Abstract
We investigated whether obese children and adolescents have early echocardiographic signs of subclinical cardiac dysfunction and evaluated the respective influence of obesity per se versus parameters of carbohydrate and lipid metabolism that are frequently abnormal in obese subjects. The role of tissue Doppler imaging as a screening tool for these abnormalities was explored. Blood pressure and echocardiographic parameters, including tissue Doppler measurements of the septal mitral annulus were evaluated in 49 obese children and adolescents and 45 age and sex matched controls. The respective influence of obesity versus parameters of carbohydrate and lipid metabolism was examined with linear regression analysis. Obese subjects showed significantly larger left ventricular wall dimensions (posterior wall, septum, and left ventricular mass index) and signs of early diastolic filling abnormalities on conventional and tissue Doppler echocardiography compared with nonobese subjects. Multiple regression analysis showed that mainly BMI-SD scores and/or body surface area explained significant proportions of the variance of the early cardiac abnormalities. In conclusion, young, obese children and adolescents have significant changes in left ventricular wall dimensions and early diastolic filling compared with nonobese subjects. Obesity per se and not the parameters of carbohydrate and lipid metabolism predicted the early cardiac abnormalities.
Similar content being viewed by others
Main
The prevalence of overweight and obesity in children is increasing worldwide at an alarming rate in both developing and developed countries (1). In the United States, approximately 31.2% of children (aged 6–11) are overweight of which 15.8% are obese. For adolescents (aged 12–19), 30.9% are overweight of which 16.1% are obese (2). It is well established that obesity is a strong risk factor for cardiovascular morbidity and mortality. Studies in adults using echocardiography, catheterization, and necropsy examinations have shown relations between morbid obesity, structural alterations of the heart and systolic function, which may lead to a clinical syndrome known as “obese cardiomyopathy” (3). However, the relation between obesity and cardiac structure and function in children is less well documented and conflicting results have been reported (4–7). In addition, obesity is associated with a heterogeneity of metabolic abnormalities (e.g., dyslipidemia (8), insulin resistance (9), hyperglycaemia) and hypertension (10) that may provide a plausible biologic link between obesity and the increased risk of cardiovascular morbidity and mortality. The clustering of these risk factors for cardiovascular disease is referred to as the “metabolic syndrome.” Although the concept and definition of the metabolic syndrome are controversial at the moment, there is no doubt that a cluster of cardiovascular risk factors is present in obese children and adolescents and that their presence increases with worsening obesity (11–13). Little is however known about the relative influence of obesity per se versus associated risk factors for cardiovascular disease (more in specific parameters of carbohydrate and lipid metabolism) on cardiac structure and function.
In the present study, we evaluated whether echocardiographic signs of diastolic and systolic dysfunction are already present in obese children and adolescents. Within the obese subjects, we investigated the relative influence of obesity versus associated cardiovascular risk factors on these abnormalities. Additionally, we explored the role of tissue Doppler imaging (TDI), an emerging technique that measures velocities of the myocardium in systole and diastole, as a screening tool for these abnormalities.
METHODS
Study population.
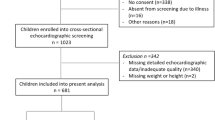
We studied 49 obese children and adolescents from the patient population attending the Obesity Clinic for Children and Adolescents of the Antwerp University Hospital. Exclusion criteria were a significant concomitant illness, medication known to modify cardiac function and obvious clinical signs of cardiac disease. The control group consisted of 45 healthy volunteers, matched for age and sex. Patient characteristics are given in Table 1. The Antwerp University Hospital ethical review board approved the study. The participants and at least one of their parents provided written informed consent.
Clinical assessment.
Each subject's height and body weight were measured. BMI was calculated using the formula (body weight in kilograms)/(body height in meters) (2) and BMI values were converted to SD scores (BMI-SDS) adjusted for age and sex using the updated British 1990 reference charts (14). Systolic (SBP) and diastolic blood pressure (DPB) was measured by the cuff method (Dinamap automated vital signs monitor, Criticon, Norderstedt, Germany). Hematological and biochemical variables were determined in the obese subjects from fasting blood samples and included glucose, insulin, total cholesterol, triglycerides (TG), and HDL (HDL) cholesterol. LDL (LDL) cholesterol and the QUICKI index, an index for insulin resistance (15), were calculated using the formulas (LDL = total cholesterol − (TG/5) − HDL) and (QUICKI = 1/(log fasting insulin + log fasting glucose), respectively.
Echocardiographic measurements.
After recording a standard 12 lead ECG (Mac 5000, GE, Marquette Medical Systems, Milwaukee, WI), a complete echocardiographic study with a simultaneous ECG (standard lead II) was performed on each patient and control subject using a Hewlett-Packard Sonos 5500, equipped with a S8 (3–8 MHz) transducer. Guided by two-dimensional echocardiography, standard M-mode recordings of the left ventricle (LV) dimensions and function were obtained. The LV mass (LVM) and relative posterior wall thickness were calculated according to the formulae of Devereux et al. (16). The methods of correcting LVM for body size have varied between studies. Left ventricular hypertrophy has been underestimated in the obese with the use of LVM divided by body surface area (BSA) because this index considers obesity as a physiologic variable. Height 2.7 (in meters) had been validated and recommended for indexing LVM (4) and was used in this study. Conventional Doppler tracings of the mitral and the tricuspid valve and pulmonary venous return flow were obtained from an apical 4-chamber view. The Doppler cursor line was placed in the inlet or the vein at an angle as parallel to flow as possible and in the position of maximal velocity. Doppler values of the aortic and pulmonary venous flow were measured from the suprasternal and parasternal short axis, respectively. Duration values were corrected for heart rate. Tissue Doppler values of the septal mitral annulus were obtained from the apical four-chamber view. The ratio of early mitral flow velocity (E-wave) to early diastolic velocity of the mitral annulus (E/E′) was calculated. The Doppler-derived index of combined systolic and diastolic myocardial performance (Tei-index), defined as the sum of isovolumetric relaxation time and isovolumetric contraction time, divided by ejection time was used for quantification of the global right and left ventricular function (Fig. 1) (17). All Doppler signals were recorded at a speed of 50 mm/s. For each parameter, the average of three cycles was used. All the measurements were made off-line by the same observer blinded to the patients' clinical details.
Statistical analysis.
Data are summarized using means and standard deviations, unless indicated otherwise. Means of obese and nonobese subjects were compared using an unpaired t test or Mann Whitney U-test, for categorical variables the χ2 test was used. To investigate the relative influence of obesity versus associated cardiovascular risk factors (parameters of carbohydrate and lipid metabolism) on the echocardiographic variables that differed between obese and nonobese, linear regression analysis was performed. BMI-SDS, BSA, age, SBP, DBP, total cholesterol, HDL, LDL, TG, fasting glucose, fasting insulin, and the QUICKI index were a priori considered as possible determinants. Univariable regression models were constructed to examine the associations of predictor variables with the dependent echocardiographic variables (a p value of 0.10 was used here to indicate statistical significance). Stepwise multiple regression analysis was then used to determine which determinants independently explained a significant (p < 0.05) fraction of the variance of the dependent variables. Residual analysis was performed to check the validity of model assumptions. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS Inc., 2001, Chicago), version 11.0. A p value of ≤0.05 was considered statistically significant.
RESULTS
Clinical characteristics of the study groups.
The clinical, anthropometric, and metabolic characteristics of the study group are shown in Table 1. The obese and nonobese subjects were comparable with respect to age, sex, and heart rate. Obese subjects, however, had significantly higher z-scores for BMI, higher body surface area, and higher SBP and DBP (Table 1).
LV dimensions and systolic function.
LV wall dimensions were higher in the obese population (Table 2). Statistical significance was reached for ventricular septum in systole and diastole (IVSs and IVSd), internal LV diameter in diastole (LVIDd), LV posterior wall in diastole and systole (LVPWd and LVPWs), relative posterior wall thickness and LVM and LVMI. The contractility indices (ejection fraction, fractional shortening, and velocity of circumferential shortening) were similar in obese and nonobese subjects (data not shown).
Diastolic function.
For the conventional Doppler measurements, the maximal and mean velocities of active mitral filling (Amax and Amean) were similar in obese and normal subjects (Table 2). Tissue Doppler derived indices of the septal mitral annulus showed generally lower velocities in the obese population, although only significant for the E′ wave velocity, resulting in a significant higher E/E′ ratio. The pulmonary venous flow velocity during systole showed a trend to be higher in obese children (p = 0.058).
Time intervals and duration.
The Tei-index for the left ventricle was significantly lower in the obese subjects (Table 2). Tei-index for the right ventricle was difficult to obtain, because it was often impossible to simultaneously record the interval between cessation and onset of the tricuspid inflow and the right ventricular ejection time. The duration of the pulmonary venous flow during atrial contraction was significantly longer in obese subjects.
Multiple regression analysis.
To investigate the relative influence of obesity per se versus the associated cardiovascular risk factors (parameters of carbohydrate and lipid metabolism) on the echocardiographic variables that differed between obese and nonobese, stepwise multiple regression analysis was performed. Mainly BMI-SDS and/or BSA had an independent effect on the echocardiographic variables that differed between obese and nonobese subjects (Table 3). The associated metabolic risk factors, more specifically fasting glucose, insulin, total cholesterol, TG, HDL cholesterol, LDL cholesterol, and the QUICKI index, did not explain a significant proportion of the variance of echocardiographic variables.
DISCUSSION
This cross-sectional study provides evidence that asymptomatic obese children already exhibit abnormalities of left ventricle structure and function (consisting of increased left ventricular wall dimensions and mass and alteration of diastolic function) that can be detected by TDI. Furthermore, BMI-SDS and/or BSA and not the associated cardiovascular risk factors (parameters of carbohydrate and lipid metabolism) were found to be independent predictors of adverse LV remodeling and of diastolic dysfunction. To our knowledge, this is the first study that evaluates early echocardiographic signs (including TDI) of subclinical cardiac dysfunction in obese children and adolescents and the respective influence of obesity per se versus the associated cardiovascular risk factors.
LV morphology and systolic function.
The association of LV remodelling and obesity in the present study is supported by previous studies in adults and children (18–20). The Bogulosa Heart Study showed a strong association between LVM in childhood and the degree of obesity (18). In the Strong Heart Study, increased levels of LVM were found in overweight and obese adolescents. Additionally, they found a significant increase in stroke volume in obese adolescents, indicating increased cardiac workload (20). In the present study, no patient presented with subclinical systolic dysfunction. Most echo-cardiographic studies that assessed systolic function in obese subjects have shown normal results (21–23). Reduction of indices of systolic function were only found in patients with a considerable degree of obesity, suggesting that left ventricular function is affected late in the course of obesity (20,24).
Diastolic function.
The Doppler method of measuring indices of left ventricular filling has been shown to be of great value in assessing diastolic function. However, when volume overload is present, as it is in obesity, normal values may result as the increase in left atrial pressure caused by intravascular volume can mask alterations observed in the early phases of abnormal diastolic relaxation. TDI is an emerging technique that modifies conventional Doppler to measure the velocity of the myocardium in systole and diastole. It has proved to be more sensitive to detect subclinical LV dysfunction in several disorders with normal standard parameters of global LV systolic function (25,26). Few studies have investigated diastolic function in obese children and adolescents. Harada et al. (27) found altered transmitral and pulmonary venous velocities in 21 obese children using pulse-wave Doppler, suggesting a reduction in early diastolic filling. In the present study, we did not find these abnormalities. Only one recent study investigated diastolic function using TDI in 25 obese and overweight children (28) providing unique insights into the effects obesity on LV diastolic function. They observed impaired early diastolic function (E′) in the overweight and obese group. The E′/A′ ratio was found to be inversely related to BMI. In the present study, we confirmed these results in a larger group of 49 young obese subjects. The relation between obesity and diastolic filling is not well understood. Although the association of myocardial fatty infiltration with obesity is well recognized, it is not a prominent finding at autopsy. Altered loading conditions are also likely to contribute. Elevated preload is to be expected in obese patients, which would indicate early filling. It has been reported to have a marked effect on peak velocity during atrial contraction and reversal flow of pulmonary venous flow with less effect on pulmonary diastolic flow velocity.
Influence of associated cardiovascular risk factors.
Obesity is associated with a group of metabolic abnormalities [e.g., dyslipidemia (8), insulin resistance (9), hyperglycaemia), and hypertension (10)[, referred to as the “metabolic syndrome.” It has been suggested that the metabolic abnormalities could be involved in the modulation of left ventricular structure. Several studies have investigated the relation between insulin resistance and left ventricular mass on both obese and hypertensive subjects with varying results. Some studies found a relation between insulin resistance and left ventricular mass (29,30), whereas others found no relation at all after adjusting for covariates. In the present study, the associated cardiovascular risk factors (more in specific parameters of carbohydrate and lipid metabolism) did not predict a significant portion of adverse LV remodelling and of diastolic dysfunction when adjusted for obesity.
Limitations.
There are some limitations to consider in the interpretation of our results. The current study was cross-sectional in design; therefore, temporal associations between obesity, blood pressure elevation, metabolic factors, and cardiac structure and function could not be evaluated. Follow-up studies should be helpful in elucidating the cause-and-effect relations and the underlying mechanism. In addition, there may be selection bias toward children with increased morbidity as this is a referral population.
In conclusion, this study has demonstrated that young, obese children and adolescents have significant changes in left ventricular wall dimensions and early diastolic filling compared with nonobese subjects. Obesity per se and not the associated cardiovascular risk factors (parameters of carbohydrate and lipid metabolism) predicted the early cardiac abnormalities. TDI proved to have additional value in the evaluation of ventricular filling in this population.
Abbreviations
- LV:
-
left ventricle
- LVM:
-
left ventricular mass = {1.04[(IVSd + LVIDd + LVPWd)3 − (LVIDd)3] − 13.6 g)
References
Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP 1999 The spread of the obesity epidemic in the United States, 1991–1998. JAMA 282: 1519–1522
Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM 2004 Prevalence of overweight and obesity among US children, adolescents, and adults 1999–2002. JAMA 291: 2847–2850
Alpert MA 2001 Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. Am J Med Sci 321: 225–236
de Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, de Divitiis O, Alderman MH 1992 Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol 20: 1251–1260
Kono Y, Yoshinaga M, Oku S, Nomura Y, Nakamura M, Aihoshi S 1994 Effect of obesity on echocardiographic parameters in children. Int J Cardiol 46: 7–13
Yoshinaga M, Yuasa Y, Hatano H, Kono Y, Nomura Y, Oku S, Nakamura M, Kanekura S, Otsubo K, Akiba S, Miyata K 1995 Effect of total adipose weight and systemic hypertension on left-ventricular mass in children. Am J Cardiol 76: 785–787
Daniels SR, Kimball TR, Morrison JA, Khoury P, Witt S, Meyer RA 1995 Effect of lean body mass, fat mass, blood pressure, and sexual maturation on left ventricular mass in children and adolescents. Statistical, biological, and clinical significance. Circulation 92: 3249–3254
Goran MI, Gower BA 1998 Abdominal obesity and cardiovascular risk in children. Coron Artery Dis 9: 483–487
Caprio S 2002 Insulin resistance in childhood obesity. J Pediatr Endocrinol Metab 15: 487–492
Steinberger J, Daniels SR 2003 Obesity, insulin resistance, diabetes, and cardiovascular risk in children: an American heart association scientific statement from the atherosclerosis, hypertension, and obesity in the young committee (Council on Cardiovascular Disease in the Young) and the diabetes committee (Council on Nutrition, Physical Activity, and Metabolism). Circulation 107: 1448–1453
Hennekens CH, Schneider WR, Barice EJ 2007 Obesity in childhood: introduction and general considerations. Pediatr Res 61: 634–635
Aggoun Y 2007 Obesity, metabolic syndrome, and cardiovascular disease. Pediatr Res 61: 653–659
Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, Allen K, Lopes M, Savoye M, Morrison J, Sherwin RS, Caprio S 2004 Obesity and the metabolic syndrome in children and adolescents. N Engl J Med 350: 2362–2374
Cole TJ, Freeman JV, Preece MA 1998 British 1990 growth reference centiles for weight, height, body mass index and head circumference fitted by maximum penalized likelihood. Stat Med 17: 407–429
Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, Quon MJ 2000 Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab 85: 2402–2410
Devereux RB, Lutas EM, Casale PN, Kligfield P, Eisenberg RR, Hammond IW, Miller DH, Reis G, Alderman MH, Laragh JH 1984 Standardization of M-mode echocardiographic left ventricular anatomic measurements. J Am Coll Cardiol 4: 1222–1230
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ, Tajik AJ, Seward JB 1995 New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function–a study in normals and dilated cardiomyopathy. J Cardiol 26: 357–366
Li X, Li S, Ulusoy E, Chen W, Srinivasan SR, Berenson GS 2004 Childhood adiposity as a predictor of cardiac mass in adulthood: the Bogalusa heart study. Circulation 110: 3488–3492
Lauer MS, Anderson KM, Kannel WB, Levy D 1991 The impact of obesity on left ventricular mass and geometry. The Framingham heart study. JAMA 266: 231–236
Chinali M, de Simone G, Roman MJ, Lee ET, Best LG, Howard BV, Devereux RB 2006 Impact of obesity on cardiac geometry and function in a population of adolescents: the strong heart study. J Am Coll Cardiol 47: 2267–2273
Lauer MS, Lauer MF, Anderson KM, Anderson KM, Levy D, Levy D 1992 Separate and joint influences of obesity and mild hypertension on left ventricular mass and geometry: the Framingham heart study. J Am Coll Cardiol 19: 130–134
Grossman E, Grossman EF, Oren S, Oren SF, Messerli FH, Messerli FH 1991 Left ventricular filling in the systemic hypertension of obesity. Am J Cardiol 68: 57–60
Alpert MA, Alpert MA, Terry BE, Terry BF, Kelly DL, Kelly DL 1985 Effect of weight loss on cardiac chamber size, wall thickness and left ventricular function in morbid obesity. Am J Cardiol 55: 783–786
Pascual M, Pascual DA, Soria F, Vicente T, Hernandez AM, Tebar FJ, Valdes M 2003 Effects of isolated obesity on systolic and diastolic left ventricular function. Heart 89: 1152–1156
Nagueh SF, Bachinski LL, Meyer D, Hill R, Zoghbi WA, Tam JW, Quinones MA, Roberts R, Marian AJ 2001 Tissue Doppler imaging consistently detects myocardial abnormalities in patients with hypertrophic cardiomyopathy and provides a novel means for an early diagnosis before and independently of hypertrophy. Circulation 104: 128–130
Yu CM, Lin H, Yang H, Kong SL, Zhang Q, Lee SW 2002 Progression of systolic abnormalities in patients with “isolated” diastolic heart failure and diastolic. Circulation 105: 1195–1201
Harada K, Orino T, Takada G 2001 Body mass index can predict left ventricular diastolic filling in asymptomatic obese children. Pediatr Cardiol 22: 273–278
Mehta SK, Holliday C, Hayduk L, Wiersma L, Richards N, Younoszai A 2004 Comparison of myocardial function in children with body mass indexes >/=25 versus those <25 kg/m2. Am J Cardiol 93: 1567–1569
Sasson Z, Rasooly Y, Bhesania T, Rasooly I 1993 Insulin resistance is an important determinant of left ventricular mass in the obese. Circulation 88: 1431–1436
Urbina EM, Gidding SS, Bao W, Elkasabany A, Berenson GS 1999 Association of fasting blood sugar level, insulin level, and obesity with left ventricular mass in healthy children and adolescents: the Bogalusa heart study. Am Heart J 138: 122–127
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by Belgian National Foundation for Research in Pediatric Cardiology.
Rights and permissions
About this article
Cite this article
van Putte-Katier, N., Rooman, R., Haas, L. et al. Early Cardiac Abnormalities in Obese Children: Importance of Obesity Per Se Versus Associated Cardiovascular Risk Factors. Pediatr Res 64, 205–209 (2008). https://doi.org/10.1203/PDR.0b013e318176182b
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e318176182b
This article is cited by
-
Sacubitril/valsartan inhibits obesity-associated diastolic dysfunction through suppression of ventricular-vascular stiffness
Cardiovascular Diabetology (2021)
-
Cardiac function in adolescents with obesity: cardiometabolic risk factors and impact on physical fitness
International Journal of Obesity (2019)
-
Impact of Obesity on Left Ventricular Thickness in Children with Hypertrophic Cardiomyopathy
Pediatric Cardiology (2019)
-
The role of dipeptidylpeptidase-4 inhibitors in management of cardiovascular disease in diabetes; focus on linagliptin
Cardiovascular Diabetology (2018)
-
Has the Time Come to Be More Aggressive With Bariatric Surgery in Obese Patients With Chronic Systolic Heart Failure?
Current Heart Failure Reports (2018)