Reduced renal length and volume 20 years after very preterm birth. Pediatr. Nephrol. 25, 499–507 (2010).
Hovi, P. et al. Blood pressure in young adults born at very low birth weight: Adults Born Preterm International Collaboration. Hypertension 68, 880–887 (2016).
Darlow, B. A., Martin, J. & Horwood, L. J. Metabolic syndrome in very low birth weight young adults and controls: The New Zealand 1986 VLBW Study. J. Pediatr. 206, 128–133 (2019).
Belfort, M. B., Rifas-Shiman, S. L., Rich-Edwards, J., Kleinman, K. P. & Gillman, M. W. Size at birth, infant growth, and blood pressure at three years of age. J. Pediatr. 151, 670–674 (2007).
Edvardsson, V. O., Steinthorsdottir, S. D., Eliasdottir, S. B., Indridason, O. S. & Palsson, R. Birth weight and childhood blood pressure. Curr. Hypertens. Rep. 14, 596–602 (2012).
Johansson, S. et al. Risk of high blood pressure among young men increases with the degree of immaturity at birth. Circulation 112, 3430–3436 (2005).
Juonala, M. et al. Effect of birth weight on life-course blood pressure levels among children born premature: the Cardiovascular Risk in Young Finns Study. J. Hypertens. 33, 1542–1548 (2015).
Vashishta, N., Surapaneni, V., Chawla, S., Kapur, G. & Natarajan, G. Association among prematurity (<30 weeks’ gestational age), blood pressure, urinary albumin, calcium, and phosphate in early childhood. Pediatr. Nephrol. 32, 1243–1250 (2017).
Duncan, A. F., Heyne, R. J., Morgan, J. S., Ahmad, N. & Rosenfeld, C. R. Elevated systolic blood pressure in preterm very-low-birth-weight infants ≤3 years of life. Pediatr. Nephrol. 26, 1115–1121 (2011).
Frankfurt, J. A., Duncan, A. F., Heyne, R. J. & Rosenfeld, C. R. Renal function and systolic blood pressure in very-low-birth-weight infants 1-3 years of age. Pediatr. Nephrol. 27, 2285–2291 (2012).
Eriksson, J. G., Forsen, T. J., Kajantie, E., Osmond, C. & Barker, D. J. Childhood growth and hypertension in later life. Hypertension 49, 1415–1421 (2007).
Huxley, R. R., Shiell, A. W. & Law, C. M. The role of size at birth and postnatal catch-up growth in determining systolic blood pressure: a systematic review of the literature. J. Hypertens. 18, 815–831 (2000).
Mhanna, M. J., Iqbal, A. M. & Kaelber, D. C. Weight gain and hypertension at three years of age and older in extremely low birth weight infants. J. Neonatal Perinat. Med. 8, 363–369 (2015).
Vohr, B. R., Allan, W., Katz, K. H., Schneider, K. C. & Ment, L. R. Early predictors of hypertension in prematurely born adolescents. Acta Pediatr. 99, 1812–1818 (2010).
Brenner, B. M. & Anderson, S. The interrelationships among filtration surface area, blood pressure, and chronic renal disease. J. Cardiovasc. Pharmacol. 6, S1–S7 (1992).
Brenner, B. M., Garcia, D. L. & Anderson, S. Glomeruli and blood pressure. Less of one, more the other? Am. J. Hypertens. 1, 335–347 (1988).
Bains, R. K., Sibbons, P. D., Murray, R. D., Howard, C. V. & van Velzen, D. Stereological estimation of the absolute number of glomeruli in the kidneys of lambs. Res. Vet. Sci. 60, 122–125 (1996).
Hibino, S. et al. Proteinuria caused by glomerular hypertension during adolescence associated with extremely premature birth: a report of two cases. Pediatr. Nephrol. 30, 1889–1892 (2015).
Hodgin, J. B., Rasoulpour, M., Markowitz, G. S. & D’Agati, V. D. Very low birth weight is a risk factor for secondary focal segmental glomerulosclerosis. Clin. J. Am. Soc. Nephrol. 4, 71–76 (2009).
Ikezumi, Y. et al. Low birthweight and premature birth are risk factors for podocytopenia and focal segmental glomerulosclerosis. Am. J. Nephrol. 38, 149–157 (2013).
Koike, K. et al. Glomerular density and volume in renal biopsy specimens of children with proteinuria relative to preterm birth and gestational age. Clin. J. Am. Soc. Nephrol. 12, 585–590 (2017).
Luyckx, V. A. Preterm birth and its impact on renal health. Semin. Nephrol. 37, 311–319 (2020).
Luyckx, V. A. & Brenner, B. M. Clinical consequences of developmental programming of low nephron number. Anat. Rec. 303, 2613–2631 (2020).
Sutherland, M. R. et al. Accelerated maturation and abnormal morphology in the preterm neonatal kidney. J. Am. Soc. Nephrol. 22, 1365–1374 (2011).
Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: clinical and laboratory data 2015-2016. https://wwwn.cdc.gov/nchs/nhanes/search.aspx (2017).
Pickering, T. G. et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 111, 697–716 (2005).
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. Fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114, 555–576 (2004).
Flynn, J. T. et al. Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140, e20171904 (2017).
Centers for Disease Control and Prevention (CDC). A SAS program for the 2017 CDC growth charts. https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm (2022).
Mian, A. N. & Schwartz, G. J. Measurement and estimation of glomerular filtration rate in children. Adv. Chronic Kidney Dis. 24, 348–356 (2017).
Wintour, E. M. et al. Reduced nephron number in adult sheep, hypertensive as a result of prenatal glucocorticoid treatment. J. Physiol. 549, 929–935 (2003).
Bonamy, A.-K. E., Kallen, K. & Norman, M. High blood pressure in 2.5-year-old children born extremely preterm. Pediatrics 129, e1199–e1204 (2012).
Edstedt Bonamy, A.-K. et al. Blood pressure in 6-year-old children born extremely preterm. J. Am. Heart Assoc. 6, e005858 (2017).
Chiolero, A., Cachat, F., Burnier, M., Paccaud, F. & Bovet, P. Prevalence of hypertension in schoolchildren based on repeated measurements and association with overweight. J. Hypertens. 25, 2209–2217 (2007).
Vohr, B. R. et al. High blood pressure at early school age among extreme preterms. Pediatrics 142, e20180269 (2018).
Roberts, G., Lee, K. J., Cheong, J. L. & Doyle, L. W. Higher ambulatory blood pressure at 18 years in adolescents born less than 28 weeks’ gestation in the 1990s compared with term controls. J. Hypertens. 32, 620–626 (2014).
South, A. M. et al. Renal function and blood pressure are altered in adolescents born preterm. Pediatr. Nephrol. 34, 137–144 (2019).
Duncan, A. F., Frankfurt, J. A., Heyne, R. J. & Rosenfeld, C. R. Biomarkers of adiposity are elevated in preterm very-low-birth-weight infants at 1, 2, and 3 years of age. Pediatr. Res. 81, 780–786 (2017).
Duncan, A. F., Rosenfeld, C. R., Morgan, J. S., Ahmad, N. & Heyne, R. J. Inter-rater variability and effect of state on blood pressure measurements in infants at 1-3 years of age. Pediatrics 22, e590–e594 (2008).
Brion, L. P. et al. Optimizing individual nutrition in preterm very low birth weight infants: double-blinded randomized controlled trial. J. Perinatol. 40, 655–665 (2020).
Vasylyeva, T. L., Chennasamudram, S. P. & Okogbo, M. E. Can we predict hypertension among preterm children? Clin. Pediatr. 50, 936–942 (2011).
Crump, C., Sundquist, J., Winkleby, M. A. & Sundquist, K. Preterm birth and risk of chronic kidney disease from childhood into mid-adulthood: national cohort study. BMJ 365, l1346 (2019).
Gilarska, M. et al. Extremely low birth weight predisposes to impaired renal health: a pooled analysis. Kidney Blood Press. Res. 44, 897–906 (2019).
Hirano, D. et al. Association between low birth weight and childhood-onset chronic kidney disease in Japan: a combined analysis of a nationwide survey for paediatric chronic kidney disease and the National Vital Statistics Report. Nephrol. Dial. Transpl. 31, 1895–1900 (2016).
Sanderson, K. R. et al. Albuminuria, hypertension, and reduced kidney volumes in adolescents born extremely premature. Front. Pediatr. 8, 230 (2020).
Starzec, K., Klimek, M., Grudzień, A., Jagła, M. & Kwinta, P. Longitudinal assessment of renal size and function in extremely low birth weight children at 7 and 11 years of age. Pediatr. Nephrol. 31, 2119–2126 (2016).
Turer, C. B., Baum, M., Dubourg, L., Selistre, L. S. & Skinner, A. C. Prevalence of hyperfiltration among US youth/young adults with overweight and obesity: a population-based association study. Obes. Sci. Pract. 5, 570–580 (2019).
Hartz, J., Li, J. S., Akintoye, O. O. & Hornik, C. P. Clinicians’ adherence to guidelines on evaluation of hypertension in children and adolescence. World J. Pediatr. Congentil. Heart Surg. 7, 440–445 (2016).
Shah, L., Hossain, J., Xie, S. & Zaritsky, J. Poor adherence to early childhood blood pressure measurement guidelines in a large pediatric healthcare system. Pediatr. Nephrol. 34, 697–701 (2019).
Acknowledgements
V.B., MD, was a Fellow in Neonatal-Perinatal Medicine and identified all the PT-VLBW Cases 10 years after their original recruitment, consented each at a clinic visit, and obtained the anthropometric and blood pressure measurements. J.W. was a Fellow in Neonatal-Perinatal Medicine. Both are presently at Phoenix Children’s Hospital and University of Arizona College of Medicine Phoenix.
Funding
These studies were supported by funds from the George L. MacGregor Professorship awarded to C.R.R. There was no extramural financial support.
Author information
Authors and Affiliations
Contributions
J.W., L.S.B., R.H., C.T., and C.R.R. made substantial contributions to conception and design, acquisition of data, analyses, and interpretation of data. V.B. contributed to the study design and acquisition of all clinical data, blood samples, and patient consent. All authors contributed to drafting the manuscript, revising it critically for important intellectual content, and provided final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Informed consent was obtained at 10–13-year follow-up.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wickland, J., Steven Brown, L., Blanco, V. et al. Persistent high blood pressure and renal dysfunction in preterm infants during childhood. Pediatr Res 93, 217–225 (2023). https://doi.org/10.1038/s41390-022-02083-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02083-y