Abstract
Identifying antagonist peptides able to inhibit the abnormal immune response triggered by gliadin peptides in celiac disease (CD) is an alternative therapeutic strategy for CD. The aim of this study was to evaluate the antagonist effect of 10mer, a decapeptide (sequence QQPQDAVQPF) from alcohol-soluble protein fraction of durum wheat, assessing its ability to prevent celiac peripheral blood lymphocytes from activation by gliadin peptides. Peripheral blood mononuclear cells (PBMC) were obtained from DQ2-positive untreated coeliac children and from healthy controls and incubated with the peptic-tryptic digest of bread wheat gliadin (GLP) and peptide 62–75 from α-gliadin both alone and with 10mer simultaneously. PBMC proliferation, release of pro-inflammatory Th1 cytokines interferon-γ and tumor necrosis factor-α, release of immunoregulatory cytokine IL-10, and analysis of CD25 expression as indexes of lymphocytes activation were carried out. Enhanced lymphocytes activation was seen after exposure to GLP and p62–75, whereas the simultaneous incubation with 10mer inhibits the lymphocytes response. These data indicate that a peptide naturally occurring in durum wheat exerts in vitro an antagonist effect against gliadin toxicity and could have a protective effect in CD disease.
Similar content being viewed by others
Main
CD is an increasingly diagnosed auto-immune enteropathy (prevalence 1:150), driven by an abnormal T-cell response to wheat gluten–derived peptides and strongly associated with HLA-DQ2, which is present in more than 90% of CD patients (1–3). So far, the only effective treatment is the withdrawal of the gluten-containing cereals from the diet (4). Complying with a gluten-free diet is difficult because of the diffusion of the cereals-based foods and it affects patients' quality of life; therefore, new treatments are being actively searched.
An alternative therapeutic possibility may be to identify modified gliadin (a gluten fraction) peptides that are not toxic and are also able to inhibit the pathogenic immune response. In fact, some single amino acid substitutions at critical position of T-cell epitopes convert highly toxic peptides in ligand antagonists, as tested both in animal and ex vivo models (5,6). It has been reported that some peptides obtained by amino acid modifications of peptide 57–73 from α-gliadin abolish the production of interferon (IFN)-γ by celiac PBMC incubated with the p57–73 itself (7).
This therapeutic strategy could also rely upon ligand antagonists naturally occurring in some grains, such as a decapeptide (10mer) identified in the peptic-tryptic digest of the alcohol-soluble protein fraction of durum wheat (GLP) (8). This molecule, whose sequence is QQPQDAVQPF, named in previous studies “1157” after its molecular weight, has been demonstrated to protect some cellular lines from gliadin toxicity (8,9).
Although in CD pathogenesis the central role is played by gluten-specific HLA DQ2/DQ8 restricted CD4+ intestinal T cells, recent studies indicate that the peripheral blood lymphocytes from celiac patients could be as informative as the intestinal ones. Polyclonal effector T-cell lines appear in the peripheral blood after in vivo gluten challenge and are able to secrete inflammatory cytokines after in vitro stimulation with gliadin peptides (7,10,11). In addition, the PBMC from celiac patients on a gluten-containing diet secrete inflammatory cytokines, express activation markers, and show immunologic modifications after incubation with gliadin (12–17). So, peripheral blood lymphocytes provide a system for rapid and easy assessment of the toxicity of gluten epitopes and the antagonist effects of ligand peptides.
In this study, fresh PBMC from celiac patients on a gluten-containing diet are used to define the antagonist effect of 10mer against the ability of gliadin peptides to induce the activation of the immune system. As gliadin peptides, the whole peptic-tryptic digestion of alcohol-soluble protein fraction of wheat and the α-gliadin sequence 62–75 have been used.
MATERIALS AND METHODS
Peptic-tryptic digestion.
The alcohol-soluble protein fraction from whole cereal flour of bread wheat (Triticum aestivum, variety S. Pastore) was extracted and subjected to peptic-tryptic digestion, as previously described (18). Gliadin preparations were assayed for endotoxin by using the QCL-100 reagent kit (BioWhittaker, Walkersville, MD) and found to have endotoxin levels of <0.5 EU/mL.
Peptide 10mer and P62–75.
The sequence of peptide 10mer (MW, 1157 D) was identified in the alcohol-soluble protein fraction of durum wheat (Triticum durum, variety Adamello) by De Vincenzi et al. (8). P62–75 contains one of the two overlapping 9-aminoacid sequences within the p57–73, a HLA-DQ2–restricted peptide able to induce an intestinal T-cell response in celiac patients (19). The peptides 10mer and p62–75 were synthesized (Primm Company, Milan, Italy) by the solid phase method using Applied Biosystems' (Foster City, CA) model 431A and purified up to 99% by reverse-phase HPLC on Varian 5020 system. The details of the peptides are listed in Table 1.
Transglutaminase deamidation.
To deamidate GLP, p62–75, and 10mer, they were incubated for 4 h at 37 C° in a mix consisting of 100 μg/mL guinea pig liver tTG, 2 mM CaCl, and 400 μL GLP, p62–75, or 10mer. All reagents were purchased from Sigma Chemical Co., St. Louis, MO.
Study population.
Ten children with biopsy-proven CD were studied (7 females, 3 males; mean age, 6.2 y; range, 3–14 y). All of them showed signs and symptoms suggesting CD and underwent diagnostic gastroduodenal endoscopy. They were on an unrestricted diet at the moment of enrollment in the present study. The mucosa of all patients showed total villous atrophy at histologic examination. CD diagnosis was made according to ESPGHAN criteria (20). All of them resulted positive for the presence of serum Ab anti-tTG. The control group consisted of five healthy sex-, age-, and DQ-matched children (Ab anti-tTG negative), referred to medical examination for nonspecific gastrointestinal symptoms, with no evidence of disease at histologic examination of small intestine. The peripheral blood samples were taken the same day of the endoscopic examination. Table 2 shows the clinical details of the subjects studied. The Ethics Committee of Istituto Superiore di Sanità approved the study (CE-ISS-05/112) and informed consent was obtained.
DQ2 determination. The HLA-DQA and DQB genotype of all subjects was determined using peripheral blood DNA and PCR with sequence-specific primer mixes (21–23).
Separation of PBMC and cell cultures.
PBMC were isolated from 6 mL of heparinized blood by Lympholyte-H (Cederlane, Hornby, Ontario, Canada) gradient centrifugation and cultured at a density of 1.0 × 106 cells per milliliter in 96-multiwell culture plates in RPMI 1640 culture medium supplemented with 10% fetal bovine serum, streptomycin (50 ng/mL), and penicillin (100 μg/mL). All these products were purchased from GIBCO-Invitrogen Ltd. (Paisley, UK). After 24 h, PBMC were incubated with GLP (0.5 mg/mL), p62–75 (10 μg/mL), Ab anti-CD3 (10 μg/mL) (DAKO, Copenhagen, Denmark), and 10mer (10 μg/mL), both alone and in combination. After 24 h stimulation, the PBMC were harvested for Western blotting and the free supernatants were collected and stored at –80°C until cytokine analyses.
Cell proliferation assay.
To assess the effect of the treatments on the PBMC proliferation, the BrdU cell proliferation test (Chemicon International, Temecula, CA) was carried out. Measurements were performed after 24, 48, 72, and 96 h of incubation, by an ELISA reader (Bio-Rad, Hercules, CA) at 450/550 nm.
Cytokines determination.
Tumor necrosis factor (TNF)-α, IFN-γ, and IL-10 concentrations were determined in PBMC supernatant samples by commercially available ELISA kits, according to the manufacturer's instructions (BioSource International, Camarillo, CA). Standards were run on each plate. Samples from the different patients were run at the same time.
Cell apoptosis and cellular staining procedure.
Apoptosis of PBMC was studied with DNA strand breaks on the terminal deoxynucleotidyl transferase-mediated dUTP nick end-labeling (TUNEL) kit (Roche Molecular Biochemicals, Mannheim, Germany). Briefly, the cells were fixed with 2% paraformaldehyde for 30 min at 4°C, washed (for 5 min at 1500 g) with PBS (Invitrogen, Carlsbad, CA) and permeabilized for 2 min on ice with 0.1%Triton X-100 0.1% sodium citrate. After washing, cells were decanted and resuspended in 50 μL of TUNEL mixture solution or in 50 μL of TUNEL labeled as a negative control. After 60 min of incubation at 37°C in a humidified atmosphere, cells were washed three times with PBS. After staining, cells were analyzed using Epics Elite ESP Flow-Cytometer (Beckman Coulter, Inc., Fullerton, CA) acquiring 10,000 events.
Western blotting.
After 24 h exposure to GLP (0.5 mg/mL), p62–75 (10 μg/mL), alone and in combination with p10mer (10 μg/mL), proteins from PBMC were obtained by lysis in a buffer containing 10 mM Tris-HCl pH 8, 0.5 mM EDTA, 1% Triton X-100, 100 mM sodium ortho vanadate, and protease inhibitors. The proteins were measured using the Lowry method.
For CD25 detection, 100 μg of proteins were heat-denatured and separated on SDS-10% polyacrylamide gels. The proteins were transferred to nitrocellulose membranes and incubated 1 h at room temperature with a monoclonal anti-CD25 (DakoCytomation Denmark A/S, Glostrup, Denmark) at a dilution of 1:500. Signals were detected with the use of an anti-mouse antibody coupled to horseradish peroxidase at a dilution of 1:3000 (Bio-Rad) and enhanced chemiluminescence was performed according to the manufacturer's instructions (Pierce, Rockford, IL). Gels were scanned using Chemidoc densitometer (Bio-Rad, Hercules, CA) and values were normalized to those obtained with an actin MAb (1:2500, Chemicon International).
Statistical analysis.
Each experiment was carried out in triplicate on three different days. Data are expressed as mean ± SEM. Comparisons between mean values were carried out using one-factor ANOVA followed by t test for each group. A p value <0.05 was considered statistically significant. All statistics were performed using SPSS software (SPSS Inc., Chicago, IL).
RESULTS
Cell proliferation assay.
To assess lymphocytes proliferation after the exposure to different peptides, BrdU cell proliferation assay was performed. This colorimetric assay consists of the immunochemical measurement of the incorporation of bromodeoxyuridine, a thymidine analog, into newly synthesized DNA stands of actively proliferating DNA. The proliferation of PBMC exposed to the different treatments has been expressed as mean percentage with respect to lymphocytes exposed to medium only (controls). Figure 1 shows that the PBMC proliferation up to fourth day of incubation was increased after treatment with gliadin peptides and the simultaneous exposure to 10mer abolished it, showing values similar to controls.
Proliferation of PBMC from celiac patients (n = 10) after 1, 2, 3, and 4 d of treatment with GLP (0.5 mg/mL, ▴ panel A), p62–75 (10 μg/mL, ♦ panel B), and 10mer (10 μg/mL) alone (•) and in combination (▪, ▾). Values are reported as percentage of control determined by BrdU assay and are the mean ± SEM of three different experiments for each patient. Statistical analysis was performed by one-factor ANOVA, followed by t test for each group. Panels A and B, *p < 0.0001. Panel A: *GLP vs 10mer, *GLP vs 10mer + GLP, *10mer vs 10mer + GLP; panel B: *p62–75 vs 10mer, *p62–75 vs 10mer + p62–75, *10mer vs 10mer + p62–75.
The proliferation of PBMC from healthy controls shows no statistically significant differences between the lymphocytes treated with gliadin peptides compared with the control.
Cytokines production.
The antagonist effect of 10mer against the gliadin peptides activation of PBMC has been tested using a commercial kit for the determination of the levels of IFN-γ and TNF-α. Antagonism was measured as mean percentage reduction or increase of cytokines release in supernatants compared with incubation with medium alone. The exposure of celiac PBMC to GLP and p62–75 significantly increases the release of both IFN-γ and TNF-α (158% and 142%, respectively), whereas the simultaneous incubation with 10mer results in a cytokines production similar to the control (Figs. 2 and 3). No significant increase of cytokines release by PBMC from healthy controls after incubation with GLP and p62–75 compared with the control was noticed.
TNF-α responses of PBMC from celiac patients (n = 10) to GLP (0.5 mg/mL,  panel A), p62–75 (10 μg/mL,
panel A), p62–75 (10 μg/mL,  panel B), and 10mer (10 μg/mL) alone (□) and in combination (▪). Values are reported as percentage of control determined by ELISA and are the mean ± SEM of three different experiments for each patient. Statistical analysis was performed by one-factor ANOVA (panel A, p < 0.0001; panel B, p < 0.0001) followed by t test for each group. πp < 0.0001; §p < 0.001; **p < 0.01; *p < 0.05. Panel A: π10mer vs GLP; §GLP vs GLP + 10mer; *10mer vs GLP + 10mer; panel B: §10mer vs p62–75, p62–75 + 10mer **p62–75 vs p62–75 + 10mer.
panel B), and 10mer (10 μg/mL) alone (□) and in combination (▪). Values are reported as percentage of control determined by ELISA and are the mean ± SEM of three different experiments for each patient. Statistical analysis was performed by one-factor ANOVA (panel A, p < 0.0001; panel B, p < 0.0001) followed by t test for each group. πp < 0.0001; §p < 0.001; **p < 0.01; *p < 0.05. Panel A: π10mer vs GLP; §GLP vs GLP + 10mer; *10mer vs GLP + 10mer; panel B: §10mer vs p62–75, p62–75 + 10mer **p62–75 vs p62–75 + 10mer.
IFN-γ responses of PBMC from celiac patients (n = 10) to GLP (0.5 mg/mL,  panel A), p62–75 (10 μg/mL,
panel A), p62–75 (10 μg/mL,  panel B), and 10mer (10 μg/mL) alone (□) and in combination (▪). Values are reported as percentage of control determined by ELISA and are the mean ± SEM of three different experiments for each patient. Statistical analysis was performed by one-factor ANOVA (panel A: p < 0.0001; panel B: p < 0.0001) followed by t test for each group. π p < 0.0001. Panel A: π10mer vs GLP; GLP vs GLp + 10mer; 10mer vs GLp + 10mer. Panel B: 10mer vs p62–75; p62–75 + 10mer p62–75 vs>p62–75 + 10mer.
panel B), and 10mer (10 μg/mL) alone (□) and in combination (▪). Values are reported as percentage of control determined by ELISA and are the mean ± SEM of three different experiments for each patient. Statistical analysis was performed by one-factor ANOVA (panel A: p < 0.0001; panel B: p < 0.0001) followed by t test for each group. π p < 0.0001. Panel A: π10mer vs GLP; GLP vs GLp + 10mer; 10mer vs GLp + 10mer. Panel B: 10mer vs p62–75; p62–75 + 10mer p62–75 vs>p62–75 + 10mer.
Figure 4 clearly shows that the incubation of peripheral lymphocytes with GLP or p62–75 simultaneously to 10mer resulted in an increase of IL-10 release in the culture medium with respect to GLP and p62–75 alone (110% versus 125% and 102% versus 140%, respectively).
IL-10 responses of PBMC from celiac patients (n = 10) to GLP (0.5 mg/mL,  panel A), p62–75 (10 μg/mL,
panel A), p62–75 (10 μg/mL,  panel B), and 10mer (10 μg/mL) alone (□) and in combination (▪). Values are reported as percentage of control determined by ELISA and are the mean ± SEM of three different experiments for each patient. Statistical analysis was performed by one-factor ANOVA (panel A: p < 0.0001; panel B: p < 0.0001) followed by t test for each group. *p < 0.0001. Panel B: *10mer vs p62–75, p62–75 + 10mer.
panel B), and 10mer (10 μg/mL) alone (□) and in combination (▪). Values are reported as percentage of control determined by ELISA and are the mean ± SEM of three different experiments for each patient. Statistical analysis was performed by one-factor ANOVA (panel A: p < 0.0001; panel B: p < 0.0001) followed by t test for each group. *p < 0.0001. Panel B: *10mer vs p62–75, p62–75 + 10mer.
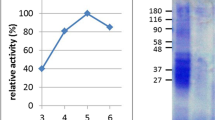
CD25 expression.
CD25 expression was analyzed by Western blotting using proteins extracted from PBMC incubated with gliadin peptides and 10mer, both alone and simultaneously.
All samples showed transcripts for CD25 (Fig. 5). However, the analysis of the ratio CD25/β-actin bands showed a marked increase of the expression of CD25 in PBMC treated with GLP and p62–75, compared with lymphocytes treated with medium alone and with 10mer simultaneously to gliadin peptides. Figure 5 shows also the mean ± SEM. CD25 protein expressions after the different treatment in densitometry arbitrary units. Even if the arbitrary unit does not reflect the real quantities of the proteins in the cells, the fact that the intensity of the bands from lymphocytes incubated with the gliadin peptides alone was increased compared with the intensity of the bands from cells treated simultaneously with 10mer in all samples suggests that this expression is really higher after GLP and p62–75 treatment.
CD25 expression of PBMC from celiac patients (n = 10) to GLP (0.5 mg/mL, panel A), p62–75 (10 μg/mL, panel B) and 10mer (10 μg/mL) alone and in combination. Values are expressed as mean ± SEM in densitometry arbitrary units of three different experiments for each patient. The figure illustrates one of three separate experiments which gave similar results. Statistical analysis was performed by one-factor ANOVA (panel A: p < 0.001; panel B: p < 0.001) followed by t test for each group. **p < 0.01; *p < 0.05. Panel A: **PBMC vs 10mer, GLP; *10mer vs GLP, GLP + 10mer. Panel B: **PBMC vs 10mer, p62–75; *PBMC vs p62-67, p62–75 + 10mer.
Activation induced by anti-CD3.
To assess whether the antagonist effect of 10mer is specific against gliadin peptides, the incubation of PBMC with anti-CD3 and 10mer simultaneously was carried out. Figure 6 demonstrates that the simultaneous exposure to 10mer is not able to suppress the increased production of pro-inflammatory cytokine IFN-γ induced by the anti-CD3.
IFN-γ responses of PBMC from coeliac patients (n = 10) to anti CD3 (10 μg/mL,  ) and 10mer (10 μg/mL) alone (□) and in combination (▪). Values are reported as percentage of control determined by ELISA and are the mean ± SEM of three different experiments for each patient. Statistical analysis was performed by one factor ANOVA (panel A: p < 0.0001; panel B: p < 0.0001) followed by t test for each group. *p < 0.0001.*10mer vs antiCD3; antiCD3 + 10mer.
) and 10mer (10 μg/mL) alone (□) and in combination (▪). Values are reported as percentage of control determined by ELISA and are the mean ± SEM of three different experiments for each patient. Statistical analysis was performed by one factor ANOVA (panel A: p < 0.0001; panel B: p < 0.0001) followed by t test for each group. *p < 0.0001.*10mer vs antiCD3; antiCD3 + 10mer.
DISCUSSION
Identifying modified gliadin peptides that are not toxic and also able to inhibit the pathogenic immune response is an alternative therapeutic strategy for celiac disease. In the present article, we described for the first time the antagonist effect of a peptide naturally occurring in a cereal avoided in gluten-free diet.
Effector T cells in peripheral blood.
The system we used provides a rapid and noninvasive tool to study not only the toxicity of wheat gliadin T-cell epitopes, but also to test the antagonist effects of their variants. Differently from the study design by Anderson and colleagues (10,11), the patients enrolled in our study did not undergo the gluten challenge, but all of them were on a gluten-containing diet. The PBMC response that we obtained after exposure to GLP and p62–75, measured as cell proliferation and IFN-γ and TNF-α production, shows that the effector T cells are equally present in peripheral blood of our patients and support the assumption of a continuous recirculation of activated immune cells between the intestine and the peripheral blood in celiac patients, not only after the gluten challenge but also in children on gluten-containing diets, consistent with previous studies (13,14,24,25). The lack of stimulation of PBMC from healthy controls by gliadin peptides shows that the immune response we obtained is CD specific.
Effects of co-incubation of PBMC with 10mer and gliadin peptides.
The simultaneous exposure of PBMC to 10mer and gliadin peptides clearly decrease the activation of celiac PBMC measured as proliferation and proinflammatory cytokines production and CD25 (IL-2R) expression. IL-10 is an important immunoregulatory cytokine that acts on antigen presenting cells inhibiting the inflammatory cytokines synthesis and the expression of costimulatory and MHC class II molecules (26,27). In addition, it interferes with T-cell proliferation and differentiation (28,29). What's more, recombinant IL-10 has been demonstrated to suppress gliadin specific T-cell activation and induce a long-term hyporesponsiveness of gliadin-specific mucosal T cells (30). It is intriguing that 10mer incubated with p62–75 increased significantly the release of IL-10 by lymphocytes, indicating that this peptide is able to down-regulate the immune response in CD. In contrast, the results about IL-10 release after incubation with 10mer and GLP are not statistically significant. This is because IL-10 response to 10mer and GLP in lymphocytes from three patients was similar to medium alone. Polyclonal-specific T cells present in PBMC are much more heterogeneous than the lamina propria T-cell clones and GLP is a mixture of different peptides that could have different effects on IL-10 production.
The fact that 10mer was not able to prevent the lymphocyte activation induced by the incubation with anti-CD3 points out its specific inhibitory effect against gliadin peptides.
We did not obtain significant results about PBMC apoptosis by fluorescence-activated cell sorting (FACS)-based analysis (data not shown) because of the very low frequency of relevant T cells, in agreement with the results described by Anderson et al. (7).
It is interesting also that the incubation with 10mer alone decreases the CD25 expression. This finding can be explained by the fact that the PBMC were from patients on a gluten-containing diet, so the resulting PBMC were already activated.
Antagonist mechanism of 10mer.
Even if investigating the mechanism responsible for the antagonist effect of 10mer is beyond the scope of the work, the amino acid sequence of 10mer is strongly suggestive of the fact that it could interfere with T-cell recognition of gliadin immunodominant peptides.
The presence of alanine in P6 of 10mer is very interesting. Glutamine residues formed by tTG-mediated deamidation are particularly critical for T-cell recognition when localized in P6 (32). Therefore, the substitution of glutamine in this position with alanine, a small neutral amino acid, in the immunogenic peptide sequence is a widely accepted approach to design antagonists (7,33). Another feature likely responsible for the antagonist effect of the 10mer is the presence of the residue of aspartic acid in P5. This amino acid is very rare in prolamin sequences and is absent in the known immunogenic peptides. We have previously shown that the deletion of the of aspartic residue results in an inactive peptide, thus indicating the importance of this residue for the antagonist effect (34).
The concentration of 10mer used for the experiments (10 μg/mL ) is the lowest we noticed to suppress IFN-γ release by PBMC against both p62–75 used at concentration of 10 μg/mL and gliadin peptides used at concentration of 0.5 mg/mL, respectively. Below that concentration, no antagonist effect of 10mer was detected (data not shown).
10mer in immunotherapy.
Identifying modified gliadin T-cell epitopes able to inhibit the toxicity of the grains is a therapeutic strategy for CD actively pursued. At the moment, different approaches have been appointed to design such antagonists. Similar to antagonist sequences so far known, 10mer could be proposed as an orally administrated T-cell modulating agent, since it significantly down-regulates the production of IFN-γ and TNF-α, two of major proinflammatory cytokines in Th1/Th0–mediated disease such as CD, and lowers the expression of CD25 (IL-2R), a lymphocyte activation markers.
Differently from the antagonists peptides so far identified, which are artificially synthesized, 10mer naturally occurs in durum wheat and a potential use for this information would be the production of a nontoxic wheat, in which the genome-encoding 10mer would be over-expressed. This will offer a cereal with the nutritional and cooking qualities of the native cultivars, but not triggering CD. However, further studies are required to validate the utilization of 10mer in immunotherapy. These results should be verified using celiac small intestinal T-cell lines and in vitro culture of small bowel mucosa before in vivo study could be considered.
Intriguingly, the presence of 10mer in the protein fraction of durum wheat could also account for the lower toxicity that gliadin peptides from durum wheat showed in small intestine cultures from celiac children (35). Recent articles pointed out that the lack of genome DD in durum wheat does not accounts by itself for lower toxicity of this grain in CD (36,37). Indeed, we don't have data to confirm that, since investigating the reasons for the lower toxicity of durum wheat for CD patients is beyond the scope of this study.
In conclusion, our data indicate that a peptide naturally occurring in alcohol-soluble protein fraction of durum wheat acts in vitro as antagonist of gliadin peptides. These findings suggest new therapeutic approaches for CD relying on peptides naturally occurring in toxic cereals.
Abbreviations
- BrdU:
-
5-bromo-2-deoxyuridine
- CD:
-
celiac disease
- GLP:
-
gliadin peptides
- PBMC:
-
peripheral blood mononuclear cells
- tTG:
-
tissue transglutaminase
References
Hin H, Bird G, Fisher P, Mahy N, Jewell D 1999 Coeliac disease in primary care: case finding study. BMJ 318: 164–167
Kendall MJ, Schneider R, Cox PS, Hawkins CF 1972 Gluten subfractions in coeliac disease. Lancet 2: 1065–1067
Sollid LM, Thorsby E 1993 HLA susceptibility genes in celiac disease: genetic mapping and role in pathogenesis. Gastroenterology 105: 910–922
Fasano A, Catassi C 2001 Current approaches to diagnosis and treatment of celiac disease: an evolving spectrum. Gastroenterology 120: 636–651
Klenerman P, Rowland-Jones S, McAdam S, Edwards J, Daenke S, Lalloo D, Koppe B, Rosenberg W, Boyd D, Edwards A, Giangrande P, Phillips RE, McMichael AJ 1994 Cytotoxic T-cell activity antagonized by naturally occurring HIV-1 Gag variants. Nature 369: 403–407
Bertoletti A, Sette A, Chisari FV, Penna A, Levrero M, De Carli M, Fiaccadori F, Ferrari C 1994 Natural variants of cytotoxic epitopes are T-cell receptor antagonists for antiviral cytotoxic T cells. Nature 369: 407–410
Anderson RP, van Heel DA, Tye-Din JA, Jewell DP, Hill AV 2006 Antagonists and non-toxic variants of the dominant wheat gliadin T-cell epitope in coeliac disease. Gut 55: 485–491
De Vincenzi M, Gasbarrini G, Silano V 1997 A small peptide from durum wheat gliadin prevents cell agglutination induced by prolamin-peptides toxic in coeliac disease. Toxicology 120: 207–213
Giovannini C, Matarrese P, Scazzocchio B, Vari R, D'Archivio M, Straface E, Masella R, Malorni W, De Vincenzi M 2003 Wheat gliadin induces apoptosis of intestinal cells via an autocrine mechanism involving Fas-Fas ligand pathway. FEBS Lett 540: 117–124
Anderson RP, Degano P, Godkin AJ, Jewell DP, Hill AV 2000 In vivo antigen challenge in celiac disease identifies a single transglutaminase-modified peptide as the dominant A-gliadin T-cell epitope. Nat Med 6: 337–342
Anderson RP, van Heel DA, Tye-Din JA, Barnardo M, Salio M, Jewell DP, Hill AV 2005 T cells in peripheral blood after gluten challenge in coeliac disease. Gut 54: 1217–1223
Di Sabatino A, Bertrandi E, Casadei Maldini M, Pennese F, Proietti F, Corazza GR 1998 Phenotyping of peripheral blood lymphocytes in adult coeliac disease. Immunology 95: 572–576
Nilsen EM, Lundin KE, Krajci P, Scott H, Sollid LM, Brandtzaeg P 1995 Gluten specific, HLA-DQ restricted T cells from coeliac mucosa produce cytokines with Th1 or Th0 profile dominated by interferon gamma. Gut 37: 766–776
Lahat N, Shapiro S, Karban A, Gerstein R, Kinarty A, Lerner A 1999 Cytokine profile in coeliac disease. Scand J Immunol 49: 441–446
Lahat N, Ben-Nun A, Cohen L, Kinarty A, Lerner A 1995 T cell receptor repertoire in the peripheral blood and intestinal mucosa of coeliac patients. Clin Exp Immunol 101: 422–427
O'Keeffe J, Mills K, Jackson J, Feighery C 1999 T cell proliferation, MHC class II restriction and cytokine products of gliadin-stimulated peripheral blood mononuclear cells. Clin Exp Immunol 117: 269–276
Di Sabatino A, D'Alo S, Millimaggi D, Ciccocioppo R, Parroni R, Sciarra G, Cifone MG, Corazza GR 2001 Apoptosis and peripheral blood lymphocyte depletion in coeliac disease. Immunology 103: 435–440
De Ritis G, Occorsio P, Auricchio S, Gramenzi F, Morisi G, Silano V 1979 Toxicity of wheat flour proteins and protein-derived peptides for in vitro developing intestine from rat fetus. Pediatr Res 13: 1255–1261
Ellis HJ, Pollock EL, Engel W, Fraser JS, Rosen-Bronson S, Wieser H, Ciclitira PJ 2003 Investigation of the putative immunodominant T cell epitopes in coeliac disease. Gut 52: 212–217
Working group of European Society of Paediatric Gastroenterology and Nutrition 1990 Revised criteria for diagnosis of coeliac disease. Arch Dis Child 65: 909–911
Bunce M, O'Neill CM, Barnardo MC, Krausa P, Browning MJ, Morris PJ, Welsh KI 1995 Phototyping: comprehensive DNA typing for HLA-A, B, C, DRB1, DRB3, DRB4, DRB5 & DQB1 by PCR with 144 primer mixes utilizing sequence-specific primers (PCR-SSP). Tissue Antigens 46: 355–367
Olerup O, Aldener A, Fogdell A 1993 HLA-DQB1 and -DQA1 typing by PCR amplification with sequence-specific primers (PCR-SSP) in 2 hours. Tissue Antigens 41: 119–134
Mullighan CG, Bunce M, Welsh KI 1997 High-resolution HLA-DQB1 typing using the polymerase chain reaction and sequence-specific primers. Tissue Antigens 50: 688–692
Mackay CR 1991 T-cell memory: the connection between function, phenotype and migration pathways. Immunol Today 12: 189–192
Kerttula TO, Hallstrom O, Maki M 1995 Phenotypical characterization of peripheral blood T cells in patients with coeliac disease: elevation of antigen-primed CD45RO+ T lymphocytes. Immunology 86: 104–109
Fiorentino DF, Zlotnik A, Vieira P, Mosmann TR, Howard M, Moore KW, O'Garra A 1991 IL-10 acts on the antigen-presenting cell to inhibit cytokine production by Th1 cells. J Immunol 146: 3444–3451
Fiorentino DF, Zlotnik A, Mosmann TR, Howard M, O'Garra A 1991 IL-10 inhibits cytokine production by activated macrophages. J Immunol 147: 3815–3822
Taga K, Mostowski H, Tosato G 1993 Human interleukin-10 can directly inhibit T-cell growth. Blood 81: 2964–2971
de Waal Malefyt R, Yssel H, de Vries JE 1993 Direct effects of IL-10 on subsets of human CD4+ T cell clones and resting T cells. Specific inhibition of IL-2 production and proliferation. J Immunol 150: 4754–4765
Salvati VM, Mazzarella G, Gianfrani C, Levings MK, Stefanile R, De Giulio B, Iaquinto G, Giardullo N, Auricchio S, Roncarolo MG, Troncone R 2005 Recombinant human interleukin 10 suppresses gliadin dependent T cell activation in ex vivo cultured coeliac intestinal mucosa. Gut 54: 46–53
Sollid LM 2002 Coeliac disease: dissecting a complex inflammatory disorder. Nat Rev Immunol 2: 647–655
Qiao SW, Bergseng E, Molberg O, Jung G, Fleckenstein B, Sollid LM 2005 Refining the rules of gliadin T cell epitope binding to the disease-associated DQ2 molecule in celiac disease: importance of proline spacing and glutamine deamidation. J Immunol 175: 254–261
Biagi F, Ellis HJ, Parnell ND, Shidrawi RG, Thomas PD, O'Reilly N, Corazza GR, Ciclitira PJ 1999 A non-toxic analogue of a coeliac-activating gliadin peptide: a basis for immunomodulation?. Aliment Pharmacol Ther 13: 945–950
De Vincenzi M, Stammati A, Luchetti R, Silano M, Gasbarrini G, Silano V 1998 Structural specificities and significance for coeliac disease of wheat gliadin peptides able to agglutinate or to prevent agglutination of K562(S) cells. Toxicology 127: 97–106
Auricchio S, De Ritis G, De Vincenzi M, Occorsio P, Silano V 1982 Effects of gliadin-derived peptides from bread and durum wheats on small intestine cultures from rat fetus and coeliac children. Pediatr Res 16: 1004–1010
Molberg O, Uhlen AK, Jensen T, Flaete NS, Fleckenstein B, Arentz-Hansen H, Raki M, Lundin KE, Sollid LM 2005 Mapping of gluten T-cell epitopes in the bread wheat ancestors: implications for celiac disease. Gastroenterology 128: 393–401
van Herpen TW, Goryunova SV, van der Schoot J, Mitreva M, Salentijn E, Vorst O, Schenk MF, van Veelen PA, Koning F, van Soest LJ, Vosman B, Bosch D, Hamer RJ, Gilissen LJ, Smulders MJ 2006 Alpha-gliadin genes from the A, B, and D genomes of wheat contain different sets of celiac disease epitopes. BMC Genomics 7: 1–13
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Silano, M., Di Benedetto, R., Trecca, A. et al. A Decapeptide from Durum Wheat Prevents Celiac Peripheral Blood Lymphocytes from Activation by Gliadin Peptides. Pediatr Res 61, 67–71 (2007). https://doi.org/10.1203/01.pdr.0000250173.88049.79
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000250173.88049.79
This article is cited by
-
Qualitative traits of perennial wheat lines derived from different Thinopyrum species
Genetic Resources and Crop Evolution (2016)
-
Partial Replacement of NaCl in Bread from Durum Wheat (Triticum turgidum L subsp. durum Desf.) with KCl and Yeast Extract: Evaluation of Quality Parameters During Long Storage
Food and Bioprocess Technology (2015)
-
Two prolamin peptides from durum wheat preclude celiac disease-specific T cell activation by gluten proteins
European Journal of Nutrition (2010)