Abstract
Background
The clinical severity of very-long-chain acyl-CoA dehydrogenase (VLCAD) deficiency is difficult to predict using conventional diagnostic methods.
Methods
Peripheral blood mononuclear cells obtained from 14 VLCAD deficiency patients and 23 healthy adults were loaded with carbon-13-universally labeled (U-13C-) fatty acids. Differences in acylcarnitine ratios between the patients and healthy groups and correlations between acylcarnitine ratios and a newly established clinical severity score (CSS) in the patient group were statistically examined.
Results
There was a significant decrease in the 13C-C2/13C-C18 and 13C-C12/13C-C14 ratios in the U-13C-stearic acid loading test and in the 13C-C2/13C-C18:1 and 13C-C12:1/13C-C14:1 ratios in the U-13C-oleic acid loading test in the patient group. The values of each ratio were significantly correlated with the CSS, suggesting that they could predict disease severity. Additionally, patients with a higher 13C-C16/13C-C18 ratio than the 13C-C14/13C-C18 ratio in the U-13C-stearic acid loading test had a significantly higher CSS and were presumed to have more severe disease.
Conclusions
Our data indicated that this method could be used to predict the clinical severity of VLCAD deficiency, and identify patients at a risk of severe disease.
Impact
-
We established a novel method to predict the severity of VLCAD deficiency by performing a loading test with carbon-13-labeled fatty acids on peripheral blood mononuclear cells.
-
The U-13C-oleic acid loading test was useful for comparing the patient group with the control group in terms of disease severity.
-
The U-13C-stearic acid loading test was useful for identifying the more severely affected patients.
-
These methods are relatively less invasive and enable rapid evaluation of the clinical severity.
Similar content being viewed by others
Introduction
Very-long-chain acyl-CoA dehydrogenase (VLCAD) deficiency is unique in its disease markers and clinical phenotypes. Although VLCAD causes the dehydrogenation of both long-chain saturated and unsaturated fatty acids during beta-oxidation, the disease marker is tetradecenoylcarnitine (C14:1) rather than tetradecanoylcarnitine (C14). C14:1 and C14 are the products of C14:1- and C14-acyl-CoA, respectively. Even in healthy individuals, C14:1 may be elevated in hypercatabolic conditions such as fasting,1 and C14:1 and C14:1/acetylcarnitine (C2) ratios may be higher than the cut-off values in newborns who are not yet fed at the time of initial blood sampling.2 The C14:1 ratio is mildly elevated in patients with mild forms of VLCAD deficiency, and hexadecanoylcarnitine (C16), octadecanoylcarnitine (C18), and octadecenoylcarnitine (C18:1) accumulate more markedly than C14:1 in patients with severe forms of VLCAD deficiency.3,4 Based on the three-dimensional structure of VLCAD, it has been speculated that structural variations in VLCAD caused by genetic mutations might affect the dehydrogenation changes of long-chain acyl-CoAs.5,6,7,8 Although the unique structure of long-chain unsaturated acyl-CoAs may affect their metabolism in VLCAD, this aspect has not yet been proven.
The clinical severity and age of onset vary among patients with VLCAD deficiency.9,10,11,12,13 Some patients develop cardiomyopathy or metabolic crisis in the neonatal or infantile period and have a poor prognosis, while others develop exercise intolerance or rhabdomyolysis in the pediatric age or adulthood or are asymptomatic throughout life. However, it is uncertain whether the C14:1 concentration in initial dried blood spots used for screening in the neonatal period and the residual enzyme activities in fibroblasts or lymphocytes are related to disease severity. Hoffman et al.14 and Bouvier et al.15 found that the values of residual enzyme activity less than 10% were diagnostic, but when the values were greater than 10%, the clinical relevance was unknown and it was difficult to distinguish between patients, carriers, and healthy individuals. Merinero et al.16 reported residual enzyme activity in asymptomatic patients, the values of which varied from single digits to the 30–50% range in each patient. In addition, Zhang et al.17 investigated the relationship between clinical characteristics and genetic mutations in Chinese patients and reported no correlation between the C14:1 levels and clinical characteristics of patients. Pons et al.18 investigated the relationship between the substrate participation rate and enzyme activity in fibroblasts but found no significant correlation between them; they hypothesized that the pathogenesis of VLCAD deficiency is multifactorial, referring to Andresen et al.19
To develop a severity evaluation index useful in clinical practice, we examined the metabolism of various fatty acids, including saturated and unsaturated fatty acids, using peripheral blood mononuclear cells (PBMCs). Although we previously analyzed the fatty acid oxidation ability by loading deuterium-labeled palmitic acid,20 the universally labeled deuterium may affect the metabolism of long-chain fatty acids during dehydrogenation and the conformation of deuterium-labeled long-chain acylcarnitines may change. Thus, in the present study, we analyzed fatty acid oxidation by loading carbon-13-universally labeled (U-13C-) fatty acids, which remain stable during the dehydrogenation process. Acylcarnitine analysis was performed using tandem mass spectrometry. Similar to our previous study, we adopted the ratios among the labeled acylcarnitines rather than the concentrations to accurately identify abnormalities in the metabolic process. These ratios helped to minimize variations in the number of PBMCs that were collected in this study.
Materials and methods
Biological samples
Table 1 shows the patient characteristics. Blood samples were collected from 14 patients with VLCAD deficiency and 23 healthy adult controls between April 1, 2020, and March 31, 2021. At the time of sample collection, the patients ranged in age from 1 to 31 years (median, 4.5 years); eight patients were men and six were women. Two patients (patients #1 and #3) presented with delayed onset of rhabdomyolysis at 12 and 14 years of age, respectively, in the period before the introduction of newborn screening (NBS). Of the 12 patients diagnosed by NBS, three patients had markedly elevated plasma creatine kinase (CK) levels (>1000 U/L), and two patients did not display myopathy symptoms such as myalgia or exercise intolerance. None of the patients had ever presented with hypoglycemia, convulsions, or cardiac abnormalities, such as arrhythmias or cardiomyopathy. The residual enzyme activity was calculated by evaluating the metabolic capacity of VLCAD using palmitoyl-CoA as a substrate, according to Tajima et al.21 All patients had their diagnoses confirmed by genetic testing. In this study, mutations such as p. R450H, p. A333fs, and p. A416T, which were previously reported in cases of myopathy,22,23,24 were detected in patients with myopathy (patients #1, 2, 4, and 5). The p. T409M mutation, which was also presumed to be common in asymptomatic cases,25 was found in asymptomatic patients (patients #12 and #13: siblings). Thus, the clinical severity inferred from the known genetic variants was reflected, to some extent, in the patients included in this study. For the C14:1 level in dried blood spots, the value measured at the first NBS test was used (except for two patients with delayed onset). In terms of treatment status, six patients used medium-chain triglyceride (MCT) milk or oil, one was treated with l-carnitine, and another with l-carnitine and bezafibrate. The remaining eight patients were followed up without treatment. The study was approved by The Research Ethics Committee of the University of Fukui (#20210018), and written informed consent was obtained from the parent or guardians.
Chemicals
The stable isotope-labeled acylcarnitines used in this study as internal standards for acylcarnitine analysis were synthesized in our laboratory.3 U-¹³C-stearic acid was purchased from Sigma-Aldrich Co. LLC. (St. Louis, MO), and U-¹³C-oleic acid was purchased from Cambridge Isotope Laboratories Inc. (Tewksbury, MA). l-Carnitine was purchased from Wako Pure Chemical Industries (Osaka, Japan), and fatty acid-free bovine serum albumin (BSA) was obtained from Sigma-Aldrich Co. LLC. (St. Louis). Phosphate-buffered saline (PBS) and Dulbecco’s PBS (D-PBS) were purchased from Nissui Pharmaceutical Co. Ltd. (Tokyo, Japan) and Nacalai Tesque (Kyoto, Japan), respectively, and Ficoll-Paque solution was purchased from GE Healthcare (Tokyo, Japan).
Sample preparation and acylcarnitine analysis by MS/MS
As previously reported,20 a mixture of 5 mL of heparinized whole blood sample and 5 mL of PBS was laid onto Ficoll-Paque solution and centrifuged. The recovered PBMC layer was washed with PBS and suspended in 0.5 mL of D-PBS. l-Carnitine and U-¹³C-stearic acid or U-¹³C-oleic acid (0.5 mg/mL) in 3% fatty acid-free BSA were added to the cell suspension, and the mixture was incubated at 37 °C for 2 h. The culture medium was centrifuged, and the re-collected PBMCs were washed with PBS. The washed PBMCs were suspended in methanol and homogenized using a glass homogenizer. A mixture of the supernatant fluid collected after centrifugation and a methanol solution of stable isotope-labeled acylcarnitines as internal standards was used for tandem mass spectrometry (MS/MS) measurements.
Flow injection and electrospray ionization MS/MS (ESI-MS/MS) analyses were performed using an API 4000 LC/MS/MS system (AB Sciex, Tokyo, Japan). A model LC-10AVP HPLC system and a model SIL-20AC autoinjector (Shimadzu, Kyoto, Japan) were used for the analyses. Five milliliters of the sample were introduced into the liquid chromatography (LC) stream of acetonitrile/water (4:1) containing 0.05% formic acid. Cationic MS/MS analysis was performed in the precursor ion scan mode by setting the product-ion mass spectra at 85 m/z. Data were recorded for 0.7 min after each sample injection, and the intensities of the specific ions recorded were averaged and quantified using Chemo View Software (AB Sciex).
Diagnostic indices of each disorder
In this study, 13C-labeled palmitoylcarnitine (13C-C18) and 13C-labeled dodecanoylcarnitine (13C-C12) indicate 13C-C18-acylcarnitine and 13C-C12-acylcarnitine, which are formed through carnitine conjugation of labeled palmitoyl-CoA and labeled dodecanoyl-CoA derived from U-13C-palmitoic acid, respectively. Ratios, such as the 13C-C12/13C-C14 and 13C-C12:1/13C-C14:1 ratios, among others, were calculated. These ratios may reflect VLCAD activities and may serve as diagnostic indices for VLCAD deficiency. Furthermore, the amount of 13C-C2 produced through the β-oxidation of 13C-labeled acyl-CoA was measured. The ratios of 13C-C2/13C-C18 and 13C-C2/13C-C18:1, as indicators of β-oxidation ability, were also investigated.
To examine the correlation between the indices mentioned above and the actual clinical severity of the disease, a clinical severity score was prepared for the patients with reference to the score used by Diekman et al.26 and Bleeker et al.27 The following criteria were included in the scoring system: (i) history of markedly elevated plasma CK concentration (≥1000 U/L), (ii) history of plasma CK concentration >500 U/L (reference values 60–270 U/L) during the asymptomatic period, (iii) history of myopathic symptoms (at least two of the following clinically relevant symptoms: myoglobinuria, myalgia, exercise intolerance, muscle weakness (Medical Research Council grade 4 or lower), and easy fatigability). A score of 1 point was assigned to each criterion (0, 1, 2, or 3) for a clinical severity score (CSS). None of our patients presented with hypoglycemia, convulsions, or cardiac abnormalities, such as arrhythmias or cardiomyopathies. The severity of the disease was examined in patients older than 3 years (except for patients #7 and #11) because it was difficult to accurately determine the risk of developing the disease or symptoms in newborns and early infants who were not exposed to physiological stresses such as fever and starvation.
Statistical analysis
The control data were represented as the median and interquartile range (25th–75th percentile). The differences between the ratios of patients and those of controls were analyzed using the Mann–Whitney test, and the accuracy of the two loading tests was compared by generating receiver operating characteristic (ROC) curves. The correlation between the following parameters was analyzed using the Spearman correlation coefficient: each ratio and CSS, CSS, and enzyme activity values, C14:1 level in initial dried blood spots, and each ratio or CSS. Statistical significance was set at p < 0.05. All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface of R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of the R commander designed to add statistical functions frequently used in biostatistics.
Results
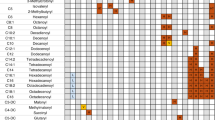
Analytical data of acylcarnitines in the fatty acid loading test for the control and patient groups are shown in Tables S1–S4 in Supplementary Materials and Fig. 1 series of labeled acylcarnitines, ranging from 13C-C18 to 13C-C2 in the U-13C-stearic acid loading test and 13C-C18:1 to 13C-C2 in the U-13C-oleic acid loading test, were detected in PBMCs from healthy controls (Fig. 1a, c). PBMCs from patients with VLCAD deficiency showed a decrease in the production of metabolites from 13C-C12 and 13C-C12:1. We analyzed the metabolic pathway deficiencies in the patient samples using metabolite ratios (Fig. 1b, d).
Peripheral blood mononuclear cells (PBMCs) were purified from healthy controls (a, c) and patients with very-long-chain acyl-CoA dehydrogenase (VLCAD) deficiency (b, d) and then loaded with U-13C-stearic acid (a, b) or U-13C-oleic acid (c, d). The homogenized cells were subjected to acylcarnitine analysis. *Stable isotope-labeled acylcarnitines were used as internal standards.
In the U-13C-stearic acid loading test, the 13C-C12/13C-C14 and 13C-C2/13C-C14 ratios of the patient group were significantly decreased compared with those of the control group.
Similarly, in the U-13C-oleic acid loading test, the 13C-C12:1/13C-C14:1 and 13C-C2/13C-C14:1 ratios of the patient group were significantly decreased compared with those of the control group (Fig. 2a, b, d, e). The 13C-C2/13C-C18 and 13C-C2/13C-C18:1 ratios, which reflected the overall fatty acid oxidation capacity, were reduced in most patients when compared with controls, but they overlapped with control ratios in some patients who were mildly symptomatic or asymptomatic (Fig. 2c, f). The ROC curves were generated to test the discriminatory power of the patient and control groups, and the area under the curve of the U-13C-oleic acid loading test was found to be larger than that of the U-13C-stearic acid loading test, indicating a higher discriminatory power (Fig. 2g).
Ratios of 13C-C12/13C-C14 (a), 13C-C2/13C-C14 (b), and 13C-C2/13C-C18 (c) in the U-13C-stearic acid loading test and ratios of 13C-C12:1/13C-C14:1 (d), 13C-C2/13C-C14:1 (e), and 13C-C2/13C-C18:1 (f) in the U-13C-oleic acid loading test were calculated from the data in Tables S1–S4. The p-values obtained from the Mann–Whitney U test are indicated. The horizontal lines in controls and patients represent the medians and interquartile ranges (25th–75th percentile). In g, receiver operating characteristic (ROC) curves for the 13C-C2/13C-C18 ratio in the U-13C-stearic acid loading test (broken line) and the 13C-C2/13C-C18:1 ratio in the U-13C-oleic acid loading test (solid line).
Based on our scoring system, the disease severity of the patients was significantly correlated with the 13C-C2 /13C-C18 or 13C-C12/13C-C14 ratio in the U-13C-stearic acid loading test and with the 13C-C2/13C-C18:1 or 13C-C12:1/13C-C14:1 ratio in the U-13C-oleic acid loading test (Fig. 3a–d). However, the enzyme activity was not significantly correlated with the clinical severity score in the patients (Fig. 4a). In contrast, although the C14:1 level in dried blood spots was significantly correlated with the clinical severity score, the C14:1 level varied greatly even in patients with a severity score of 0. Thus, it is unclear if the C14:1 level reflected the clinical severity score (Fig. 4b). The 13C-C2/13C-C18 or 13C-C2/13C-C18:1 ratio was significantly correlated with the C14:1 level in initial blood spots (Fig. 4, d).
Additionally, patients were divided into two groups according to whether the 13C-C14/13C-C18 or 13C-C16/13C-C18 ratio was greater in the U-13C-stearic acid loading test. The group with a higher 13C-C14/13C-C18 was designated as Group 1, and the group with a higher 13C-C16/13C-C18 ratio was designated as Group 2 (Fig. 5a). One patient with almost equal values of both the ratios was excluded. The 13C-C2/13C-C18, 13C-C12/13C-C14, and 13C-C2/13C-C14 ratios in the U-13C-stearic acid loading test were lower in Group 2, and CSS was also significantly lower in Group 2 (Fig. 5b, c). In the U-13C-oleic acid loading test, the 13C-C14:1/13C-C18:1 ratio was higher than the 13C-C16:1/13C-C18:1 ratio in all patients.
Line graph showing the ratio of 13C-C10 to 13C-C16 acylcarnitines to 13C-C18 in the U-13C-stearic acid loading test (a) (Group 1, solid line and white circle, Group 2, broken line and gray circle). Comparison of the 13C-C2/13C-C18 ratio between Group 1 and Group 2 in the U-13C-stearic acid loading test (b). Comparison of CSS between Group 1 (white circle) and Group 2 (gray circle) in the U-13C-stearic acid loading test (c). Mann–Whitney U test p-values are indicated. The horizontal lines in controls and patients represent the medians and interquartile ranges (25th–75th percentile).
Discussion
In this study, PBMCs obtained from patients and healthy controls were loaded with U-13C-stearic acid or U-13C-oleic acid, and the results of both tests were used to distinguish the patient group from the control group. The ROC curve showed that the U-13C-oleic acid loading test was more accurate in distinguishing the patient group from the control group. Additionally, the results of the test were correlated with the disease severity, which was assessed from the clinical history of the patients. Conversely, no significant correlation was found between enzyme activity values and the disease severity. This difference might have arisen because the lymphocyte-based enzyme activity assay was based on a single reaction with a single substrate, from palmitoyl-CoA to 2-hexadecanoyl CoA.21 This test could be used to assess the entire process of β-oxidation of long-chain fatty acids, i.e., the overall oxidation capacity could be determined by evaluating multi-step reactions using many substrates. We also examined the correlation between the C14:1 level in dried blood spot and CSS, the 13C-C2/13C-C18 ratio in the U-13C-stearic acid loading test, and the 13C-C2/13C-C18:1 ratio in the U-13C-oleic acid loading test.
Furthermore, the metabolic flow during the U-13C-stearic acid loading test could successfully describe the characteristics of mild VLCAD variants in detail, thus demonstrating the usefulness of this assay. Depending on the degree of mutation in the VLCAD enzyme gene, β-oxidation of long-chain saturated fatty acids could be divided into two groups: one with a metabolic block at C14 and the other with a metabolic block at C16, a longer chain. The latter group is expected to have more prominent VLCAD enzyme dysfunction. We divided the patients according to whether the 13C-C14/13C-C18 or 13C-C16/13C-C18 ratio was higher; the group with a higher 13C-C16/13C-C18 ratio, i.e., the group with an accumulation of 16-carbon acyl-CoA, tended to have a more severe form of the disease. This could reflect the enzymatic function of VLCAD, which is mainly responsible for the dehydrogenation of long-chain acyl-CoAs with 14 to 18 carbons. In the U-13C-oleic acid loading test, the 13C-C14:1/13C-C18:1 ratio was higher than the 13C-C16:1/13C-C18:1 ratio in all patients. However, the values of these ratios were not significantly different among relatively mild cases, indicating that the loading test with U-13C-stearic acid could identify more severe cases in the patient group.
VLCAD deficiency has been identified by screening for the C14:1 acylcarnitine level and the C14:1/C2 ratio in dried blood spots in the neonatal period as indicators However, these indicators are not always reliable, as false positives and false negatives have been reported.2,28,29,30 In the U-13C-oleic acid loading test, the 13C-C14:1/13C-C18:1 ratio was higher than the 13C-C16:1/13C-C18:1 ratio, reflecting the accumulation of 13C-C14:1 in all patients and healthy controls. In contrast, in the U-13C-stearic acid loading test, the 13C-C14/13C-C18 ratio was higher or lower than the 13C-C16/13C-C18 ratio in both patients and healthy controls. These results suggest that C14:1 tends to accumulate during the β-oxidation of long-chain unsaturated fatty acids, which was originally thought to be mediated by VLCAD.
In Japan, the C14:1 serum assay is performed as a confirmatory test for screening positive patients, and then tests for definitive diagnosis are conducted. Genetic tests, enzyme activity measurements, and fatty acid oxidizing ability tests are used for definitive diagnosis,21,31 and the results of these tests are also used to predict the clinical phenotype. However, most patients with NBS are mildly ill or asymptomatic,13,27 and it is inefficient to perform diagnostic tests on all patients with VLCAD deficiency, including such patients. Genetic testing has revealed the correlation of some known mutations with severe to mild clinical phenotypes; however, new mutations have an unclear correlation with clinical phenotypes, and genetic tests take time to show results.20,32,33,34,35 Furthermore, the residual enzyme activity did not always correlate with the actual clinical phenotype, especially in asymptomatic patients and patients with the mild form of the disease, who account for most cases of VLCAD deficiency. In addition, clinical severity scores may be modified by daily life activities and treatment strategies.
The advantage of the U-13C-stearic acid loading test is that it uses the same method and analytical equipment as those of the newborn mass screening test, and it is relatively less invasive to the patient, requiring only blood sampling. Additionally, the test takes ~5–6 h to complete, enabling rapid evaluation. This greatly benefits the patients because early detection and treatment are useful for the efficient management of the disease.20 Carbon-13-labeled fatty acids could be efficiently used to distinguish acylcarnitine-derived loading fatty acids from endogenous acylcarnitines, and the results of the test correctly reflected the metabolic process.
There are several limitations to this study. First, the sample size was small, and almost all patients had the mild disease; therefore, the inclusion of both mild and severe cases is necessary to predict the course of severe disease. Second, the clinical course of the disease was affected by daily habits and treatment status, and muscle symptoms and metabolic crisis often occurred in school-going children and adolescents, who were more active. Therefore, to determine the clinical severity of the disease, the patients should be followed up for a long term in the future.
At this point, this assay is not a substitute for genetic testing or enzyme activity assay as a definitive diagnostic method for VLCAD deficiency. Although many mild cases of NBS have been identified, mild or asymptomatic cases do not need to be treated the same way as those with the actual “disease”, and the results of this assay can be used to avoid excessive treatment or lifestyle restrictions in cases who are judged to be at a low risk for the future metabolic crisis. Further studies should be conducted to establish this method for the rapid diagnosis of patients with VLCAD deficiency and the prediction of disease severity.
In conclusion, fatty acid loading tests on PBMCs with U-13C-stearic acid and U-13C-oleic acid could predict the clinical severity of VLCAD deficiency. The U-13C-oleic acid loading test was useful for comparing the patient group with the control group in terms of disease severity, and the U-13C-stearic acid loading test was useful for identifying the more severely affected patients. The results of this test indicate that early prediction of disease severity in patients with VLCAD deficiency could lead to a more efficient management of these patients.
References
Burrage, L. C. et al. Elevations of C14:1 and C14:2 plasma acylcarnitines in fasted children: a diagnostic dilemma. J. Pediatr. 169, 208–213 (2016).
Bo, R. et al. False positive cases of elevated tetradecenoyl carnitine in newborn mass screening showed significant loss of body weight. Mol. Genet. Metab. Rep. 24, 100634 (2020).
Shigematsu, Y. et al. Selective screening for fatty acid oxidation disorders by tandem mass spectrometry: difficulties in practical discrimination. J. Chromatogr. B 792, 63–72 (2003).
Roe, D. S., Vianey-Saban, C., Sharma, S., Zabot, M. T. & Roe, C. R. Oxidation of unsaturated fatty acids by human fibroblasts with very-long-chain acyl-CoA dehydrogenase deficiency: aspects of substrate specificity and correlation with clinical phenotype. Clin. Chim. Acta 312, 55–67 (2001).
Souri, M., Aoyama, T., Cox, G. F. & Hashimoto, T. Catalytic and FAD-binding residues of mitochondrial very long chain acyl-coenzyme A dehydrogenase. J. Biol. Chem. 273, 4227–4231 (1998).
Souri, M., Aoyama, T., Yamaguchi, S. & Hashimoto, T. Relationship between structure and substrate-chain-length specificity of mitochondrial very-long-chain acyl-coenzyme A dehydrogenase. Eur. J. Biochem. 257, 592–598 (1998).
McAndrew, R. P. et al. Structural basis for substrate fatty acyl chain specificity. J. Biol. Chem. 283, 9435–9443 (2008).
Hisahara, S. et al. A heterozygous missense mutation in adolescent-onset very long-chain acyl-CoA dehydrogenase deficiency with exercise-induced rhabdomyolysis. Tohoku J. Exp. Med. 235, 305–310 (2015).
Spiekerkoetter, U. et al. MS/MS-based newborn and family screening detects asymptomatic patients with very-long-chain acyl-CoA dehydrogenase deficiency. J. Pediatr. 143, 335–342 (2003).
Baruteau, J. et al. Clinical and biological features at diagnosis in mitochondrial fatty acid beta-oxidation defects: a French pediatric study of 187 patients. J. Inherit. Metab. Dis. 36, 795–803 (2013).
Takusa, Y. et al. Identification and characterization of temperature-sensitive mild mutations in three japanese patients with nonsevere forms of very-long-chain acyl-CoA dehydrogenase deficiency. Mol. Genet. Metab. 75, 227–234 (2002).
Diekman, E. et al. The newborn screening paradox: sensitivity vs. overdiagnosis in VLCAD deficiency. Jimd Rep. 27, 101–106 (2016).
Pena, L. D. M. et al. Outcomes and genotype-phenotype correlations in 52 individuals with VLCAD deficiency diagnosed by NBS and enrolled in the IBEM-IS database. Mol. Genet. Metab. 118, 272–281 (2016).
Hoffmann, L., Haussmann, U., Mueller, M. & Spiekerkoetter, U. VLCAD enzyme activity determinations in newborns identified by screening: a valuable tool for risk assessment. J. Inherit. Metab. Dis. 35, 269–277 (2012).
Bouvier, D., Vianey-Saban, C., Ruet, S. & Acquaviva, C. Development of a tandem mass spectrometry method for rapid measurement of medium- and very-long-chain Acyl-CoA dehydrogenase activity in fibroblasts. Jimd Rep. 35, 71–78 (2017).
Merinero, B. et al. Four years’ experience in the diagnosis of very long-chain acyl-CoA dehydrogenase deficiency in infants detected in three Spanish Newborn Screening centers. Jimd Rep. 39, 63–74 (2018).
Zhang, R. N. et al. Clinical features and mutations in seven Chinese patients with very long chain acyl-CoA dehydrogenase deficiency. World J. Pediatr. 10, 119–125 (2014).
Pons, R. et al. Clinical and molecular heterogeneity in very-long-chain acyl-coenzyme A dehydrogenase deficiency. Pediatr. Neurol. 22, 98–105 (2000).
Andresen, B. S. et al. Cloning and characterization of human very-long-chain acyl-CoA dehydrogenase cDNA, chromosomal assignment of the gene and identification in four patients of nine different mutations within the VLCAD gene. Hum. Mol. Genet. 5, 461–472 (1996).
Yuasa, M. et al. Evaluation of metabolic defects in fatty acid oxidation using peripheral blood mononuclear cells loaded with deuterium-labeled fatty acids. Dis. Markers 2019, 2984747 (2019).
Tajima, G. et al. Development of a new enzymatic diagnosis method for very-long-chain acyl-CoA dehydrogenase deficiency by detecting 2-hexadecenoyl-CoA production and its application in tandem mass spectrometry-based selective screening and newborn screening in Japan. Pediatr. Res. 64, 667–672 (2008).
Yamada, K. et al. Open-label clinical trial of bezafibrate treatment in patients with fatty acid oxidation disorders in Japan. Mol. Genet. Metab. Rep. 15, 55–63 (2018).
Fuseya, Y. et al. Adult-onset repeat rhabdomyolysis with a very long-chain acyl-CoA dehydrogenase deficiency due to compound heterozygous ACADVL mutations. Intern. Med. 59, 2729–2732 (2020).
Shiraishi, H. et al. Efficacy of bezafibrate for preventing myopathic attacks in patients with very long-chain acyl-CoA dehydrogenase deficiency. Brain Dev. 43, 214–219 (2021).
Rydel, B. et al. The natural history of elevated tetradecenoyl-L-carnitine detected by newborn screening in New Zealand: implications for very long chain acyl-CoA dehydrogenase deficiency screening and treatment. J. Inherit. Metab. Dis. 39, 409–414 (2016).
Diekman, E. F. et al. Fatty acid oxidation flux predicts the clinical severity of VLCAD deficiency. Genet. Med. 17, 989–994 (2015).
Bleeker, J. C. et al. Impact of newborn screening for very-long-chain acyl-CoA dehydrogenase deficiency on genetic, enzymatic, and clinical outcomes. J. Inherit. Metab. Dis. 42, 414–423 (2019).
Yamada, K. et al. Serum C14:1/C12:1 ratio is a useful marker for differentiating affected patients with very long-chain acyl-CoA dehydrogenase deficiency from heterozygous carriers. Mol. Genet. Metab. Rep. 21, 100535 (2019).
Atkins, A. E., Tarini, B. A., Phillips, E. K. & Calhoun, A. R. U. L. Misclassification of VLCAD carriers due to variable confirmatory testing after a positive NBS result. J. Commun. Genet. 10, 447–451 (2019).
Spiekerkoetter, U. et al. Tandem mass spectrometry screening for very long-chain acyl-CoA dehydrogenase deficiency: the value of second-tier enzyme testing. J. Pediatr. 157, 668–673 (2010).
Hesse, J. et al. The diagnostic challenge in very-long chain acyl-CoA dehydrogenase deficiency (VLCADD). J. Inherit. Metab. Dis. 41, 1169–1178 (2018).
Spiekerkoetter, U. Mitochondrial fatty acid oxidation disorders: clinical presentation of long-chain fatty acid oxidation defects before and after newborn screening. J. Inherit. Metab. Dis. 33, 527–532 (2010).
Andresen, B. S. et al. Clear correlation of genotype with disease phenotype in very-long-chain acyl-CoA dehydrogenase deficiency. Am. J. Hum. Genet. 64, 479–494 (1999).
Mathur, A. et al. Molecular heterogeneity in very-long-chain acyl-CoA dehydrogenase deficiency causing pediatric cardiomyopathy and sudden death. Circulation 99, 1337–1343 (1999).
Gregersen, N. et al. Mutation analysis in mitochondrial fatty acid oxidation defects: exemplified by acyl-CoA dehydrogenase deficiencies, with special focus on genotype-phenotype relationship. Hum. Mutat. 18, 169–189 (2001).
Acknowledgements
We thank Ms. Komeno for her assistance in carrying out acylcarnitine analysis by MS/MS.
Funding
This study was supported in part by a Grant-in-Aid for Young Scientists No. 19K17355 from the Japan Society for the Promotion of Science (K.S.) and by the Health and Labor Sciences Research Grants for Health Research on Children, Youth and Families (G.T.).
Author information
Authors and Affiliations
Contributions
K.S. and Y.S. conceptualized and designed the study. K.S., M.Y., Y.I., and I.H. collected and analyzed the data. K.S. and Y.S. drafted the initial manuscript. Y.O. supervised the study. T.H., T.K., M.A., N.I., Y.K., F.T., R.K., and G.T. reviewed and revised the manuscript critically. All authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
The study was approved by The Research Ethics Committee of the University of Fukui (#20210018), and written informed consent was obtained from the parent or guardians.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sugihara, K., Yuasa, M., Isozaki, Y. et al. Severity estimation of very-long-chain acyl-CoA dehydrogenase deficiency via 13C-fatty acid loading test. Pediatr Res 92, 1391–1399 (2022). https://doi.org/10.1038/s41390-022-01979-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-01979-z