Abstract
Positive end expiratory pressure (PEEP) is important for neonatal ventilation but is not considered in guidelines for resuscitation. Our aim was to investigate the effects of PEEP on cardiorespiratory parameters during resuscitation of very premature lambs delivered by hysterotomy at ∼125 d gestation (term ∼147 d). Before delivery, they were intubated and lung fluid was drained. Immediately after delivery, they were ventilated with a Dräger Babylog plus ventilator in volume guarantee mode with a tidal volume of 5 mL/kg. Lambs were randomized to receive 0, 4, 8, or 12 cm H2O of PEEP. They were ventilated for a 15-min resuscitation period followed by 2 h of stabilization at the same PEEP. Tidal volume, peak inspiratory pressure, PEEP, arterial pressure, oxygen saturation, and blood gases were measured regularly, and respiratory system compliance and alveolar/ arterial oxygen differences were calculated. Lambs that received 12 cm H2O of PEEP died from pneumothoraces; all others survived without pneumothoraces. Oxygenation was significantly improved by 8 and 12 cm H2O of PEEP compared with 0 and 4 cm H2O of PEEP. Lambs with 0 PEEP did not oxygenate adequately. The compliance of the respiratory system was significantly higher at 4 and 8 cm H2O of PEEP than at 0 PEEP. There were no significant differences in partial pressure of carbon dioxide in arterial blood between groups. Arterial pressure was highest with 8 cm H2O of PEEP, and there was no cardiorespiratory compromise at any level of PEEP. Applying PEEP during resuscitation of very premature infants might be advantageous and merits further investigation.
Similar content being viewed by others
Main
At birth, the lungs of premature infants are completely airless, fluid filled, surfactant deficient, and noncompliant. It is common for these infants to require ventilation after birth. The recommended technique of resuscitating infants is with a neonatal resuscitation bag (1,2) connected to a face mask or endotracheal tube. The most common devices used do not provide positive end expiratory pressure (PEEP) and therefore may contribute to atelectasis, acute lung injury (3), and hyaline membrane formation. Although PEEP valves are available for self-inflating resuscitation bags, they are not in common use or recommended. PEEP and continuous positive airway pressure (CPAP) are available during neonatal resuscitation with the Neopuff Infant Resuscitator (Fischer & Paykel, Auckland, New Zealand). Little is known about the clinical or physiologic effects of PEEP during resuscitation of the premature infant (4).
Previous studies have shown that the application of PEEP during the mechanical ventilation of premature infants with respiratory distress improves blood oxygenation (5–7). This is because PEEP increases lung volume (8–11), surface area, and compliance (6,8,12). Increasing the PEEP lowers expiratory resistance (12), conserves surfactant (6), and reduces hyaline membrane formation (12–14), alveolar collapse, and the expression of proinflammatory mediators (15). Without PEEP, the lung volume falls in intubated ventilated infants (16).
In view of its beneficial effects, it is surprising that PEEP and CPAP have not been considered in guidelines for resuscitation of premature infants. Neither the International Liaison Committee on Resuscitation advisory statement nor other guidelines on resuscitation of very premature infants suggest the use of PEEP or CPAP (1,2,17).
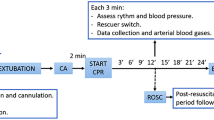
In this study, our objective was to determine the effects of different levels of PEEP on ventilation parameters, blood gases, and arterial pressure during the resuscitation and stabilization of very premature lambs at birth. The study continued beyond the immediate resuscitation period, defined as the first 15 min, to determine whether any effects of PEEP persisted during the next 2 h of ventilation.
METHODS
This study was approved by the Monash University Animal Welfare Committee.
Surgical procedures.
We studied lambs of 19 Merino × Border Leicester ewes at ∼125 d gestation, which corresponds to ∼26 wk of human lung development (18). The ewes were anesthetized (halothane, 2–3% in O2), intubated, and placed supine; a hysterotomy was performed to expose and exteriorize the fetal head and neck. Catheters were inserted into the fetal carotid artery for blood sampling and arterial pressure monitoring and into the jugular vein for the administration, after delivery, of anesthetic (pentobarbitone) and glucose (5% dextrose at 2.5 mL · kg−1 · h−1). The fetus was intubated with a 3.5-mm cuffed endotracheal tube, and excess lung liquid was drained by gravity before the umbilical cord was clamped and cut. The lamb was delivered, weighed, dried, placed in a neonatal warmer unit in the supine/lateral position, and connected to a Babylog 8000 plus ventilator (Dräger Medical, Lubeck, Germany) initially at a fraction of inspired oxygen (Fio2) of 1.0. Rectal temperature was recorded continuously and maintained as near to 39°C as possible. After delivery of lambs, the ewes were killed.
Ventilation protocol.
Before delivery, each lamb was randomly allocated to receive ventilation with 0, 4, 8, or 12 cm H2O of PEEP. It was believed to be important to maintain a constant tidal volume (VT), so the Dräger 8000 plus ventilator was used in volume guarantee mode to deliver an expired VT of 5 mL/kg from the first inflation. This ventilator uses a hot-wire anemometer to measure flow and calculate VT. In volume guarantee mode, the ventilator adjusts the peak inspiratory pressure (PIP), on a breath-by-breath basis, to ensure that the set VT is delivered. The maximum PIP was set at 70 cm H2O to enable the ventilator to vary the PIP up to this level. The ventilator flow was initially set at 10 L/min and then adjusted manually by observing the pressure wave form to ensure that the PIP was maintained for the last 30% of the inspiratory time. The inspiratory time was initially set at 0.3 s and a ventilator rate of 80 inflations/min. Flow waves were observed to ensure that there was no air trapping. The expiratory time and Fio2 were altered to try to maintain arterial pH at 7.30–7.45, partial pressure of carbon dioxide in arterial blood (Pa CO2) at 35–60 mm Hg, and oxygen saturation (Sao2) at 90–98%. The lambs were ventilated for 135 min consisting of a 15-min resuscitation period followed by 2 h of stabilization at the same PEEP. At autopsy, the diaphragm was examined to detect pneumothoraces before the chest wall was opened.
Data collection.
VT, PIP, PEEP, arterial pressure, and heart rate were recorded continuously using a data acquisition system (PowerLab, ADInstruments Pty. Ltd., Castle Hill, NSW, Australia). Respiratory system compliance (CRS) was calculated as the change in volume divided by change in pressure at two points of zero flow in a respiratory cycle. Arterial blood gases (ABL 520; Radiometer, Copenhagen, Denmark) were measured and corrected for body temperature every 5 min for 15 min and then every 10 min for the remainder of the 2-h period. As the Fio2, Paco2, and the partial pressure of oxygen in arterial blood (Pao2) changed with time, the alveolar-arterial oxygen difference (AaDO2) was calculated, where AaDO2 = [(Pbarometric − PH2O) × Fio2 − Paco2/0.8) − Pao2].
Statistical analysis.
Results are presented as mean (± SEM) unless otherwise indicated. At 15 min after the onset of ventilation, each parameter was compared among the four groups by a one-way ANOVA. The data for the entire experimental period were compared using a two-way repeated measures ANOVA with a least-squares differences post hoc analysis to detect changes with time. Fio2 and AaDO2 were transformed to normalize the data using an arcsine square root. Statistical significance was set at P < 0.05.
RESULTS
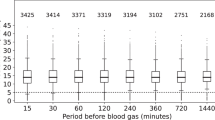
Data about the lamb weights, VT values, pneumothoraces, and survival during the studies are shown in Table 1.
PIP
As the expired VT was set at 5 mL/kg, the PIP differed for each level of PEEP. At 15 min after birth, for the 0-, 4-, 8-, and 12-cm H2O of PEEP groups, respectively, the mean (SEM) PIP was 35.8 (1.0), 31.4 (1.6), 34.3 (1.6), and 45.7 (2.0) cm H2O (Fig. 1a). At 15 min, PIP in the 12-cm H2O of PEEP group was significantly greater (P < 0.001) than the PIP for the 0-, 4-, and 8-cm H2O of PEEP groups. There were no significant differences in PIP among the 0-, 4-, and 8-cm H2O of PEEP groups at 15 min.
During the 135-min study, the mean PIP significantly increased with time (P < 0.05) in the 0 PEEP group. In contrast, the PIP decreased with time in the other three treatment groups.
MEAN AIRWAY PRESSURE
The mean airway pressures at 15 min after birth with 0, 4, 8, and 12 cm H2O of PEEP were 11.9 (0.3), 12.9 (0.5), 16.5 (0.5), and 22.9 (0.7) cm H2O, respectively (Fig. 1b). At this time, the mean airway pressure with 8 cm H2O of PEEP was significantly lower (P < 0.001) than with 12 cm H2O of PEEP and significantly higher than with 0 or 4 cm H2O of PEEP (P < 0.001). There was no significant difference between 0 and 4 cm H2O of PEEP.
With 0 PEEP, the mean airway pressure increased with time. In contrast, with 4-cm H2O of PEEP, the mean airway pressure decreased slightly over the first few minutes and then steadied. With 8 cm H2O of PEEP, the mean airway pressure fell slowly, and with 12 cm H2O of PEEP, it increased rapidly in the first few minutes and then slowly declined to the starting pressure. There was little change in mean airway pressure during the 2 h, although it tended to increase with 0 PEEP.
COMPLIANCE OF THE RESPIRATORY SYSTEM
The CRS at 15 min, with 0, 4, 8, and 12 cm H2O of PEEP, respectively, was 0.14 (0.00), 0.17 (0.01), 0.17 (0.01), and 0.15 (0.01) mL · cm H2O −1 · kg−1 (Fig. 1c). These were not significantly different. With 0 PEEP, CRS decreased significantly up to 85 min and then steadied. With a PEEP of 4, 8, or 12 cm H2O, the CRS significantly improved with time.
INSPIRED OXYGEN
The Fio2 was changed to maintain Sao2 in the target range. At 15 min, the mean Fio2 was 1.0 (0.0), 0.92 (0.0), 0.7 (0.1), and 0.75 (0.1) with 0, 4, 8, and 12 cmH2O of PEEP, respectively (Fig. 2a). Although there was no difference between groups at 15 min or for the whole study, the Fio2 tended to be lower with 8 or 12 cm H2O of PEEP than with 0 or 4 cm H2O of PEEP (P = 0.08). Over the next 2 h, the Fio2 continued to fall to ∼0.5 with 8 cm H2O but remained at ∼0.9 with 4 cm H2O.
OXYGEN SATURATION
At 15 min, Sao2 was 62.5 (7.7), 98.1 (1.6), 97.8 (1.0), and 100% (0.0) with 0, 4, 8, and 12 cm H2O of PEEP, respectively (Fig. 2b). Sao2 in the 0 PEEP group was significantly lower (P ≤ 0.006) than in the other three groups throughout the studies and was suboptimal at ∼65% despite an Fio2 of 1.0. There were no significant differences between the other groups. There was no significant change in Sao2 with time in any group.
AaDO2
At 15 min, AaDO2 was 600 (3), 478 (56), 255 (81), and 198 (27) mmHg with 0, 4, 8, and 12 cm H2O of PEEP, respectively (Fig. 2c). During the first 10–15 min, the AaDO2 improved in all groups except 0 PEEP, in which there was no effect. With 8 and 12 cm H2O of PEEP, the AaDO2 halved. At 15 min, AaDO2 was significantly better with 8 and 12 cm H2O of PEEP than with either 0 or 4 cm H2O of PEEP (P ≤ 0.009), and with 4 cm H2O of PEEP, it was significantly better than with 0 PEEP (P = 0.040). There was no significant difference between AaDO2 at 8 and 12 cm H2O of PEEP. During the rest of the study, AaDO2 remained stable for all groups with differences that were similar to those at 15 min.
ARTERIAL CARBON DIOXIDE
At 15 min, Pa CO2 was 65.4 (2.7), 58.6 (7.2), 63.9 (5.3), and 64.3 (3.2) mmHg with 0, 4, 8, and 12 cmH2O of PEEP, respectively (Fig. 3a). There were no significant differences between the groups. Most values were at or above the upper end of the target range. During the rest of the study, Paco2 increased steadily and significantly to ∼90 mm Hg with 0 PEEP. There was no significant change with time at the other PEEP levels. The increase in Paco2 with 0 PEEP was significantly different from the other groups (P < 0.05), although the overall values in each of the groups were not significantly different.
ARTERIAL PH
The arterial pH at 15 min was 7.14 (0.02), 7.20 (0.03), 7.14 (0.03), and 7.15 (0.03) with 0, 4, 8, and 12 cmH2O of PEEP, respectively, with no significant differences between groups (Fig. 3b). During the study, pH deteriorated in the 0 PEEP group and improved in the 8 cmH2O of PEEP group. It was unchanged with 12 cm H2O of PEEP and decreased very slightly with 4 cm H2O of PEEP.
MEAN ARTERIAL PRESSURE
The mean blood pressure was within the normal range. At 15 min, it was 36.8 (1.5), 37.8 (1.8), 45.5 (2.9), and 41.6 (1.5) mmHg with 0, 4, 8, and 12 cm H2O of PEEP, respectively (Fig. 3c). It was significantly higher with 8 cm H2O of PEEP than either 0 (P = 0.008) or 4 cm H2O of PEEP (P = 0.022). There was no significant difference between 0 and 4 cm H2O of PEEP or between 8 and 12 cm H2O of PEEP.
Mean arterial pressure (MAP) increased slightly but significantly during the 2 h, with 0, 4, and 8 cm H2O of PEEP, but was unchanged with 12 cm H2O of PEEP. With 8 and 12 cm H2O of PEEP, it was significantly elevated compared with 0 0.05). There was no significant and 4 cm H2O of PEEP (P < difference between 0 and 4 cm H2O of PEEP.
DISCUSSION
This study has shown that the use of PEEP during resuscitation and short-term ventilation of very immature lambs produced a marked improvement in oxygenation, halving the AaDO2 within 10 min of delivery, with little increase in Paco2 or adverse effects on arterial pressure. The implication of this finding is that PEEP up to 8 cm H2O should be considered, after further evaluation, for use during resuscitation of premature infants at birth.
The study was done without fetal exposure to antenatal steroids to investigate the response of extremely immature lungs to PEEP during resuscitation because the sickest infants often have not received the benefits of this treatment. Surfactant was not used because it is still common practice to give surfactant to very premature infants only after they are stabilized in the neonatal intensive care unit. The acute improvement in oxygenation with 8 cm H2O of PEEP was similar to the well-known effect of surfactant treatment on Fio2 in premature infants. It is not possible to extrapolate from this study what the effect of PEEP would have been if surfactant had been given before the first breath. Further experiments are needed to investigate the effects after treatment with antenatal steroids and postnatal surfactant.
The effect of PEEP on oxygenation was evident within 5 min of birth and persisted almost unchanged for the remainder of the 135 min. At 0 PEEP, the oxygenation was always suboptimal despite an Fio2 of 1.0. The effect of PEEP on oxygenation improved when the PEEP increased up to 8 cm H2O, but no further benefit was seen at 12 cm H2O of PEEP.
This study has shown that the use of any level of PEEP significantly increases lung compliance by ∼25%, compared with 0 PEEP, with 8 cm H2O having the biggest effect. This improvement is similar to the effect of surfactant treatment on compliance in the first few hours of life of very premature infants (19).
Although PEEP is used during mechanical ventilation of very premature infants, it has not been considered in the guidelines for resuscitation at birth, at a time when the lung gas volume is being established (1). There is increasing evidence that this may be just the time when the immature lung is the most susceptible to injury (20,21). It has been stated that “the greatest volutrauma occurs when lung units are cycled from collapse to overinflation, and it is probable that this is precisely what happens in the delivery room” (3). PEEP conserves surfactant and is important for maintaining lung volume and oxygenation in ventilated neonates (6). It has been shown in lambs that received respiratory support with either endotracheal CPAP alone or ventilation with PEEP that lambs that were supported with CPAP alone had higher lung volumes and less evidence of acute lung injury (22).
In newborn lambs, the larynx modulates lung volume by restricting the expiratory flow of air, thereby producing positive intratracheal pressures during expiration (23). This intrinsic PEEP, or expiratory braking, promotes lung distension (24,25). Intubating infants for resuscitation effectively bypasses the larynx and abolishes this intrinsic PEEP. As a result, ventilation of intubated newborns in the absence of PEEP significantly reduces lung volumes (26,27).
This study involved intubated lambs, whereas most preterm infants are initially resuscitated with a mask connected to a resuscitation bag. It thus is difficult to fully extrapolate our findings to the delivery room. However, the effect of PEEP on oxygenation in the first few minutes of resuscitation was so large that it would be surprising if PEEP during endotracheal ventilation and CPAP during bag and mask ventilation do not have some beneficial effect on oxygenation during resuscitation of very premature infants. The effects of CPAP in infants in the early stages of respiratory distress syndrome (RDS) are well described (5,28,29). It therefore seems appropriate that a positive end expiratory pressure be applied to the airway from birth in premature infants who are at risk of developing RDS.
Premature lambs at 125 d of gestation were used as a model for very premature infants because their lung structure is similar (30). Indeed, they have stiff, fluid-filled lungs with a compliance in a similar range to ventilated very immature infants (19,31). The levels of PIP required to achieve a VT of 5 mL/kg at the different PEEP levels in these lambs were similar to those used during ventilation of very premature infants who are untreated with antenatal steroids and surfactant, although it is to be noted that a PEEP of 12 cm H2O resulted in a very high PIP and mean airway pressure that may have caused the pneumothoraces.
A VT of 5 mL/kg was chosen for several reasons. This is within the range of VT values used for spontaneously breathing premature infants (32). Using a set VT in the Dräger Babylog 8000 plus volume guarantee mode meant that an arbitrary PIP did not have to be chosen for the studies. With increasing concern that high VT ventilation causes lung damage, this was a modest VT (33–35). This study has shown that a VT of 5 mL/kg, in the presence of PEEP, can be used to successfully ventilate very premature lambs from birth without any other maneuver to inflate the lung. The Paco2 levels were a little high at all levels of PEEP, and a slightly greater VT might have produced a lower Paco2. However, the relative merit of hypercarbia and normocarbia in the ventilation of premature infants is still being debated (36).
Some would consider a PEEP of 8 cm H2O so high that it might compromise arterial pressure by compressing the heart and blood vessels in the thorax. The use of 6 cm H2O of PEEP had no effect on arterial pressure in ventilated infants with severe RDS (37). In a study of ventilated premature infants at a PEEP of 8 cm H2O, systemic and pulmonary blood flow were reduced but the heart rate and MAP remained constant (38). The present study has shown, with stiff lungs (compliance 0.15–0.2 mL · kg−1 · cm H2O −1), no adverse effect on MAP during resuscitation. In fact, the highest MAP was with a PEEP of 8 cm H2O. The effect of a pressure applied to the lungs on blood pressure depends on how much pressure is transmitted to the heart and blood vessels in the thorax. This will depend on the compliance of the lungs.
Another concern about high levels of PEEP is that the lungs may become overdistended and interfere with gas exchange. Others have shown, in ventilated premature infants, that with every increase in PEEP, there is an associated increase in Paco2 (3,5,35). In the current study, Paco2 and oxygen levels in the lambs that were treated with PEEP were better than with 0 PEEP. The improved compliance also strongly suggests that the lungs were not overexpanded by the 8 cm H2O of PEEP (39). However, although a PEEP of 12 cm H2O achieved very good oxygenation and the Paco2 was similar to that at lower PEEP levels, all lambs that were treated with this level of PEEP developed pneumothoraces and died. This is a strong indication that 12 cm H2O of PEEP may be too high for human infants.
One problem with using premature lambs for these studies is that they were anesthetized. Therefore, they did not gasp after birth or show evidence of Head's or Hering-Breuer reflexes to aid their lung expansion in the first few minutes (40). These reflexes may be significant factors in establishing a FRC after birth in spontaneously breathing infants (17). It was not possible to study unanesthetized lambs, and as some infants are too ill or immature to breathe at birth, our observations could provide an indication of what might happen in the most difficult clinical situation; that is, an apneic infant born by cesarean section without antenatal steroids or prophylactic surfactant.
Oxygen is toxic, particularly to the tissues of premature infants who have poor antioxidant defenses. Although there is a long-accepted practice of administering 100% oxygen during resuscitation, there is an increasing desire that infants should be resuscitated with the lowest concentration necessary (41). In the current study, the use of 8 cm H2O of PEEP halved the inspired oxygen requirement after 10 min of resuscitation. This may be beneficial by maintaining oxygen saturation and reducing oxygen toxicity.
In conclusion, this study of very premature lambs ventilated from birth has shown that PEEP improves oxygenation, lung compliance, Paco2, pH, and MAP. It seems that a PEEP of 8 cm H2O may be optimal, but this needs further investigation. Applying PEEP during resuscitation of very premature infants might be advantageous and merits further investigation.
Abbreviations
- AaDO2:
-
alveolar-arterial oxygen difference
- CPAP:
-
continuous positive airway pressure
- CRS:
-
compliance of the respiratory system
- Fio2:
-
fraction of inspired oxygen
- FRC:
-
functional residual capacity
- MAP:
-
mean arterial pressure
- Paco2:
-
partial pressure of carbon dioxide in arterial blood
- Pao2:
-
partial pressure of oxygen in arterial blood
- PEEP:
-
positive end expiratory pressure
- PIP:
-
peak inspiratory pressure
- RDS:
-
respiratory distress syndrome
- Sao2:
-
oxygen saturation
- VT:
-
tidal volume
References
Kattwinkel J, Niermeyer S, Nadkarni V, Tibballs J, Phillips B, Zideman D, Van Reempts P, Osmond M 1999 ILCOR advisory statement: resuscitation of the newly born infant. An advisory statement from the pediatric working group of the International Liaison Committee on Resuscitation. Circulation 99: 1927–1938.
Phillips B, Zideman D, Wyllie J, Richmond S, Van Reempts P 2001 European Resuscitation Council Guidelines 2000 for Newly Born Life Support. A statement from the Paediatric Life Support Working Group and approved by the Executive Committee of the European Resuscitation Council. Resuscitation 48: 235–239.
Clark RH 1999 Support of gas exchange in the delivery room and beyond: how do we avoid hurting the baby we seek to save? Clin Perinatol 26: 669–681, vii–viii
Finer NN, Rich W, Craft A, Henderson C 2001 Comparison of methods of bag and mask ventilation for neonatal resuscitation. Resuscitation 49: 299–305.
Gregory GA, Kitterman JA, Phibbs RH, Tooley WH, Hamilton WK 1971 Treatment of the idiopathic respiratory distress syndrome with continuous positive airway pressure. N Engl J Med 284: 1333–1340.
Michna J, Jobe AH, Ikegami M 1999 Positive end-expiratory pressure preserves surfactant function in preterm lambs. Am J Respir Crit Care Med 160: 634–639.
Naik S, Greenough A, Giffin FJ, Baker A 1998 Manoeuvres to elevate mean airway pressure, effects on blood gases and lung function in children with and without pulmonary pathology. Eur J Pediatr 157: 309–312.
Shaffer TH, Koen PA, Moskowitz GD, Ferguson JD, Delivoria-Papadopoulos M 1978 Positive end expiratory pressure: effects on lung mechanics of premature lambs. Biol Neonate 34: 1–10.
Dinger J, Topfer A, Schaller P, Schwarze R 2001 Effect of positive end expiratory pressure on functional residual capacity and compliance in surfactant-treated preterm infants. J Perinat Med 29: 137–143.
Thome U, Topfer A, Schaller P, Pohlandt F 1998 The effect of positive endexpiratory pressure, peak inspiratory pressure, and inspiratory time on functional residual capacity in mechanically ventilated preterm infants. Eur J Pediatr 157: 831–837.
Vilstrup CT, Bjorklund LJ, Larsson A, Lachmann B, Werner O 1992 Functional residual capacity and ventilation homogeneity in mechanically ventilated small neonates. J Appl Physiol 73: 276–283.
Nilsson R, Grossmann G, Robertson B 1980 Artificial ventilation of premature newborn rabbits: effects of positive end expiratory pressure on lung mechanics and lung morphology. Acta Paediatr Scand 69: 597–602.
Argiras EP, Blakeley CR, Dunnill MS, Otremski S, Sykes MK 1987 High PEEP decreases hyaline membrane formation in surfactant deficient lungs. Br J Anaesth 59: 1278–1285.
Sandhar BK, Niblett DJ, Argiras EP, Dunnill MS, Sykes MK 1988 Effects of positive end-expiratory pressure on hyaline membrane formation in a rabbit model of the neonatal respiratory distress syndrome. Intensive Care Med 14: 538–546.
Naik AS, Kallapur SG, Bachurski CJ, Jobe AH, Michna J, Kramer BW, Ikegami M 2001 Effects of ventilation with different positive end-expiratory pressures on cytokine expression in the preterm lamb lung. Am J Respir Crit Care Med 164: 494–498.
Harrison VC, Heese HB, Klein M 1968 The significance of grunting in hyaline membrane disease. Pediatrics 41: 549
Milner AD 1991 Resuscitation of the newborn. Arch Dis Child 66: 66–69.
Harding R, Hooper SB 1996 Regulation of lung expansion and lung growth before birth. J Appl Physiol 81: 209–224.
Baraldi E, Pettenazzo A, Filippone M, Magagnin P, Saia OS, Zacchello F 1993 Rapid improvement of static compliance after surfactant treatment in preterm infants with respiratory distress syndrome. Pediatr Pulmonol 15: 157–162.
Attar MA, Donn SM 2002 Mechanisms of ventilator-induced lung injury in premature infants. Semin Neonatol 7: 353–360.
Bjorklund LJ, Ingimarsson J, Curstedt T, John J, Robertson B, Werner O, Vilstrup CT 1997 Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr Res 42: 348–355.
Jobe AH, Kramer BW, Moss TJ, Newnham JP, Ikegami M 2002 Decreased indicators of lung injury with continuous positive expiratory pressure in preterm lambs. Pediatr Res 52: 387–392.
Harding R, Johnson P, McClelland ME 1980 Respiratory function of the larynx in developing sheep and the influence of sleep state. Respir Physiol 40: 165–179.
Stark AR, Cohlan A, Waggener TB, Frantz ID, Kosch PC 1987 Regulation of end-expiratory lung volume during sleep in premature infants. J Appl Physiol 62: 1117–1123.
Carlo WA, Kosch PC, Bruce EN, Strohl KP, Martin RJ 1987 Control of laryngeal muscle activity in preterm infants. Pediatr Res 22: 87–91.
Miller J, Law AB, Parker RA, Sundell H, Silberberg AR, Cotton RB 1994 Effects of morphine and pancuronium on lung volume and oxygenation in premature infants with hyaline membrane disease. J Pediatr 125: 97–103.
Wiswell TE, Gannon CM, Jacob J, Goldsmith L, Szyld E, Weiss K, Schutzman D, Cleary GM, Filipov P, Kurlat I, Caballero CL, Abassi S, Sprague D, Oltorf C, Padula M 2000 Delivery room management of the apparently vigorous meconium-stained neonate: results of the multicenter, International Collaborative Trial. Pediatrics 105: 1–7.
Ho JJ, Subramaniam P, Henderson-Smart DJ, Davis PG 2002 Continuous distending pressure for respiratory distress syndrome in preterm infants. Cochrane Database Syst Rev 2: CD002271
Morley CJ 1999 Continuous distending pressure. Arch Dis Child Fetal Neonatal Ed 81: F152–F156.
Pringle KC 1986 Human fetal lung development and related animal models. Clin Obstet Gynecol 29: 502–513.
Greenspan JS, Abbasi S, Bhutani VK 1988 Sequential changes in pulmonary mechanics in the very low birth weight (less than or equal to 1000 grams) infant. J Pediatr 113: 732–737.
Itakura Y, Ogawa Y 1998 Effect of body position on tidal volume and minute ventilation in very low birthweight infants. Acta Paediatr Jpn 40: 555–557.
Kacmarek RM 1999 Ventilator-associated lung injury. Int Anesthesiol Clin 37: 47–64.
Dreyfuss D, Basset G, Soler P, Saumon G 1985 Intermittent positive-pressure hyperventilation with high inflation pressures produces pulmonary microvascular injury in rats. Am Rev Respir Dis 132: 880–884.
International Consensus Conferences in Intensive Care Medicine 1999 Ventilator-associated lung injury in ARDS. Am J Respir Crit Care Med 160: 2118–2124.
Varughese M, Patole S, Shama A, Whitehall J 2002 Permissive hypercapnia in neonates: the case of the good, the bad, and the ugly. Pediatr Pulmonol 33: 56–64.
Shortland DB, Field D, Archer LNJ, Gibson NA, Woods KL, Evans DH, Levene MI 1989 Cerebral haemodynamic effects of changes in positive end expiratory pressure in preterm infants. Arch Dis Child 64: 465–469.
Hausdorf G, Hellwege H-H 1987 Influence of positive end-expiratory pressure on cardiac performance in premature infants: a doppler-echocardiographic study. Crit Care Med 15: 661–664.
Aufricht C, Frenzel K, Votava F, Simbruner G 1995 Quasistatic volume-pressure curve to predict the effects of positive end-expiratory pressure on lung mechanics and gas exchange in neonates ventilated for respiratory distress syndrome. Am J Perinatol 12: 67–72.
Greenough A, Morley CJ, Davis JA 1983 Respiratory reflexes in ventilated premature babies. Early Hum Dev 8: 65–75.
Saugstad OD 2001 Resuscitation of newborn infants with room air or oxygen. Semin Neonatol 6: 233–239.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by the National Health and Medical Research Council, Australia, grant number 148003.
Rights and permissions
About this article
Cite this article
Probyn, M., Hooper, S., Dargaville, P. et al. Positive End Expiratory Pressure during Resuscitation of Premature Lambs Rapidly Improves Blood Gases without Adversely Affecting Arterial Pressure. Pediatr Res 56, 198–204 (2004). https://doi.org/10.1203/01.PDR.0000132752.94155.13
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000132752.94155.13
This article is cited by
-
Respiratory strategy at birth initiates distinct lung injury phenotypes in the preterm lamb lung
Respiratory Research (2022)
-
Higher CPAP levels improve functional residual capacity at birth in preterm rabbits
Pediatric Research (2022)
-
Stimulating and maintaining spontaneous breathing during transition of preterm infants
Pediatric Research (2021)
-
Versorgung und Reanimation des Neugeborenen nach der Geburt
Notfall + Rettungsmedizin (2021)
-
Application of two different nasal CPAP levels for the treatment of respiratory distress syndrome in preterm infants—“The OPTTIMMAL-Trial”—Optimizing PEEP To The IMMAture Lungs: study protocol of a randomized controlled trial
Trials (2020)