Abstract
Background:
Factors affecting innate immunity and acting as inflammatory regulators, such as the nuclear peroxisome proliferator-activated receptors (PPAR) could be crucial in the pathogenesis of necrotizing enterocolitis (NEC). We hypothesized that the PPARγ agonist pioglitazone (PIO) might be effective in preventing the development of NEC and/or reducing its severity.
Methods:
We studied preterm rats in which NEC was induced using the hypoxia-hypothermia model. The treatment group (TG; n = 30) received enteral PIO (10 mg/kg/d) for 72 h and the control group (CG; n = 30) did not. Animals were sacrificed 96 h after birth. NEC was diagnosed evaluating histological ileum changes, and mRNA levels of IL-4, IL-12, IL-6, IL-10, INF-γ, and TNF-α cytokines were measured.
Results:
NEC occurrence was higher in the CG (18/30; 60%) than in the TG (5/30; 16.7%) and was more severe. Proinflammatory IL-12 and INF-γ mRNA levels were significantly lower in the TG than in the CG; conversely, the anti-inflammatory IL-4 mRNA level was significantly higher in the TG than in the CG.
Conclusion:
Our results demonstrate for the first time that PIO is effective in reducing the incidence and severity of NEC and in decreasing renal injuries in a preterm rat model.
Similar content being viewed by others
Main
Necrotizing enterocolitis (NEC) is the most common neonatal gastrointestinal complication in preterm infants (1). The prevalence of this disease is about 7% in infants with birth weght from 500 to 1,500 g, with a mortality of 30% in 28 to 36 wk of gestation infants and 40 % in <28-wk infants (2). Moreover, the development of NEC increases the risk of a delay in neurodevelopment, because inflammatory processes occurring in the gut can have a systemic diffusion, affecting other organs such as the brain (3), and, as recently suggested, the kidney (4). The physiopathology of NEC is not completely understood; however it is considered a multifactoral disease including intestinal immaturity, microbial colonization, and hypoxia–ischemia damage as risk factors. Recently, many studies have suggested that the intestinal mucosa and innate immune system play major roles in the pathogenesis of NEC (5). Thus, factors affecting innate immunity and regulating inflammation, such as the nuclear peroxisome proliferator-activated receptors (PPAR), could be crucial. PPAR are a family of ligand-activated nuclear receptor transcription factors that regulates the function and expression of complex gene networks, especially involved in energy homeostasis and inflammation (6). They consist of three isoforms (α, β, γ), and PPARγ has been shown to induce anti-inflammatory responses inhibiting proinflammatory transcription factors such as nuclear factor κ-light-chain-enhancer of activated B cells (NF-κB) (7,8,9). Moreover, PPARγ can promote an anti-inflammatory antioxidant response interacting with different enzymatic pathways such as cyclooxygenase 2 (COX-2), inducible nitric oxide synthase (iNOS), and endothelial nitric oxide synthase (eNOS) (6). For these reasons, many PPARγ agonists have been implicated in the treatment of oxidative stress-related diseases, such as inflammatory bowel diseases (10) and Parkinson’s disease (11).
Thus, we hypothesized that the thiazolidinedione PPARγ agonist pioglitazone (PIO) might be effective in preventing the development of NEC and/or reducing its severity, and limiting the renal diffusion of related inflammatory processes as markers of a systemic action of the drug. To assess this hypothesis, we pretreated newborn preterm rats in which NEC had been experimentally induced with PIO.
Methods
Animal Model and Experimental Design
The study protocol was approved by the Italian Ministry of Veterinary Public Health (ordinance n 178/2013 B). In vivo experiments were performed using Sprague-Dawley newborn rats (Harlan Laboratories S.r.l., S.Pietro al Natisone, Udine, Italy), born by cesarian section 1 d before scheduled birth. Newborn rat pups were weighed and placed in an incubator to control body temperature. Animals were fed six times a day with a total volume of 850 μl (12) of a formula obtained by the combination of Similac infant formula (15 g; Abbott Laboratories, Columbus, OH) and Esbilac canine replacement milk (75 ml; PetAg, Hampshire, IL) (13). The weight of the rats was recorded daily.
NEC was induced following the hypoxia/hypothermia protocol as previously described (13,14). Briefly, rats were fed with formula (see above) and stressed twice a day with hypoxia by breathing 100% nitrogen gas in a closed chamber for 60 s, followed by a 10-min exposure to 4 °C temperature.
Rat pups were divided into the treatment group (TG), which was treated with enteral PIO (daily dose 10 mg/kg divided into four aliquots) for 72 h and the control group (CG), which was not.
Ninety-six hours after birth, all surviving animals were sacrificed. Animals with signs of distress or imminent death before the end of the study period were terminated and included in the study.
Tissue Harvest and NEC Evaluation
The gastrointestinal tract was carefully removed. A 2-cm tract of distal ileum was collected, separated into four alternative pieces, and stored at −80 °C for RNA extraction or formaldehyde (4%) fixed-paraffin embedded, and stained with hematoxylin and eosin for histological evaluation (12).
Histological changes in the ileum were scored by a blinded evaluator and graded as described by Dvorak et al. (15) for NEC diagnosis and severity evaluation. In detail, NEC scores were given as follows: 0 (normal), no tissue damage; 1 (mild), slight submucosal and/or lamina propria separation; 2 (moderate), moderate detachment of submucosa and/or lamina propria, and/or edema in submucosal and muscular layers; 3 (severe), severe detachment of submucosa and/or lamina propria, and/or severe edema in submucosa and muscular layers, regional villi sloughing; 4 (necrosis), loss of villi and tissue necrosis. Intermediate scores of 0.5, 1.5, 2.5, and 3.5 were also utilized to more accurately assess the severity of ileal damage when necessary. The diagnosis of NEC was made for histological scores ≥ 2 (16,17).
RNA Purification and Quantitative polymerase chain reaction
Total RNA was extracted from frozen ileal tissues using the TRIzol reagent (Life Technologies, Milan, Italy) or from formaldehyde fixed-paraffin embedded tissues with the ReliaPrep RNA Miniprep System extraction kit (Promega, Milan, Italy) following manufacturers’ instructions. One microgram of RNA was initially reverse transcribed with the High-Capacity RNA-to-cDNA Kit (Life Technologies) in 20 ml reaction volume and then the cDNA was diluted to a final volume of 200 ml. Quantitative PCR for interleukin (IL)-4, IL-12, IL-6, IL-10, Interferon-γ (INF-γ), tumor necrosis factor-α (TNF-α), and Glyceraldehyde-3-Phosphate Dehydrogenase (GAPDH) (Qiagen, Milan, Italy) was performed on an ABI PRISM 7000 (Applied Biosystem, Milan, Italy) with GoTaq qPCR Master Mix (Promega) using 5 ml of cDNA as template. Relative expression levels were calculated with the ΔΔCt method with GAPDH as housekeeping gene, using the Data Assist software (Life Technologies).
Evaluation of Kidney Fibrosis
Sirius red staining was used to evaluate renal interstitial fibrosis according to established methods (18). The collagen proteins (extracellular matrix) were stained distinctly red under a light microscope and luminous color under polarized light. Sirius red staining was performed on 7-μm sections of kidney tissues fixed in 4% formalin and embedded in paraffin, mounted on slides. After brief rehydration, deparaffinized sections were incubated for 60 min with Sirius red solution (saturated solution of picric acid 0.1% Direct red 80); after two washes in acidified water, sections were dehydrated by alcohol, cleared in xylene, and mounted with DPX mounting medium. Sirius staining was quantified with ImageJ (imagej.nih.gov/ij/). Briefly, low-magnification images of stained sections were acquired with a Leica DM4000B light microscope equipped with a DFC320 camera. After color correction and threshold with ImageJ, Sirius red-stained areas were measured and normalized for the total area of the sections; results are reported as percentage of stained area.
Statistical Analysis
Numerical data are expressed as mean ± SD for normal distributed value or as median and interquartile range for non-normal distributed value. Cytokine mRNA was expressed as relative quantity (RQ) with 95% confidence interval (CI). Normality was tested with D’Agostino-Pearson Omnibus test. Rat weight and stained Sirius red renal areas were compared between TG and CG using an unpaired t-test. NEC scores between the TG and CG were compared using the Mann-Whitney U-test for nonparametric values, while the chi-square test was used to analyze differences in incidence of NEC between groups. Differences in gene expression were analyzed by Mann-Whitney U-test adjusting the P value with the Benjamini-Hochberg false discovery rate (FDR) method for statistical correction of multiple comparison. All statistical analyses were carried out using the statistical program R (19) and Graph Pad prism 6 (GraphPad Software, Inc, La Jolla, CA).
The sample size was calculated assuming an incidence of NEC of 60 and 25% in the CG and TG, respectively. We calculated that we needed to study 30 rats in each group to detect this difference as statistically significant with 80% power at 0.05 level.
Results
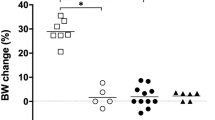
Sixty preterm rats delivered from four separate litters were enrolled in the study and randomly assigned to the treatment group (TG, n = 30) or control group (CG, n = 30). Birth weight was similar in the two groups (TG vs. CG: 5.8 g ± 0.6 g vs. 5.8 g ± 0.6 g; P = 0.86). During the study period, body weights gradually decreased in both groups but the reduction was higher in the CG than in the TG starting from 48 h (TG vs. CG: 4.4 ± 0.4 g vs. 4.0 g ± 0.4 g, P < 0.01) until to 96 h of life (TG vs. CG 4.2 g ± 0.4 g vs. 3.5 g ± 0.5 g, P < 0.01) ( Figure 1 ). Mortality at 96 h of age was lower in the TG (2/30, 7%) than in the CG (5/30, 17%), but this difference was not statistically significant (P = 0.42).
Pioglitazone treatment ameliorates necrotizing enterocolitis severity in the preterm newborn rat. Body weights of rats were measured once a day from birth to the end of the experiments; loss of body weight was significantly decreased in TG rats (▪, black squares) and remained statistically different from CG rats (• , black circles) starting from 48 h after pioglitazone treatment. **P < 0.01. Data are reported as means ± SD.
Macroscopically, the intestinal tracts of CG rats were darker and more hemorrhagic than those of TG rats, suggesting the development of typical NEC injuries ( Figure 2a ). Histological examination confirmed that the large majority of villi and mucosal structures in TG rats had normal morphology, but were severely injured in CG rats ( Figure 2b ). Consequently, the NEC score was higher (P < 0.01) in the CG (2 (1.5–2.9)) than in the TG (1 (1–1.5)) ( Figure 3a ), and the occurrence of NEC was significantly higher (P < 0.01) in the CG (18/30; 60%) than in the TG (5/30; 17%) ( Figure 3b ). PIO reduced the incidence of NEC in the TG by 72% in comparison with the CG (60 vs. 17%).
Macroscopic and histological aspect of rat intestines. (a) Representative macroscopic pictures of a normal intestine in a TG rat (right panel) and a CG rat intestine (left panel) with severe and diffuse necrotizing enterocolitis. (b) Representative hematoxylin and eosin (H&E) stained ileal sections showing normal mucosa in pioglitazone-treated rats and severe damage in the CG rat. Black-rounded squares indicate area shown at higher magnification in the near right panels. Scale bar: 200 µm for left panels; 50 µm for right panels.
NEC quantification in newborn rats. NEC evaluation was performed on H&E stained sections of ileum tracts of rats. The NEC incidence was lower in TG rats (a) (17% vs. 60%) and was associated with a significantly decreased NEC score (b) compared to CG. **P < 0.01. NEC, necrotizing enterocolitis.
IL-12 and INF-γ mRNA levels were significantly reduced in the TG compared to the CG by 3.9- and 2.7-fold, respectively (IL-12 RQ 0.25 95% CI median (0.06, 0.51); INFγ 0.37 95% CI median (0.23, 0.61), P < 0.05 for both); conversely, IL-4 was increased by 4.2-fold in the TG (RQ 4.2 95% CI median (1.96, 5.41), P<0.05) ( Figure 4 ). TNF-α (P: 0.377, FDR:0.45), IL-6 (P: 0.453, FDR: 0.45), and IL-10 (P: 0.235, FDR: 0.5) mRNA levels were similar in the TG and CG rats.
Pioglitazone modulates inflammatory cytokines. Expression of inflammatory cytokines was evaluated by quantitative PCR on RNA extracted from ilea of CG and TG rats. Significant differences were detected in the expression of mRNA levels of the IL-12, INFγ, and IL-4 in the ileus of TG compared to the CG. Data are represented as the median fold induction calculated with the ΔΔCt method; error bars are 95% confidence interval of the median relative quantity. The dotted line denotes the basal level in CG rats.
Sirius red staining showed that deposition of extracellular matrix in the peritubular space was lower in the TG than in the CG (13.37 ± 7% vs. 5.9 ± 4.5%, CG vs. TG, P < 0.05) ( Figure 5 ).
Effect of pioglitazone on kidney fibrosis. Collagen deposition after necrotizing enterocolitis induction was analyzed by Sirius red staining; representative images of CG (a) and TG (b) clearly show a marked reduction of fibrosis in renal parenchyma, suggestive of a systemic protective effect of pioglitazone treatment. (c) Quantitative analysis of collagen staining in CG and TG rats demonstrates a reduction of collagen fibers in treated rats. **P < 0.01. Scale bar: 50 µm.
Discussion
In this study, we evaluated for the first time the efficacy of PPAR-γ agonist PIO in preventing NEC in a neonatal rat model. We were able to demonstrate that PIO decreases the occurrence of NEC and its severity.
Baregamian et al. (20) first reported the overexpression of PPAR-γ in the rat model of NEC and the effectiveness of pretreatment with PIO in attenuating small bowel injury. However, their study was performed using an adult animal model in which NEC was induced following an ischemia–reperfusion procedure (20) that might not resemble the pathogenesis of NEC in the preterm infant very well. Similarly, Okada et al. (21) reported the overexpression of PPAR-γ in an NEC rat model. Their study was also performed using an adult animal model in which NEC was induced by overfeeding with formula milk but the possible role of PIO in preventing NEC was not evaluated (21). On the other hand, our animal model includes most NEC risk factors, such as prematurity, hypoxia, hypothermia, and formula feeding (22,23). Thus, our results represent a valuable confirmation of the previous study (20) and emphasize the possible role of the PPAR-γ agonist in the treatment of NEC.
The mechanism of action of PPAR-γ agonist has not been fully clarified but it is well known that inflammatory processes are crucial to the pathogenesis of NEC (5) and that the imbalance between pro- and anti-inflammatory cytokines can favor its development. In our study, we demonstrate that pretreatment with PIO is associated with an increase of anti-inflammatory IL-4 and decrease of the proinflammatory IL-12 and INF-γ in the gut of TG rats. This is relevant because it has been demonstrated that IL-4 leads to polarization of Th cell differentiation toward Th-2 cells that produce a variety of anti-inflammatory cytokines, including IL-4 itself, rather than toward Th1-type cells that produce several proinflammatory cytokines including TNF-α and INF-γ (24). Moreover, it has been found that there is an upregulation of IL-12 and a positive correlation between its production and the progression of tissue damage in an NEC rat model (25). Although IL-12 can induce the release of INF-γ by T-lymphocytes activating both innate and acquired immunity, its excessive production might favor organ disorders leading to the disruption of the immune system (26). Furthermore, INF-γ has been reported to inhibit intestinal recovery by preventing gap junction communication between enterocytes (27). Thus, our findings that PIO treatment is associated with an increase of IL-4 and decrease of IL-12 and INF-γ levels in the small bowel tissues can explain, at least partially, the mechanism by which it can prevent the development of NEC and/or decrease its severity in our animal model.
Our results are also consistent with previous studies in rat models of colitis (28,29) and myocarditis (14), which show that PPAR-γ receptor agonists (i.e., rosiglitazone, troglitazone, PIO) can exert protective effects on tissues by inhibiting Th-1-inflammatory processes and favoring the shift of immune system activity toward Th-2-dependent protective processes.
In our NEC rat model, PIO was effective in reducing kidney fibrosis secondary to inflammation suggesting a systemic action of this drug. This point may be potentially very important because it has been recently demonstrated that NEC leads not only to inflammation in the gastrointestinal tract, but also to renal inflammation, apoptosis, and altered expression of several renal tight junction that explain from a clinical point of view the frequent occurrence of acute renal failure in severe cases of NEC (29).
We found that PIO treatment was associated with a lower weight loss of preterm rats. This observation is interesting because the difference in weight loss between the TG and the CG becomes significant after 48 h of life. This probably occurs because, as suggested by Caplan et al. (30), gut injuries start within 36 h of life in this rat model of NEC, and the protective effect of PIO cannot be ascertained before 48 h of life.
In conclusion, we demonstrated for the first time that pretreatment with the PPAR-γ agonist PIO is effective in preventing the development of NEC and limiting its severity and decreasing renal injuries in a preterm rat model. This action is associated with an increase of the anti-inflammatory IL-4 and decrease of the proinflammatory IL-12 and INF-γ levels in the ileal tract of treated animals. Therefore, PIO could improve the balance between anti- and proinflammatory cytokines in the gastrointestinal tract. Our findings confirm that PPAR-γ agonists, such as PIO, are promising drugs for the pharmacological prevention and treatment of NEC and provide encouragement to the planning of clinical studies in the preterm infant.
Statement of Financial Support
This work was supported by Fondo per gli Investimenti della Ricerca di Base (FIRB) (RBAP10MY35_002), by Ente Cassa di Risparmio di Firenze and by FiorGen ONLUS to A.G.
Disclosure
The authors declare that they do not have any financial relationships that could be broadly relevant to this work. The authors declare no conflicts of interest in relation to the manuscript.
References
Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med 2011;364:255–64.
Murthy K, Yanowitz TD, DiGeronimo R, et al. Short-term outcomes for preterm infants with surgical necrotizing enterocolitis. J Perinatol 2014;34:736–40.
Hintz SR, Kendrick DE, Stoll BJ, et al.; NICHD Neonatal Research Network. Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics 2005;115:696–703.
Garg PM, Tatum R, Ravisankar S, Shekhawat PS, Chen YH. Necrotizing enterocolitis in a mouse model leads to widespread renal inflammation, acute kidney injury, and disruption of renal tight junction proteins. Pediatr Res 2015;78:527–32.
Terrin G, Scipione A, De Curtis M. Update in pathogenesis and prospective in treatment of necrotizing enterocolitis. Biomed Res Int 2014;2014:543765.
Polvani S, Tarocchi M, Galli A. PPARγ and oxidative stress: Con(β) catenating NRF2 and FOXO. PPAR Res 2012;2012:641087.
Li M, Pascual G, Glass CK. Peroxisome proliferator-activated receptor gamma-dependent repression of the inducible nitric oxide synthase gene. Mol Cell Biol 2000;20:4699–707.
Vandewalle B, Moerman E, Lefebvre B, et al. PPARgamma-dependent and -independent effects of rosiglitazone on lipotoxic human pancreatic islets. Biochem Biophys Res Commun 2008;366:1096–101.
Chung SW, Kang BY, Kim SH, et al. Oxidized low density lipoprotein inhibits interleukin-12 production in lipopolysaccharide-activated mouse macrophages via direct interactions between peroxisome proliferator-activated receptor-gamma and nuclear factor-kappa B. J Biol Chem 2000;275:32681–7.
Dubuquoy L, Rousseaux C, Thuru X, et al. PPARgamma as a new therapeutic target in inflammatory bowel diseases. Gut 2006;55:1341–9.
Randy LH, Guoying B. Agonism of peroxisome proliferator receptor-gamma may have therapeutic potential for neuroinflammation and Parkinson’s disease. Curr Neuropharmacol 2007;5:35–46.
Coursodon-Boyiddle CF, Snarrenberg CL, Adkins-Rieck CK, et al. Pomegranate seed oil reduces intestinal damage in a rat model of necrotizing enterocolitis. Am J Physiol Gastrointest Liver Physiol 2012;303:G744–51.
Dingle BM, Liu Y, Fatheree NY, Min J, Rhoads JM, Tran DQ. FoxP3= regulatory T cells attenuate experimental necrotizing enterocolitis. PLoS One 2013;8:e82963.
Hasegawa H, Takano H, Zou Y, et al. Pioglitazone, a peroxisome proliferator-activated receptor gamma activator, ameliorates experimental autoimmune myocarditis by modulating Th1/Th2 balance. J Mol Cell Cardiol 2005;38:257–65.
Dvorak B, Halpern MD, Holubec H, et al. Epidermal growth factor reduces the development of necrotizing enterocolitis in a neonatal rat model. Am J Physiol Gastrointest Liver Physiol 2002;282:G156–64.
Khailova L, Mount Patrick SK, Arganbright KM, Halpern MD, Kinouchi T, Dvorak B. Bifidobacterium bifidum reduces apoptosis in the intestinal epithelium in necrotizing enterocolitis. Am J Physiol Gastrointest Liver Physiol 2010;299:G1118–27.
Ran-Ressler RR, Khailova L, Arganbright KM, et al. Branched chain fatty acids reduce the incidence of necrotizing enterocolitis and alter gastrointestinal microbial ecology in a neonatal rat model. PLoS One 2011;6:e29032.
Lin SL, Kisseleva T, Brenner DA, Duffield JS. Pericytes and perivascular fibroblasts are the primary source of collagen-producing cells in obstructive fibrosis of the kidney. Am J Pathol 2008;173:1617–27.
R Core Team. R: A Language and Environment for Statistical Computing. Vienna, 2014. (http://www.R-project.org).
Baregamian N, Mourot JM, Ballard AR, Evers BM, Chung DH. PPAR-gamma agonist protects against intestinal injury during necrotizing enterocolitis. Biochem Biophys Res Commun 2009;379:423–7.
Okada K, Fujii T, Ohtsuka Y, et al. Overfeeding can cause NEC-like enterocolitis in premature rat pups. Neonatology 2010;97:218–24.
Hsueh W, Caplan MS, Qu XW, Tan XD, De Plaen IG, Gonzalez-Crussi F. Neonatal necrotizing enterocolitis: clinical considerations and pathogenetic concepts. Pediatr Dev Pathol 2003;6:6–23.
Travadi J, Patole S, Charles A, Dvorak B, Doherty D, Simmer K. Pentoxifylline reduces the incidence and severity of necrotizing enterocolitis in a neonatal rat model. Pediatr Res 2006;60:185–9.
Opal SM, DePalo VA. Anti-inflammatory cytokines. Chest 2000;117:1162–72.
Halpern MD, Holubec H, Dominguez JA, et al. Up-regulation of IL-18 and IL-12 in the ileum of neonatal rats with necrotizing enterocolitis. Pediatr Res 2002;51:733–9.
Okamura H, Kashiwamura S, Tsutsui H, Yoshimoto T, Nakanishi K. Regulation of interferon-gamma production by IL-12 and IL-18. Curr Opin Immunol 1998;10:259–64.
Leaphart CL, Qureshi F, Cetin S, et al. Interferon-gamma inhibits intestinal restitution by preventing gap junction communication between enterocytes. Gastroenterology 2007;132:2395–411.
Celinski K, Dworzanski T, Fornal R, et al. Comparison of anti-inflammatory properties of peroxisome proliferator-activated receptor gamma agonists rosiglitazone and troglitazone in prophylactic treatment of experimental colitis. J Physiol Pharmacol 2013;64:587–95.
Saubermann LJ, Nakajima A, Wada K, et al. Peroxisome proliferator-activated receptor gamma agonist ligands stimulate a Th2 cytokine response and prevent acute colitis. Inflamm Bowel Dis 2002;8:330–9.
Caplan MS, Hedlund E, Adler L, Hsueh W. Role of asphyxia and feeding in a neonatal rat model of necrotizing enterocolitis. Pediatr Pathol 1994;14:1017–28.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Corsini, I., Polvani, S., Tarocchi, M. et al. Peroxisome proliferator-activated receptor-γ agonist pioglitazone reduces the development of necrotizing enterocolitis in a neonatal preterm rat model. Pediatr Res 81, 364–368 (2017). https://doi.org/10.1038/pr.2016.214
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2016.214
This article is cited by
-
Peroxisome proliferator-activator receptor γ and psoriasis, molecular and cellular biochemistry
Molecular and Cellular Biochemistry (2022)
-
Characterization of the pathoimmunology of necrotizing enterocolitis reveals novel therapeutic opportunities
Nature Communications (2020)
-
Preventing dysbiosis of the neonatal mouse intestinal microbiome protects against late-onset sepsis
Nature Medicine (2019)
-
Recent Advances in Prevention and Therapies for Clinical or Experimental Necrotizing Enterocolitis
Digestive Diseases and Sciences (2019)