Abstract
Organic acid (OAD) and fatty acid oxidation disorders (FAOD) are inborn errors of metabolism often presenting with life-threatening metabolic decompensation followed by (irreversible) organ failure, and even death during catabolic state. Most of these diseases are considered as treatable, and metabolic decompensations can be avoided by early diagnosis and start of therapy. Confirmation of suspected diagnosis currently relies on enzymatic and mutation analyses and in vitro loading of palmitic acid in human skin fibroblast cultures. Furthermore, in some cases potentially life-threatening in vivo loading or fasting tests are still performed. In this study, we established a standardized in vitro loading test in peripheral blood mononuclear cells (PBMC) that allows reliable biochemical confirmation of a suspected diagnosis within 1 week. Patients with confirmed diagnosis of short-, medium-, very-long-chain, and long-chain 3-hydroxyacyl-CoA dehydrogenase deficiencies, methylmalonic, propionic, isovaleric acidurias, and glutaric aciduria type I were included in the study. PBMC, isolated from heparinized venous blood samples of these individuals were incubated for 5 days with palmitic acid or 2-oxoadipic acid (glutaric aciduria type I), respectively, and quantitative acylcarnitine profiling was subsequently performed in supernatants using electrospray ionization tandem mass spectrometry. All patients were clearly identified, including those with mild biochemical phenotypes who, in particular, are at risk to be missed under balanced metabolic conditions. In glutaric aciduria type I, the same results were also obtained using lymphoblasts. In conclusion, our assay allows biochemical confirmation of a number of FAOD and OAD and could easily be implemented into the confirmatory diagnostic work-up.
Similar content being viewed by others
Main
Organic acids and fatty acids comprise a group of physiologically occurring intermediates in a variety of intracellular metabolic pathways, such as catabolism of amino acids, mitochondrial β-oxidation of fatty acids, tricarboxylic acid cycle, and cholesterol biosynthesis. Organic acid (OAD) and fatty acid oxidation disorders (FAOD) are caused by autosomal recessive inherited deficiencies of single enzymes (or in the metabolism of required coenzymes) in the outlined metabolic pathways and appear with an estimated cumulative prevalence of 1:15,000 (selective screening of symptomatic patients) to 1:6000 (in expanded neonatal screening) newborns, being the most common, life-threatening group of inborn errors of metabolism (1–3). The diagnostic hallmark of OAD and FAOD is an accumulation of characteristic organic acids and/or their corresponding acylcarnitines upstream of the enzymatic block. Organic acids can be detected by gas chromatography/mass spectrometry (GC/MS) in blood, urine, and cerebrospinal fluid, and acylcarnitines by electrospray ionization–tandem mass spectrometry (MS/MS) in dried blood spots (4–9).
FAOD and OAD are treatable with mostly satisfactory outcome if diagnosed before manifestation of life-threatening metabolic decompensations (2,3,10–17). In FAOD, such as deficiencies of short-chain acyl-CoA dehydrogenase (SCADD), medium-chain acyl-CoA dehydrogenase (MCADD), very-long-chain acyl-CoA dehydrogenase (VLCADD), and long-chain 3-hydroxy-acyl-CoA dehydrogenase (LCHADD), catabolism induced by prolonged fasting or infections could trigger acute life-threatening metabolic decompensations, in particular hypoketotic hypoglycemia. Classical OAD, such as methylmalonic aciduria (MMA), propionic aciduria (PA), and isovaleric aciduria (IVA), characteristically present with metabolic acidosis, hypoglycemia, hyperketosis, elevated lactate, and hyperammonia during catabolic state, whereas cerebral OAD, such as glutaric aciduria type I (GA-I), predominantly exhibit neurologic symptoms (dystonia, ataxia, encephalopathy, seizures) (2,10,11,13–16,18–21). At present, genotype phenotype correlation in the majority of these diseases is poorly understood and remarkable variations in the disease course have been described, ranging from asymptomatic patients to fatal course after neonatal onset (10,15,22–27).
FAOD and most OAD can be detected by a specific pattern of acylcarnitines using MS/MS. Implementation of MS/MS to expanded neonatal screening programs allows an early diagnosis and treatment of affected children (3,5,9,17,28,29). However, in some of these diseases, children under balanced metabolic conditions or those with mild biochemical phenotype may present with an intermittently normal acylcarnitine profile and, thus, are at risk for being missed. Confirmation of diagnosis in FAOD and OAD is usually based on enzyme and mutation analyses (25,30–32). In FAOD, biochemical confirmation can also be performed in human skin fibroblasts using standardized in vitro loading with 13C-labelled (33) or unlabeled palmitic acid (34), specifically increasing the flux through deficient metabolic pathways of mitochondrial β-oxidation of fatty acids. Furthermore, in some cases, potentially life-threatening in vivo loading or fasting tests are still performed.
In this study, we present a modified method for the diagnosis of FAOD (SCADD, MCADD, VLCADD, LCHADD), classical OAD (MMA, PA, IVA), and the cerebral OAD GA-I using in vitro loading of peripheral blood mononuclear cells (PBMC) or lymphoblasts with palmitic acid and other substrates. This alternative method allows the reliable detection of mild and classical biochemical phenotypes of these diseases. It is more rapidly available and less cost-intensive than enzyme and mutation analysis as well as in vitro loading in human skin fibroblasts. This method is helpful for the biochemical confirmation of patients with suspected diagnosis of FAOD and OAD, in particular those with mild biochemical phenotypes, and to bridge the time period until conventional confirmatory diagnosis is performed.
MATERIALS AND METHODS
Patients.
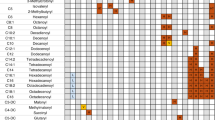
Patients with confirmed diagnosis of FAOD (n = 13) or OAD (n = 22) were included in this study (Tables 1–3), such as patients with SCADD (n = 2), MCADD (n = 5), VLCADD (n = 4), LCHADD (n = 2), MMA (n = 6), PA (n = 3), IVA (n = 4), and GA-I (n = 9). Most patients (20/35) have been diagnosed after clinical presentation, such as metabolic decompensation, psychomotor retardation (PMR), and movement disorders (MD). Three patients were found by screening of high-risk families (i.e., with a previously identified index patient) or high-risk populations (i.e., Canadian Oji-Cree Indians). Twelve patients were identified by MS/MS-based neonatal screening and confirmed by further biochemical tests, mutation analysis, and/or enzyme analysis (in fibroblasts), with most of them (10/12) remaining asymptomatic while being treated. Obviously, the natural history in this subgroup of patients cannot be predicted because correlations of genotypes respectively biochemical phenotypes and clinical phenotypes are poorly understood. Therefore, it cannot be fully excluded that some of them would have remained asymptomatic without treatment. Biochemical monitoring was performed in all included patients using MS/MS-based acylcarniting profiling in dried blood spots (DBS) and/or GC/MS-based organic acid analysis in urine. Results were considered as positive if any of the following items were significantly elevated: (1) MCADD: octanoylcarnitine (C8; DBS), C6-C10 dicarboxylic acids, hexanoylglycine, or suberylglycine (urine); (2) SCADD: butyrylcarnitine (C4, DBS); ethylmalonic acid, methylsuccinic acid, or butyrylglycine (urine); (3) VLCADD: myristoleylcarnitine (C14:1, DBS); C6-C14 dicarboxylic acids (urine); (4) LCHADD: 3-hydroxypalmitoyl (C16OH)-, and -myristoyl- or -stearylcarnitine (DBS); C6-C14 (hydroxy-)dicarboxylic acids (urine); (5) MMA: propionylcarnitine (C3, DBS); methylmalonic acid, or 2-methylcitric acid (urine); (6) PA: propionylcarnitine (C3, DBS); 3-hydroxpropionic acid, propionylglycine, or 2-methylcitric acid (urine); (7) IVA: isovalerylcarnitine (C5, DBS); isovalerylglycine, or 3-hydroxyisovaleric acid (urine); and (8) GA-I: glutarylcarnitine (C5DC, DBS); glutaric acid, or 3-hydroxyglutaric acid (urine). More specific, quantitative methods for the evaluation of urinary excretion of acylglycines, e.g., using GC negative chemical ionization MS (35) or MS/MS (36), have not been used for biochemical confirmation of diagnosis or biochemical monitoring in these patients. Furthermore, heterozygous carriers for disease-causing MCAD mutations (n = 8) and healthy volunteers for the analysis in PBMC (n = 26) respectively lymphoblasts (n = 10) were included. Informed consent was obtained from the parents and healthy volunteers. The study was approved by the Institutional Review Board (#083/2003).
PBMC and lymphoblasts.
PBMC from affected patients (n = 32), healthy volunteers (n = 26), and heterozygous MCAD carriers (n = 8) were isolated from 3 to 4 mL heparinized venous blood samples using Ficoll density gradient centrifugation (37). Blood samples were diluted 1:1 (vol/vol) with RPMI medium. The diluted samples were superposed on a Ficoll phase (twice the volume of the diluted sample, 25°C) in 15 mL tubes (Falcon®; BD Biosciences), carefully avoiding mixture of sample and Ficoll. Centrifugation was performed for 35 minutes at 2000 × g and 20°C. Then, the PBMC interphase was carefully removed and washed twice for each 5 minutes with RPMI medium. The PBMC pellet was resolved in standard growing medium (see later) and maintained at 37°C. For the generation of lymphoblasts, B lymphocytes of at least 5 mL venous EDTA blood samples from GA-I patients (n = 3) and healthy volunteers (n = 10) were immortalized using EBV virus supernatant and cultivated for 6 wk prior application. All preparations and subsequent loading experiments were performed in a blinded fashion.
Loading with palmitic acid or other substrates.
Standard cultivation procedures were as follows. After isolation and preparation, PBMC and lymphoblasts were maintained in RPMI 1640 medium (PAA Laboratories GmbH, Linz, Austria) supplemented with 10% fetal calf serum (PAA Laboratories GmbH, Cölbe, Germany), 25 μg/mL amphotericin B, 1000 IU/mL penicillin and 1 mg/mL streptomycin (all purchased from PAA Laboratories). Twenty-five U/mL IL-2 (IL-2) were added to PBMC. Cell viability was determined by trypan blue exclusion, and 3 × 106 viable cells were used immediately after isolation (PBMC) or after 6 weeks in culture (lymphoblasts) for the loading experiments with unlabeled substrates (palmitic acid, 2-oxoadipic acid, propionic acid, leucine, lysine, and tryptophan (all obtained from Sigma Chemical Co., Aldrich, Deisenhofen, Germany). Cells were washed twice in phosphate-buffered saline and resuspended in 1 mL SMEM (Invitrogen, Karlsruhe, Germany) supplemented with 0.4% bovine serum albumin (wt/vol; Sigma Chemical Co.), 1000 IU/mL penicillin, 1 mg/mL streptomycin and 25 μg/mL amphotericin B, 400 μM L-carnitine (Sigma Chemical Co.), 25 U/mL IL-2 (for PBMC only), 2 mM l-glutamine (Invitrogen) and 100 μM palmitic (all except for GA-I), respectively, 2 mM 2-oxoadipic acid (GA-I). In vitro loading was performed for 5 days, followed by quantitative analysis of acylcarnitines. Aliquots of PBMC or lymphoblasts were used to determine cell viability at the end of the experiments using FACS analysis (Becton-Dickinson, Heidelberg, Germany) and trypan blue exclusion assay.
To establish optimal assay conditions, different parameters were stepwise modified, such as culture media, concentrations of l-glutamine and palmitic acid, and incubation period. In addition, alternative substrates (lysine, tryptophan, leucine, propionic acid) were investigated in sister cultures.
Quantitative acylcarnitine profiling by MS/MS.
Quantitative acylcarnitine profiling in PBMC or lymphoblasts was performed as previously described (34). In brief, aliquots of 20 μL supernatant were collected after 5 days of incubation and were mixed for 20 minutes with 100 μL of isotope-labeled internal standard solution (Cambridge Isotope Laboratories, Kit NSK-A/B, Cambridge, U.K.) in methanol. Samples were filtered and methanol was removed, followed by butylation of the dried samples. Twenty-five μL of the butylated samples were injected by a CTC-PAL autosampler and a Rheos Flux 2000 HPLC pump into the electrospray ion source of a triple quadruple MS/MS (Micromass Quattro Ultima). Each analysis was performed at least in triplicate. Further experiments were performed in sister cultures at different time points (1–6 d of incubation) to determine the optimal time point for quantitative acylcarnitine profiling.
Statistical analysis.
Results were presented as mean ± SD. Cutoffs for acylcarnitines and acylcarnitine ratios were defined as more than mean + 1.96 × SD. All experiments were performed at least in triplicate. Data were analyzed by t test (two groups) or one-way analysis of variance (ANOVA) followed by post hoc Scheffé's test (three or more group). p < 0.05 was considered as significant.
RESULTS
Influence of assay conditions on cell viability and generation of acylcarnitines.
First, different parameters of the assay were varied to establish an optimized standard protocol. During incubation with palmitic acid (100 μM) concentrations of acylcarnitines increased in a time-dependent fashion, reaching a maximum after 4 to 5 days of incubation. Cell viability remained stable for 4 days. Prolongation of the incubation period with 100 μM palmitic acid for 5 days or more did not further increase the concentrations of acylcarnitines, whereas cell viability significantly decreased after 5 days of incubation or more (n = 6; Fig. 1A). Therefore, acylcarnitine profiling was determined at day 5 of incubation.
Influence of assay conditions on cell viability of PBMC and acylcarnitine concentrations. (A) Time-dependent decrease in cell viability of PBMC (n = 6) during incubation with palmitic acid (100 μM). Cell viability was determined by FACS analysis (forward/sideward Scatter). *p < 0.05 vs 1 day of incubation (one-way ANOVA followed by post hoc Scheffé's test). (B) PBMC from controls (n = 8) were loaded with palmitic acid (100 μM) in the presence of l-glutamine (0–2 mM; SMEM medium). Cell viability was determined at day 5 of incubation by FACS analysis. Cell viability in l-glutamine–treated (2 mM) cells was taken as 100%. *p < 0.001 vs glutamine-free media (one-way ANOVA followed by post hoc Scheffé's test). (C) PBMC from controls (n = 5) were incubated with 0–800 μM palmitic acid in SMEM medium, and cell viability was determined at day 5 of incubation by FACS analysis. Cell viability in palmitic acid-free media was normalized to 100%. *p < 0.001 vs palmitic acid-free media (one-way ANOVA followed by post hoc Scheffé's test). (D) Quantitative acylcarnitine profiling of the control group (n = 26) after 5 days of incubation with palmitic acid (100 μM) under standard conditions. All data represent mean ± SD.
Palmitic acid induced a concentration-dependent decrease in cell viability in PBMC from healthy volunteers (n = 5), reaching significance at concentrations of 400 and 800 μM palmitic acid (Fig. 1B). A concentration of 100 μM palmitic acid was chosen for the investigation of FAOD and classical OAD.
Because it is widely accepted that glutamine increases the cell survival of cultivated cells in general (38) and increases viability and many functional parameters of immune cells in particular (39), we incubated PBMC at different glutamine concentrations. In fact, administration of l-glutamine to the culture media increased the cell viability in a concentration-dependent way, reaching a maximum at a concentration of 2 mM l-glutamine (Fig. 1C), which was subsequently chosen for all experiments. Furthermore, we demonstrated that IL-2 known to be a crucial factor for T lymphocytes constituting a major part of PBMC had a positive effect on PBMC viability. Because the absence of IL-2 in the incubation media induced a decrease in cell viability (palmitic acid + IL-2: 80 ± 5%; palmitic acid w/o IL-2: 65 ± 8%; p < 0.05), this cytokine (25 U/mL medium) was supplemented. The acylcarnitine profile of the control group at day 5 of incubation with palmitic acid (100 μM) under standard conditions is shown in Figure 1D.
Next, the effect of different culture media on the production of acylcarnitines was investigated. SMEM, a medium imitating catabolic conditions in vitro (D-glucose content: 1000 mg/L), was shown to induce a considerably higher increase in pathognomonic acylcarnitines compared with other culture media such as the standard medium RPMI 1640 (D-glucose content 2000 mg/L). For example, loading of PBMC from MCADD patients (n = 4) with palmitic acid (100 μM) showed a significant increase in C8 only if SMEM was used, whereas incubation in RPMI medium failed to demonstrate this effect (Fig. 2A). These results highlight that culture conditions failing to simulate metabolic stress in vitro (i.e., by inducing catabolic state and increasing flux through deficient metabolic pathways) are not appropriate for an investigation of FAOD and OAD in PBMC. Similar results regarding the above mentioned assay conditions were found in lymphoblasts (data not shown).
MCADD patients. (A) The effect of different metabolic in vitro conditions (anabolic state applying RPMI medium vs catabolic state using SMEM medium) on C8 levels in MCADD patients (n = 4; squares) and healthy volunteers (n = 10; circles) was investigated at day 5 of incubation with palmitic acid (100 μM). Mean values of triplicates are presented. (B) All patients were clearly identified by elevated C8 (100% sensitivity), whereas none of the controls showed an pathologically elevated concentration of C8 after incubation with palmitic acid (100% specificity). Biochemical differentiation of MCADD patients (n = 6) from heterozygous carriers of disease-causing mutations (n = 8) and controls (n = 26) was reliably performed by plotting of C8 against C8/C2 and C8/C12 (C). In contrast, plotting of C8 against C8/C6 or C8/C10 did not result in a clear differentiation of these three groups (not shown). Grey boxes represent mean ± 1.96 × SD of controls.
Fatty acid oxidation disorders.
Next, PBMC from patients with FAOD (n = 13), i.e., SCADD (n = 2), MCADD (n = 5), VLCADD (n = 4), LCHADD (n = 2), and carriers for disease-causing MCAD mutations (n = 8) were incubated according to the previously established standard protocol for in vitro loading with palmitic acid (SMEM medium, 2 mM l-glutamine, 25 U/mL IL-2, 400 μM carnitine).
MS/MS analysis in PBMC at day 5 of incubation showed increased concentrations of the key acylcarnitines (i.e., above the 95% reference interval of controls; > mean + 1.96 × SD) in all patients (Figs. 2, 3). The disease-specific key acylcarnitines in PBMC were as follows: C4 (Fig. 3A) in SCADD, C8 (Fig. 2A), and decanoylcarnitine (C10) in MCADD, myristoylcarnitine (C14; Fig. 3B) and C14:1 (Fig. 3C) in VLCADD, and C16OH (Fig. 3D) in LCHADD. Notably, this assay clearly elicited the characteristic biochemical features also in PBMC of patients with an intermittently normal biochemical phenotype (8/13 patients): 2/2 patients with SCADD, 1/5 patients with MCADD, 4/4 patients with VLCADD, and 1/2 patients with LCHADD (Table 1), highlighting that some patients with FAOD are at risk to be missed by selective screening using MS/MS in (DBS) or GC/MS in urine under balanced metabolic conditions. In contrast, diagnosis was unambiguously confirmed after selective in vitro loading with palmitic acid in PBMC.
Key acylcarnitines in PBMC from patients (squares) with SCADD (n = 2; A), VLCADD (n = 4; B, C), and LCHADD (n = 2; D) after incubation with palmitic acid (100 μM). All patients were identified by the characteristic acylcarnitine profile (100% sensitivity), revealing an elevation of C4 in SCADD (A), C14 (B), and C14:1 (C) in VLCADD, and C16OH in LCHADD (D). None of the controls (n = 26; circles) revealed an elevation of the mentioned key acylcarnitines (100% specificity). All patients also showed an elevation of characteristic acylcarnitine ratios (Table 4). In contrast, serial investigations of MS/MS in DBS and/or GC/MS in urine of the same patients revealed an intermittently normal biochemical phenotype under balanced metabolic conditions (Table 2). Data represent mean of at least triplicates at day 5 of incubation. Grey boxes represent mean ± 1.96 × SD of controls (n = 26).
In further experiments, we investigated whether palmitic acid loading allowed a differentiation between MCADD patients (n = 5) and heterozygous carriers of a disease-causing MCAD mutation (n = 8) – in analogy to a previous study in human skin fibroblasts (Okun et al. 2002). In fact, homozygous MCADD patients, heterozygous carriers and controls (n = 26) were reliably distinguished by plotting the key metabolite C8 against C8/acetylcarnitine (C2; Fig. 2B) or C8/dodecanolycarnitine (C12; Fig. 2C).
Classical organic acid disorders.
PBMC from patients with classical OAD (MMA [n = 6], PA [n = 3], IVA [n = 4]; Table 2) were loaded with palmitic acid in analogy to patients with FAOD. Increased levels of C3 were found in patients with MMA (Fig. 4A) and PA (Fig. 4B). Patients with IVA showed elevated C5 concentrations (Fig. 4C). In contrast to patients with FAOD included into this study, patients with classical OAD demonstrated the characteristic biochemical features in serial investigation of MS/MS in DBS or GC/MS in urine. Therefore, in vitro loading in this group of patients did not further increase the diagnostic sensitivity of conventional metabolic screening. In further experiments, we also investigated whether other substrates than palmitic acid could be helpful for quantitative acylcarnitine profiling in PBMC. However, neither incubation with leucine (IVA) nor incubation with propionic acid (PA, MMA) resulted in a better differentiation between patients and controls than palmitic acid loading (data not shown).
Key acylcarnitines in classical OAD using in vitro loading of PBMC with palmitic acid (100 μM). All patients (squares) were identified by the characteristic acylcarnitine profile (100% sensitivity), revealing an elevation of C3 in MMA (n = 6; A) and PA (n = 3; B), as well as C5 in IVA (n = 4; C). None of the controls (n = 26; circles) revealed an elevation of the mentioned key acylcarnitines (100% specificity). All patients also showed an elevation of characteristic acylcarnitine ratios (Table 2). Patients persistently showed disease-specific abnormalities in serial investigations of MS/MS in DBS and/or GC/MS in urine (Table 1). Data are represented mean of at least triplicates determined at day 5 of incubation. Grey boxes represent mean ± 1.96 × SD of controls (n = 26).
Glutaric aciduria type I.
PBMC of patients with confirmed GA-I (n = 6; Table 3) were loaded with 2-oxoadipic acid in a concentration of 2 mM. All of them—including two patients with the low excretor phenotype according to the definition of Baric et al. (1999)—demonstrated increased C5DC concentrations in PBMC (Fig. 5A). Furthermore, C5DC/C8 and C5DC/palmitoylcarnitine (C16) were elevated in all patients. Loading with 2-oxoadipic acid (2 mM) was found to be the most appropriate condition to specifically increase C5DC levels in lymphoblasts (n = 3) from affected patients (Fig. 5B). In contrast, no pathologic profile could be detected using palmitic acid in any of these patients (Fig. 5B). In further experiments, incubation with lysine and/or tryptophan was tested as alternative strategy, however, was not as reliable as incubation with 2-oxoadipic acid for the diagnosis of GA-I. Similar results were obtained for PBMC (data not shown).
In vitro loading of PBMC (n = 6; A) or lymphoblasts (n = 3; B) from GA-I patients (squares). In contrast to FAOD and classical OAD, characteristic elevation of C5DC was only found after incubation with 2-oxoadipic acid (2 mM) but not with palmitic acid (100 μM). All patients, including those with the low excretor phenotype (Table 3), were reliably differentiated from controls (n = 26 [PBMC] respectively n = 10 [lymphoblasts]; circles) by this alternative assay (100% sensitivity). In all patients C5DC/C8 and C5DC/C16 ratios were also clearly elevated (Table 2). Data are presented as mean of at least triplicates determined at 5th day of incubation. Grey boxes represent mean ± 1.96 × SD of controls (n = 26).
In conclusion, in vitro loading in PBMC and lymphoblasts reliably detected patients with known FAOD and OAD by pathognomonic acylcarnitines and acylcarnitine ratios (Table 4). Notably, all biochemically mild disease variants, revealing intermittently normal biochemical phenotypes (SCADD, MCADD, VLCADD, LCHADD, GA-I) were clearly unraveled by this assay.
DISCUSSION
In the present study, we described a modified method for the diagnosis of FAOD and OAD using in vitro loading of human PBMC cultures and lymphoblasts with palmitic acid or 2-oxoadipic acid based on a previously published method for quantitative acylcarnitine profiling in human skin fibroblast cultures using unlabeled palmitic acid (34). All patients enrolled in this study were clearly identified, including those with an intermittently normal biochemical phenotype in serial analyses by GC/MS in urine or by MS/MS in DBS (Tables 1–3). Diagnosis was confirmed by increased key acylcarnitine(s) and acylcarnitine ratios (Table 4), reaching a diagnostic sensitivity and specificity of 100% in the patients included. Furthermore, heterozygous carriers of disease-causing MCAD mutations were differentiated from controls and MCADD patients.
A reliable diagnostic procedure independent from the metabolic state of patients is fundamental for the biochemical confirmation of a suspected diagnosis of FAOD and OAD. Under balanced metabolic conditions acylcarnitine profiling in DBS by MS/MS may present false-negative results (Tables 1 and 3). Among the patients included in our study, a number of patients with FAOD but not with OAD showed an intermittently normal biochemical phenotype in serial investigations. Loading tests in vivo may induce metabolic derangements in affected children, potentially resulting in metabolic crises, acute organ failure, and even death. Thus, in vitro loading of PBMC has several advantages compared with conventional procedures: (1) patients are not threatened by in vitro loading tests; (2) the variability can be kept low and the reliability of this assay is high because of standardized biochemical conditions; (3) selective increase in flux through deficient metabolic pathways using in vitro loading also allows a reliable detection of patients with a mild biochemical phenotype; (4) PBMC are easily available, and results can be obtained within less than 1 week, whereas cultivation of fibroblasts requires at least 6 weeks; (5) loading tests with PBMC can be easily repeated if necessary (although this should be restricted, in particular in neonates and infants), and venous puncture is less invasive than a skin biopsy (except for a punch biopsy); and (6) no radiochemicals are used for this assay.
Despite the aforementioned advantages for in vitro loading in PBMC, there remain some obstacles. Experiments cannot be repeated in the same sample. In case of borderline or equivocal results, a second venous puncture may be necessary. Cell viability decreases in a time-dependent fashion after the venous puncture and, thus, the sample should reach the laboratory within 24 to 48 hours. These methodological disadvantages are not shared by lymphoblasts obtained from venous blood samples after transformation with EBV virus, which can be used repeatedly for experiments. Unfortunately, lymphoblasts require 6 weeks of cultivation before they can be used for the experiments. Furthermore, it cannot be completely excluded at present that cell populations in PBMC, i.e., mainly lymphocytes, some monocytes, and few basophiles, may have a different impact on the generation of pathognomonic acylcarnitine profiles. However, we could not demonstrate any relevant influence of the relative amount of these cell populations on acylcarnitine profiles in various experimental series using standard assay conditions (data not shown). In conclusion, in vitro loading in PBMC could be implemented as biochemical confirmatory test before results from enzymatic and/or mutation analysis can be obtained (25,30–32).
At present, in vitro loading in PBMC cannot replace the conventional enzymatic analysis. However, this seems theoretically possible in future if these results will be confirmed in a larger number of patients and correlations between residual enzyme activities and quantitative acylcarnitine profiles will be investigated in detail. Obviously, our loading assay is not appropriate for mass screening, such as MS/MS-based extended neonatal screening, or for emergency metabolic screening (5,9), and it cannot predict the clinical course in patients with FAOD or OAD. Of course, this assay should not interfere with good clinical practice, i.e., immediate start of treatment in suspected cases of theoretically life-threatening, treatable FAOD or OAD (10–16,20,21). In addition to their diagnostic properties, PBMC or lymphocytes are an easily available model system for the simulation of metabolic derangement in vitro, e.g., by comparison of cell viability or various biochemical parameters varying metabolic conditions and treatment protocols (preliminary data not shown).
In conclusion, in vitro loading in PBMC is a reliable and safe tool for the biochemical confirmation of patients with suspected diagnosis of FAOD and OAD, including those with an (intermittently) normal biochemical phenotype using MS/MS in DBS or GC/MS in urine under balanced metabolic conditions.
Abbreviations
- DBS:
-
dried blood spots
- FAOD:
-
fatty acid oxidation disorders
- GA-I:
-
glutaric aciduria type I
- GC/MS:
-
gas chromatography/mass spectrometry
- IL-2:
-
interleukin-2
- IVA:
-
isovaleric aciduria
- LCHAD(D):
-
long-chain 3-hydroxyacyl-CoA dehydrogenase [EC 1.1.1.211] (deficiency)
- MCAD(D):
-
medium-chain acyl-CoA dehydrogenase [EC 1.3.99.3] (deficiency)
- MMA:
-
methylmalonic aciduria
- MS/MS:
-
electrospray ionisation-tandem mass spectrometry
- OAD:
-
organic acid disorders
- PA:
-
propionic aciduria
- PBMC:
-
peripheral blood mononuclear cells
- SCAD(D):
-
short-chain acyl-CoA dehydrogenase [EC 1.3.99.2] (deficiency)
- VLCAD(D):
-
very long-chain acyl-CoA dehydrogenase [EC 1.3.99.13] (deficiency)
References
Hoffmann GF, von Kries R, Klose D, Lindner M, Schulze A, Muntau AC, Röschinger W, Liebl B, Mayatepek E, Roscher AA 2004 Frequencies of inherited organic acidurias and disorders of mitochondrial fatty acid transportation and oxidation in Germany. Eur J Pediatr 163: 76–80
Klose DA, Kölker S, Heinrich B, Prietsch V, Mayatepek E, von Kries R, Hoffmann GF 2002 Incidence and short-term outcome of children with symptomatic presentation of organic acid and fatty acid oxidation disorders in Germany. Pediatrics 110: 1204–1211
Schulze A, Lindner M, Kohlmüller D, Olgemöller K, Mayatepek E, Hoffmann GF 2003 Expanded newborn screening for inborn errors of metabolism by electrospray ionization-tandem mass spectrometry: results, outcome, and implications. Pediatrics 111: 1399–1406
Baric I, Wagner L, Feyh P, Liesert M, Buckel W, Hoffmann GF 1999 Sensitivity and specificity of free and total glutaric acid and 3-hydroxyglutaric acid measurements by stable-isotope dilution assays for the diagnosis of glutaric aciduria type 1. J Inherit Metab Dis 22: 867–881
Chace DH, Kalas TA, Naylor EW 2003 Use of tandem mass spectrometry for multianalyte screening of dried blood specimens from newborns. Clin Chem 49: 1797–1817
Hoffmann G, Aramaki S, Blum-Hoffmann E, Nyhan WL, Sweetman L 1989 Quantitative analysis for organic acids in biological samples: batch isolation followed by gas chromatographic-mass spectrometric analysis. Clin Chem 35: 587–595
Lehnert W 1994 Long-term results of selective screening for inborn errors of metabolism. Eur J Pediatr 153( Suppl 1): S9–S13
Rinaldo P, Raymond K, al-Odaib A, Bennett MJ 1998 Clinical and biochemical features of fatty acid oxidation disorders. Curr Opin Pediatr 10: 615–621
Zytkovicz TH, Fitzgerald EF, Marsden D, Larson CA, Shih VE, Johnson DM, Strauss AW, Comeau AM, Eaton RB, Grady GF 2001 Tandem mass spectrometry analysis for amino, organic, and fatty acid disorders in newborn dried blood spots: a two-year summary from the New England screening program. Clin Chem 47: 1945–1955
den Boer ME, Wanders RJ, Morris AA, Ijlst L, Heymans HA, Wijburg FA 2002 Long-chain 3-hydroxyacyl-CoA dehydrogenase deficiency: Clinical presentation and follow-up of 50 patients. Pediatrics 109: 99–104
Hoffmann GF, Athanassopoulos S, Burlina AB, Duran M, de Klerck JB, Lehnert W, Leonard JV, Monavari AA, Müller E, Muntau AC, Naughten ER, Plecko-Starting B, Superti-Furga A, Zschocke J, Christensen E 1996 Clinical course, early diagnosis, treatment, and prevention of disease in glutaryl-CoA dehydrogenase deficiency. Neuropediatrics 27: 115–123
Leonard JV, Vijayaraghavan S, Walter JH 2003 The impact of screening for propionic and methylmalonic acidaemia. Eur J Pediatr 162( Suppl 1): S21–S24
Nicolaides P, Leonard J, Surtees R 1998 Neurological outcome of methylmalonic acidaemia. Arch Dis Child 78: 508–512
Spiekerkoetter U, Sun B, Zytkovicz T, Wanders R, Strauss AW, Wendel U 2003 MS/MS-based newborn and family screening detects asymptomatic patients with very-long-chain acyl-CoA dehydrogenase deficiency. J Pediatr 143: 335–342
Strauss KA, Puffenberger EG, Robinson DL, Morton DH 2003 Type I glutaric aciduria, part 1: natural history of 77 patients. Am J Med Genet C Semin Med Genet 121: 38–52
Surtees RA, Matthews EE, Leonard JV 1992 Neurologic outcome of propionic academia. Pediatr Neurol 8: 333–337
Wilcken B, Carpenter K, Wiley V 2002 Neonatal screening for medium-chain acyl-CoA dehydrogenase deficiency. Lancet 359: 627–678
Kölker S, Koeller DM, Okun JG, Hoffmann GF 2004 Pathomechanisms of neurodegeneration in glutaryl-CoA dehydrogenase deficiency. Ann Neurol 55: 7–12
Leonard JV 1995 The management and outcome of propionic and methylmalonic acidaemia. J Inherit Metab Dis 18: 430–434
Van der Meer SB, Poggi F, Spada M, Bonnefont JP, Ogier H, Hubert P, Depondt E, Rapoport D, Rabier D, Charpentier C, Parvy P, Bardet J, Kamoun P, Saudubray JM 1994 Clinical outcome of long-term management of patients with vitamin B12-unresponsive methylmalonic acidemia. J Pediatr 125: 903–908
Vianey-Saban C, Divry P, Brivet M, Nada M, Zabot MT, Mathieu M, Roe C 1998 Mitochondrial very-long-chain acyl-coenzyme A dehydrogenase deficiency: clinical characteristics and diagnostic considerations in 30 patients. Clin Chim Acta 269: 43–62
Andresen BS, Dobrowolski SF, O'Reilly L, Muenzer J, Mc Candless SE, Frazier DM, Udvari S, Bross P, Knudsen I, Banas R, Chace DH, Engel P, Naylor EW, Gregersen N 2001 Medium-chain acyl-CoA dehydrogenase (MCAD) mutations identified by MS/MS-based prospective screening of newborns differ from those observed in patients with clinical symptoms: identification and characterization of a new, prevalent mutation that results in mild MCAD deficiency. Am J Hum Genet 68: 1408–1418
Bok LA, Vreken P, Wijburg FA, Wanders RJ, Gregersen N, Corydon MJ, Waterham HR, Duran M 2003 Short-chain acyl-CoA dehydrogenase deficiency: studies in a large family adding to the complexity of the disorder. Pediatrics 112: 1152–1155
Greenberg CR, Prasad AN, Dilling LA, Thompson JR, Haworth JC, Martin B, Wood-Steiman P, Seargeant LE, Seifert B, Booth FA, Prasad C 2002 Outcome of the first 3-years of a DNA-based neonatal screening program for glutaric acidemia type 1 in Manitoba and northwestern Ontario, Canada. Mol Genet Metab 75: 70–78
Gregersen N, Andresen BS, Corydon MJ, Corydon TJ, Olsen RK, Bolund L, Bross P 2001 Mutation analysis in mitochondrial fatty acid oxidation defects: Exemplified by acyl-CoA dehydrognease deficiencies, with special focus on genotype-phenotype relationship. Hum Mutat 18: 169–189
Busquets C, Merinero B, Christensen E, Gelpi JL, Campistol J, Pineda M, Fernandez-Alvarez E, Prats JM, Sans A, Arteaga R, Marti M, Campos J, Martinez-Pardo M, Martinez-Bermejo A, Ruiz-Falco ML, Vaquerizo J, Orozco M, Ugarte M, Coll MJ, Ribes A 2000 Glutaryl-CoA dehydrogenase deficiency in Spain: evidence of two groups of patients, genetically, and biochemically distinct. Pediatr Res 48: 315–322
Zschocke J, Schulze A, Lindner M, Fiesel S, Olgemöller K, Hoffmann GF, Penzien J, Ruiter JP, Wanders RJ, Mayatepek E 2001 Molecular and functional characterisation of mild MCAD deficiency. Hum Genet 108: 404–408
Lindner M, Kölker S, Schulze A, Christensen E, Greenberg CR, Hoffmann GF 2004 Neonatal screening for glutaryl-CoA dehydrogenase deficiency. J Inherit Metab Dis 27: 851–859
Pourfarzam M, Morris A, Appleton M, Craft A, Bartlett K 2001 Neonatal screening for medium-chain acyl-CoA dehydrogenase deficiency. Lancet 358: 1063–1064
Christensen E 1993 A fibroblast glutaryl-CoA dehydrogenase assay using detritiation of 3H-labelled glutaryl-CoA: application in the genotyping of the glutaryl-CoA dehydrogenase locus. Clin Chim Acta 220: 71–80
Wanders RJ, Vreken P, den Boer ME, Wijburg FA, van Gennip AH, Ijlst L 1999 Disorders of mitochondrial fatty acyl-CoA β-oxidation. J Inherit Metab Dis 22: 442–487
Zschocke J, Quak E, Guldberg P, Hoffmann GF 2000 Mutation analysis in glutaric aciduria type I. J Med Genet 37: 177–181
Ventura FV, Costa CG, Struys EA, Ruiter J, Allers P, Ijlst L, Tavares de Almeida I, Duran M, Jakobs C, Wanders RJ 1999 Quantitative acylcarnitine profiling in fibroblasts using [U-13C] palmitic acid: an improved tool for the diagnosis of fatty acid oxidation defects. Clin Chim Acta 281: 1–17
Okun JG, Kölker S, Schulze A, Kohlmüller D, Olgemöller K, Lindner M, Hoffmann GF, Wanders RJ, Mayatepek E 2002 A method for quantitative acylcarnitine profiling in human skin fibroblasts using unlabelled palmitic acid: Diagnosis of fatty acid oxidation disorders and differentiation between biochemical phenotypes of MCAD deficiency. Biochim Biophys Acta 1584: 91–98
Costa CG, Guerand WS, Struys EA, Holwerda U, ten Brink HJ, Tavares de Almeida I, Duran M, Jakobs C 2000 Quantitative analysis of urinary acylglycines for the diagnosis of beta-oxidation defects using GC-NCI-MS. J Pharm Biomed Anal 21: 1215–1224
Bonafe L, Troxler H, Kuster T, Heizmann CW, Chamoles NA, Burlina AB, Blau N 2000 Evaluation of urinary acylglycines by electrospray tandem mass spectrometry in mitochondrial energy metabolism defects and organic acidurias. Mol Genet Metab 69: 302–311
Tripodi D, Lyons S, Davies D 1971 Separation of peripheral leukocytes by Ficoll density gradient centrifugation. Transplantation 11: 487–488
Eagle H, Washington CL, Levy M, Cohen L 1966 The population-dependent requirement by cultured mammalian cells for metabolites, which they can synthesize. II. Glutamic acid and glutamine; aspartic acid and asparagine. J Biol Chem 241: 4994–4999
Kew S, Wells SM, Yaqoob P, Wallace FA, Miles EA, Calder PC 1999 Dietary glutamine enhances murine T-lymphocyte responsiveness. J Nutr 129: 1524–1531
Acknowledgements
The authors are grateful to S. Exner-Camps and M. Herm for excellent technical support.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by a grant from the Medical Faculty of the University of Heidelberg to A. S.-B. (# F.206611) and by a grant from the German Federal Ministry of Education and Science (BMBF # 01GM0305; project # 8) to S. K.
Rights and permissions
About this article
Cite this article
Schulze-Bergkamen, A., Okun, J., Spiekerkötter, U. et al. Quantitative Acylcarnitine Profiling in Peripheral Blood Mononuclear Cells Using In Vitro Loading With Palmitic and 2-Oxoadipic Acids: Biochemical Confirmation of Fatty Acid Oxidation and Organic Acid Disorders. Pediatr Res 58, 873–880 (2005). https://doi.org/10.1203/01.PDR.0000181378.98593.3E
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000181378.98593.3E
This article is cited by
-
Proposed recommendations for diagnosing and managing individuals with glutaric aciduria type I: second revision
Journal of Inherited Metabolic Disease (2017)
-
Intracellular in vitro probe acylcarnitine assay for identifying deficiencies of carnitine transporter and carnitine palmitoyltransferase-1
Analytical and Bioanalytical Chemistry (2013)
-
Guideline for the diagnosis and management of glutaryl‐CoA dehydrogenase deficiency (glutaric aciduria type I)
Journal of Inherited Metabolic Disease (2007)