Abstract
Persistent pulmonary hypertension is an important cause of mortality and morbidity in term infants. The lung assist device (LAD) is a novel, pumpless, low-resistance extracorporeal oxygenator to supplement mechanical ventilation. The LAD may be associated with fewer complications compared with conventional extracorporeal membrane oxygenation. The objective was to test the feasibility and efficacy of the LAD in juvenile piglets with hypoxia-induced pulmonary hypertension. Pulmonary hypertension was acutely induced by hypoxia in six 3- to 4-wk-old acutely instrumented and intubated piglets. The LAD was attached between a carotid artery and jugular vein. Gas exchange and hemodynamic variables, including pulmonary arterial pressure (PAP) and cardiac output (CO), were measured. Successful LAD cannulation was achieved without complications in all animals. Extracorporeal shunt flow through the device averaged 18% of CO. The LAD achieved oxygen delivery of 20% of total oxygen consumption. PAP was reduced by 35% from 28 ± 5 to 18 ± 4 mm Hg (p < 0.05) and systemic Pao2 increased by 33% from 27 ± 2 to 36 ± 4 mm Hg (p < 0.05). Other hemodynamic variables remained stable. The novel LAD shows feasibility and efficacy in improving gas exchange and reducing PAPs in a juvenile animal model of hypoxia-induced pulmonary hypertension.
Similar content being viewed by others
Main
Persistent pulmonary hypertension of the newborn (PPHN) is a serious clinical problem, affecting approximately 0.2% of liveborn infants, and it is associated with high morbidity and mortality (1). PPHN is characterized by delayed relaxation of the pulmonary vascular bed. The high pulmonary vascular resistance causes pulmonary hypertension, leading to right-to-left shunting resulting in severe hypoxemia (2). The mainstay of management is supportive care with mechanical ventilation in addition to adjunctive therapies, such as high-frequency ventilation, surfactant therapy, inhaled nitric oxide, and extracorporeal membrane oxygenation (ECMO) (3–6). Because of serious inherent risks, such as coagulopathy and the need for systemic anticoagulation, which predisposes to systemic and intracranial hemorrhage, ECMO is currently reserved for newborn infants with reversible pulmonary disease in whom conventional or high frequency ventilation with inhaled nitric oxide has failed. An essential element in the ECMO circuit is the mechanical pump, which causes shear stress injury to blood components (7–10).
Advances in membrane and oxygenator technology have led to low-resistance membrane gas exchange devices that allow adequate flow even when the circuit is not driven by a pump. These pumpless extracorporeal lung assist devices (pECLA) and pumpless extracorporeal CO2 removal devices have been evaluated in animal studies (11–14) and adult patients (15–19). The lung assist device (LAD; MC3, Ann Arbor, MI) was initially designed as an artificial lung serving as a bridge for lung transplantation, to be placed in series with the main pulmonary artery (20,21). The LAD could support full gas exchange, and survival up to 7 d with complete diversion of pulmonary blood flow through the LAD with maintenance of hemodynamic stability has been shown with this device (22). Modifications of the LAD design have greatly improved cardiac function and initial survival in a healthy ovine model (23). In a prospective, randomized, unblinded study, the artificial lung decreased ventilator-induced lung injury in a severe ARDS model and improved 5-d survival (24). Recently, the thoracic artificial lung was found to be suitable for 7-d attachment (25) and 30-day respiratory support (26).
In this study, we used an acutely instrumented 3- to 4-wk-old piglet model to evaluate the feasibility and efficacy of the LAD in improving gas exchange and reducing hypoxia-induced pulmonary arterial hypertension. We hypothesized that the LAD would improve gas exchange and reduce hypoxia-induced pulmonary hypertension in a juvenile whole animal model.
METHODS
The Institutional Animal Care and Use Committee of the University of Alabama at Birmingham approved the research protocol. All animal care and handling were in accordance with the guidelines of the National Institutes of Health (27).
The LAD design.
The LAD was based on MC3s proprietary radial flow design. The device was composed of a series of parallel microporous hollow fibers (×30 240 Membrana-Celgard, Inc., Charlotte, NC) potted at both ends to separate the gas flow inside the fibers from the blood flowing outside the fibers. The blood entered an inlet centrally located within the fiber bundle, flowed radially over the microporous hollow fibers, and then exited a tangentially placed outlet (Fig. 1). The membrane surface area of the LAD used in this study was 0.5 m2. Previous bench studies of the LAD have characterized the relationship between surface area, gas exchange, blood flow rate, and sweep gas flow rate. MC3 was able to adapt the housing geometry to alter the device size and fiber bundle surface area to meet our requirements of smaller priming volume (60 mL) and gas exchange rates for the piglet model.
Surgery.
Six 3- to 4-wk-old piglets were heavily sedated with pentobarbital, endotracheally intubated, and mechanically ventilated using an Infant Star ventilator (Infant Star 950, Nellcor Puritan Bennett, Pleasanton, CA). Animals were placed on a table with a heating pad to maintain body temperature at 37 to 38°C. Pentobarbital (10 mg/kg/h i.v.) and diazepam (1 mg/kg/h i.v.) were used for sedation. The aorta, inferior vena cava, and pulmonary arteries were catheterized as previously described (28). Briefly, 5-Fr catheters were inserted into the thoracic aorta and inferior vena cava through the right femoral artery and right femoral vein, respectively, through a right groin incision. After a left thoracotomy between the second and third ribs, the pericardium was opened. A 10- or 12-mm precalibrated ultrasonic flow transducer (HT110, Transonic systems, Ithaca, NY) was affixed around the main pulmonary artery. A 5-Fr polyurethane catheter was then placed into the main pulmonary artery using purse-string sutures, and a similar catheter was placed into the left atrial appendage.
The left carotid artery and internal jugular vein were surgically exposed and cannulated with low-resistance cannulae (Medtronic, Minneapolis, MN) of 5 or 7 Fr and 8 or10 Fr diameter, respectively. The LAD was primed with 60 mL of heparinized normal saline, debubbled of air, and attached to the vascular cannulae. Animals were anticoagulated with a bolus of 50 units/kg of heparin after cannulation.
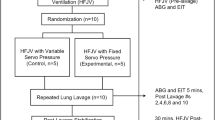
Experimental protocols.
Experiments were performed on sedated piglets after stabilization after surgery. After baseline recording of hemodynamic measurements for 15 min and ensuring stability of the recordings, hypoxia was induced by combining air with nitrogen to attain a delivered endotracheal FiO2 of 0.10. Final oxygen concentration was measured using an oxygen analyzer placed in series with the ventilator tubing. After additional continuous recording for 15 min and ensuring stability of the recordings, 100% oxygen at 1 L/min was allowed to flow through the LAD for 15 min. The oxygen flow through the LAD was then turned off for 15 min for a second baseline recording during hypoxia, followed by resumption of oxygen flow through the LAD. The duration of the experiment for each animal was limited to 2 h, after which the animal was killed with an overdose of pentobarbital.
Blood samples.
Femoral arterial and pre- and post-LAD blood gases were monitored using a blood gas analyzer (ABL 700 series, Radiometer America Inc., Westlake, OH) at the following time points: at baseline, 15 min after initiation of hypoxia, and 15 min after initiation of flow through the LAD.
Measurements.
Throughout the experiment, the heart rate, systemic arterial pressure (SAP), pulmonary arterial pressure (PAP), left atrial pressure (LAP), pulmonary blood flow [= cardiac output (CO)] were recorded using pressure transducers (Spectramed P23XL, Oxnard, CA) attached to the physiologic recorders (Gould-Brush 2400S, Oxnard, CA) and the ultrasonic flow transducer. Oxygen saturation was continuously monitored by pulse oximetry (N-100 C, Nellcor, Pleasanton, CA) on a forelimb. Extracorporeal flow was continuously measured by another ultrasonic flow probe (12XL, Transonic systems, Ithaca, NY) placed on the arterial side of the LAD. Pulmonary vascular resistance index (PVRI) was calculated as (PAP-LAP)/cardiac index (CI), and systemic vascular resistance index (SVRI) was calculated as (SAP−central venous pressure)/CI [CI = CO (mL/min)/weight (kg)]. The oxygen consumption (V˙o2) was calculated by measuring CO, femoral arterial oxygen tension and saturation, femoral venous oxygen tension and saturation, and Hb concentration, and calculations using the Fick equation [V˙o2 = CO × (CaO2 − CvO2)]. The capacity of the LAD to provide additional oxygen was calculated as the product of the flow rate through the device times the difference between the postdevice oxygen content and predevice oxygen content [oxygen transfer (mL/min) = LAD flow rate (mL/min) × difference in oxygen content as volume %].
Statistical analysis.
Data were expressed as mean ± SEM and analyzed by SigmaStat v. 3.5 (Jandel Scientific, San Rafael, CA). A p value of <0.05 was considered statistically significant.
Hemodynamic variables, blood gases, PAP, CO, and flow through the device before and after the experimental conditions were analyzed using ANOVA. If significant differences were found by repeated measures ANOVA, multiple comparisons by Holm-Sidak's test (for hemodynamic variables) or Tukey's test (for blood gases) were performed.
RESULTS
The six piglets were healthy 3- to 4-wk old female piglets weighing 4 to 6 kg. Successful LAD cannulation was achieved in all six animals with no complications. Five animals remained alive throughout the experiment, and one died during the hypoxic exposure.
At baseline, all the animals were ventilated at FiO2 of 1.0 with corresponding mean Pao2 of 453 ± 21 mm Hg, whereas PAP and PVRI were 11 ± 1 mm Hg and 0.041 ± 0.004 mm Hg·mL/min/kg, respectively. Hypoxia significantly reduced Pao2 and Pao2/FiO2 (Table 1), with a parallel increase in PAP and PVRI (Fig. 2).
Effect of the LAD on PAP, PVRI, mean SAP, and SVRI. Hypoxia: piglet exposed to endotracheal 10% oxygen without sweep gas flow through the LAD. LAD on: piglet exposed to endotracheal 10% oxygen in combination with sweep gas running through LAD. During induced hypoxia, blood gases were drawn from the pulmonary artery. (*p < 0.05. Mean ± SEM; n = 6; p < 0.05 by ANOVA for PAP and PVRI; p > 0.05 by ANOVA for SAP and SVRI.).
Insertion of the LAD did not significantly affect the CO. Blood flow through the device was stable throughout the experiment (Fig. 3). Extracorporeal shunt flow through the LAD was proportionally related to the catheter size. It increased from 7% of CO when 5 and 7 Fr catheters were used to cannulate the carotid artery and jugular vein, respectively, to 20% when 8 and 10 Fr catheters were used to cannulate the same respective vessels (Fig. 4). The LAD increased mean Pao2 from 37 ± 13 mm Hg (predevice) to 501 ± 90 mm Hg (postdevice) and decreased PaCO2 from 28 ± 8 mm Hg (predevice) to 7 ± 3 mm Hg (postdevice) (p < 0.05). Predevice arterial oxygen saturation averaged 78 ± 7%. Mean oxygen consumption V˙o2 was 6 ± 1 mL O2/kg/min, whereas the mean LAD capacity to add oxygen was 1.2 ± 0.5 mL O2/kg/min or 20% of total oxygen consumption.
The passage of 100% oxygen at 1 lpm through the LAD while endotracheal FiO2 was maintained at 0.10 reproducibly reversed the hypoxia effect on Pao2, PaO2/FiO2, PAP, and PVRI (Fig. 5). Mean PAP and PVRI were reduced by 35% from 28 ± 5 mm Hg to 18 ± 4 mm Hg and from 0.147 ± 0.030 mm Hg·mL/kg/min to 0.088 ± 0.001 mm Hg·mL/kg/min, respectively (p < 0.05). Pao2 increased by 33% from 27 ± 2 mm Hg to 36 ± 4 mm Hg (p < 0.05), and mean systemic CO2 tension (PaCO2) decreased from 35 ± 7 mm Hg to 29 ± 8 mm Hg (p > 0.05). Mean SAP decreased by a statistically insignificant 14% from 70 ± 8 mm Hg to 60 ± 5 mm Hg, and SVRI from 0.45 ± 0.05 mm Hg·mL/kg/min to 0.38 ± 0.03 mm Hg·mL/kg/min (p > 0.05), but no vasopressors were required. No significant changes were noted in the pH or calculated bicarbonate (Table 1).
DISCUSSION
We evaluated the feasibility and efficacy of a pumpless low-resistance membrane oxygenator in reducing PAP and improving gas exchange in hypoxia-induced pulmonary hypertension in juvenile piglets. We intended to study the LAD under experimental conditions that resembled the clinical situation of PPHN. The animal model used has been extensively studied by our group and shown to be a reliable model for the study of pulmonary hypertension (28–30).
ECMO provides for comprehensive gas exchange, but it is associated with many inherent complications, including consumption of blood components because of the large surface area of the ECMO circuit and shear stress effects of the mechanical pump. In theory, the LAD reduces these risks because of its small surface area that limits the interaction of blood with foreign material while still providing adequate surface area for partial gas exchange, and its low resistance that eliminates the need for a mechanical pump. An increasing recent emphasis on maintenance of large surface areas and short path lengths have enabled the development of low-resistance membrane oxygenators (pressure drop through the device <10 mm Hg), such as those used in the LAD. Gas exchange through these devices depends on sweep gas flow through the device, surface area of the hollow fiber membrane, and the extent of extracorporeal shunt. Compared with other commercially available gas exchangers, the LAD offers several advantages, including significantly smaller priming volume and pressure drop, hence reducing blood damage and allowing its application in situations with less than optimal CO and hemodynamic status. Because of the low resistance of the LAD and very efficient gas exchange through the hollow fiber membrane, the magnitude of the extracorporeal shunt is the most important variable in gas exchange. This is primarily determined by CO and luminal diameter of the catheters used to cannulate the vessels. The amount of oxygen added to the venous blood stream depended on the blood flow rate through the device and the magnitude of desaturation of Hb. The lower the oxygen saturation entering the LAD, the higher the amount of oxygen added to it, because the LAD adds a significant amount of dissolved oxygen thereby significantly increasing the oxygen content of blood leaving the device compared with the blood entering it {V˙o2 = flow × [(1.34 × Hb × SaO2) + (0.0031 × Pao2)] − [(1.34 × Hb × SvO2) + (0.0031 × PvO2)]}. These findings were consistent with the results of Zick et al. (14) who showed that oxygen delivery linearly correlated with the arterial oxygen saturation and the oxygenator blood flow.
Hemodynamically, the animals had stable heart rate and SAP after connecting the LAD and had sufficient and stable blood flow through the device. Under optimal in vitro experimental conditions and extrapolating from higher flow rate results, the LAD was expected to provide 2 to 2.5 mL O2/kg/min. In our current in vivo study, the oxygen delivery through the LAD was significantly increased by the higher shunt flow rate that was achieved with increasing catheter size. Increasing the catheter size from 5 Fr to 7 Fr internal diameter on the arterial side and from 8 Fr to 10 Fr on the venous side enabled us to improve the device oxygen delivery by 6-fold, up to a maximum of 40% of total oxygen consumption. Increasing the catheter sizes and hence the flow through the device to around 20% of the CO was well tolerated by the animals because there was no significant change in arterial pH or other systemic hemodynamic variables. Although Hb oxygen saturation is a more important determining factor in calculating blood oxygen content and hence oxygen delivery, we found that the capability of the LAD to improve oxygenation was positively affected by additional factors. First, the LAD provided a significant amount of dissolved oxygen, an addition of up to 14% compared with fully oxygen-saturated Hb, as described in the previous paragraph. Second, although similar devices are known for their capacity to remove CO2, PaCO2 decreased only by 17% in our study. This may be due to the fact that PaCO2 at the start of the experiment was low. Still, this decrease in PaCO2 may have positively affected oxygenation by increasing pH, thereby shifting the oxygen dissociation curve to the left and improving Hb oxygen saturation. The efficacy of CO2 removal would have been more pronounced if permissive hypercapnia was allowed. PAP and PVRI were significantly reduced, whereas Pao2 and Pao2/FiO2 were significantly increased in all animals. The effect of the LAD on PAP was immediate because Pao2 consistently increased whenever sweep gas through the LAD was turned on.
Our study had several limitations. Juvenile piglets may have different hemodynamic responses to hypoxia or to extracorporeal shunts compared with newborn humans. However, our laboratory has demonstrated similar responses to hypoxia in acutely instrumented newborn piglets (28–30). In addition, because this experiment was a feasibility study over a limited period of time, coagulation variables that would be of importance over a longer duration of extracorporeal support were not evaluated. In this preparation, the use of the LAD required cannulation of the carotid artery, which has been associated with complications when used in conventional arterio-venous ECMO. Finally, the LAD depends on normal or near-normal cardiac function and hence would be much less effective in low CO situations, such as cardiogenic shock.
In summary, we demonstrated the feasibility and efficacy of a pumpless low-resistance hollow fiber membrane oxygenator in the management of hypoxia-induced pulmonary hypertension in juvenile piglets. Although oxygen delivery through the LAD comprised only 20% of total oxygen consumption, the contribution of the LAD to oxygenation was significant with a subsequent reduction in pulmonary vasoconstriction secondary to hypoxia. Our results may have been accentuated by the fact that the induced arterial hypoxemia was severe. However, the Pao2 values in our study are similar to those seen in the clinical situation of PPHN. Full oxygenation through the LAD would require a higher shunt flow rate that may not be feasible with the currently available technology or CO. To reduce the risks of carotid artery cannulation, a trial of the LAD through the umbilical vessels is required. Still, this technology has potential as a simple, relatively inexpensive adjunct in the management of severe neonatal respiratory failure, perhaps reducing the need of conventional ECMO, or as a tool to be used during transport. Further studies on efficacy, safety, and biocompatibility are required before human clinical trials can be performed.
Abbreviations
- CI:
-
cardiac index
- CO:
-
cardiac output
- ECMO:
-
extracorporeal membrane oxygenation
- LAD:
-
lung assist device
- PPHN:
-
persistent pulmonary hypertension of the newborn
- PAP:
-
pulmonary arterial pressure
- PVRI:
-
pulmonary vascular resistance index
- VO2:
-
oxygen consumption
References
Walsh-Sukys MC, Tyson JE, Wright LL, Bauer CR, Korones SB, Stevenson DK, Verter J, Stoll BJ, Lemons JA, Papile LA, Shankaran S, Donovan EF, Oh W, Ehrenkranz RA, Fanaroff AA 2000 Persistent pulmonary hypertension of the newborn in the era before nitric oxide: practice variation and outcomes. Pediatrics 105: 14–20
Konduri GG 2004 New approaches for persistent pulmonary hypertension of newborn. Clin Perinatol 31: 591–611
UK Collaborative ECMO Trial Group 1996 UK collaborative randomised trial of neonatal extracorporeal membrane oxygenation. Lancet 348: 75–82
Kinsella JP, Truog WE, Walsh WF, Goldberg RN, Bancalari E, Mayock DE, Redding GJ, de Lemos RA, Sardesai S, McCurnin DC 1997 Randomized, multicenter trial of inhaled nitric oxide and high frequency oscillatory ventilation in severe, persistent pulmonary hypertension of the newborn. J Pediatr 131: 55–62
1997 Inhaled nitric oxide in full-term and nearly full-term infants with hypoxic respiratory failure. The Neonatal Inhaled Nitric Oxide Study Group. N Engl J Med 336: 597–604
Clark RH, Gertsmann DR, Jobe AH, Moffitt St, Slutsky AS, Yoder BA 2001 Lung injury in neonates: causes, strategies for prevention, and long-term consequences. J Pediatr 139: 478–486
Zwischenberger JB, Nguyen TT, Upp JR Jr, Bush PE, Cox CS Jr, Delosh T 1994 Complications of neonatal extracorporeal membrane oxygenation: collective experience from the extracorporeal life support organization. J Thorac Cardiovasc Surg 107: 838–849
Plotz FB, van Oeveren W, Bartlett RH, Wildevuur CR 1993 Blood activation during neonatal extracorporeal life support. J Thorac Cardiovasc Surg 105: 823–832
Hirthler MA, Blackwell E, Abbe D, Doe-Chapman R, Le Clair Smith C, Goldthorn J, Canizaro P 1992 Coagulation parameter instability as an early predictor of intracranial hemorrhage during extracorporeal membrane oxygenation. J Pediatr Surg 27: 40–43
Stallion A, Cofer BR, Rafferly JA, Ziegler MM, Ryckman FC 1994 The significant relationship between platelet count and haemorrhagic complications on ECMO. Perfusion 9: 265–269
Iglesias M, Junglebluth P, Petit C, Matute MP, Rovira I, Martinez E, Catalan M, Ramirez J, Macchiarini P 2008 Extracorporeal lung membrane provides lung protection than conventional treatment for severe postpneumonectomy noncardiogenic acute respiratory distress syndrome. J Thorac Cardiovasc Surg 135: 1362–1371
Nielsen ND, Kjaergaard B, Koefoed-Nielsen J, Steensen CO, Larsson A 2008 Apneic oxygenation combined with extracorporeal arteriovenous carbon dioxide removal provides sufficient gas exchange in experimental lung injury. ASAIO J 54: 401–405
Dembinski R, Hochhausen N, Terbeck S, Uhlig S, Dassow C, Schneider M, Schachtrupp A, Henzler D, Rossaint R, Kuhlen R 2007 Pumpless extracorporeal lung assist for protective mechanical ventilation in experimental lung injury. Crit Care Med 35: 2359–2366
Zick G, Frerichs I, Schädler D, Schmitz G, Pulletz S, Cavus E, Wachtler F, Scholz J, Weiler N 2006 Oxygenation effect of interventional lung assist in a lavage model of acute lung injury: a prospective experimental study. Crit Care 10: R56
Flörchinger B, Philipp A, Flose A, Hilker M, Kobuch R, Rupprecht L, Keyer A, Pühler T, Hirt S, Wiebe K, Müller T, Langgartner J, Lehle K, Schmid C 2008 Pumpless extracorporeal lung assist: a 10-year institutional experience. Ann Thorac Surg 86: 410–417
Hommel M, Deja M, von Dossow V, Diemel K, Heidenhain C, Spies C, Weber-Carstens S 2008 Bronchial fistulae in ARDS patients: management with an extracorporeal lung assist device. Eur Respir J 32: 1652–1655
Walles T 2007 Clinical experience with the iLA membrane ventilator pumpless extracorporeal lung-assist device. Expert Rev Med Devices 4: 297–305
Zimmermann M, Philipp A, Scmid FX, Dorlac W, Arlt M, Bein T 2007 From Baghdad to Germany: use of a new pumpless extracorporeal lung assist system in two severely injured US soldiers. ASAIO J 53: e4–e6
Bein T, Scherer MN, Philipp A, Weber F, Woertgen C 2005 Pumpless extracorporeal lung assist (pECLA) in patients with acute respiratory distress syndrome and severe brain injury. J Trauma 58: 1294–1297
Fazzalari FL, Montoya JP, Bonnell MR, Bliss DW, Hirschl RB, Bartlett RH 1994 The development of an implantable artificial lung. ASAIO J 40: M728–M731
Lynch WR, Montoya JP, Brant DO, Schreiner RJ, Iannettoni MD, Bartlett RH 2000 Hemodynamic effect of a low-resistance artificial lung in series with the native lungs of sheep. Ann Thorac Surg 69: 351–356
Lick SD, Zwischenberger JB, Alpard SK, Witt SA, Deyo DM, Merz SI 2001 Development of an ambulatory artificial lung in an ovine survival model. ASAIO J 47: 486–491
Lick SD, Zwischenberger JB, Wang D, Deyo DM, Alpard SK, Chambers SD 2001 Improved right heart function with a compliant inflow artificial lung in series with the pulmonary circulation. Ann Thorac Surg 72: 899–904
Zwischenberger JB, Wang D, Lick SD, Deyo DJ, Alpard SK, Chambers SD 2002 The paracorporeal artificial lung improves 5-day outcomes from lethal smoke/burn-induced acute respiratory distress syndrome in sheep. Ann Thorac Surg 74: 1011–1016
Sato H, Griffith GW, Hall CM, Toomasian JM, Hirschl RB, Bartlett RH, Cook KE 2007 Seven day artificial lung testing in an in-parallel configuration. Ann Thorac Surg 84: 988–994
Sato H, Hall CM, Lafayette NG, Pohlmann J, Padiyar N, Toomasian JM, Haft JW, Cook KE 2007 Thirty-day, in parallel artificial lung testing in sheep. Ann Thorac Surg 84: 1136–1143
Institute of Laboratory Animal Research Commission on Life Sciences, National Research Council 1997 The Guide for the Care and Use of Laboratory Animals 7th ed. National Academy Press, Washington D.C
Ambalavanan N, Bulger A, Murphy-Ullrich J, Oparil S, Chen YF 2005 Endothelin-A receptor blockade prevents and partially reverses neonatal hypoxic pulmonary vascular remodeling. Pediatr Res 57: 631–636
Ambalavanan N, Philips JB III, Bulger A, Oparil S, Chen YF 2002 Endothelin-A receptor blockade in porcine pulmonary hypertension. Pediatr Res 52: 913–921
Ambalavanan N, Bulger A, Ware J, Philips JB III 2001 Hemodynamic effects of levcromakalin in neonatal porcine pulmonary hypertension. Biol Neonate 80: 74–80
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported in part by PHA 0526041H, K08 HD 046513, R01 HL092906, and a grant from the Children's Center for Research and Innovation.
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
El-Ferzli, G., Philips, J., Bulger, A. et al. Evaluation of a Pumpless Lung Assist Device in Hypoxia-Induced Pulmonary Hypertension in Juvenile Piglets. Pediatr Res 66, 677–681 (2009). https://doi.org/10.1203/PDR.0b013e3181bbc7ec
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181bbc7ec