Abstract
Background:
The underlying neuro-protective mechanisms of antenatal magnesium sulfate (MgSO4) in infants born preterm remain poorly understood. Early neonatal brain injury may be preceded by low cerebral blood flow (CBF) and elevated cerebral fractional tissue oxygen extraction (cFTOE). This study investigated the effect of antenatal MgSO4 on cerebral oxygen delivery, consumption, and cFTOE in preterm infants.
Methods:
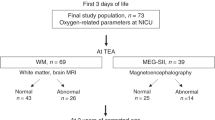
CBF and tissue oxygenation index were measured, and oxygen delivery, consumption, and cFTOE calculated within 24 h of birth and at 48 and 72 h of life in 36 infants ≤ 30 wk gestation exposed to MgSO4 and 29 unexposed infants.
Results:
Total internal carotid blood flow and cerebral oxygen delivery did not differ between the groups at the three study time-points. Cerebral oxygen consumption and cFTOE were lower in infants exposed to antenatal MgSO4 (P = 0.012) compared to unexposed infants within 24 h of delivery. This difference was not evident by 48 h of age. Fewer infants in the MgSO4 group developed P/IVH by 72 h of age (P = 0.03).
Conclusion:
Infants exposed to MgSO4 had similar systemic and cerebral hemodynamics but lower cFTOE compared to nonexposed. These findings suggest reduced cerebral metabolism maybe a component of the neuro-protective actions of antenatal MgSO4.
Similar content being viewed by others
Main
Despite significant improvements in survival for infants born preterm, the rate of major neurodevelopmental impairment in survivors has not diminished (1). As a result, strategies designed to reduce adverse neurological outcomes have been a major perinatal research focus. Antenatal magnesium sulfate (MgSO4) is one such strategy. Following the first report of an association between perinatal administration of MgSO4 and a reduction in the risk of peri/intraventricular hemorrhage (P/IVH) (2), its use as a neuro-protective therapy when given to women at risk of preterm birth has become established practice (3). While MgSO4 has been shown to decrease the risk of P/IVH (4), cerebral palsy and the rate of substantial gross motor dysfunction (5), the mechanisms underlying these effects remain poorly understood.
Proposed mechanisms by which MgSO4 exerts a neuro-protective effect include effects on the cardiovascular system through its role in the regulation of vascular tone (6), cerebral metabolism including prevention of excess glutamate release (7), and reductions in systemic proinflammatory cytokine production (8). The effect of antenatal MgSO4 administration on the neonatal systemic and cerebral vasculature is unclear. While increased cerebral blood flow (CBF) velocities have been reported in infants whose mothers received MgSO4 for the management of pre-eclampsia or tocolysis (9,10) another study has reported significant lowering of neonatal cerebral perfusion (11). The sole study reporting neonatal cardiovascular effects of antenatal MgSO4 for neuro-protection found no difference in echocardiographic measures of systemic blood flow on the first day of life (12).
For extremely preterm infants, the transition to extra-uterine life is characterized by low baseline CBF and high cerebral oxygen consumption (13), with cerebral oxygen consumption reflecting cerebral metabolic activity (14). Elevated cerebral fractional tissue oxygen extraction (cFTOE), derived by near infrared spectroscopy (NIRS), is a readily measurable variable of the relationship between cerebral oxygen delivery and consumption and precedes early neonatal brain injury following very preterm birth (15,16). While studies in fetal sheep have reported temporary reductions in cerebral oxygen consumption following MgSO4 administration (17), it is only recently that similar effects have been described in infants born to women given antenatal MgSO4 for pre-eclampsia (18). We hypothesized that reduced neonatal cerebral oxygen consumption contributes to the observed neuro-protective actions of antenatally administered MgSO4. Therefore, the aim of the current study was to investigate the effect of antenatal MgSO4 on cerebral oxygen delivery, consumption and cFTOE in preterm infants less than 30 wk gestation.
Results
Clinical characteristics of infants are shown in Table 1 . Thirty-six infants were exposed to MgSO4 for neuro-protection, with three receiving a 4 g loading dose alone prior to preterm delivery. The mean (minimum-maximum) maintenance dose received was 8 g (0.5–23 g). There was no significant difference for any clinical characteristics between those infants exposed to MgSO4 prior to delivery and those not. For the 28 infants not exposed to antenatal MgSO4, 12 (43%) delivered vaginally within 1 h of presentation to hospital and 16 (57%) required urgent emergency caesarean section following presentation (seven as a result of a significant cardiotocographic abnormality (such as persistent fetal tachycardia or prolonged fetal heart rate decelerations), six secondary to antepartum hemorrhage, two secondary to acute maternal sepsis/chorioamnionitis, and one following umbilical cord prolapse). The mean (SD) age of the infants at time of the initial NIRS and cranial ultrasound study was 11 (6) hours for the nonexposed group and 12 (7) hours for the MgSO4 group. While four infants had cranial ultrasound evidence of P/IVH at the time of the NIRS study (all unilateral grade 1 IVH), fewer infants in the MgSO4 group (n = 4) were diagnosed with P/IVH (all grades) compared to those not exposed to MgSO4 (n = 9) by 72 h of life (P = 0.03).
A significant main effect for time was observed for mean arterial blood pressure ( Figure 1a , P = 0.01) and right ventricular output ( Figure 1b , P = 0.02). On post-hoc analysis mean arterial pressure at 72 h of age was significantly higher compared to 24 h (P < 0.01) and 48 h (P = 0.01) and right ventricular output significantly higher at 72 h of age compared to 24 h of age (P < 0.01). No significant time effect was seen for total internal carotid blood flow ( Figure 1c , P = 0.19). No effect of MgSO4 exposure was observed for any of these systemic hemodynamic variables at any time point. As a result, NIRS-derived modified cerebral oxygen delivery was similar across the study period ( Figure 2a , P = 0.25) and between the MgSO4 exposure groups.
Postnatal alterations in systemic hemodynamics. (a) Invasive mean arterial blood pressure (mmHg), (b) right ventricular output (ml/kg/min), and (c) total internal carotid blood flow (ml/kg/min) in infants on days 1–3 of postnatal life. Black bars represent infants not exposed to MgSO4 and open bars represent infants exposed to antenatal MgSO4. For Panels a and b, *P = 0.01; **P < 0.01.
Postnatal changes in NIRS derived cerebral oxygen kinetics. (a) Modified cerebral oxygen delivery (ModcerbDO2), (b) modified cerebral oxygen consumption (ModcerbVO2), and (c) cerebral fractional tissue oxygen extraction (%) in infants on days 1–3 of postnatal life. Black bars represent infants not exposed to MgSO4 and open bars represent infants exposed to antenatal MgSO4. For panel b, *P = 0.01. For panel c, *P < 0.05, **P = 0.01, §P < 0.01.
A significant interaction effect for time and MgSO4 exposure was observed for modified cerebral oxygen consumption ( Figure 2b , P = 0.04). On post-hoc analysis modified cerebral oxygen consumption was significantly lower within 24 h of age in those infants exposed to MgSO4 antenatally compared to the nonexposed group (P = 0.01). No significant difference between the groups was seen at either 48 or 72 h of age. A similar interaction effect between postnatal age and MgSO4 was seen for cFTOE ( Figure 2c , P = 0.03). On post-hoc analysis, cFTOE was significantly lower in those infants exposed to antenatal MgSO4 within 24 h of delivery (P = 0.01). This difference between the groups was no longer evident by 48 h of age ( Figure 2b ). Further, in the nonexposed group, cFTOE was significantly lower on day 2 (P < 0.01) and day 3 (P = 0.01) compared to day 1 of life, a temporal change that was not observed in the MgSO4 exposed infants. Regression modeling indicated no significant dose-dependent relationship between total magnesium sulfate dose and any systemic or cerebral hemodynamic variable.
Discussion
In the current study, preterm infants <30 wk gestation exposed to antenatal MgSO4 for neuro-protection had significantly lower cFTOE than those not exposed to antenatal MgSO4 but similar measures of systemic and cerebral hemodynamics including mean blood pressure, right ventricular output and total internal carotid blood flow. Interestingly, this difference was confined to the first 24 h of life. With tissue oxygen extraction a dynamic variable primarily determined by oxygen consumption in the context of prevailing oxygen delivery, this data would suggest that one mechanism of action for MgSO4 in the very preterm newborn is a reduction in cerebral metabolic demand and therefore cFTOE. As elevated cFTOE in the immediate newborn period is predictive of early neonatal brain injury (15), the alteration in the balance of cerebral oxygen delivery and consumption resulting in reduced cFTOE may contribute to the neuro-protective actions of MgSO4. However, the lack of a linear relationship between any of the systemic and cerebral hemodynamic variables and MgSO4 dose received suggests a higher cumulative dose may not provide a greater degree of neuro-protection.
The majority of clinical studies investigating neonatal systemic and cerebral hemodynamic effects of MgSO4 have been in the setting of MgSO4 used as an antihypertensive for pregnancy-induced hypertension or as a tocolytic for threatened preterm labor (9,11,19). These studies have reported conflicting results, with reduced (11), unchanged (19), and increased CBF velocities and cerebral vascular resistance in the postnatal period (9). The discrepancy in these findings may relate differences in gestational age of preterm infants investigated and the dose of MgSO4 administered. For instance, the loading (9) and continuous infusion dose (19) of antenatal MgSO4 for tocolysis is significantly higher than that used for neuro-protection in the current study. With elevated neonatal circulating magnesium levels known to persist beyond the initial transition to postnatal life (20), exposure to a lower total MgSO4 dose antenatally, with subsequent differences in neonatal plasma magnesium levels in the first few days of life, may also explain our observation that the difference in cFTOE was confined to the first 24 h of postnatal life.
While magnesium results in vasodilatation and reduced vascular reactivity (21), our data are consistent with the sole study of cardiovascular function following MgSO4 use for neuro-protection in infants of a comparable gestational age (12), with no differences in right ventricular output or mean arterial blood pressure observed. Further, we observed no differences in total internal carotid blood flow between the MgSO4 exposed and nonexposed infants, suggesting this therapy does not impact upon CBF and oxygen delivery.
There is little data focusing on alterations in cerebral oxygen consumption following antenatal MgSO4 exposure in preterm infants. The current study is, however, supported by animal studies, where a temporary reduction in cerebral oxygen consumption not associated with any alteration in CBF has been described in fetal sheep (17). Studies of preterm infants born to mothers with pregnancy-induced hypertension treated with antihypertensive medications, including MgSO4, have also reported reduced cFTOE in the first 24 h of life (18). The generalization of this latter study to preterm infants of normotensive mothers, however, is limited, given that pregnancy induced hypertension results in alterations in placental blood flow (22), and both fetal and neonatal circulations (23,24). For instance, CBF may be greater in infants with evidence of brain-sparing in pregnancies complicated by pregnancy induced hypertension as a result of changes in fetal cerebral vascular resistance (23). To avoid the potential confounding effects of maternal hypertension in pregnancy on neonatal cerebral oxygen delivery and consumption, we excluded mothers who received any hypertensive medications, including MgSO4. However, our observation of a significantly lower cFTOE in those preterm infants exposed to MgSO4 purely for neuro-protection is consistent with this previous report (18), and supports MgSO4-induced changes to cerebral oxygen kinetics.
While focusing on cerebral oxygen kinetics following exposure to antenatal MgSO4, this study did not aim to characterize the mechanisms through which cerebral oxygen consumption and therefore extraction was altered. It is known that MgSO4 rapidly crosses the placenta (25) and fetal blood brain barrier (26) blocking n-methyl-d-aspartate receptors (27) and glutamate receptors (28), receptors critically involved in neuronal death during hypoxic–ischemic injury. Whether these actions result in reduced neuronal excitation remains open to question (29). Recent evidence also supports a role for MgSO4 in immunomodulation with in vitro exposure of neonatal monocytes to clinically relevant doses of MgSO4 producing a reduction in both constitutive and toll-like receptor-stimulated TNFα and IL-6 gene and protein expression (8). Animal data indicate that neonatal cerebral oxygen consumption is elevated following exposure to in utero inflammation (30). It is therefore possible that protection from inflammatory processes conferred by MgSO4 could manifest as reduced cerebral oxygen consumption and cFTOE. However, further investigation is required of the mechanisms of MgSO4 action, particularly in light of a recent long-term follow-up study that reported no significant neuro-developmental benefit at school age of antenatal MgSO4 exposure (31).
There are limitations to the current study. With antenatal MgSO4 a proven antenatal therapy for neuro-protection (3), we could not randomize women presenting in preterm labor to receive MgSO4 or not. While those in the nonexposed group did not receive antenatal MgSO4 as a result of rapid delivery following presentation, there was no difference between the groups for the underlying etiology of their preterm delivery or the physiological stability of the infants following birth. With respect to the determination of cerebral oxygen delivery and consumption, the NIRS data was derived from a single sensor and CBF inferred from total internal carotid blood flow. However, NIRS-derived cFTOE varies minimally between regions of the brain (32) and the current data are consistent with frequency domain NIRS measurements from multiple regions of the brain (33). Further, episodic sampling of dynamic measures, such as total internal carotid blood flow, may result in over-interpretation, particularly, if the duration and severity of adverse oxygen handling varies between infants. However, measurement of total internal carotid flow does provide greater insight into cerebral hemodynamics than measures of maximal or mean cerebral artery velocities commonly reported previously. Due to the in vivo nature of the current study, it was impossible to investigate the underlying mechanistic pathways relating antenatal MgSO4 to reduced cerebral oxygen consumption and cFTOE. Further, while this study identified a lower incidence of P/IVH in the MgSO4-exposed group, we acknowledge that the study was not designed to assess this outcome and is there for under-powered to adequately address this question. Nonetheless this finding is consistent with previous reports of reduced rates of P/IVH following antenatal MgSO4 exposure (4).
In summary, antenatal exposure to MgSO4 for neuro-protection was associated with reduced cerebral oxygen consumption and cFTOE in very preterm infants without alterations in systemic or cerebral hemodynamics. While maintenance of adequate oxygen delivery while avoiding restricted oxygen consumption is critically important in the preterm newborn, this data highlights the importance of considering both sides of the oxygen delivery-consumption relationship in understanding antecedents to acquired brain injury. While the exact mechanism/s through which MgSO4 exerts a neuro-protective effect remain unknown, the current data suggest that reduced cerebral metabolic load may contribute to this beneficial action.
Methods
Study Participants
In this observational study, preterm newborns ≤30 wk gestational age, admitted to the neonatal intensive care unit of the Women’s and Children’s Hospital, Adelaide were recruited. Exclusion criteria included maternal use of antihypertensive medications, including MgSO4, for essential hypertension or pregnancy-induced hypertension, and those infants with life threatening congenital abnormalities or congenital heart disease. Clinical characteristics were recorded from the medical records. Antenatal exposure to MgSO4 for neuro-protection was defined as maternal administration of a 4 g MgSO4 loading dose ± 1 g MgSO4 per hour for a maximum of 24 h prior to delivery (34). No women received multiple courses of MgSO4. The presence of a significant patent ductus arteriosus was defined as echocardiographic measurement of ductal diameter >1.4 mm with bi-directional or left to right shunt. Cranial ultrasounds were performed on days 1 and 3 of life with P/IVH defined as per Papile (35). All infants received a 20 mg/kg-loading dose of intravenous caffeine on day 1 of life prior to a daily 10 mg/kg daily maintenance dose. The institutional human research ethics committee approved the study and parental consent was obtained for each newborn prior to inclusion.
Cerebral Oxygen Delivery and Consumption
Oxygen saturation was maintained within a target band (85–95%) and pCO2 within the range of 45–55 mmHg. NIRS and cranial ultrasound studies were performed within 24 h of birth and repeated at 48 and 72 h of life. NIRS and cerebral ultrasound were not performed within 2 h of clinical interventions that are known to alter cerebral oxygen supply and extraction, including administration of surfactant (36), indomethacin/ibuprofen (37), and caffeine (38).
Tissue oxygen index (TOI) and systemic arterial saturation (SaO2) were measured by NIRS (Hamamatsu NIRO-200, Hamamatsu Photonics K. K Hamamatsu City, Japan) and co-oximetry as described previously (15). Briefly, the sensor was placed on the right fronto-temporal region and NIRS data and contemporaneous SaO2 was captured at 1 s intervals. A 10-min epoch of stable NIRS and SaO2 data (from a 30-min recording period) were averaged with TOI, as a surrogate for cerebral venous oxygen saturation (15), and SaO2 values used for the oxygen kinetic equations.
At the end of each NIRS study, internal carotid artery blood flow measured by pulsed-wave Doppler ultrasound measurement of the internal carotid artery using an 8 MHz linear phased-array transducer (Philips iE33 Ultrasound System, Andover, MA) (15) and right and left ventricular output and patency of the ductus arteriosus (including flow direction) were determined by functional echocardiography. An arterial hemoglobin concentration [Hb], lactate, pH, paO2, and paCO2 were measured by co-oximeter (128 wavelength, spectrophotometer Radiometer Copenhagen, ABL 725, Denmark).
Calculations
cFTOE was calculated from the formula: cFTOE = [(((SaO2 – TOI)/SaO2) where SaO2 = systemic arterial saturation (co-oximetry) and TOI was used in place of cerebral venous oxygen saturation (15). Modified cerebral oxygen delivery (mCerbDO2) was calculated from the formula: mCerbDO2 = (CBF × ((1.39× Hb × Hbsat/100) + (0.003 × PaO2)); where total internal carotid blood flow was used as a surrogate of CBF; Hb = Hemoglobin concentration (g/dl); Hbsat= Hemoglobin saturation. Modified cerebral oxygen consumption (mCerbVO2) was calculated according to the Fick principle, i.e., mCerbVO2 = (CBF × (SaO2 – TOI)) where TICF was used as a surrogate of CBF and TOI was used as a surrogate of cerebral venous oxygen saturation (15).
Statistical Analysis
Neonatal demographic data were compared using ANOVA. Frequency data were analyzed using Fishers exact test. Differences in cerebral hemodynamic and oxygenation measures according to MgSO4 exposure were assessed using repeated measures ANOVA with post-hoc analysis by paired t-test comparisons using the Bonferroni correction. Regression analyses were conducted to assess the associations between total magnesium sulfate dose and all hemodynamic variables, including gestational age and hemoglobin in the regression models. Statistical analyses were performed with SPSS v20.0 (SPSS, Chicago, IL) with a P value < 0.05 considered significant.
Statement of Financial Support
Financial support for this study was provided by a Channel 7 Research Foundation Project Grant, Australia and a Women’s and Children’s Hospital Research Foundation Project Grant, Adelaide, Australia.
Disclosure
The authors have no potential /perceived conflicts of interest to disclose.
References
Fanaroff AA, Stoll BJ, Wright LL, et al.; NICHD Neonatal Research Network. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol 2007;196:147.e1–8.
Kuban KC, Leviton A, Pagano M, Fenton T, Strassfeld R, Wolff M. Maternal toxemia is associated with reduced incidence of germinal matrix hemorrhage in premature babies. J Child Neurol 1992;7:70–6.
American College of O, Gynecologists Committee on Obstetric P, Society for Maternal-Fetal M. Committee Opinion No. 455: Magnesium sulfate before anticipated preterm birth for neuroprotection. Obstet Gynecol 2010;115:669–71.
Petrova A, Mehta R. Magnesium sulfate tocolysis and intraventricular hemorrhage in very preterm infants. Indian J Pediatr 2012;79:43–7.
Doyle LW, Crowther CA, Middleton P, Marret S, Rouse D. Magnesium sulphate for women at risk of preterm birth for neuroprotection of the fetus. Cochrane Database Syst Rev 2009:CD004661.
Rantone TH, Grönlund JU, Jalonen JO, et al. Comparison of the effects of antenatal magnesium sulphate and ritodrine exposure on circulatory adaptation in preterm infants. Clin Physiol Funct Imaging 2002;22:13–7.
Antonov SM, Johnson JW. Permeant ion regulation of N-methyl-D-aspartate receptor channel block by Mg(2+). Proc Natl Acad Sci U S A 1999;96:14571–6.
Suzuki-Kakisaka H, Sugimoto J, Tetarbe M, Romani AM, Ramirez Kitchen CM, Bernstein HB. Magnesium sulfate increases intracellular magnesium reducing inflammatory cytokine release in neonates. Am J Reprod Immunol 2013;70:213–20.
Imamoglu EY, Gursoy T, Karatekin G, Ovali F. Effects of antenatal magnesium sulfate treatment on cerebral blood flow velocities in preterm neonates. J Perinatol 2014;34:192–6.
Belfort MA, Saade GR, Moise KJ Jr . The effect of magnesium sulfate on maternal and fetal blood flow in pregnancy-induced hypertension. Acta Obstet Gynecol Scand 1993;72:526–30.
Shokry M, Elsedfy GO, Bassiouny MM, Anmin M, Abozid H. Effects of antenatal magnesium sulfate therapy on cerebral and systemic hemodynamics in preterm newborns. Acta Obstet Gynecol Scand 2010;89:801–6.
Paradisis M, Osborn DA, Evans N, Kluckow M. Randomized controlled trial of magnesium sulfate in women at risk of preterm delivery-neonatal cardiovascular effects. J Perinatol 2012;32:665–70.
Greisen G, Børch K. White matter injury in the preterm neonate: the role of perfusion. Dev Neurosci 2001;23:209–12.
Altman DI, Perlman JM, Volpe JJ, Powers WJ. Cerebral oxygen metabolism in newborns. Pediatrics 1993;92:99–104.
Balegar KK, Stark MJ, Briggs N, Andersen CC. Early cerebral oxygen extraction and the risk of death or sonographic brain injury in very preterm infants. J Pediatr 2014;164:475–80.e1.
Noori S, McCoy M, Anderson MP, Ramji F, Seri I. Changes in cardiac function and cerebral blood flow in relation to peri/intraventricular hemorrhage in extremely preterm infants. J Pediatr 2014;164:264–70.e1–3.
Ayromlooi J, Desiderio DM, Tobias M, Berg P. Effect of magnesium sulfate on maternal and fetal hemodynamics and fetal brain function and metabolism. Pediatr Pharmacol (New York) 1982;2:305–15.
Verhagen EA, Kooi EM, van den Berg PP, Bos AF. Maternal antihypertensive drugs may influence cerebral oxygen extraction in preterm infants during the first days after birth. J Matern Fetal Neonatal Med 2013;26:871–6.
Pezzati M, Giani T, Gambi B, et al. Influence of maternal magnesium sulphate and ritodrine treatment on cerebral blood flow velocity of the preterm newborn. Acta Obstet Gynecol Scand 2001;80:818–23.
Mittendorf R, Dammann O, Lee KS. Brain lesions in newborns exposed to high-dose magnesium sulfate during preterm labor. J Perinatol 2006;26:57–63.
Euser AG, Cipolla MJ. Magnesium sulfate for the treatment of eclampsia: a brief review. Stroke 2009;40:1169–75.
Fairlie FM. Doppler flow velocimetry in hypertension in pregnancy. Clin Perinatol 1991;18:749–78.
Rasmussen K. Fetal haemodynamics before and after treatment of maternal hypertension in pregnancy. Dan Med Bull 1987;34:170–2.
Stark MJ, Clifton VL, Wright IM. Neonates born to mothers with preeclampsia exhibit sex-specific alterations in microvascular function. Pediatr Res 2009;65:292–5.
Hallak M, Berry SM, Madincea F, Romero R, Evans MI, Cotton DB. Fetal serum and amniotic fluid magnesium concentrations with maternal treatment. Obstet Gynecol 1993;81:185–8.
Hallak M, Cotton DB. Transfer of maternally administered magnesium sulfate into the fetal compartment of the rat: assessment of amniotic fluid, blood, and brain concentrations. Am J Obstet Gynecol 1993;169(2 Pt 1):427–31.
McDonald JW, Silverstein FS, Johnston MV. Magnesium reduces N-methyl-D-aspartate (NMDA)-mediated brain injury in perinatal rats. Neurosci Lett 1990;109:234–8.
Espinoza MI, Parer JT. Mechanisms of asphyxial brain damage, and possible pharmacologic interventions, in the fetus. Am J Obstet Gynecol 1991;164(6 Pt 1):1582–9; discussion 1589–91.
de Haan HH, Gunn AJ, Williams CE, Heymann MA, Gluckman PD. Magnesium sulfate therapy during asphyxia in near-term fetal lambs does not compromise the fetus but does not reduce cerebral injury. Am J Obstet Gynecol 1997;176(1 Pt 1):18–27.
Andersen CC, Pillow JJ, Gill AW, et al. The cerebral critical oxygen threshold of ventilated preterm lambs and the influence of antenatal inflammation. J Appl Physiol (1985) 2011;111:775–81.
Doyle LW, Anderson PJ, Haslam R, Lee KJ, Crowther C ; Australasian Collaborative Trial of Magnesium Sulphate (ACTOMgSO4) Study Group. School-age outcomes of very preterm infants after antenatal treatment with magnesium sulfate vs placebo. JAMA 2014;312:1105–13.
Wijbenga RG, Lemmers PM, van Bel F. Cerebral oxygenation during the first days of life in preterm and term neonates: differences between different brain regions. Pediatr Res 2011;70:389–94.
Grant PE, Roche-Labarbe N, Surova A, et al. Increased cerebral blood volume and oxygen consumption in neonatal brain injury. J Cereb Blood Flow Metab 2009;29:1704–13.
SA Maternal & Neonatal Clinical Network. Magnesium sulphate for neuroprotection of the fetus in women at risk of preterm birth. South Australian Perinatal Practice Guidelines. South Australia: Department of Health, Government of South Australia, 2012.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978;92:529–34.
Skov L, Ryding J, Pryds O, Greisen G. Changes in cerebral oxygenation and cerebral blood volume during endotracheal suctioning in ventilated neonates. Acta Paediatr 1992;81:389–93.
Van Bel F, Van de Bor M, Stijnen T, Baan J, Ruys JH. Cerebral blood flow velocity changes in preterm infants after a single dose of indomethacin: duration of its effect. Pediatrics 1989;84:802–7.
Hoecker C, Nelle M, Poeschl J, Beedgen B, Linderkamp O. Caffeine impairs cerebral and intestinal blood flow velocity in preterm infants. Pediatrics 2002;109:784–7.
Author information
Authors and Affiliations
Corresponding author
PowerPoint slides
Rights and permissions
About this article
Cite this article
Stark, M., Hodyl, N. & Andersen, C. Effects of antenatal magnesium sulfate treatment for neonatal neuro-protection on cerebral oxygen kinetics. Pediatr Res 78, 310–314 (2015). https://doi.org/10.1038/pr.2015.96
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2015.96
This article is cited by
-
Blood pressure values and hypotension management in extremely preterm infants: a multi-center study
Journal of Perinatology (2022)