Abstract
Assessing body composition during infancy requires data for the so-called reference infant. Currently available data for this purpose need to be updated and extended using methods based on principles different from those used previously to define the reference infant. Thus, magnetic resonance imaging was applied to full-term healthy boys (n = 25) and girls (n = 21), 4–131 d old, to estimate adipose tissue volume (ATV) and the amounts of s.c. and non-s.c. adipose tissue (AT). Total body water was estimated using isotope dilution. Total body fat (TBF), fat free weight (FFW) and the degree of hydration in FFW were calculated. Increases in weight, TBF, and FFW with age agreed with current reference data, although when compared with the reference, a slightly more rapid increase in % TBF was observed for boys. The degree of hydration in FFW was 78.9 ± 4.5% (n = 45). Both sexes showed significant increases with age in s.c. ATV (14.7 and 13.0 mL/d for boys and girls, respectively) and in non-s.c. ATV (1.58 and 1.26 mL/d, respectively). Subcutaneous ATV was 90.5 ± 1.8% (boys) and 91.1 ± 1.9% (girls) of total ATV. In conclusion, a pronounced increase with age in the amount of AT was demonstrated involving a considerable gain in s.c. fat during early life. Except for % TBF in boys, changes in body composition with age agreed with current reference data.
Similar content being viewed by others
Main
Much interest has recently been focused on the relationship between early nutrition and the future health of humans (1–3). Poor growth during early life has been associated with disorders such as coronary heart disease, hypertension, and impaired glucose tolerance during adulthood (1), whereas a large weight gain during infancy may act as a risk factor for childhood type 1 diabetes mellitus as well as for obesity later in life (2–4). A relationship between an increased cancer risk and size at birth has also been reported (5). Studies on how the nutritional situation interacts with the growth process during early life in humans are therefore important. In such studies, assessment of body composition, i.e. determination of the amount of fat and FFW in the body, becomes of interest. Unfortunately, no true reference method for studies of body composition during infancy is available. Therefore, to make studies in this area possible, data for the so-called reference infant are needed.
In 1982 Fomon et al.(6) published their classical body composition model that provided age- and gender-specific data for TBF, FFW, TBW, and the degree of hydration in FFW. The latter is of particular importance, as TBF is often calculated as the difference between body weight and FFW, obtained using direct or indirect estimates of TBW and a value for the degree of hydration in FFW. The Fomon model, which provided data from birth to 10 y of age, was, however, presented as preliminary and crude because it was based on quite a limited data set (6). Butte et al.(7) have recently presented data from a longitudinal study where human body composition was studied at 0.5, 3, 6, 9, 12, 18, and 24 mo of age. Their data were in good agreement with Fomon's data for children older than 3 mo, but for younger infants the data reported by Butte et al. were different.
The data presented by Fomon et al.(6) and by Butte et al.(7) are based on measurements of the lean body constituents potassium and water. From these data TBF is calculated using a number of assumptions. Fomon's data for TBF are also based on skinfold measurements assuming a linear relationship between percent TBF and truncal skinfolds (6, 7). However, the validity of these results cannot be evaluated because, as indicated above, no true reference method to assess body composition during infancy is available. Therefore, attempts to provide reference body composition data for infants using alternative methods and assumptions are motivated. We have previously described and evaluated a method based on MRI, by which direct estimates of AT and its distribution in the body can be obtained (8). This method can be applied to infants up to at least 4–5 mo of age. In such infants, estimates of ATV using this method were inversely correlated to percentage TBW (8). Consequently, the MRI method represents a new possibility to study the development of AT and body fatness during early infancy. If combined with estimates of TBW, it has the potential to provide information regarding the degree of hydration in FFW.
This article describes a cross-sectional study where the total amount of AT, as well as its distribution between s.c. and non-s.c. AT, is assessed using our MRI method in 46 full-term infants. TBW of these infants was also measured. The results were used to describe body composition development during the first 4 mo of life.
METHODS
Protocol.
As soon as an infant entered the study, the day of investigation was scheduled. When deciding this we attempted to cover the age interval between birth and 4 mo of age as completely as possible. The mother collected three urine samples from the infant before the day of investigation. On that day, anthropometric measurements were taken, and the infant was given a dose of stable isotopes and studied by means of the MRI method. The mother collected urine samples from the infant during the following 10 d for estimation of the child's TBW. For infants receiving formula during these 10 d, the amount consumed daily was recorded by the mother.
Subjects.
Healthy full-term born infants 4 mo of age or younger and weighing more than 2.5 kg at birth were recruited from mother and child health units in Linköping, Sweden. All infants were studied after receiving informed consent from their parents and approval from the human ethics committee at the University of Linköping. At the time of investigation, all infants except five boys (G, I, K, N, Z) and five girls (m, o, p, r, t) were breast-fed. Infants Z, m, o, p, r, and t were fed formula and infants G, I, K, and N were fed both formula and breast milk. For each of the latter four infants, the amount of formula consumed daily was constant throughout the 10-d urine collection period. Data for 11 of the 46 infants (E, F, G, I, K, M, P, X, g, j, m) have been reported earlier (8).
Assessment of ATV by MRI.
ATV was measured by MRI (8) using a Signa, General Electric, 1.5 tesla. The procedure involved the following steps. After being fed, the infant was swaddled using an elastic bandage and fixed in a straight position with a vacuum sack (vac Fix Sac, Scan Flex Medical AB, Täby, Sweden). The scanning procedure started when the infant was asleep, which always occurred without any use of sedative drugs. Starting from C7 of the cervical spine, 16 transaxial images (T1-weighted, spin echo, repetition time 700 ms, echo time 12 ms, two acquisitions, matrix 512 × 256, 8-mm thick) were taken during a period of 6 min. The head was not included in the scan. The images were evenly distributed over the body, i.e. for a particular infant the distance between adjacent images was always the same. In the images, AT was white in contrast to other tissues that were gray or black. The AT area in the images was assessed using a computer program in which the exact criteria were defined by the observer, and which allowed separation of s.c. from non-s.c. AT by manually tracing the appropriate AT area. The sum of AT areas in all images in one scan was multiplied by the distance between the images to obtain ATV. The data reported in this article represent the average of two AT area evaluations that were carried out on two different occasions by the same observer. On each occasion scans from all infants (including E, F, G, I, K, M, P, X, g, j, m) were arranged in a randomized order, which was changed for the second occasion. Precision based on the two evaluations was 1.7, 1.6, and 8.7% for total, s.c., and non-s.c. ATV, respectively.
Calculation of TBF.
Procedures to calculate TBF from ATV using figures for AT composition have been published for adults (9, 10) as well as for infants (11). In the latter study, AT from 17 boys and 5 girls between 1 and 5 mo were found to contain 0.67 ± 0.07 g fat/mL. Reported values for the fat content in AT from newborn full-term infants are slightly lower (12, 13). We have selected the figure 0.456 g/mL (12) to represent the fat content of AT at birth and assumed a linear increase in the fat content of AT during the first 30 d of life until a level of 0.67 g/mL was reached. Thus, for infants below 30 d of age, TBF (g) was calculated as: [0.456 + (0.67–0.456)/30 × age in days] (g/mL) × total ATV (mL). For infants older than 30 d, TBF (g) was 0.67 (g/mL) × total ATV (mL).
Assessment of TBW.
Urine samples were taken using a baby urine collector (Coloplast A/S, Copenhagen, Denmark). An accurately weighed dose containing 0.08 g of 2H2O and 0.24 g of H218O/kg body weight was given to the infant through a nasogastric tube and flushed through with 2–5 mL of water. To estimate TBW, urine samples were collected 4–6 h after dosing (39 infants) as well as on d 1, 3, 8, and 10 after dosing (44 infants). For infant s, the only postdose sample obtained was collected 4 h after dosing. The time (date and time of day) of sampling was always noted. Urine samples were transferred to glass vials with internal aluminum-lined screw-cap sealing and kept at 4°C until sample collection was finished. They were then placed at −20°C and kept there until analyzed. For infants E, F, G, I, K, M, P, X, g, and m, isotope enrichment in dose and urine samples was analyzed at the Department of Clinical Physiology, University of Uppsala, using a mass spectrometer (SIRA Series II, VG Isogas Ltd., Middlewich, UK) as described previously (8). Dose and urine samples from the remaining infants were analyzed in our own laboratory using a mass spectrometer (Deltaplus XL, Thermo Finnigan AB, Dreieich, Germany) fitted with a CO2/H2/H2O equilibrium device. The analytic procedure described by Thielecke and Noah (14) was followed, except that equilibration time was 180 and 840 min for H2 and CO2, respectively. Deuterium and oxygen dilution spaces (ND and NO, respectively) were calculated from the zero-time enrichments obtained from the exponential isotope disappearance curves that provided estimates for the rate constants for 2H and 18O, respectively. For boys, ND/NO was 1.03 ± 0.02 (n = 25) and for girls 1.03 ± 0.01 (n = 20). In both laboratories, the masspectrometric response was standardized using Vienna standard mean ocean water as well as standards 304 A and B (for 18O) and 302 A and B (for 2H) obtained from the International Atomic Energy Agency, Vienna. A linear response was confirmed for both isotopes for each set of samples analyzed. Analytical precision in the measurement range, for results expressed as mol fraction, was 0.58 ppm (Uppsala), 0.44 ppm (Linköping) for 2H and 0.49 ppm (Uppsala), 0.15 ppm (Linköping) for 18O. For infant s, ND and NO were calculated using the plateau method after correction for the amount of isotope lost during 4 h, assuming kO = 0.275 and kD = 0.229 24 h−1. These figures represented the average of the appropriate values as obtained from infants p, q, r, t, and u. TBW was calculated as the average of ND divided by 1.04 and NO divided by 1.01 (15).
FFW and the degree of hydration in FFW.
FFW (g) was body weight (g) minus TBF (g) and the degree of hydration in FFW was calculated as [TBW (g)/FFW (g)] × 100.
Anthropometry.
The infants were weighed naked on an electronic baby scale (Tanita Corp., Tokyo, Japan) to the nearest 5 g. Crown–heel length was measured to the nearest centimeter on a length board.
Statistics.
Values are expressed as means ± SD. The data were analyzed using PC statistical software Minitab (release 12, Minitab Inc., State College, PA, U.S.A.). Correlation and regression analysis was performed as described by Kirkwood (16). Precision (%) was calculated using the following formula:

where a and b are duplicate estimates of the variable under investigation, and n is the number of duplicates.
RESULTS
Subjects.
At birth, boys were 51 ± 2 cm tall and weighed 3645 ± 430 g (n = 25). The corresponding figures for girls were 50 ± 3 cm and 3515 ± 520 g (n = 21). The gestational age at birth for the infants was 40.0 ± 1.3 wk. Table 1 shows weight-for-age, length-for-age, and weight-for-length z scores at the time of investigation for the boys and girls in the study as obtained using two different U.S. growth references (17, 18). Obviously, when compared with these references our infants tended to be heavy and tall but slightly light for their length.
Degree of hydration in FFW.
Tables 2 and 3 show TBW and age of all infants in the study. Using data from 45 of these infants, the degree of hydration in FFW was calculated to be 78.9 ± 4.5%, CV = 5.7% [79.2 ± 3.6% for boys (n = 25), 78.5 ± 5.6% for girls (n = 20)]. The regression equation relating this variable (y) to age in days (x) was: y = −0.0137 × +79.7 and its correlation coefficient (0.11) was nonsignificant.
Body weight, TBF, FFW, and ATV in relation to age.
Tables 2 and 3 show body weight, TBF, and age of boys and girls in the study. Figure 1A shows FFW and TBF for the boys in the study together with the corresponding data for the reference boy as reported by Fomon et al.(6). The corresponding data for the girls in the study are shown in Figure 1B. The linear relationships between weight in grams (y) and age in days (x) (y = 30.7x + 3628 for boys and y = 24.9x + 3477 for girls) were significant for boys [r = 0.86 (p < 0.001)] and for girls [r = 0.90 (p < 0.001)]. Furthermore, significant linear relationships between FFW in grams (y) and age in days (x) were found for boys (y = 18.6x + 3143, r = 0.86, p < 0.001) and for girls (y = 13.8x + 3052, r = 0.81, p < 0.001). The linear relationships between TBF in grams (y) and age in days (x)—y = 12.1x + 485, r = 0.83, p < 0.001 (boys) and y = 11.1x + 424, r = 0.93, p < 0.001 (girls)—were also significant. According to these relationships, daily increases in body weight, FFW, and TBF for boys were 30.7, 18.6, and 12.1 g, respectively, during the first 4 mo of life. The corresponding figures for girls were 24.9, 13.8, and 11.1 g. Fomon's reference boy and girl gained 29.3 and 24.5 g of body weight, 18.4 and 15.2 g of FFW, and 10.8 and 9.3 g of TBF, respectively, during the corresponding period of infancy.
TBF and FFW vs age of infants in the study. Dotted and solid lines represent the growth of the reference infant (6) in FFW and FFW + TBF, respectively. (A) boys, n = 25; (B) girls, n = 21.
Tables 2 and 3 show TBF in percentage of body weight and age of boys and girls in the study. Figure 2A shows TBF in percentage of body weight in relation to age for boys compared with the corresponding figures for Fomon's reference infant (6). The corresponding data for the girls in the study are shown in Figure 2B. When compared with Fomon's reference boy, the body fat content for the boys in our study tended to increase slightly more rapidly. The corresponding increase for our girls, however, agreed well with that of the reference girl.
TBF in percentage of body weight vs age of infants in the study. Solid lines represent the fat content of the reference infant (6). (A) boys, n = 25; (B) girls, n = 21.
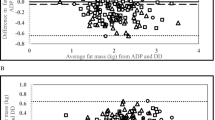
Tables 2 and 3 show total ATV, s.c. ATV in percent of total ATV, and age of boys and girls in the study. Figure 3, A and B, shows the amounts of s.c and non-s.c. ATV in relation to age for boys and girls in the study. Obviously, s.c. ATV increases rapidly with age in both sexes. The linear relationship between s.c ATV in milliliters (y) and age in days (x) for boys was y = 14.7x + 790, r = 0.79, p < 0.001, and for girls it was y = 13.0x + 761, r = 0.87, p < 0.001. The corresponding relationship for non-s.c. ATV was y = 1.58x + 78.6, r = 0.81, p < 0.001 (boys) and y = 1.26x + 72.4, r = 0.76, p < 0.001 (girls). For both sexes, ATV in relation to body weight (mL/kg, y) increased with age (days, x); boys: y = 253 + 1.22x, r = 0.70 (p < 0.001); girls: y = 253 + 1.28x, r = 0.72 (p < 0.001). This increase did not differ significantly between boys and girls. The proportion of total ATV present as s.c. ATV was 90.5 ± 1.8% (boys) and 91.1 ± 1.9% (girls). No significant relationship between percentage of total ATV located s.c. and age was found for boys or girls or for the sexes combined.
DISCUSSION
The average birth weight of our infants was slightly higher than the corresponding figure for the reference infant whereas the observed relationships between weight and age corresponded well to the weight gains of the reference boy and girl (6). The frequency of breast-feeding among our infants was high and similar to that of contemporary Swedish infants (19). At the time of investigation, our infants tended to be heavy and tall but slightly light for their length when compared with reference data for U.S. infants (17, 18). Nevertheless, it is reasonable to consider our data as complements to existing reference data for infants below 4 mo of age.
We have previously shown that our MRI procedure can estimate ATV with good precision and with a relative validity, i.e. it is possible to arrange the infants in a study in a specific order with respect to the amount of ATV they contain as long as all images in the study are evaluated using criteria defined by one observer (8). This requires that the scans from all infants are evaluated at least twice, and that each time they are presented to the observer in a randomized order, as was done in the present study where results for infants E, F, G, I, K, M, P, X, g, j, and m were arranged in the same order as that reported previously (8). However, although our estimates of ATV have good precision and a relative validity, the possibility that they may be slightly biased cannot be excluded, as there is no true reference method available to evaluate measurements of this kind.
The procedure used in this study to calculate TBF from ATV is likely to be more correct than using 0.66 g fat/mL throughout infancy, as previously suggested (11). It should be pointed out, however, that the present calculation is based on assumptions that there is a linear increase in the fat content of AT with age during the first month of life and that the fat content of AT remains at the level 0.67 g fat/mL during the following 3 mo. These assumptions are based on results obtained by means of chemical analysis of AT of infants at various ages and it should be noted that comparatively few such results are available in the literature. Our procedure to calculate TBF from ATV may therefore need modification when more data on infant AT composition becomes available.
Our data demonstrate that the main part of the fat retained in the infant body during the first 4 mo of life is located subcutaneously, and that this period of life is associated with considerable growth in s.c. AT. This new finding is of interest, because at birth and in the newborn period the human is one of the fattest species on record (20). This can be reconciled with the finding by Sohlström et al.(10) that excess body fat tends to be stored subcutaneously in adult women. It has been suggested that AT in human infants serves as insulation to compensate for hairlessness, but support for this hypothesis is weak (20). It is more widely accepted that the role of body fat is to serve as an energy store (20, 21), presumably in preparation for future needs, such as during weaning. In addition, knowledge regarding the location of body fat is important when anthropometric methods based on caliper measurements are being developed. It has been suggested (11, 22) that one reason for the lack of accuracy of such methods is that the caliper is unable to measure non-s.c. AT.
When compared with the infants studied by Butte et al.(7) as well as with Fomon's reference infant (6), our infants were slightly heavier at birth. However, as shown in this study, in relation to age, their weight was comparable to Fomon's reference data. When compared with this reference, the infants studied by Butte et al.(7) tended to grow more rapidly. Despite these differences it is relevant to compare body composition data for our infants to the corresponding data provided by Butte et al.(7) and by Fomon et al.(6). Thus, with the exception of a slightly more rapid increase in percentage TBF for boys, the changes in body composition as estimated by the MRI method are similar to the corresponding changes described by Fomon et al.(6) for the reference infant throughout the first 4 mo of life. However, according to Butte et al.(7), the increase in TBF between 0.5 and 3 mo of age is much more pronounced, and a peak is reached at 3–4 mo when TBF is as high as 30%. At this age the infants in our study as well as those studied by Fomon et al.(6) contained only about 25% TBF. With respect to the degree of hydration in FFW, our results are slightly lower than those reported by Fomon et al.(6) or Butte et al.(7). This may be related to the fact that our estimates of ATV do not include the head. Furthermore, it should be pointed out that we have no specific reason to suspect that the accuracy of our estimate of the degree of hydration in FFW is influenced by the age of the infant. With respect to the precision of this estimate, the following comments are relevant. In their study on infants, Butte et al.(7) found the CV of estimates of the degree of hydration in FFW to be only 1–2%, and in a study on children 8–12 y of age, Wells et al.(23) found that the biologic variation in the degree of hydration of FFW is quite small. Therefore, it is likely that the biologic variation in the degree of hydration in FFW is also small during infancy. If this is the case, the obvious explanation for the comparatively large variation in our estimate of the degree of hydration in FFW is that the fat concentration in AT varies between individual infants not only in analyzed AT biopsies (11) but also at the whole body level. This explanation is interesting because it gives rise to several questions regarding the significance of this variation for the possibilities to identify and prevent obesity early in life. However, the procedures used to assess the degree of hydration in FFW are different in the studies by Wells et al.(23) and by Butte et al.(7). Therefore, it is not presently possible to definitely conclude that the biologic variation in the degree of hydration in FFW is small also during infancy.
Some relevant points with respect to estimates of the degree of hydration in FFW as obtained in our study as well as in the studies by Butte et al.(7) and by Fomon et al.(6) are summarized in Table 4. At 14 d of age the degree of hydration in FFW, as reported by Butte et al.(7), tends to be higher than the corresponding figures found in the present study or by Fomon et al.(6). Table 4 also demonstrates that at 14 d of age, percentage TBW of the infants studied by Butte et al.(7) was higher than comparable figures obtained in the present study or by Fomon et al.(6). In a study on alternative approaches for calculating TBW, Davies and Wells (15) compared the so-called plateaux method to the so-called back extrapolation method using procedures apparently similar to those used by Butte et al.(7). Davies and Wells (15) observed that the former method produced higher values than the latter, which is of is of relevance inasmuch as Butte et al.(7) used the plateaux method in their 14-d-old infants and the back extrapolation method for older infants. The latter method, also used in the present study, has been shown to produce values for TBW in close agreement with data for Fomon's reference infant (15). These methodological comments are relevant, because an overestimation of TBW will result in an overestimation of the degree of hydration in FFW.
CONCLUSION
In conclusion, we have demonstrated a pronounced increase in ATV during the first 4 mo of extrauterine life in boys as well as in girls that involves a considerable gain in s.c. fat. We have also provided data on the degree of hydration in FFW as well as on body weight and body composition during this period of life. Our data have been obtained using MRI, a method that is independent of the methodology previously used to obtain body composition data for the reference infant. Nevertheless, with the exception of a slightly more rapid increase in percentage TBF for boys, our data confirm corresponding data previously published by Fomon et al.(6).
Abbreviations
- FFW:
-
fat free weight
- TBF:
-
total body fat
- TBW:
-
total body water
- MRI:
-
magnetic resonance imaging
- AT:
-
adipose tissue
- ATV:
-
adipose tissue volume
REFERENCES
Barker DJ 1998 Early growth and cardiovascular disease. Arch Dis Child 80: 305–307
Hypponen E, Kenward MG, Virtanen SM, Piitulainen A, Virta-Autio P, Tuomilehto J, Knip M, Åkerblom HK 1999 Infant feeding, early weight gain, and risk of type 1 diabetes. Diabetes Care 22: 1961–1965
Martorell R, Stein AD, Schroeder DG 2001 Early nutrition and later adiposity. J Nutr 131: 874S–880S
Stettler N, Zemel BS, Kumanyika S, Stallings VA 2002 Infant weight gain and childhood overweight status in a multicenter, cohort study. Pediatrics 109: 194–199
Andersson SW, Bengtsson C, Hallberg L, Lapidus L, Niklasson A, Wallgren A, Hulthén L 2001 Cancer risk in Swedish women: the relation to size at birth. Br J Cancer 84: 1193–1198
Fomon SJ, Haschke F, Ziegler E, Nelson S 1982 Body composition of reference children from birth to age 10 years. Am J Clin Nutr 35: 1169–1175
Butte NF, Hopkinson JM, Wong WW, Smith EO, Ellis KJ 2000 Body composition during the first 2 years of life: an updated reference. Pediatr Res 47: 578–585
Olhager E, Thuomas KA, Wigstrom L, Forsum E 1998 Description and evaluation of a method based on magnetic resonance imaging to estimate adipose tissue volume and total body fat in infants. Pediatr Res 44: 572–577
Sjöström L, Kvist H, Cederblad Å, Tylén U 1986 Determination of total adipose tissue and body fat in women by computed tomography, 40K and tritium. Am J Physiol 250( 6 Pt 1): E736–E745
Sohlström A, Wahlund L-O, Forsum E 1993 Adipose tissue distribution as assessed by magnetic resonance imaging and total body fat by magnetic resonance imaging, underwater weighing and body water dilution in healthy women. Am J Clin Nutr 58: 830–838
Kabir N, Forsum E 1993 Estimation of total body fat and subcutaneous adipose tissue in full-term infants less than 3 months old. Pediatr Res 34: 448–454
Baker GL 1969 Human adipose tissue composition and age. Am J Clin Nutr 22: 829–835
McGowan AR 1979 The fat and water content of the dead infants skinfold. Pediatr Res 13: 1304–1306
Thielecke F, Noack R 1997 Evaluation of an automated equilibration technique for deuterium/hydrogen isotope ratio measurements with respect to assessing total energy expenditure by the doubly labelled water method. J Mass Spectrom 32: 323–327
Davies PS, Wells JC 1994 Calculation of total body water in infancy. Eur J Clin Nutr 48: 490–495
Kirkwood BR 1995 Essentials of Medical Statistics. Blackwell Science, London
WHO 1983 Measuring Change in Nutritional Status. Guidelines for Assessing the Nutritional Impact of Supplementary Feeding Programmes for Vulnerable Groups. World Health Organization, Geneva, pp 63–97.
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL 2000 CDC Growth Charts: United States Advance Data from Vital and Health Statistics, no. 314. National Center for Health Statistics, Hyattsville, MD
Ivarsson A, Persson LA, Nystrom L, Ascher H, Cavell B, Danielsson L, Dannaeus A, Lindberg T, Lindquist B, Stenhammar L, Hernell O 2000 Epidemic of coeliac disease in Swedish children. Acta Paediatr 89: 165–171
Kuzawa CW 1998 Adipose tissue in human infancy and childhood: an evolutionary perspective. Am J Phys Anthropol Suppl 27: 177–209
Norgan NG 1997 The beneficial effects of body fat and adipose tissue in humans. Int J Obes Relat Metab Disord 21: 738–746
Wells JC 2001 A critique of the expression of paediatric body composition data. Arch Dis Child 85: 67–72
Wells JC, Fuller NJ, Dewit O, Fewtrell MS, Elia M, Cole TJ 1999 Four-component model of body composition in children: density and hydration of fat-free mass and comparison with simpler models. Am J Clin Nutr 69: 904–912
Acknowledgements
The authors thank the parents and infants who participated in the study; Karin Boström, Margareta Jönsson, and Christine Rosén for help with subject recruitment; Eva Sjödahl for laboratory assistance; and Olle Eriksson for statistical advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants from the Östergötland County Council, Wera Ekström's Fund for Pediatric Research, Crown Princess Lovisa's Fund for Pediatric Research, the Swedish Nutrition Foundation, and the Swedish Research Council (Project No. 12172).
Rights and permissions
About this article
Cite this article
Olhager, E., Flinke, E., Hannerstad, U. et al. Studies on Human Body Composition during the First 4 Months of Life Using Magnetic Resonance Imaging and Isotope Dilution. Pediatr Res 54, 906–912 (2003). https://doi.org/10.1203/01.PDR.0000088064.63106.5E
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000088064.63106.5E
This article is cited by
-
Growth and body composition trajectories in infants meeting the WHO growth standards study requirements
Pediatric Research (2022)
-
The mysterious values of adipose tissue density and fat content in infants: MRI-measured body composition studies
Pediatric Research (2021)
-
Free-breathing 3-D quantification of infant body composition and hepatic fat using a stack-of-radial magnetic resonance imaging technique
Pediatric Radiology (2019)
-
High-resolution rapid neonatal whole-body composition using 3.0 Tesla chemical shift magnetic resonance imaging
Pediatric Research (2018)
-
Body composition of term healthy Indian newborns
European Journal of Clinical Nutrition (2016)