Abstract
The effect of oxygen concentration on lowering pulmonary vascular resistance (PVR) during resuscitation in a model of persistent pulmonary hypertension of the newborn (PPHN) is not known. PPHN was induced in fetal lambs by ductal ligation 9 d before delivery. After delivery by cesarean section, resuscitation of PPHN lambs with 21%, 50%, or 100% O2 (n = 6 each) for 30 min produced similar decreases in PVR. Lambs were then ventilated with 50% O2 for 60 min and exposed to inhaled nitric oxide (iNO, 20 ppm). Initial resuscitation with 100% O2 significantly impaired the subsequent response to iNO compared with 21% O2 (42 ± 9% vs 22 ± 4% decrease from baseline PVR). Finally, each lamb was randomly and sequentially ventilated with 10%, 21%, 50%, or 100% O2. PVR decreased with increased concentrations of inhaled O2 up to 50%, there being no additional decrease in PVR with 100% O2. When PVR was correlated with Pao2, the maximal change in PVR was achieved at Pao2 values <60 mm Hg. We conclude that resuscitation with 100% O2 does not enhance pulmonary vasodilation compared with 21% and 50% O2, but impairs the subsequent response to iNO in PPHN lambs. Hypoxia increases PVR but hyperoxia does not confer significant additional pulmonary vasodilation in lambs with PPHN.
Similar content being viewed by others
Main
The Neonatal Resuscitation Program currently recommends resuscitation of term newborn infants with 100% O2 (1). However, as 21% O2 has been associated with reduced neonatal mortality (2), some suggest that it may be appropriate for initial resuscitation of term infants (3). Although there is increasing availability of oxygen blenders for neonatal resuscitation (4), few studies have addressed the effect of resuscitation with an intermediate range of oxygen in the delivery room. We recently reported that ventilation of normal term lambs for 30 min at birth (referred to as “resuscitation”) with 50% and 100% O2 resulted in greater decrease in pulmonary vascular resistance (PVR) compared with 21% O2 (5).
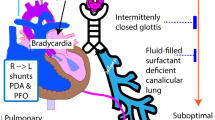
As oxygen mediates reduction of high fetal PVR at birth (1,6), 100% O2 is often recommended as the first line of resuscitation for circumstances associated with persistent pulmonary hypertension of the newborn (PPHN) (7). However, it is not always possible to anticipate conditions that might lead to in utero pulmonary hypertension (8,9). If PPHN infants are resuscitated at birth with 21% O2, PVR may remain high, resulting in severe PPHN and altered response to inhaled nitric oxide (iNO).
Once identified, babies with PPHN are traditionally managed with mechanical ventilation with high FiO2 (fraction of inspired oxygen) and iNO. Hyperoxic ventilation may increase production of reactive oxygen species (ROS), which in turn impair pulmonary vasodilation (10,11). However, little is known about the optimal FiO2 or Pao2 that maximizes pulmonary vasodilation in PPHN (12). We recently reported that ventilation with 100% O2 increases contractile responses of pulmonary arteries (PA) to norepinephrine from both control (13) and PPHN lambs (14), and blunts vascular responses to iNO in newborn lambs with acute pharmacologically induced PPHN (5). The effect of resuscitation with high FiO2 at birth on subsequent vasodilation to iNO in PPHN associated with vascular remodeling is not known.
This study examines the impact of FiO2 during resuscitation on the initial decrease in PVR at birth in lambs with PPHN induced by antenatal ductal ligation. We hypothesized that ventilation with 100% O2 would lead to a more rapid decline in PVR at birth in PPHN lambs compared with 21% or 50% O2 but would impair subsequent pulmonary vasodilation to iNO. Finally, at 2–3 h of age, when PVR had decreased from high fetal values, we studied the effect of change in FiO2 on PVR. We hypothesized that higher FiO2 and Pao2 would result in lower PVR in control and PPHN lambs.
METHODS
The Institutional Animal Care and Use Committee at Buffalo approved this study. Time-dated pregnant ewes were obtained from the Swartz family farm, Attica, NY. After 12 h of fasting, ewes were anesthetized with i.v. thiopental (20 mg/kg) and inhaled isoflurane (2%). Epidural preservative-free morphine (6 mg) and transdermal fentanyl patches (100 μg/h) provided postoperative analgesia. Fetal ductal ligation was performed at 126–128 d gestational age (term ∼ 145 d) to induce PPHN as previously described (14) and fetus was replaced in the uterus and allowed to recover for 9 d. The study consisted of three different postnatal time periods and protocols.
Effect of resuscitation with 21%, 50%, or 100% O2 for 30 min on pulmonary hemodynamics at birth.
Eighteen PPHN lambs and four control twins were partially exteriorized by cesarean section. While still on placental circulation, catheters were placed in the jugular vein, carotid artery, PA and left atrium, and an ultrasonic flow transducer around the main PA. Fetal carotid arterial blood gases (ABG) were obtained. The umbilical cord was clamped and cut. The lamb was weighed and ventilated with PIP 30, PEEP 5 cmH2O, rate 40/min. The four control (non-PPHN) lambs were resuscitated with 21% O2. For the PPHN lambs, the O2 concentration was randomly set at 21%, 50%, or 100% (n = 6 each). The ductus was tied during instrumentation before delivery in control lambs. Analgesia for the lamb was provided with a ketamine bolus (3 mg/kg) followed by an infusion of 20–100 μg/kg/min ketamine and 2 μg/kg/min of diazepam. One dose of pancuronium (0.1 mg/kg) was administered to all lambs at birth. Dextrose 10% solution with 25 mEq NaCl, 20 mEq KCl, and 10 mEq NaHCO3/L were administered at 120 mL/kg/d. ABGs were drawn every 5 min for 30 min, and ventilator adjustments were made to maintain Paco2 between 35 and 50 mm Hg. PVR was calculated using the following equation: PVR (mm Hg·mL−1·min·kg body weight) = (mean PA pressure − left atrial pressure in mm Hg) 47 pulmonary blood flow corrected for body weight (Qp, mL·min−1·kg−1).
Response to inhaled no.
After 30 min of ventilation at 21%, 50%, or 100% O2, PPHN lambs in all the three groups were ventilated with 50% O2 for 60 min. This concentration of oxygen was chosen because preliminary studies in PPHN lambs ventilated with 50% O2 for 24 h demonstrated similar survival with lower risk of oxygen toxicity compared with 100% O2. During this period, hypotension [mean systemic blood pressure (BP) <40 mm Hg] was treated with a transfusion of cord blood (10 mL/kg). When systemic BP was >40 mm Hg and PVR was stable, iNO was administered at 20 ppm for 10 min. The percent decrease in PVR after iNO was calculated.
Effect of varying FiO2 on PVR at 2–3 h of age.
Approximately 30 min after discontinuing iNO, and when PVR was stable, PPHN lambs were ventilated randomly and sequentially with 21%, 50%, and 100% O2 (two periods of 20 min each per lamb) and 10% O2 for 10 min. Eighteen control lambs without PPHN (twin lambs from other studies) with gestational age between 135 and 142 d were similarly ventilated. A shorter duration of ventilation with 10% O2 was chosen as PPHN lambs did not tolerate prolonged hypoxic ventilation. Two to three ABGs and PVR were obtained after 8–10 min of ventilation with each FiO2. Lambs were euthanized with pentobarbital (100 mg/kg) at the end of the study.
Statistical analysis was performed with ANOVA. The change points in Pao2 and PVR were determined by Markov chain Monte Carlo (MCMC) procedure using SAS 9.2 software (SAS, Cary, NC).
RESULTS
Thirty-four fetal lambs from time-dated pregnant ewes underwent antenatal fetal ductal ligation to induce PPHN. Eight premature deliveries after surgery, three still births, and four cases of severe hydrops were excluded. One lamb assigned to the 50% O2 group was hypotensive, acidotic, died at 60 min of life, and was excluded. There were no significant differences in birth weight and fetal ABG between the three groups of PPHN lambs (Table 1).
After delivery, all lambs with PPHN were hypoxemic compared with controls. Control lambs resuscitated with 21% O2 increased Pao2 significantly better than PPHN lambs by 30 min of age. Resuscitation of PPHN lambs with 100% O2 for 30 min significantly increased Pao2 compared with both fetal levels and lambs ventilated with 21% O2 for 30 min (Table 1).
Effect of resuscitation with 21%, 50%, and 100% O2 for 30 min on pulmonary hemodynamics at birth.
PA pressure was greater at all time points in lambs with PPHN compared with controls. PA pressure significantly decreased after 30 min of ventilation with 21%, 50%, or 100% O2 in all groups. There were no differences in PA pressures between the three PPHN groups (Fig. 1).
Changes in mean main pulmonary arterial pressure (mean ± SEM) during fetal life, at birth, and during the first 30 min of life in PPHN lambs ventilated with 21% (black squares), 50% (white triangles), or 100% O2 (gray circles) (n = 6 each). Similar changes in PA pressure in four control twin lambs without PPHN ventilated with air (dashed line) are shown for comparison. (*p < 0.05 by ANOVA over time; p < 0.05 compared with control by repeated measures ANOVA).
During fetal life, PPHN lambs had low Qp compared with controls but increased significantly after ventilation (Fig. 2). The increase in Qp with ventilation in PPHN lambs was significantly less compared with controls, but there were no differences between the three groups of PPHN lambs.
Changes in the blood flow in the main pulmonary artery (mean ± SEM) during fetal life, at birth, and during the first 30 min of life in PPHN lambs ventilated with 21% (black squares), 50% (white triangles), or 100% O2 (gray circles). Similar changes in Qp in four control twin lambs without PPHN ventilated with air (dashed line) are shown for comparison. (*p < 0.05 by ANOVA over time; p < 0.05 compared with control by repeated measures ANOVA).
Left atrial pressure was similar in all groups of lambs and increased significantly compared with fetal values in PPHN lambs ventilated with 50% and 100% O2. Systemic BP increased after delivery in all groups. There were no differences between control and PPHN lambs (data not shown).
PVR was significantly higher in PPHN lambs compared with controls (Fig. 3). Ventilation decreased PVR in all groups of lambs. However, ventilation with different FiO2 produced similar decreases in PVR in lambs with PPHN. After 30 min of ventilation, PVR remained significantly higher in all PPHN lambs compared with controls.
Changes in pulmonary vascular resistance (mean ± SEM) during fetal life, at birth, and during the first 30 min of life in PPHN lambs ventilated with 21% (black squares), 50% (white triangles), or 100% O2 (gray circles) (n = 6 each). Similar changes in PVR in four control twin lambs without PPHN ventilated with air are shown for comparison (dashed line). (*p < 0.05 by ANOVA over time; p < 0.05 compared with control by repeated measures ANOVA).
Systemic blood pressure increased after delivery in all groups of lambs. There were no differences between control and PPHN lambs (Fig. 4).
Changes in mean systemic arterial pressure (mean ± SEM) during fetal life, at birth, and during the first 30 min of life in lambs with PPHN ventilated with 21% (black squares), 50% (white triangles), or 100% O2 (gray circles) (n = 6 each). Similar changes in systemic arterial pressure in four control twin lambs without PPHN ventilated with air (dashed line) are shown for comparison. (*p < 0.05 compared with fetal values by ANOVA).
Response to iNO.
After 30 min of ventilation with 21%, 50%, or 100% O2, all the three groups of PPHN lambs were ventilated with 50% O2 for 60 min. After 90 min of ventilation (30 min with 21, 50, or 100% followed by 60 min with 50% O2), there were no significant differences in PVR among the three groups of PPHN lambs (baseline PVR in Fig. 5A). Inhaled NO (20 ppm with 50% O2) for 10 min significantly reduced PVR in all groups of lambs. Changes in Pao2 after iNO are shown in Figure 5B. The decrease in PVR, expressed as a percent of baseline, was significantly greater in PPHN lambs resuscitated with 21% compared with 100% O2 (42 ± 9% vs 22 ± 4%; Fig. 5C). However, PVR values did not differ among the three groups of lambs after exposure to iNO (Fig. 5A).
Changes in PVR (A) and Pao2 (B) at 90 min of age (baseline) and after 10 min of ventilation with 20 ppm of iNO. Lambs with PPHN were ventilated with 21% (black squares), 50% (white triangles), or 100% O2 (gray circles) for 30 min at birth and all the groups were ventilated with 50% O2 for 60 min before and during exposure to NO. (*p < 0.05 compared with baseline PVR). The percent fall in PVR with inhaled NO is shown in C (black bar, 21%; white bar, 50%; and gray bar, 100% O2 at birth). (†p < 0.05 compared with 100% O2).
Effect of varying FiO2 on pulmonary hemodynamics after the initial decrease in PVR at birth.
PPHN lambs were ventilated with 50%O2 for 30 min after cessation of iNO. When PVR was stable, they were randomly ventilated with 10%, 21%, 50%, and 100% O2 to examine the response of PVR to varying oxygen concentrations. Six PPHN lambs were unstable (bradycardia and/or cardiac arrest) during 10% O2 ventilation and required chest compressions and/or epinephrine and were excluded from the study. ABG values, PA pressure, and PVR at each FiO2 in control and PPHN lambs are shown in Table 2. Pao2 values significantly increased with increasing FiO2 in control and PPHN lambs. PA pressure and PVR decreased with increase in O2 from 10 to 21% and from 21 to 50% in both control and PPHN lambs. There was no further decrease in PA pressure or PVR after an increase from 50 to 100% O2 (Fig. 6A).
Changes in PVR in 2- to 3-h-old control and PPHN lambs with changing inspired oxygen concentration (A). PVR in control (white squares) and PPHN lambs (black circles) significantly decrease with increasing oxygen concentration from 10 to 21 to 50% O2. However, PVR does not decrease further with increase in oxygen from 50 to 100% O2 in both control and PPHN lambs. Scatter-plot showing PVR and Pao2 in control and PPHN lambs (B). The two regression lines for the control lambs correspond to PVR = 0.2 − 0.00667 (Po2 − 52.5) and PVR = 0.24 − 0.00013 (Po2 − 52.5), where 52.5 is the mean change point. The three regression lines for the PPHN lambs correspond to PVR = 1.41–0.5495 (Po2 − 13.9), PVR = 1.41–0.0152 (Po2 − 13.9), and PVR = 0.7206–0.00286 (Po2 − 59.6) where 13.9 and 59.6 are the means of the two change points. (C) Median and interquartile range (dashed lines) of PVR plotted against a clinically relevant range of oxygen saturations (80–100%) in control (white squares) and PPHN (black circles) lambs.
Figure 6B is a scatter plot of Pao2 and PVR in control and PPHN lambs. Data points from control lambs corresponded to a two-line regression model with one change point (Pao2 value at which the slope of the regression line changes) at 52.5 ± 1.7 mm Hg (Fig. 6B). The PVR values were significantly higher in PPHN lambs (especially with low Pao2 values, note change in y axis). These data points corresponded to a three-line regression model with two change point Pao2 values at 13.9 ± 1 and 59.6 ± 15.3 mm Hg. PVR values were plotted against a clinically relevant range of oxygen saturation from 80 to 100% (Fig. 6C).
DISCUSSION
PPHN is a syndrome of failed pulmonary circulatory adaptation at birth, resulting in high PVR and neonatal respiratory failure (12). Recent studies suggest that resuscitation with 21% O2 is just as successful as resuscitation with 100% O2 in term neonates (2). Theoretically, the use of supplemental oxygen during resuscitation may result in a more rapid increase in Qp (1) and improve brain oxygenation (15) in a neonate with PPHN. Also, the optimal FiO2 and Pao2 in the management of neonates with PPHN is not known (12). This is the first study to examine the effect of varying FiO2 on PVR in an animal model of in utero pulmonary hypertension with vascular remodeling. We studied this effect at birth, when fetal PVR is high, and at 2–3 h of age, after the initial decrease in PVR with postnatal ventilation.
In term lambs with normal pulmonary vasculature, we recently reported that 100% O2 decreased PVR more rapidly and to a greater magnitude than 21% O2 (5). As PPHN has been reported to affect as many as 10% of neonates with respiratory failure (9), we extended these studies to determine the effectiveness of 21%, 50%, and 100% O2 during resuscitation in reducing PVR in a well established lamb model of PPHN with remodeled pulmonary circulation (14,16).
In lambs with PPHN, PVR decreased from high fetal values without any significant increase in Pao2 after resuscitation with 21% and 50% O2 (Fig. 3) probably secondary to ventilation and several fold increase in alveolar oxygen levels. Contrary to our hypothesis, 100% O2 did not enhance the decrease in PA pressure and PVR, or increase Qp compared with 21% or 50% O2 (Figs. 1–3). The differences in transitional responses to varying FiO2 relative to control lambs could be explained by three possible mechanisms. Control fetal ovine PA smooth muscle cells respond to an acute increase in Po2 by decreasing intracellular calcium concentration, resulting in vasodilation (17), whereas PA smooth muscle cells isolated from lambs with PPHN after ductal ligation do not (18). Decreased PA NO synthase (NOS) function and activity in PPHN lambs (16,19,20) could also be a contributory factor. Lastly, this model of PPHN is associated with increased oxidative stress, even with fetal Po2 levels (21). Ventilation with 100% O2 would be expected to increase in alveolar oxygen tension at birth by 20- to 25-fold and promote further ROS formation to enhance vasoconstrictive effects on the neonatal pulmonary circulation (11,22,23). These effects of ROS on pulmonary circulation may be mediated by the formation of isoprostanes (24). In fact, we have previously shown that 24 h exposure to 100% O2 significantly increases lung isoprostane levels in PPHN lambs (14).
The primary aim of PPHN therapy is selective pulmonary vasodilation (25). Inhaled NO is a rapid, potent, and selective pulmonary vasodilator that has been shown to reduce PVR in ductal ligation lambs and improve oxygenation and reduce ECMO use in human infants with PPHN (26–29). Although iNO significantly decreased PVR in all groups of lambs in this study, prior exposure to 100% O2 decreased the magnitude of response to iNO (Fig. 6). We previously reported that resuscitation with 100% O2 similarly blunted subsequent pulmonary vascular responses to iNO in normal lambs with acute pulmonary hypertension induced by pharmacological infusion of a thromboxane analog (5).
Why does prior exposure to 100% O2 reduce the effectiveness of iNO? More than a decade ago, Sanderud et al. (30) suspected that ROS-mediated inactivation of NO contributes to pulmonary vasoconstriction. We speculate that exposure to 100% O2 increases superoxide anions resulting in rapid inactivation of NO (31) through formation of peroxynitrite (14,24). We recently reported an increase in superoxide anion and peroxynitrite production after 24 h ventilation of lambs with PPHN with 100% O2 and iNO (14,32). Hyperoxia and ROS also increase activity and expression of phosphodiesterase 5, inactivating the critical second messenger, cGMP (10). The role of ROS in pulmonary vasoconstriction is further established by the effectiveness of antioxidants in counteracting the effects of ROS on pulmonary vasculature (26,30,33).
The optimal FiO2 and Pao2 during ventilation of neonates with PPHN are not known. Traditional management of PPHN included hyperoxic ventilation during the acute phase of PPHN to promote pulmonary vasodilation. However, we found that ventilation with 100% O2 did not decrease PVR compared with 50% in control and PPHN lambs despite a significant increase in Pao2 (Fig. 6A). Rudolph and Yuan (34) first reported the relationship between Pao2 and PVR in young, healthy calves. They found that PVR rose steeply when the Pao2 fell below 45 to 50 mm Hg, but decreased minimally when the Pao2 was >50 mm Hg (34). We found a similar relationship between Pao2 and PVR in control lambs in this study, observing an acute increase in PVR with Pao2 <52.5 ± 1.7 mm Hg (Fig. 6B). In PPHN lambs, severe hypoxemia with Pao2 below 13.9 ± 1.1 mm Hg resulted in a steep increase in PVR (Fig. 6B), and PVR decreased only minimally when the Pao2 rose above 59.6 ± 15.3 mm Hg. This demonstrates that, except in the presence of extreme hypoxemia, the remodeled pulmonary vasculature in PPHN lambs is not responsive to increased FiO2 or Pao2. This may account for the similar decrease in PVR with 21%, 50%, and 100% O2 ventilation at birth in PPHN lambs (Fig. 3) in contrast with our previous study in control lambs (5). Pao2 exceeding 60 mm Hg (corresponding to an oxygen saturation of 90%) resulted in very little further decrease in PVR in control and PPHN lambs (Fig. 6). These findings are similar to previous clinical observations in children with bronchopulmonary dysplasia and pulmonary hypertension (35).
We acknowledge several limitations for this study. First, the ductal ligation model represents idiopathic PPHN associated with remodeled pulmonary vasculature. The findings in this study may not be applicable to all forms of pulmonary hypertension. For instance, while right to left shunting is common in human infants with PPHN, ductal occlusion prevents right to left shunt at this level and may contribute to increase right ventricular afterload. Factors known to increase pulmonary vascular sensitivity to oxygen such as hypercarbia and acidosis (34) are often associated with PPHN with acute asphyxia (36) but are not present in our model. However, other studies in asphyxiated piglets have shown similar reductions in PVR with 21% and 100% O2 resuscitation (37,38). The same set of PPHN lambs were used to study two inter-related questions about the effect of FiO2 and PVR. We did not see any significant impact of oxygen concentration during resuscitation at birth (Fig. 3) on subsequent PVR response to oxygen after stabilization (Fig. 6). However, the brief period of exposure to iNO might have influenced these results. Moreover, our study design did not allow us to perform mechanistic studies to explain our findings. Our main aim was to determine the physiologic and hemodynamic changes associated with early transition in the pulmonary circulation. These findings now provide the basis for future investigations into the vascular mechanisms underlying these responses.
We conclude that, even in a model of PPHN associated with remodeled pulmonary vasculature, initial resuscitation with 21% or 50% O2 reduces PVR as effectively as 100% O2. Exposure of PPHN lambs to initial resuscitation in 21% O2 allowed a greater response later to iNO compared with 100% O2. We speculate that infants with in utero pulmonary hypertension who are adequately ventilated and briefly resuscitated with 21% O2 in the delivery room will likely respond with a significant decrease in PVR without any impairment of subsequent pulmonary vasodilation to iNO. Finally, maintaining Pao2 significantly above 60 mm Hg may not confer additional pulmonary vasodilation in the management of PPHN. Further clinical studies focused on the effect of varying FiO2 on PVR in PPHN are warranted.
Abbreviations
- ABG:
-
arterial blood gas
- BP:
-
blood pressure
- FiO2:
-
fraction of inspired oxygen
- PPHN:
-
persistent pulmonary hypertension of the newborn
- PA:
-
pulmonary artery
- Qp:
-
pulmonary blood flow
- PVR:
-
pulmonary vascular resistance
- ROS:
-
reactive oxygen species
References
Kattwinkel J 2006 Textbook of Neonatal Resuscitation. American Academy of Pediatrics, Elk Grove Village, IL p 272
Saugstad OD, Ramji S, Soll RF, Vento M 2008 Resuscitation of newborn infants with 21% or 100% oxygen: an updated systematic review and meta-analysis. Neonatology 94: 176–182
Hansmann G, Humpl T, Zimmermann A, Buhrer C, Wauer R, Stannigel H, Hoehn T, ILCOR 2007 [ILCOR's new resuscitation guidelines in preterm and term infants: critical discussion and suggestions for implementation]. Klin Padiatr 219: 50–57
Sola A, Deulofeut R 2006 Oxygen and oxygenation in the delivery room. J Pediatr 148: 564–565
Lakshminrusimha S, Russell JA, Steinhorn RH, Swartz DD, Ryan RM, Gugino SF, Wynn KA, Kumar VH, Mathew B, Kirmani K, Morin FC III 2007 Pulmonary hemodynamics in neonatal lambs resuscitated with 21%, 50%, and 100% oxygen. Pediatr Res 62: 313–318
Teitel DF, Iwamoto HS, Rudolph AM 1990 Changes in the pulmonary circulation during birth-related events. Pediatr Res 27: 372–378
Paneth N 2005 The evidence mounts against use of pure oxygen in newborn resuscitation. J Pediatr 147: 4–6
Hernandez-Diaz S, Van Marter LJ, Werler MM, Louik C, Mitchell AA 2007 Risk factors for persistent pulmonary hypertension of the newborn. Pediatrics 120: e272–e282
Walsh-Sukys MC, Tyson JE, Wright LL, Bauer CR, Korones SB, Stevenson DK, Verter J, Stoll BJ, Lemons JA, Papile LA, Shankaran S, Donovan EF, Oh W, Ehrenkranz RA, Fanaroff AA 2000 Persistent pulmonary hypertension of the newborn in the era before nitric oxide: practice variation and outcomes. Pediatrics 105: 14–20
Farrow KN, Groh BS, Schumacker PT, Lakshminrusimha S, Czech L, Gugino SF, Russell JA, Steinhorn RH 2008 Hyperoxia increases phosphodiesterase 5 expression and activity in ovine fetal pulmonary artery smooth muscle cells. Circ Res 102: 226–233
Saugstad OD, Sanderud J 1989 Circulatory effects of oxygen radicals. Biomed Biochim Acta 48: S20–S24
Aschner JL, Fike CD 2008 New developments in the pathogenesis and management of neonatal pulmonary hypertension. In: Bancalari E (ed) The Newborn Lung. Saunders Elsevier, Philadelphia pp 241–299
Lakshminrusimha S, Russell JA, Steinhorn RH, Ryan RM, Gugino SF, Morin FC III Swartz DD, Kumar VH 2006 Pulmonary arterial contractility in neonatal lambs increases with 100% oxygen resuscitation. Pediatr Res 59: 137–141
Lakshminrusimha S, Russell JA, Wedgwood S, Gugino SF, Kazzaz JA, Davis JM, Steinhorn RH 2006 Superoxide dismutase improves oxygenation and reduces oxidation in neonatal pulmonary hypertension. Am J Respir Crit Care Med 174: 1370–1377
Perez-de-Sa V, Cunha-Goncalves D, Nordh A, Hansson S, Larsson A, Ley D, Fellman V, Werner O 2009 High brain tissue oxygen tension during ventilation with 100% oxygen after fetal asphyxia in newborn sheep. Pediatr Res 65: 57–61
Steinhorn RH, Russell JA, Morin FC III 1995 Disruption of cGMP production in pulmonary arteries isolated from fetal lambs with pulmonary hypertension. Am J Physiol 268: H1483–H1489
Rhodes MT, Porter VA, Saqueton CB, Herron JM, Resnik ER, Cornfield DN 2001 Pulmonary vascular response to normoxia and K(Ca) channel activity is developmentally regulated. Am J Physiol Lung Cell Mol Physiol 280: L1250–L1257
Linden BC, Resnik ER, Hendrickson KJ, Herron JM, O'Connor TJ, Cornfield DN 2003 Chronic intrauterine pulmonary hypertension compromises fetal pulmonary artery smooth muscle cell O2 sensing. Am J Physiol Lung Cell Mol Physiol 285: L1354–L1361
Konduri GG, Ou J, Shi Y, Pritchard KA Jr 2003 Decreased association of HSP90 impairs endothelial nitric oxide synthase in fetal lambs with persistent pulmonary hypertension. Am J Physiol Heart Circ Physiol 285: H204–H211
Tzao C, Nickerson PA, Steinhorn RH, Noble BK, Swartz DD, Russell JA 2002 Type I nitric oxide synthase is decreased in the fetal pulmonary circulation of hypertensive lambs. Pediatr Pulmonol 33: 437–442
Brennan LA, Steinhorn RH, Wedgwood S, Mata-Greenwood E, Roark EA, Russell JA, Black SM 2003 Increased superoxide generation is associated with pulmonary hypertension in fetal lambs: a role for NADPH oxidase. Circ Res 92: 683–691
Sanderud J, Bjoro K, Saugstad OD 1993 Oxygen radicals stimulate thromboxane and prostacyclin synthesis and induce vasoconstriction in pig lungs. Scand J Clin Lab Invest 53: 447–455
Sanderud J, Norstein J, Saugstad OD 1991 Reactive oxygen metabolites produce pulmonary vasoconstriction in young pigs. Pediatr Res 29: 543–547
Belik J, Jankov RP, Pan J, Yi M, Chaudhry I, Tanswell AK 2004 Chronic O2 exposure in the newborn rat results in decreased pulmonary arterial nitric oxide release and altered smooth muscle response to isoprostane. J Appl Physiol 96: 725–730
Steinhorn RH 2008 Nitric oxide and beyond: new insights and therapies for pulmonary hypertension. J Perinatol 28: S67–S71
Steinhorn RH, Albert G, Swartz DD, Russell JA, Levine CR, Davis JM 2001 Recombinant human superoxide dismutase enhances the effect of inhaled nitric oxide in persistent pulmonary hypertension. Am J Respir Crit Care Med 164: 834–839
Zayek M, Cleveland D, Morin FC III 1993 Treatment of persistent pulmonary hypertension in the newborn lamb by inhaled nitric oxide. J Pediatr 122: 743–750
Kinsella JP, Abman SH 2005 Inhaled nitric oxide therapy in children. Paediatr Respir Rev 6: 190–198
Roberts JD Jr, Fineman JR, Morin FC III, Shaul PW, Rimar S, Schreiber MD, Polin RA, Zwass MS, Zayek MM, Gross I, Heymann MA, Zapol WM 1997 Inhaled nitric oxide and persistent pulmonary hypertension of the newborn. The Inhaled Nitric Oxide Study Group. N Engl J Med 336: 605–610
Sanderud J, Oroszlan G, Bjoro K, Kumlin M, Saugstad OD 1995 d-penicillamine inhibits the action of reactive oxygen species in the pig pulmonary circulation. J Perinat Med 23: 385–393
Faraci FM, Didion SP 2004 Vascular protection: superoxide dismutase isoforms in the vessel wall. Arterioscler Thromb Vasc Biol 24: 1367–1373
Farrow KN, Lakshminrusimha S, Reda WJ, Wedgwood S, Czech L, Gugino SF, Davis JM, Russell JA, Steinhorn RH 2008 Superoxide dismutase restores eNOS expression and function in resistance pulmonary arteries from neonatal lambs with persistent pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol 295: L979–L987
Fike CD, Slaughter JC, Kaplowitz MR, Zhang Y, Aschner JL 2008 Reactive oxygen species from NADPH oxidase contribute to altered pulmonary vascular responses in piglets with chronic hypoxia-induced pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol 295: L881–L888
Rudolph AM, Yuan S 1966 Response of the pulmonary vasculature to hypoxia and H+ ion concentration changes. J Clin Invest 45: 399–411
Mourani PM, Ivy DD, Gao D, Abman SH 2004 Pulmonary vascular effects of inhaled nitric oxide and oxygen tension in bronchopulmonary dysplasia. Am J Respir Crit Care Med 170: 1006–1013
Richmond S, Goldsmith JP 2008 Refining the role of oxygen administration during delivery room resuscitation: what are the future goals?. Semin Fetal Neonatal Med 13: 368–374
Fugelseth D, Borke WB, Lenes K, Matthews I, Saugstad OD, Thaulow E 2005 Restoration of cardiopulmonary function with 21% versus 100% oxygen after hypoxaemia in newborn pigs. Arch Dis Child Fetal Neonatal Ed 90: F229–F234
Medbo S, Tollofsrud PA, Saugstad OD 1999 Pulmonary hemodynamics in newborn piglets during hypoxemia and reoxygenation: blocking of the endothelin-1 receptors. Pediatr Res 46: 514–522
Acknowledgements
We thank Ikaria for providing iNO and Aeronox delivery systems.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the American Academy of Pediatrics/Neonatal Resuscitation Program (S.L.) and Grant HL-54705 from the National Heart, Lung, and Blood Institute (R.H.S.).
Rights and permissions
About this article
Cite this article
Lakshminrusimha, S., Swartz, D., Gugino, S. et al. Oxygen Concentration and Pulmonary Hemodynamics in Newborn Lambs With Pulmonary Hypertension. Pediatr Res 66, 539–544 (2009). https://doi.org/10.1203/PDR.0b013e3181bab0c7
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181bab0c7
This article is cited by
-
Occurrence of hyperoxia during iNO treatment for persistent pulmonary hypertension of the newborn: a cohort study
European Journal of Pediatrics (2024)
-
Meconium aspiration syndrome: a comprehensive review
Journal of Perinatology (2023)
-
Maternal and neonatal risk factors for neonatal respiratory distress syndrome in term neonates in Cyprus: a prospective case–control study
Italian Journal of Pediatrics (2021)
-
Left-sided congenital diaphragmatic hernia: can we improve survival while decreasing ECMO?
Journal of Perinatology (2020)
-
Inhaled nitric oxide as an adjunct to neonatal resuscitation in premature infants: a pilot, double blind, randomized controlled trial
Pediatric Research (2020)