Abstract
Cerebral perfusion and its relation with systemic circulation in extremely LBW (ELBW) infants in the early neonatal period are not well understood. The cerebral tissue oxygenation index (TOI) and cerebral fractional tissue oxygen extraction (FTOE) were monitored in stable 16 ELBW infants (GA <29 wk) using near-infrared spectroscopy (NIRS) at 3–6, 12, 18, 24, 36, 48, and 72 h after birth. The left ventricular end-systolic wall stress (ESWS), left ventricular ejection fraction (LVEF), left ventricular cardiac output (LVCO), and superior vena cava (SVC) flow were also measured simultaneously using echocardiography. The ESWS increased till 18 h and then decreased; LVEF, LVCO, and SVC flow decreased till 12 h and increased thereafter. The TOI decreased till 12 h and correlated with SVC flow; FTOE increased until 12 h and then decreased. These changes in variables of NIRS and echocardiographic measurements contrasted to changes in mean arterial blood pressure (MABP), which showed trends of continuous and gradual increase after birth. We conclude that even stable ELBW infants undergo evident transitional changes in cerebral oxygenation and perfusion in the early postnatal period, which may reflect changes in cardiac function and cardiac output.
Similar content being viewed by others
Main
The survival rate of extremely LBW (ELBW) infants has markedly improved owing to advances in medical technology and patient management as well as better understanding of neonatal pathophysiology. However, cerebral complications remain a major problem causing long-term neurodevelopmental sequelae (1). Intraventricular hemorrhage (IVH) is known to occur in ELBW infants and is attributable to multiple pathogenetic factors including vulnerability of the vasculature and fragility of the germinal matrix of the brain (2). Hypotension and hypoperfusion of the brain during the immediate postnatal period have been reported to be related with cerebral damage in sick preterm infants (3–5). Kluckow and Evans (6) proposed Doppler echocardiographic measurement of blood flow in the superior vena cava (SVC) as a consistent marker of upper body perfusion, including cerebral blood flow (CBF). They reported that sick preterm infants who developed IVH experienced a period of low SVC flow within the first 48 h of life (7).
Although some recent studies have found changes in cerebral oxygenation in very LBW (VLBW) infants (8,9) using near-infrared spectroscopy (NIRS), there have been no studies on longitudinal and detailed assessment of cerebral perfusion in ELBW infants in the early postnatal period. Furthermore, the relationship between cerebral perfusion, systemic perfusion, and arterial blood pressure during the immediate postnatal period is determined by multiple factors and has not been fully understood. The aim of this study was to characterize in detail the cerebral oxygenation and oxygen extraction, as determined by NIRS, and systemic blood flow and cardiac function, as evaluated by echocardiography, in ELBW infants during the early postnatal period.
METHODS
Subjects.
ELBW infants (birth weight <1000 g) who were born at a GA of <29 wk and admitted to the NICU of Tokyo Medical University Hospital between May 1, 2006, and December 31, 2008, were included in this study. The inclusion criteria of the subjects were ELBW infants 1) without anomalies and who were not small for GA (birth weight < the 10th percentile for GA), 2) who did not develop IVH and/or periventricular leukomalacia (PVL), as diagnosed by echoencephalography, 3) who did not show severe electrolyte abnormalities or metabolic acidosis during the study, 4) who were kept in stable respiratory condition with or without mechanical ventilation; SpO2 >90% and Pco2 range between 30 and 50 mm Hg during the study period, and 5) whose mean arterial blood pressure (MABP) were maintained at a level above the infant's GA in weeks within 12 h after birth. Infants who showed severe hypotension (MABP below the above-mentioned level despite volume expansion and inotropic support with dopamine and/or dobutamine >10 μg · kg−1 · min−1) were excluded. Informed consent was obtained from the parents of all the infants. The study was approved by the Research Ethics Committee of Tokyo Medical University.
NIRS measurement.
The oxygenated Hb (O2Hb), deoxygenated Hb (HHb), and total Hb (cHb = O2Hb + HHb) levels and the tissue oxygenation index (TOI = O2Hb/cHb × 100) were measured using NIRS (NIRO-200/300; Hamamatsu Photonics KK, Shizuoka, Japan). The optode was placed in the frontotemporal region of the head with the sensors at 3 cm distance (10). Measurements were taken 3–6, 12, 18, 24, 36, 48, and 72 h after birth, and each measurement session lasted for 30 min. The results were recorded and stored as graphs and numerical values in a personal computer. The signals were sampled at 2.0 s intervals, and the TOI was expressed as a median of 900 values (30/min × 30 min) for 30 min for each measurement session. The cerebral fractional tissue oxygen extraction (FTOE) was then calculated from the TOI and oxygen saturation (SpO2) values [FTOE = (SpO2 − TOI)/SpO2] (11).
Echocardiographic measurement.
All 16 infants underwent serial echocardiographic examinations at the same time as the NIRS measurements. All scans were performed by a single examiner (T.T.) to avoid the error between observers using Hewlett-Packard SONOS 2000 equipped with a 7.5-MHz transducer (12). The end-systolic wall stress (ESWS) of the left ventricle (LV) was measured as an index of LV afterload in the M mode echocardiograms taken in the parasternal long-axis view according to the method by Colan et al. (13). The LV ejection fraction (LVEF) measured as an index of systolic function of the LV in the M mode echocardiograms taken in the parasternal long-axis view according to the method by Sahn et al. (14). Doppler volumetric measurements of the left ventricular cardiac output (LVCO) and SVC flow were measured by the methods by Alverson et al. (15) and Kluckow and Evans (6), respectively. Based on these echocardiographic data obtained at 3–6 h after birth, treatment with volume expansion and/or inotrope administration was decided.
Measurement of other variables.
Blood was collected from an arterial line in 11 infants and by heel lance in five infants. The pH was measured with the blood from the umbilical cord at birth or with the first blood sample collected from an infant after birth. The MABP was measured either directly (in 11 infants with arterial lines) or indirectly (oscillometric technique with an inflatable cuff BSN-2303; Nihon Kohden Corporation, Tokyo, Japan) in five infants (16). The Pco2, hematocrit (Ht) values, and indirect MABP were measured after NIRS and echocardiographic measurement. The heart rate (HR) and the SpO2 in the right upper arm were continuously measured using a pulse oximeter (Nellcor Pulse Oximeter N-200; Tyco Healthcare Japan, Tokyo, Japan). The HR, direct MABP, and SpO2 were monitored and recorded at the same time as the NIRS measurement by a neonatal monitoring system (BSM-2300; Nihon Kohden Corporation, Tokyo, Japan). The data were stored in a personal computer, and median values were calculated over the measurement period.
Respiratory and cardiovascular support.
Infants were kept in a stable condition on mechanical ventilation or nasal continuous positive airway pressure (CPAP; Infant Flow Nasal CPAP System, Cardinal Health, OH), aiming for a Pco2 range between 30 and 50 mm Hg during the study period. The MABP was aimed to maintain a level above the infant's GA in weeks (17). When an infant was hypotensive according to the above criteria, they were treated first with volume expansion (10 mL · kg−1 normal saline), followed by dobutamine infusion (5–10 μg · kg−1 · min−1) depending on patient's response. When the blood pressure (BP) still remained low despite these treatments, dopamine (5–10 μg · kg−1 · min−1) was administered. Indomethacin (0.2–0.25 mg/kg) was i.v. administered at 12–24-h intervals starting at 18 h after birth to infants with echocardiographically proven significant patent ductus arteriosus (PDA).
Statistics.
Statistical analyses were performed using the computer package SPSS for Windows (SPSS Japan, Tokyo, Japan). The GA, birth weight, and blood pH of the 16 infants were expressed as “mean (SD).” Serial data obtained using NIRS, echocardiography, and physical examination at different time points were compared using repeated-measures ANOVA, followed by Bonferroni's multiple comparison tests. Pearson's correlation coefficients and simple linear regression analysis were used to determine the relationships among the MABP, SpO2, Pco2, Ht, ESWS, LVEF, LVCO, SVC flow, TOI, and FTOE. p < 0.05 was considered statistically significant.
RESULTS
A total of 16 infants were included in the study. No infants developed PVL, as determined by MRI at the time of discharge. The mean (SD) of GAs of the infants was 25.2 wk (1.6 wk), range, 23–28 wk; the mean birth weight was 749 g (252 g), range, 551–998 g; the mean initial blood pH was 7.30 (0.20). Ten infants received antenatal maternal corticosteroids. Ten infants received mechanical ventilation and three required nasal CPAP. Ten infants received infusion of i.v. volume expander for circulatory support. Six received inotropic support with dobutamine (2–5 μg · kg−1 · min−1) only and three with dopamine (5 μg · kg−1 · min−1) in addition to dobutamine. Five infants received indomethacin for treatment of PDA (Table 1).
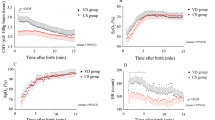
There were no significant changes in HR (p = 0.59), SpO2 (p = 0.41), Ht value (p = 0.16), or Pco2 (p = 0.31) during the study period (Fig. 1). In contrast, the MABP (p < 0.05) showed trends of gradual increase after birth (significant increase from 3–6 to 12 h after birth; Fig. 1).
There were significant changes in the ESWS (p < 0.05), LVEF (p < 0.05), LVCO (p < 0.05), and SVC flow (p < 0.05) in the 72 h (Fig. 2). The ESWS (g · cm−1) increased until 18 h [34.1 (8.0)] and showed trends of decrease after 24 h. The LVEF (%) decreased until 12 h [57.2% (6.7)] and showed trends of gradual increase after 24 h. Both LVCO (ml · kg−1 · min−1) and SVC flow (ml · kg−1 · min−1) decreased until 12 h [166 (35) and 65.0 (24.3), respectively] and showed trends of increase after 18 h.
Both TOI (p < 0.05) and FTOE (p = 0.028) showed significant changes in the 72 h (Fig. 3). The TOI (%) was decreased until 12 h [57.6 (6.9)] and showed trends of gradual increase after 18 h. The FTOE increased until 12 h [0.38 (0.10)] and showed trends of gradual decrease after 18 h. There was a positive correlation between the TOI and SVC flow (n = 16; r = 0.33; p = 0.01) and the SVC flow and LVCO (n = 16; r = 0.66; p < 0.01) and a negative correlation between the TOI and FTOE (n = 16; r = 0.94; p < 0.01; Fig. 4).
DISCUSSION
This is the first report that studied indicators of cerebral perfusion and systemic perfusion and their relationship using NIRS and echocardiography in ELBW infants during the first 72 h of life. The TOI and SVC flow, which are indicators of cerebral oxygenation and upper body perfusion, respectively, showed significant changes in the early postnatal period, although the physiological data such as HR, SpO2, Ht value, and Pco2 in the subjects were stable. Both TOI and SVC flow decreased within 24 h after birth and then increased which corresponded with a decrease in LVEF and LVCO with an increase in ESWS but not with BP. However, the FTOE was negatively correlated with TOI and increased within 24 h after birth.
There have been several reports on ESWS, LVEF, and LVCO in neonates by echocardiography (15,18,19). However, only a few of them have conducted detailed measurements of these parameters in preterm infants soon after birth. Murase et al. (20) reported values on serial Doppler echocardiographic measurements of the LVCO, evaluating systolic function of the LV, in critically ill VLBW infants from 3 h to 28 d after birth. They found that values of these parameters decreased till 12 h, then increased after 24 h, and those values were significantly lower in the group of more preterm infants. Infants in our study showed a similar changing pattern of LVEF and LVCO to those in their report, although we studied clinically more stable ELBW infants with minimal fluctuations in HR, Ht value, SpO2, or Pco2 than their study. We speculate that even apparently stable ELBW infants undergo a period of temporary reduction in LVEF and LVCO within 12 h of birth probably because of limited capacity of immature myocardium to adapt to the perinatal circulatory change. That might be why the postnatal changing pattern of LVEF and LVCO in ELBW infants in this study was similar to that in more ill but less preterm infants in other studies (20,21). This study also revealed that the changes in LVEF and LVCO were associated with the change in ESWS (representing LV afterload, i.e. the peripheral vascular resistance) (22). It can be speculated that the findings of our study indicate that fluctuations in the LVEF and LVCO in preterm infants reflect immaturity of perinatal circulatory adaptation, involving immature myocardial contractility, during the transition from fetal to extrauterine life, which is likely to be associated with an increase in the peripheral vascular resistance. Impairment of right ventricular (RV) cardiac function because of increased RV afterload after positive-pressure ventilation may also have contributed to the observed decrease in LVCO. Reduction in the RV output may result in a concordant reduction in the LVCO because the circulatory system of the right and left sides of the heart are connected in series (17). Findings of this study suggest that in ELBW infants on mechanical ventilation, the systemic circulation is vulnerable and can be easily affected during the transition from fetal to extrauterine life.
NIRS measures the O2Hb, HHb, and cHb levels and the TOI in noninvasive manner. The TOI is determined by oxygenation status and metabolic state. Because oxygen delivery is primarily related to the oxygen content of the blood and to the amount of blood flowing to a given organ (23), changes in TOI are determined mainly by changes in Hb levels, SpO2, blood flow, and cerebral metabolic rate of oxygen utilization. For this reason, in infants with stable Ht and SpO2 values, changes in the TOI mainly reflect changes in the CBF (24,25). Naulaers et al. (9) reported that the median TOI showed an increase over the first 3 d of life in 15 stable VLBW infants and speculated that this increase in the TOI indicated an increase in the CBF during this period. This study revealed that in ELBW infants, the TOI of the brain markedly decreases on the first day of life and then increases. Changes in the TOI, which have not been seen in previous studies, may have been observed in this study because the subjects were more immature and the measurements were started earlier after birth (8,9). The findings of this study showed that even stable ELBW infants are at a risk of developing tissue deoxygenation and hypoperfusion within the first 24 h of birth.
The changing pattern of SVC flow in our study was similar to that of TOI measured by NIRS (i.e. both parameters decreased until 12 h and increased after 18 h of birth), probably because the TOI value is determined mainly by venous oxygen saturation, especially of the internal jugular vein, which is located upstream of the SVC (26). The value of LVCO is influenced by shunt flow through the PDA (19). Therefore, in the clinical setting, determination of both the TOI and SVC flow provides useful information on cerebral circulation, including the status of cerebral oxygenation and perfusion in the early postnatal period.
The cerebral fractional oxygen extraction (FOE), which represents the ratio of oxygen uptake to oxygen delivery (27), is another indicator of cerebral oxygenation. Recently, Naulaers et al. (11) showed a close correlation between the FTOE measured by NIRS and the actual FOE in piglets and concluded that FTOE is likely to provide important information on oxygenation status of the brain continuously. In our study, the TOI decreased and the FTOE increased significantly, which corresponded with the timing of impaired cardiac function and cardiac output during the first 24 h after birth. Increased cerebral FTOE reflects increased oxygen extraction by the brain tissue and suggests that the oxygen consumption exceeds the rate of oxygen delivery. Thus, increased FTOE may indicate a compensatory mechanism for the decreased cerebral tissue oxygenation associated with reduced CBF and reduced oxygen delivery (28). Continuous measurement of TOI and FTOE using NIRS may be useful by providing noninvasive and continuous monitoring of both cerebral oxygenation and oxygen extraction in ELBW infants.
In the management of VLBW infants, systemic BP is one of the commonly used indicators of systemic perfusion, because there is no easy way to determine cardiovascular function in routine clinical practice. It is generally accepted that MABP should be maintained above a certain level to minimize the risk of hypoperfusion. Some clinicians recommend that the MABP should not be allowed to fall <30 mm Hg in sick infants (3,19) and others recommend to maintain the MABP above the value of an infant's GA in weeks (17), although there is little evidence to support this protocol. In this study, in all 16 infants, the MABP was initially <30 mm Hg and the value of GA in weeks but then gradually increased. However, the changes in MABP were not closely related to those in the TOI, SVC flow, and LVCO. The results of this study are compatible with those of previous studies in that the MABP is not closely related to the CBF measured by NIRS (8,29,30), the SVC flow (31), or the LVCO (32,33) during the immediate postnatal period. However, Munro et al. (34) and Wong et al. (25) showed a strong correlation between MABP and CBF or TOI in clinically ill preterm infants with disrupted cerebral autoregulation. One possible explanation for these apparently contradictory results is that only infants with severe hypotension (who were excluded from our study) might show correlations of MABP with CBF and TOI. Another possibility may be related to different time window when measurements were performed in these studies. We started measuring parameters of cerebral and systemic perfusion earlier than the previous studies. However, these previous studies have not examined infants within 12 h after birth. During this early period, most ELBW infants have large PDA with massive shunt flow (left to right, right to left, or bidirectional). For example, LVCO in infants with significant LR shunt through large PDA may double compared with those without PDA, which influence CBF because of a stealing shunt flow from the descending aorta to the main pulmonary artery (35,36). However, the direction and the amount of the shunt flow often do not depend on the BP but on the pulmonary vascular resistance, which in turn, depends on the respiratory status. Finally, in our study, the NIRS data were averaged for long periods and may have missed correlations that might exist in dynamic data. Taking all these factors into consideration, we think that BP remains a useful parameter in evaluating systemic perfusion in the management of ELBW infants, especially for those with severe hypotension.
In conclusion, we longitudinally measured and assessed cerebral perfusion, systemic perfusion, and their relationships by studying variables of NIRS and echocardiographic measurements in ELBW infants during the immediate postnatal period. We demonstrated that even stable ELBW infants have reduced cerebral oxygenation and perfusion immediately after birth, which was not closely associated with BP changes but was more likely to reflect low cardiac output because of decreased LV contractility following increased peripheral vascular resistance. These findings may indicate inadequate hemodynamic adaptation during the transition from fetal to extrauterine life.
Abbreviations
- CBF:
-
cerebral blood flow
- CPAP:
-
continuous positive airway pressure
- ELBW:
-
extremely LBW
- ESWS:
-
left ventricular end-systolic wall stress
- FTOE:
-
cerebral fractional tissue oxygen extraction
- HR:
-
heart rate
- Ht:
-
hematocrit
- IVH:
-
intraventricular hemorrhage
- LVCO:
-
left ventricular cardiac output
- LVEF:
-
left ventricular ejection fraction
- MABP:
-
mean arterial blood pressure
- NIRS:
-
near-infrared spectroscopy
- PDA:
-
patent ductus arteriosus
- SpO2:
-
oxygen saturation
- SVC:
-
superior vena cava
- TOI:
-
tissue oxygenation index
References
Volpe JJ 1998 Neurologic outcome of prematurity. Arch Neurol 55: 297–300
Volpe JJ, Edward B 1989 Neuhauser lecture. Current concepts of brain injury in the premature infant. AJR Am J Roentgenol 153: 243–251
Bada HS, Korones SB, Perry EH, Arheart KL, Ray JD, Pourcyrous M, Magill HL, Runyan W III, Somes GW, Clark FC 1990 Mean arterial blood pressure changes in premature infants and those at risk for intraventricular hemorrhage. J Pediatr 117: 607–614
Meek JH, Tyszczuk L, Elwell CE, Wyatt JS 1999 Low cerebral blood flow is a risk factor for severe intraventricular haemorrhage. Arch Dis Child Fetal Neonatal Ed 81: F15–F18
Osborn DA, Evans N, Kluckow M 2003 Hemodynamic and antecedent risk factors of early and late periventricular/intraventricular hemorrhage in premature infants. Pediatrics 112: 33–39
Kluckow M, Evans N 2000 Superior vena cava flow in newborn infants: a novel marker of systemic blood flow. Arch Dis Child Fetal Neonatal Ed 82: F182–F187
Kluckow M, Evans N 2000 Low superior vena cava flow and intraventricular haemorrhage in preterm infants. Arch Dis Child Fetal Neonatal Ed 82: F188–F194
Soul JS, Hammer PE, Tsuji M, Saul M, Philip J, Bassan H, Limperopoulos C, Disalvo DN, Moore M, Akins P, Ringer S, Volpe JJ, Trachtenberg F, du Plessis AJ 2007 Fluctuating pressure-passivity is common in the cerebral circulation of sick premature infants. Pediatr Res 61: 467–473
Naulaers G, Morren G, Van Huffel S, Casaer P, Devlieger H 2002 Cerebral tissue oxygenation index in very premature infants. Arch Dis Child Fetal Neonatal Ed 87: F189–F192
Takami T, Yamamura H, Inai K, Nishikawa Y, Takei Y, Hoshika A, Nakazawa M 2005 Monitoring of cerebral oxygenation during hypoxic gas management in congenital heart disease with increased pulmonary blood flow. Pediatr Res 58: 521–524
Naulaers G, Meyns B, Miserez M, Leunens V, Van Huffel S, Casaer P, Weindling M, Devlieger H 2007 Use of tissue oxygenation index and fractional tissue oxygen extraction as non-invasive parameters for cerebral oxygenation. A validation study in piglets. Neonatology 92: 120–126
Groves AM, Kuschel CA, Knight DB, Skinner JR 2008 Echocardiographic assessment of blood flow volume in the superior vena cava and descending aorta in the newborn infant. Arch Dis Child Fetal Neonatal Ed 93: F24–F28
Colan SD, Borow KM, Neumann A 1984 Left ventricular end-systolic wall stress-velocity of fiber shortening relation: aload-independent index of myocardial contractility. J Am Coll Cardiol 4: 715–724
Sahn DJ, DeMaria A, Kisslo J, Weyman A 1978 Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation 58: 1072–1083
Alverson DC, Eldridge M, Dillon T, Yabek SM, Berman W Jr 1982 Noninvasive pulsed Doppler determination of cardiac output in neonates and children. J Pediatr 101: 46–50
Spinazzola RM, Harper RG, de Soler M, Lesser M 1991 Blood pressure values in 500- to 750- gram birthweight infants in the first week of life. J Perinatol 11: 147–151
Levene MI, Joint Working Group of the British Association of Perinatal Medicine and the Research Unit of the Royal College of Physicians 1992 Development of audit measures and guidelines for good practice in the management of neonatal respiratory distress syndrome. Arch Dis Child 67: 1221–1227
Igarashi H, Shiraishi H, Endoh H, Yanagisawa M 1994 Left ventricular contractile state in preterm infants: relation between wall stress and velocity of circumferential fiber shortening. Am Heart J 127: 1336–1340
Evans N, Kluckow M 1996 Early determinants of right and left ventricular output in ventilated preterm infants. Arch Dis Child Fetal Neonatal Ed 74: F88–F94
Murase M, Ishida A, Momota T 2002 Serial pulsed Doppler assessment of early left ventricular output in critically ill very low-birth-weight infants. Pediatr Cardiol 23: 442–448
Gill AB, Weindling AM 1993 Echocardiographic assessment of cardiac function in shocked very low birthweight infants. Arch Dis Child 68: 17–21
Kluckow M, Evans N 2001 Low systemic blood flow in the preterm infant. Semin Neonatol 6: 75–84
Weindling AM, Kissack CM 2001 Blood pressure and tissue oxygenation in the newborn baby at risk of brain damage. Biol Neonate 79: 241–245
Elwell CE, Henty JR, Leung TS, Austin T, Meek JH, Delpy DT, Wyatt JS 2005 Measurement of CMRO2 in neonates undergoing intensive care using near infrared spectroscopy. Adv Exp Med Biol 566: 263–268
Wong FY, Leung TS, Austin T, Wilkinson M, Meek JH, Wyatt JS, Walker AM 2008 Impaired autoregulation in preterm infants identified by using spatially resolved spectroscopy. Pediatrics 121: e604–e611
Yoxall CW, Weindling AM, Dawani NH, Peart I 1995 Measurement of cerebral venous oxyhemoglobin saturation in children by near-infrared spectroscopy and partial jugular venous occlusion. Pediatr Res 38: 319–323
Yoxall CW, Weindling AM 1998 Measurement of cerebral oxygen consumption in the human neonate using near infrared spectroscopy: cerebral oxygen consumption increases with advancing gestational age. Pediatr Res 44: 283–290
Kissack CM, Garr R, Wardle SP, Weindling AM 2005 Cerebral fractional oxygen extraction is inversely correlated with oxygen delivery in the sick, newborn, preterm infant. J Cereb Blood Flow Metab 25: 545–553
Miall-Allen VM, de Vries LS, Whitelaw AG 1987 Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child 62: 1068–1069
Younkin DP, Reivich M, Jaggi JL, Obrist WD, Delivoria-Papadopoulos M 1987 The effect of hematocrit and systolic blood pressure on cerebral blood flow in newborn infants. J Cereb Blood Flow Metab 7: 295–299
Groves AM, Kuschel CA, Knight DB, Skinner JR 2008 Relationship between blood pressure and blood flow in newborn preterm infants. Arch Dis Child Fetal Neonatal Ed 93: F29–F32
Kluckow M, Evans N 1996 Relationship between blood pressure and cardiac output in preterm infants requiring mechanical ventilation. J Pediatr 129: 506–512
Pladys P, Wodey E, Beuchee A, Branger B, Betremieux P 1999 Left ventricle output and mean arterial blood pressure in preterm infants during the 1st day of life. Eur J Pediatr 158: 817–824
Munro MJ, Walker AM, Barfield CP 2004 Hypotensive extremely low birth weight infants have reduced cerebral blood flow. Pediatrics 114: 1591–1596
Vanderhaegen J, De Smet D, Meyns B, Van De Velde M, Van Huffel S, Naulaers G 2008 Surgical closure of the patent ductus arteriosus and its effect on the cerebral tissue oxygenation. Acta Paediatr 97: 1640–1644
Lemmers PM, Toet MC, van Bel F 2008 Impact of patent ductus arteriosus and subsequent therapy with indomethacin on cerebral oxygenation in preterm infants. Pediatrics 121: 142–147
Acknowledgements
We thank Dr Keiji Suzuki (Department of Pediatrics, Saitama Medical University) for assistance in preparation of the article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takami, T., Sunohara, D., Kondo, A. et al. Changes in Cerebral Perfusion in Extremely LBW Infants During the First 72 h After Birth. Pediatr Res 68, 435–439 (2010). https://doi.org/10.1203/PDR.0b013e3181f2bd4d
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181f2bd4d
This article is cited by
-
Correlations between near-infrared spectroscopy, perfusion index, and cardiac outputs in extremely preterm infants in the first 72 h of life
European Journal of Pediatrics (2018)