Abstract
The optimum body temperature for infants <1000 g is unknown. We investigated body temperature effects on spontaneous breathing using proportional assist ventilation (PAV), because this mode supports spontaneous breathing such that all breathing pattern variables remain controlled by the infant. Minute volume (MV), respiratory rate (RR), tidal volume (Vt), incidence and duration of respiratory pauses, arterial oxygen desaturations <85%, and arterial Pco2 levels will remain unaffected by targeting core body temperature to 36.1–36.5°C (low normal range) versus 37.7–37.9°C (upper normal). Twenty infants (mean ± SD: birth weight, 696 ± 155 g; gestational age, 25 ± 1 wk; age, 5 ± 3 d) who were supported by PAV were exposed to each target temperature range on 2 consecutive days in four 2-h intervals for a total of 8 h with the sequence of the temperature ranges randomized. Core body temperature was 36.5 ± 0.2°C and 37.9 ± 0.2°C in the two conditions. MV was 291 and 314 mL · min−1 · kg−1, respectively (7% difference; p < 0.001) as a result of a difference in RR (8%; p < 0.001). The infants maintained their blood CO2 levels and Vt (5.25 ± 0.6 versus 5.19 ± 0.6 mL/kg). Incidence and duration of respiratory pauses were not different between conditions. Extremely immature infants who are supported by PAV modify their spontaneous breathing in response to changes in thermal environment such that Pco2 levels are appropriately maintained early in postnatal life. This response pattern occurred consistently and is currently of uncertain clinical significance.
Similar content being viewed by others
Main
It is well established that body temperature affects morbidity and mortality in preterm infants (1). However, the “normal” or “optimum” core body temperature range of extremely immature infants who are nursed in incubators is unknown.
Recommendations on body temperatures for newborns and preterm infants have mainly been based on investigations done 20 to 40 y ago (2–4). Thermoneutral temperature, at which the metabolic rate reaches a minimum, is regarded as the “gold standard” for nursing preterm infants in incubators or under radiant warmers. This temperature, however, depends on gestational and postnatal age in extremely low birth weight (ELBW) infants (4). Other investigators suggested keeping these infants at fetal temperature, which is a body temperature of close to 38°C (5).
Thermoregulation, breathing, and metabolism are interlinked in a complex relationship (6). The decrease in body temperature induces continuous breathing after birth (7, 8); however, it may also impair the metabolic response to hypoxia, as shown in rats (9). Small changes in ambient temperature have an age-dependent effect on respiratory rate and pattern postnatally in newborn lambs (10). The stimulus to these changes seems to be a decrease in metabolic rate.
The purpose of this study was to determine the effects of two different target body temperature ranges on respiration in ventilator-dependent ELBW infants. We chose one target range at the higher end and one at the lower end of body temperatures that are commonly targeted in ELBW infants. Those ranges represent temperatures close to fetal temperature versus those regarded as thermoneutral from previous studies in less immature infants. During the study, the infants were supported by proportional assist ventilation (PAV). This ventilatory modality enabled them to express fully their endogenous respiratory pattern (11). Minute ventilation (MV), respiratory rate (RR), tidal volume (Vt), incidence and duration of respiratory pauses, arterial oxygen desaturations <85% associated with respiratory pauses, and blood Pco2 levels were evaluated.
METHODS
Subjects
All ELBW infants who were admitted to intensive care in our unit were enrolled in the study when they met the following inclusion criteria:1) birth weight <1000 g, 2) postnatal age 2–14 d, 3) presence of regular spontaneous respiratory activity, 4) requiring mechanical ventilation, 5) stable pulmonary and cardiovascular condition, and 6) informed parental consent. Exclusion criteria were 1) major congenital anomalies, 2) intracranial hemorrhage more than grade II, 3) sepsis, 4) major surgery except status post patent ductus arteriosus ligation, and 5) endotracheal tube leak >20% of the Vt, measured as the difference between the inspiratory and expiratory volume under the respiratory mode before the infant entered the study.
Most of the infants received parenteral nutrition. All were fed breast milk or preterm formula through an indwelling nasogastric tube every 3 h. Caloric intake and composition of feeds did not vary within the same infant during the study period. Differences in total caloric intake were small in infants of similar age. Sedative or analgesic drugs were not applied. Infants were nursed in a supine position in incubators (model 8000 SC or 8000 IC; Dräger, Lübeck, Germany) and were dressed only with a small diaper.
Protocol
The study protocol and the parental consent form were approved by the institutional review board at the University of Munich, Germany. Each infant was exposed to two target body temperature ranges on each of 2 consecutive days. Low normal body temperature was defined as a temperature target value of 36.1–36.5°C measured at the anterior abdominal wall above the liver. High normal body temperature was defined as values of 37.7–37.9°C. The sequence of the two target body temperature ranges was randomized using sealed opaque envelopes. It was reversed on day 2 of the study. This study design was chosen to exclude sequence and carryover effects. Each of the two temperature ranges was applied over approximately 3 h, of which the last 2 h were recorded giving a total of 8 h of recording per infant. The ambient temperature was manually adjusted to keep the abdominal temperature constant. The humidity in the incubator was kept at 80%. The circulation of air inside the incubator did not vary between the two study conditions (velocity 8 cm/s). After nursing procedures, the incubator outlets were closed and 30–45 min were allowed to achieve steady-state temperature conditions. When core body temperature changes did not exceed 0.2°C over a period of 15 min, recordings were started. After the first recording episode, followed by blood sampling, the temperature of the incubator was changed to achieve the alternate target temperature. Nursing procedures were then started and restricted to 30–40 min. The study segments were started at the same time of the day in each individual infant. There were, however, between-infants differences in the time of the study onset.
Measurements
Temperature settings.
Skin temperature measurements were obtained from two different sites: from the anterior abdominal wall above the liver, representing a core body temperature value, and from the foot on the outer side of the first toe, representing a peripheral body temperature. Rectal temperature was recorded from a probe inserted 2 cm into the rectum. All body temperature probes were thermistors (HP 21091 without shield; Hewlett Packard, Böblingen, Germany) with a small thermal mass. Skin temperature probes were insulated with a double-layer foam pad (Microfoam, 3M, St. Paul, MN, U.S.A.). Ambient temperature was measured by a metal surface probe (HP 21078A) mounted 10 cm above the head of the infant within the incubator. The temperature of the inner wall of the incubator was measured by a thermometer taped to the incubator wall (T690; Thermo Schneider, Wertheim, Germany). All temperature probes were calibrated to a precision of ± 0.1°C with a glass precision thermometer (25E; Thermo Schneider) in a water bath before each recording period.
Ventilatory settings.
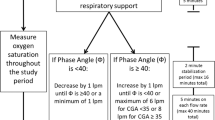
The infants were ventilated with a Stephanie Infant Ventilator (Stephan Biomedical, Gackenbach, Germany) and received PAV throughout the study. The fraction of inspired oxygen was adjusted when pulse-oximetry readings were <85% and >96% for >10 s. All other ventilator settings were not modified during the study. The end-expiratory pressure previously chosen by the clinical team was kept constant throughout the study. For applying PAV, the upper airway pressure limit was set at the peak inspiratory pressure level as used with the ventilatory mode before the study. The gain of resistive unloading was set at 25 H2O · L−1 · s−1 (2.5 mm inner diameter (ID) endotracheal tube) or at 40 cm H2O · L−1 · s−1 (2.0 mm ID endotracheal tube) to approximately compensate for the resistance of the endotracheal tube. The elastic unloading gain was determined individually by increasing it from 0 cm H2O/mL to a level at which the infant was breathing with least chest wall distortions (12). In an additional attempt to determine an appropriate elastic unloading gain for each infant individually, the degree of elastic unloading was briefly increased until overcompensation occurred and then reduced below this threshold. It was finally adjusted to a level in this range when the infant adopted the most regular breathing pattern and when appropriate Vts were achieved. Backup conventional mechanical ventilation was automatically initiated 8 s after cessation of spontaneous breathing (in the first four infants of the study after 2 s). Three infants required shorter intervals of 2–4 s for the initiation of backup ventilatory support because frequent oxygen desaturations <85% occurred during apneic pauses. When a spontaneous breath recurred, backup ventilation was automatically suppressed and PAV was resumed. The temperature of the inspired air was kept at 37°C in every infant throughout the study.
Pco2.
Pco2 was measured at the end of each recording in arterial blood samples from indwelling umbilical arterial lines or from capillary and venous samples when no arterial catheter was in place. The same method of sampling was applied within the same infant during the study.
Assessment of infant behavior.
For establishing an adequate sampling period without periods of vigorous activity, the infants were observed continuously and their activity was assessed every 5 min on a five-point scale adapted from Brück et al.(2). Behavior was coded as follows: 0 = quiet sleep, no movements; 1 = active asleep, occasional movements; 2 = quiet awake, occasional movements; 3 = active awake, body movements; 4 = vigorous activity, such as kicking and crying. Moderate, not continuously occurring movements were tolerated during the recording periods. Recordings were interrupted when states 3 and 4 on the scale were reached. A time average of the activity scores was calculated by dividing the sum of activity scores by the number of assessments.
Data Processing and Analysis/Statistics
The tracings of airflow, airway pressure, and fraction of inspired oxygen were obtained from the analogue outlets of the ventilator; heart rate, pulse oximetry, and body and ambient temperatures were obtained from the analogue outlet of a cardiorespiratory monitor (Viridia CMS; Hewlett Packard). All signals were digitized at 100 Hz and recorded on disk using data acquisition software (Windaq Pro+; Dataq Instruments, Akron, OH, U.S.A.).
Data analysis was done by two computer programs (Windaq Playback, Dataq Instruments; and Labdat, Nelson Claure, Miami, FL, U.S.A.). MV and Vt were calculated by integration of the airflow signal over time. The means of all variables in an infant were determined as the arithmetic mean of all samples over the cumulative period of 4 h for each temperature setting. A respiratory pause was defined as cessation of breathing for the average duration of three breaths. The duration of backup ventilation was calculated for each infant as percentage of the duration of backup ventilation to total recording time under each target temperature. When this percentage exceeded 2% of total recording time, the calculation of MV was based exclusively on the time the infant spent under PAV.
MV was defined as primary outcome criterion. Secondary outcome criteria were respiratory rate, Vt, incidence and duration of respiratory pauses, number of desaturations <85%, Pco2, and heart rate. The differences of the four recorded temperatures in the two conditions were additionally evaluated. Two-tailed t tests on paired observations were applied after testing for normality according to Kolmogorov-Smirnov.
RESULTS
Twenty infants were enrolled in the study. Their gestational age was 25 ± 1 wk (mean ± SD), birth weight was 696 ± 155 g, age at study was 5 ± 3 d, and weight at study was 649 ± 153 g. The mothers of nine infants had received 24 mg of betamethasone; the others received a partial antenatal steroid course (12 mg of betamethasone). Eighteen infants were born by cesarean section; 14 were female, and four were small for gestational age. All but one had received exogenous surfactant; none was on early postnatal dexamethasone treatment. One infant received indomethacin therapy for patent ductus arteriosus, and two were on theophylline treatment.
In four infants, the study had to be truncated after 1 d for the following reasons: improvement in respiratory condition allowing extubation, poor respiratory drive precluding PAV, inadvertent change in ventilator settings violating the protocol, and long-lasting gross body movements with frequent changes of behavioral state. In two of the 20 studied infants, recording time had to be shortened to 90 min in one temperature range because opening of the portholes became necessary.
Temperatures.
Mean skin temperature of the anterior abdominal wall was 1.4°C higher in the higher target temperature range (p < 0.001;Table 1). The mean peripheral temperature difference between the two target conditions was 2.3°C (p < 0.001;Table 1). The core to periphery temperature gradient was significantly larger in the low normal temperature range (1.8°C versus 0.9°C). Rectal temperature was nearly identical to the anterior abdominal wall temperature (Table 1). Ambient temperature was approximately 2°C lower than anterior abdominal wall temperature in the two target conditions (Table 1).
Ventilatory variables.
MV was significantly higher in the upper target temperature range with mean values of 314 mL · min−1 · kg−1versus 291 mL · min−1 · kg−1, which represents a difference of 7% (Table 1). This was mainly due to an increase in RR from 56 ± 7/min in the lower temperature range to 61 ± 8/min in the higher temperature range (8% difference; p < 0.001). Vt remained largely unchanged (5.25 ± 0.6 versus 5.19 ± 0.6 mL in both temperature ranges).
The incidence and duration of respiratory pauses per hour did not differ between target temperature conditions. Desaturations <85% occurred rarely, and their number and average duration were not different between the two conditions (Table 1).
Backup ventilation for >2% of total recording time was present in five infants. The time spent in backup ventilation was not different between the two target conditions.
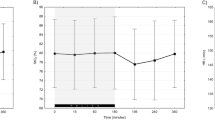
Arterial blood samples could be obtained from an umbilical line in all but six infants (capillary blood sampling was done in two, and venous sampling was done in four other infants). The measured Pco2 was statistically not higher in the higher temperature range (Table 1). In case this represents a β error, we can still rule out (given our sample size of n = 20) with 90% certainty that this difference is >2.7 mm Hg. MV, RR, Vt, and Pco2 of each infant in the lower and in the higher temperature range are presented in Fig. 1. The heart rate was higher in the warmer environment (155 ± 9/min versus 142 ± 9/min; p < 0.001). The behavioral assessment showed a higher mean score in the low temperature range, which indicates more restlessness and less quiet sleep (Table 1).
DISCUSSION
Previous observations in term newborn infants (13) and studies on newborn lambs (10) have shown an elevated RR in a warmer than thermoneutral climate (14). Our study adds new results for the human extremely immature infant very early in postnatal life under conditions of PAV to these previous findings. We found that an increase in mean body temperature of 1.4°C to a level close to fetal temperature induced a rise in MV of 7%, whereas Vts and blood CO2 levels were closely maintained. Incidence and duration of respiratory pauses were not different between the two body temperature ranges. These investigations were performed with the infants undergoing PAV, a mode that allows unrestricted control of all variables of the ventilatory pattern by the infant. We therefore assume that the recorded breathing pattern data represent the infants' endogenous respiratory drive.
In contrast to earlier publications on larger infants without mechanical respiratory support (15, 16), we did not find an increased rate of respiratory pauses in the warmer environment. Our recordings, however, were not started before body temperature did not change for >0.2°C over a 15-min interval. We did not record the breathing pattern during an increase or a decline in body temperature, i.e. during the transitional periods between the target steady-state conditions. Therefore, our data do not allow conclusions about changes in the respiratory pattern that may occur during transitional temperature states.
This population of extremely premature infants was able to express a different respiratory pattern in the higher temperature range compared with the lower range. In other words, PAV enabled them to mount a respiratory response to a change in their climate. Ventilation was appropriately modified under these changes in condition as evidenced by maintenance of close to identical Pco2 levels. This demonstrates that ELBW infants, when supported by PAV, are able to control their arterial Pco2 levels within a narrow range when body temperature is close to fetal body temperature.
The difference in environmental conditions between the two target temperature ranges was associated with a major difference in the core to periphery temperature gradient. The larger gradient in the colder environment likely represents an active thermoregulatory response with peripheral vasoconstriction.
Our data may suggest that the metabolic rate, i.e. oxygen consumption and CO2 production, was higher near fetal temperature because our infants' alveolar ventilation was higher without a decrease in blood Pco2 levels. This may indicate that the neural component of the ventilation–CO2 feedback loop is appropriately developed at this very early gestational and postnatal age. Heart rate increased significantly with the higher temperature in our study population. It has been shown in exercising children (17) that there is a linear relationship between the pulse rate and oxygen consumption. However, hot climates tend to shift the oxygen consumption–heart rate plot to the right, i.e. there are more beats per minute for the same caloric levels in hot climates compared with cool climates (18). Also, earlier studies on immature, nonventilated preterm infants did not show an increased oxygen consumption at central body temperatures of 37.5°C (3) or an increased heat production when rectal temperature increased rapidly (19). Riesenfeld et al.(13) examined the effect of temperatures close to heat stress conditions on respiratory water loss, oxygen consumption, and CO2 production in term infants on their first day of life. He showed that RR and respiratory water loss increased significantly when rectal temperature rose to 37.8°C or when the infants started sweating. Oxygen consumption and CO2 production, however, did not increase in the absence of motor activity. To answer definitely the question of whether a core body temperature close to fetal body temperature increases energy expenditure in ELBW infants compared with lower temperatures requires the application of techniques to measure oxygen consumption directly.
The increased RR may also reflect an attempt to dissipate excess heat. The thermoneutral state is assumed to range from 36 to 37°C abdominal skin temperature in premature infants of 1000 to 1500 g of body weight (3) or between 36.7 and 37.3°C core temperature in infants of 29 to 34 wk gestational age (4). In this state, body temperature is regulated mainly through changes in peripheral skin blood flow and heat exchange with the environment via radiation, convection, and conduction. Evaporative heat loss plays a minor part when ambient humidity is kept at a high level. Evaporative heat loss can be increased considerably when an upper critical temperature of the ambient and body temperature is surpassed (20, 21). Heat-dissipating mechanisms are limited in preterm infants, because sweating is not yet developed and passive loss of water by diffusion through the skin is reduced in a high-humidity climate (22). Therefore, peripheral vasodilation and water evaporation from the surfaces of the respiratory tract are the only possibilities to eliminate heat. When body temperature rises above an upper critical temperature, the breathing pattern becomes more rapid and shallow, increasing dead space ventilation while alveolar ventilation is maintained constant (6). This breathing pattern is also called thermal polypnea, or panting. Panting as defined in lambs (10) represents a major increase in RR, much higher than the average increase observed in our infants. Their respiratory rate was on average 5 breaths per minute higher in the higher temperature range compared with the lower one, whereas Vt remained largely unchanged. Therefore, our findings are compatible with the assumption that close to fetal body temperature heat-dissipating mechanisms begin to evolve but panting has not fully developed.
In conclusion, this study on extremely immature infants of early postnatal age demonstrates that relatively minor changes in core body temperature within a range that is commonly accepted in routine clinical care induce pronounced and consistent changes in spontaneous breathing. This demonstrates that these infants' endogenous respiratory control system is sensitive to such changes in environmental conditions that are likely also associated with changes in energy expenditure. When supported by PAV, these infants can obviously mount an appropriate ventilatory response to such changes in their thermal condition. Whether the type and magnitude of the observed changes suggest clinically important longer-term effects is unknown. None of the observed changes, however, conveys any obvious adverse effects.
Abbreviations
- ELBW:
-
extremely low birth weight
- MV:
-
minute volume
- PAV:
-
proportional assist ventilation
- RR:
-
respiratory rate
- Vt:
-
tidal volume
References
Sinclair JC 1995 Effect of the thermal environment on neonatal mortality and morbidity: state of the evidence. In: Okken A, Koch J (eds) Thermoregulation of Sick and Low Birth Weight Neonates. Springer, Berlin, pp 127–141.
Brück K, Parmelee A, Brück M 1962 Neutral temperature range and range of thermal comfort in premature infants. Biol Neonate 4: 32–51
Silverman WA, Sinclair JC, Agate FJ 1966 The oxygen cost of minor changes in heat balance of small newborn infants. Acta Paediatr Scand 55: 294–300
Sauer PJ, Dane HJ, Visser HK 1984 New standards for neutral thermal environment of healthy very low birthweight infants in week one of life. Arch Dis Child 59: 18–22
Lemburg P 1995 Thermal monitoring of very preterm infants. Which temperature should be measured. In: Okken A, Koch J (eds) Thermoregulation of Sick and Low Birth Weight Infants. Springer, Berlin, pp 63–68.
Mortola JP, Frappell PB 2000 Ventilatory responses to changes in temperature in mammals and other vertebrates. Annu Rev Physiol 62: 847–874
Kuipers IM, Maertzdorf WJ, De Jong DS, Hanson MA, Blanco CE 1997 Initiation and maintenance of continuous breathing at birth. Pediatr Res 42: 163–168
Harned HS, Ferreiro J 1973 Initiation of breathing by cold stimulation: effects of change in ambient temperature on respiratory activity of the full-term fetal lamb. J Pediatr 83: 663–669
Frappell P, Westwood K, Maskrey M 1995 Ventilatory and metabolic responses to hypoxia during moderate hypothermia in anesthetized rats. J Appl Physiol 79: 256–260
Andrews DC, Symonds ME, Johnson P 1991 Thermoregulation and the control of breathing during non-REM sleep in the developing lamb. J Dev Physiol 16: 27–36
Schulze A, Bancalari E 2001 Proportional assist ventilation in infants. Clin Perinatol 28: 561–578
Schulze A, Gerhardt T, Musante G, Schaller P, Claure N, Everett R, Gomez-Marin O, Bancalari E 1999 Proportional assist ventilation in low birth weight infants with acute respiratory disease: a comparison to assist/control and conventional mechanical ventilation. J Pediatr 135: 339–344
Riesenfeld T, Hammarlund K, Sedin G 1990 The effect of a warm environment on respiratory water loss in fullterm newborn infants on their first day after birth. Acta Paediatr Scand 79: 893–898
Andrews DC, Johnson P 1991 Breathing pattern and brain surface temperature interactions during pyrogenic responses in the developing lamb. J Physiol 438: 243P
Perlstein PH, Edwards NK, Sutherland JM 1970 Apnea in premature infants and incubator-air-temperature changes. N Engl J Med 282: 461–466
Bohnhorst B, Heyne T, Peter CS, Poets CF 2001 Skin-to-skin (kangaroo) care, respiratory control, and thermoregulation. J Pediatr 138: 193–197
Cumming GR, Friesen W 1967 Bicycle ergometer measurement of maximal oxygen uptake in children. Can J Physiol Pharmacol 45: 937–946
Bradfield RB 1971 A technique for determination of usual daily energy expenditure in the field. Am J Clin Nutr 24: 1148–1154
Hey EN, Katz G 1970 The optimum thermal environment for naked babies. Arch Dis Child 45: 328–334
Risbourg B, Vural M, Kremp O, de Broca A, Leke L, Freville M 1991 Neonatal thermoregulation. Turk J Pediatr 33: 121–134
Gordon CJ 1990 Thermal biology of the laboratory rat. Physiol Behav 47: 963–991
Sedin G, Hammarlund K, Riesenfeld T, Sjörs G, Strömberg B 1991 Water and heat balance in newborn infants. In: Lemburg P, Koch J (eds) Zukünftige Entwicklung medizinischer Technik in der Pädiatrie II. Drägerwerk AG, Lübeck, pp 63–75.
Acknowledgements
We thank the parents of our study participants and the nursing staff of our neonatal ward for interest in and support of this work. The authors thank Annegret Hofmiller for helpful assistance in recording the data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funded by the German Research Council (Deutsche Forschungsgemeinschaft Schu 931/2-1).
Rights and permissions
About this article
Cite this article
Rieger-Fackeldey, E., Schaller-Bals, S. & Schulze, A. Effect of Body Temperature on the Pattern of Spontaneous Breathing in Extremely Low Birth Weight Infants Supported by Proportional Assist Ventilation. Pediatr Res 54, 332–336 (2003). https://doi.org/10.1203/01.PDR.0000076664.65100.FF
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000076664.65100.FF
This article is cited by
-
Apnea of prematurity: from cause to treatment
European Journal of Pediatrics (2011)
-
Adaptive mechanical backup ventilation for preterm infants on respiratory assist modes – a pilot study
Intensive Care Medicine (2006)