Abstract
Autoimmune lymphoproliferative syndrome (ALPS) is characterized by autoimmune features and lymphoproliferations and is generally caused by defective Fas-mediated apoptosis. This report describes a child with clinical features of ALPS without detectable Fas expression on freshly isolated blood leukocytes. Detection of FAS transcripts via real-time quantitative PCR made a severe transcriptional defect unlikely. Sequencing of the FAS gene revealed a 20-nucleotide duplication in the last exon affecting the cytoplasmic signaling domain. The patient was homozygous for this mutation, whereas the consanguineous parents and the siblings were heterozygous. The patient reported here is a human homologue of the Fas-null mouse, inasmuch as she carries an autosomal homozygous mutation in the FAS gene and she shows the severe and accelerated ALPS phenotype. The heterozygous family members did not have the ALPS phenotype, indicating that the disease-causing FAS mutation in this family is autosomal recessive.
Similar content being viewed by others
Main
ALPS is characterized by lymphadenopathy, splenomegaly, accumulation of nonmalignant CD4−CD8−TCRαβ+ T cells, and several autoimmune features, such as autoantibody production and autoimmune hemolytic anemia (1). It is caused by a defect in apoptosis mediated by Fas (also designated CD95, Apo1, or Apt1). ALPS features are highly comparable to the phenotype of mice with lpr or gld mutations, which carry an autosomal recessive mutations in the FAS gene or in the gene encoding Fas ligand (FASL), respectively, causing autoimmunity, lymphoproliferations and accumulation of CD4−CD8−TCRαβ+ T cells (2–4). There are three mouse strains carrying different FAS mutations i.e. the lpr, the lprcg and the Fas-null strains (2, 5). Although these mice have a similar phenotype, there are differences in severity and the time of development of the symptoms (6).
Both FasL and Fas are transmembrane proteins, which belong to the tumor necrosis factor and tumor necrosis factor receptor family, respectively (7, 8). Fas is expressed as a trimer on peripheral activated lymphocytes and also in tissues such as liver, lung, heart, and ovary. The intracellular part of the Fas protein contains a death domain, which is essential for the induction of apoptosis on interaction of Fas and FasL trimers (9). Fas-mediated apoptosis is needed for the elimination of autoreactive T lymphocytes that escaped thymic selection, but seems not to be involved in negative selection of immature cells in the thymus (10–12). The Fas-FasL interaction also appears to be important in B cell homeostasis and is involved in the control of immune responses (13, 14). A soluble form of Fas without the transmembrane domain (FasΔTM) has been shown to be capable of inhibiting Fas-mediated apoptosis by blocking membrane bound FasL in vitro (15). The human FAS gene consists of 9 exons and is located on chromosome 10 (16–18).
The patients with ALPS that have been described thus far show largely comparable clinical features, with variation in severity (1, 19–24). We herein present a new patient in whom Fas protein expression studies were followed by extensive molecular analysis of the FAS gene of the patient as well as her parents and siblings. The unique genotype and phenotype of this patient are discussed in the context of previously described patients with ALPS and the different mouse strains with distinct FAS gene mutations.
METHODS
Clinical report.
The patient is a girl from consanguineous parents. She has three healthy siblings, but two other siblings died at the ages of 1.5 and 2 y. Immediately after the girl's birth, petechiae, generalized edema, and hepatosplenomegaly were noticed. During the first month of life, autoantibodies against red blood cells and platelets were demonstrated. A liver biopsy showed extensive extramedullary hematopoiesis. In PB-MNC, a high percentage (15%) of CD4−CD8−TCRαβ+ T cells was observed. Hypergammaglobulinemia (IgG, 13.8 g/L; IgM, 0.85 g/L; IgA, 2.48 g/L) remained persistent for several years. At the age of 8 mo, she had massive generalized adenopathy of the cervical, mesenterial, and para-aortal lymph nodes and chronic pulmonary disease not responding to bronchodilation and not associated with detection of pathogens.
Flow cytometric immunophenotyping of PB-MNC and lymph node biopsy specimens indicated that 30% and 70% of cells, respectively, were CD4−CD8−TCRαβ+ T cells. Figure 1A shows the T lymphoblast infiltration in the lymph node. Lymphoproliferative responses to the mitogens PHA, ConA, PWM, ProtA, and SAC, and the CD3 (OKT3) antibody indicated no functional T and B cell impairment. Analysis of a lymph node biopsy was suggestive of a T cell non-Hodgkin's lymphoma, but TCRB analysis did not show monoclonal or oligoclonal rearrangements. Skin biopsy specimens taken during relapse showed IgM and complement depositions in the dermis consistent with lupus-like disease. At the same time, rheumatoid factors (IgM and IgA) as well as autoantibodies against nuclear antigens, smooth muscle, striated muscle, and neutrophil cytoplasmic antigens were demonstrated in serum. Subsequently, the girl remained in a stable condition without hemolytic anemia, and her pulmonary function improved gradually. At the age of 4–5 y, she had maculopapular to nodular skin abnormalities on the face and on both arms and legs. Clinically this skin disease resembled mycosis fungoides. Skin biopsies showed the histopathologic aspects of malignant cutaneous T cell lymphoma (Fig. 1B). Approximately 30% of T cells in the dermal infiltrates were CD3+CD4+CD8−. DNA analysis showed biallelic TCRB gene rearrangements in one of the biopsy specimens, but not in others, making mycosis fungoides less likely. A bone marrow biopsy did not reveal abnormal T cells. Immunophenotyping of PB-MNC yielded normal results. The girl was diagnosed with ALPS and during the following years she became increasingly ill. Her lung disease required continuous oxygen administration. The paresis of the right arm and diaphragm persisted, whereas the cutaneous symptoms had a chronically intermittent course. She finally died at the age of 8 y as a result of pulmonary failure.
Blood samples and DNA and RNA extraction.
PB samples from the patient, her parents, and three healthy siblings, as well as from healthy control subjects were obtained. MNC were isolated from PB by Ficoll density centrifugation (Ficoll-Paque; density, 1.077 g/mL; Pharmacia, Uppsala, Sweden). After Ficoll density centrifugation, both MNC and granulocyte fractions were used for DNA extraction with the phenol-chloroform method and for RNA extraction using the method according to Chomczynski and Sacchi (25).
Immunophenotyping.
Double and triple flow cytometric immunophenotyping was performed to study Fas (CD95) expression on granulocytes, monocytes, and CD4+CD3+, CD8+CD3+, CD45RO+CD3+, and CD45RA+CD3+ T lymphocyte subpopulations. For this purpose, 50 μL of whole blood or MNC was incubated with 50 μL of various combinations of FITC, phycoerythrin, and phycoerythrin-cyanin-5 conjugated with CD95 (UB-2 and CH11; Immunotech, Marseille, France), CD95 (DX-2; PharMingen, San Diego, CA), CD95 (7C11; Beckman Coulter, Fullerton, CA), CD3 (HIT3a), CD4 (Leu-3a), CD8 (Leu-2a), CD45RO (UCHL1; Becton Dickinson, San Jose, CA), and CD45RA (2H4; Coulter Clone, Hialeah, FL) antibodies for 10 min at room temperature. After incubation, the cells were washed, and, in the case of whole blood, the erythrocytes were lysed with lysing solution (Becton Dickinson). Appropriate isotype controls were performed in every test.
To quantitate the density of Fas expression in terms of numbers of molecules of equivalent soluble fluorochrome, the fluorescence intensity was calibrated using Quantum FITC premixed microbead standards (Flow Cytometry Standard Corp., San Juan, PR).
To investigate Fas expression on stimulated T lymphocytes, PB-MNC were cultured (0.5 × 106 cells/mL) in RPMI 1640 medium with Glutamax-I, supplemented with 100 U/mL penicillin, 100 μg/mL streptomycin, and 10% FCS in the presence of PHA (0.2 μg/mL). The cells were maintained for 7 d at 37°C in a humidified atmosphere of 5% CO2 in air. Fas expression was evaluated daily with triple immunostainings as described above.
RT-PCR and RQ-PCR.
cDNA was prepared from mRNA using AMV reverse transcriptase (Promega, Madison, WI). RT-PCR was performed with different combinations of the cDNA primers EU, ED, CU and CD (see Fig. 4) to amplify parts of the coding region (EU: CTGGGAATTCCTACCTCTGGTTCTTACGTCTG, ED: CATGAATTCATCAAGGAATGCACACTCACC, CU: TGAGAAGCTTGGTTTTCCTTTCTGTG, CD: CTAGACCAAGCTTGGATTTCATTTC). RT-PCR conditions were 1 min at 94°C, 1 min at 60°C, and 2 min at 72°C for 35 cycles. The PCR products were separated on a 6% polyacrylamide gel.
RT-PCR analysis of FAS mRNA. A, Schematic diagram of FAS mRNA encoding the extracellular, transmembrane (TM), and cytoplasmic domain. Four primers for RT-PCR are indicated as well as the size of the two ED-CD RT-PCR products, including and excluding the transmembrane domain. B, PAGE analysis of the ED-CD RT-PCR products of the patient and a healthy control subject. The two products of the patient are larger in comparison to those of the healthy control subject.
For the quantification of FAS mRNA, we performed RQ-PCR with ABI Prism 7700 Sequence Detection (PE Biosystems, Foster City, CA) (26). Two FAS primers and a Taq Man probe were designed with the ABI Prism Primer Express (PE Biosystems) (FASTM5′: TCCTCAAGGACATTACTAGTGACTCAG, FASTM3′: ATCTTTTCAAACACTAATTGCATATACTCAG, FAS Taq Man probe labeled with FAM reporter dye: GAAATCCAAAGCTTGGTCTAGAGTGAAAAACAAC). During the PCR the Taq Man probe first hybridizes to the DNA target, followed by primer annealing. The emission of the reporter dye of the Taq Man probe is quenched until the probe is cleaved by the exonuclease activity of the Taq polymerase, generating a fluorescent reporter signal.
The RQ-PCR conditions were 2 min at 50°C for the AmpErase Uracil N-glycosylase step, 10 min at 95°C to activate Ampli Taq Gold, followed by 50 cycles of 15 s at 95°C and 1 min at 60°C. Taq Man GAPDH control reagents (PE Biosystems) were used to quantify the amount of cDNA in the reaction.
PCR of genomic DNA and heteroduplex analysis.
For amplification of genomic DNA, nine primer sets were designed to amplify each of the nine exons. All primers were positioned in the introns, at least 25 base pairs upstream or downstream of the splice sites of the involved exons. The conditions for PCR analysis of genomic DNA were essentially the same as for the RT-PCR method. PCR products were further analyzed by heteroduplex analysis to detect potential differences between the exons of the two alleles. After denaturation (5 min at 94°C) and renaturation (1 h at 4°C), the resulting duplexes (hetero- and/or homoduplexes) were separated in nondenaturing 6% polyacrylamide gels (27).
Southern blot analysis.
Genomic DNA samples of 20 μg were digested with Eco RI, Bam HI, Hin dIII, or Sac I. The restriction fragments were separated in 0.7% agarose gels, transferred to Nytran-13N nylon membranes (Scheichler and Schuell, Dassel, Germany), and hybridized with exon 1, exon 3, and exon 9 probes (28). The probes were generated by PCR amplification of the exons using MNC DNA from a healthy individual and radioactively labeled with [α-32P]dATP and [α-32P]dCTP using the random primer labeling method.
Sequence analysis.
The products of both RT-PCR and genomic PCR amplification were sequenced with the T7 Sequence Kit (Pharmacia) using 35S radiolabeling after cloning in pMosBlue (Amersham Int., Amersham, UK), and the fragments were run in a denaturing 8% polyacrylamide sequence gel. Exons were also analyzed by cycle sequencing on the ABI 373 fluorescent sequencer (PE Biosystems).
RESULTS
Fas protein expression.
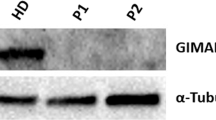
In contrast to healthy children and adults, the granulocytes, monocytes, and CD45RO+ T lymphocytes of the patient did not express detectable levels of Fas protein (Fig. 2A). The absence of Fas expression on MNC of the patient was confirmed with three different CD95 antibodies (data not shown). Two family members showed intermediate Fas protein expression (Fig. 2B), but they did not show any of the clinical features. Furthermore, PB-MNC were stimulated in vitro with PHA to induce Fas protein expression on activated and proliferating T lymphocytes. As expected, within 2 d of culture, virtually all MNC of healthy control subjects expressed Fas (Fig. 3A). Maximum levels of Fas density per cell were reached after 4 to 5 d of culture (Fig. 3B). In contrast, only a small fraction of the patient's MNC (10–20%) expressed Fas at low density levels, which were 5 to 6-fold lower than in healthy control subjects (Fig. 3).
Fas (CD95) expression on freshly obtained blood leukocytes of the patient and a healthy control subject. A, Dot plots show CD95 (UB-2) expression vs side scatter (SSC) of the leukocytes. In the healthy control subject, Fas expression is found on granulocytes, monocytes, and a part of the lymphocytes. Detailed immunophenotyping revealed that natural killer cells and B lymphocytes do not express detectable levels of Fas, whereas CD45RO+ T lymphocytes are Fas-positive. This is in contrast to the patient, who did not show detectable Fas levels on any leukocyte subset. B, Fas expression on CD3+ T lymphocytes of healthy control subjects, family members, and the patient. Healthy control subjects show strong positivity on a subset of the T lymphocytes, whereas other T cells are weakly positive. The T lymphocytes of the parents show intermediate Fas expression, whereas the majority of the T lymphocytes in the siblings are weakly Fas-positive, with comparable intensity as a T cell subset in healthy control subjects. The patient's T lymphocytes are negative for Fas expression. The low number of events in the patient is caused by lymphopenia.
Fas (CD95) expression on cultured MNC from the patient and healthy control subjects. A, PHA-stimulated MNC cultures of healthy age-matched and adult control subjects resulted in Fas expression on virtually all MNC within 2 d. These MNC mainly consisted of CD45RO+CD3+ T lymphocytes, as was the case in the patient's culture. However, only a minor fraction of the patient's cells expressed Fas. B, The density of the Fas expression (number of molecules of equivalent soluble fluorochrome, MESF values) in the patient was essentially lower than in the healthy control subjects.
RT-PCR analysis of FAS mRNA.
The observation that FAS RT-PCR products could be generated with the four primers EU, ED, CU, and CD (Fig. 4A) indicated that FAS mRNA was expressed in leukocytes from the patient. cDNA amplification with the ED and CD primers, which are located in the extracellular and cytoplasmic regions, respectively, should generate two products: one including and one excluding the transmembrane region (Fig. 4A). Both in the healthy control subjects and in the patient, two PCR products were obtained, indicating that both splice variants were present. However, the two products of the patient were found to be larger compared with those of healthy control subjects (Fig. 4B). This suggested that there may be a defect in the cytoplasmic region.
Quantification of FAS mRNA by RQ-PCR.
RQ-PCR was subsequently performed to determine whether the amount of FAS mRNA in MNC of the patient was comparable to that of healthy control subjects. In RQ-PCR, the CT is a measure of the amount of template present in the sample. A GAPDH housekeeping gene control reaction was performed to check for the amount of cDNA in the reaction mixture, which was found to be equal (similar CT values) in the patient and the two healthy control subjects (Fig. 5A). Figure 5B shows that the amount of FAS mRNA in the patient equals the amount present in the healthy control subjects, as evidenced from the similar CT values.
Heteroduplex PCR analysis and sequencing of FAS exons.
All FAS exons were amplified using intron primers, and the resulting PCR products were subjected to heteroduplex analysis to find possible allelic differences. Heteroduplex analysis is based on denaturation and renaturation of the PCR products, leading to the formation of one homoduplex in a homozygous situation and two homoduplexes as well as two heteroduplexes in a heterozygous situation. Homo- and heteroduplexes can be separated by PAGE on the basis of the differences in conformation. Heteroduplexes are more retarded in a polyacrylamide gel because of mismatches or bulging loops. At low renaturation temperatures (<20°C) some single-strand PCR products will remain that have a different (generally lower) mobility compared with heteroduplexes in gel electrophoresis. Using this assay for PCR products derived from exons 1 to 8, only homoduplexes and no heteroduplexes were found in the patient, her family members, and healthy control subjects. Moreover, in these exons, no size differences were found between patient, siblings, and control subjects (data not shown). However, the homoduplexes of the PCR products of exon 9 of the patient and control subjects showed a difference in size similar to that seen with the ED and CD primers in the RT-PCR analysis (Fig. 6, A and B), suggesting that the patient was homozygous for a larger exon 9 product. Hemizygosity of the FAS gene in the patient was excluded, because Southern blot analysis showed equal band intensities in the patient and control subjects, suggesting the presence of two FAS alleles without major deletions or rearrangements (data not shown). In the family members, we identified two homoduplexes, representing the allele with the normal and the one with the larger exon 9 product, as well as two heteroduplexes, representing cross-annealed single-strand fragments of the two alleles (Fig. 6B). These findings were further supported by the presence of two single-strand bands in the lanes of samples from the patient and control subject, which represent the coding and noncoding fragments of the homozygous alleles. In the lanes of samples from the family members, three single-stranded bands were observed, representing the coding and noncoding fragments of the two different alleles, two of which probably comigrated (Fig. 6B).
PCR and sequence analysis of the FAS gene. A, Schematic representation of the entire FAS gene. The enlarged exon 9 consists of a coding region (shaded) and 3′ untranslated region (UTR) (blank). Primers 9U and 9D were used for amplification and subsequent analysis of exon 9. B, Heteroduplex analysis of exon 9 PCR products of the patient, her family members, and five healthy control subjects. The control subjects and the patient (last lane) are homozygous for exon 9 as evidenced from the presence of one homoduplex and two single-strand bands. The homoduplex of the patient is larger than the homoduplex of the control subjects. The presence of two homoduplexes and two heteroduplexes shows that the family members are heterozygous for exon 9. C, Sequence analysis of exon 9 using the 9D primer. The duplication of 20 base pairs in the patient is indicated. D, Predicted amino acid sequence of the C-terminus of the patient's Fas protein in comparison to the wild-type Fas protein sequence.
Sequencing of FAS exon 9 revealed a duplication of 20 nucleotides (Fig. 6C). In the cDNA, the same mutation was found. This duplication causes a frameshift resulting in an extended predicted protein (Fig. 6D). The six C-terminal amino acids (Glu-Ile-Gln-Ser-Leu-Val) are replaced by 37 amino acids. The second and third amino acids in the altered reading frame are not changed as a result of the duplication. Sequencing of all other exons revealed no additional mutations.
DISCUSSION
The patient reported here developed the classic features of ALPS immediately after birth. She showed all phenotypic characteristics, including cutaneous lupus-like disease at a later stage. Moreover, the patient showed histologically malignant lymph nodes, although monoclonal or oligoclonal rearrangements could not be detected on TCRB gene analysis. Both the early onset and the extensiveness of the ALPS characteristics suggest that the phenotype of the reported patient was very severe compared with other patients with ALPS that have previously been described (Table 1). The consanguineous parents and siblings of the patient did not show these autoimmune features and lymphoproliferations.
Immunophenotyping demonstrated that leukocytes of the patient did not show detectable levels of Fas protein, whereas the expression on leukocytes of the family members was intermediate. In vitro stimulation of PB-MNC resulted in low levels of Fas expression on only a minor fraction of the proliferating T cells. This suggests that Fas protein can potentially be expressed, but only with strong stimuli in vitro. Molecular analysis was performed to determine the genotype of the patient. RT-PCR data showed that both the FAS and FASΔTM splice variants were present, although they were enlarged in the region encoding the cytoplasmic part of the protein. Quantitative mRNA analysis with RQ-PCR showed that the same amount of FAS mRNA was present in the patient compared with the healthy control subjects. This made a transcriptional defect unlikely. Heteroduplex PCR analysis of the FAS gene exons and sequencing analysis showed that the patient had a homozygous duplication of 20 bp in the death domain encoding exon 9. The patient is most probably not hemizygous for this mutation, because Southern blot analysis of the patient did not show any abnormality compared with healthy control subjects and family members. The duplication introduces a frameshift resulting in a longer predicted protein, which might be less stable or defective in proper transport to the cell surface. Both parents and siblings were heterozygous for this mutation and did not show typical ALPS features. Therefore, this patient carries a unique homozygous recessive mutation in the FAS gene.
All previously described patients with ALPS are phenotypically largely comparable as is shown in Table 1. However, considerable differences are found in severity, age of onset, and in the presence or absence of some specific characteristics. All patients showed lymphoproliferations, but the manifestation of the autoimmune features varied. Even siblings or other family members carrying the same mutation (patients 1a and b, patients 10 a, b, and c, and patients 13 a, b, and c) showed differences in the extent of autoimmune features (19, 21, 23). In lpr and lprcg mice, FAS mutations result in lymphoproliferations, whereas autoimmunity in these mice is strongly influenced by the genetic background (29). The collective patient data suggest that also in man genetic background might influence the clinical manifestation of autoimmune features.
On the basis of different genotypes, three groups of patients with ALPS can be distinguished. The first group includes patients with a heterozygous FAS mutation (patients 1–10 in Table 1), suggesting a dominant-negative defect in Fas-mediated apoptosis. Healthy family members of these patients with ALPS who have a heterozygous FAS mutation showed defects in in vitro Fas-mediated apoptosis without clearly showing the clinical symptoms, although some of the family members of patients 3, 4, 6, and 10 in Table 1 did show a few ALPS symptoms. In case a particular mutation does not cause clinical symptoms in the family members, it might well be that the involved FAS mutation is not the single cause of ALPS in these children. It is likely that another defect, for example affecting FasL or downstream signaling molecules of Fas-mediated apoptosis, is inherited from the parent without the FAS gene defect. Candidates for Fas-mediated signaling defects are proteins that associate with the death domain, such as RIP, FADD, and FLICE (30–33). One could speculate that in this situation, ALPS may result from a digenic defect. In that case the FAS mutation might be called autosomal recessive, although this can formally only be proven in a clinically symptomatic individual showing the homozygous FAS mutation. It remains unclear whether another defect is also present in heterozygous family members showing only a few clinical symptoms of ALPS. So far, symptomatic heterozygous Fas-deficient mice have not been described.
A second group of patients with ALPS (patients 11-13 in Table 1) is associated with biallelic recessive mutations. In these patients, both alleles are affected, whereas heterozygous family members do not show clinical symptoms. Our patient reported here (patient 11) carries the same mutation on both alleles and is therefore homozygous for this recessive FAS gene mutation. Recessive mutations are also found in the lpr, lprcg, and Fas-null mice. Lpr mice having a transposon in intron 2 are able to express low levels of normal FAS mRNA, implying that they are not completely deficient for Fas. Lprcg mice express Fas protein on the membrane, although this protein is not functional because of one amino acid substitution. Fas-null mice are completely Fas protein deficient and display the same phenotype as lpr mice, but the phenotype is more severe and accelerated in presentation. Fas-null mice also have liver cell hyperplasia, which is not seen in lpr and lprcg mice (5). Therefore, it is clear that the type of FAS gene mutation determines the level of (aberrant) protein expression and thereby influences the severity of the phenotype. The patient studied in this report (patient 11) carries a homozygous mutation affecting the cytoplasmic tail of the protein. This mutation severely affects Fas protein expression. Patient 12 also lacks Fas expression because of a homozygous deletion of the last 290 bp. Both patients had ALPS from birth on and showed all characteristic ALPS symptoms. It is therefore tempting to compare these human FAS gene mutations with the murine Fas-null mutation, in which deletion of the death domain also affects Fas protein expression. However, the hepatomegaly in our patient was not clearly caused by liver cell hyperplasia, but was probably caused by erythropoiesis and some swelling of the hepatocytes. There was no striking difference in nuclear sizes in comparison with an age-matched liver from a girl who died of sudden infant death syndrome.
The patients described by Bettinardi et al. (21) (patients 13 a, b, and c) also have double mutations, but these concern different missense point mutations on the two alleles. These mutations do not seem to disturb trimerization, but result in the expression of a Fas trimer on the membrane, which is apparently not entirely functional. The slightly reduced Fas expression in these patients was explained by reduced density rather than by a conformational change. On the basis of severity, age of onset, and type of mutation, these patients are phenotypically and genotypically similar to lprcg mice.
In addition, yet a third group of patients with ALPS has been reported by Sneller et al. (22) and Dianzani et al. (34). These patients show the same clinical features, but do not carry a FAS gene mutation. Probably, a defect in FasL or in the signaling pathway downstream of Fas, gives rise to deficient Fas-mediated apoptosis.
In summary, ALPS is caused by defective Fas-mediated apoptosis related to a monoallelic defect in the FAS gene, possibly accompanied by an additional defect and thereby potentially recessive, although there are some examples in which dominant inheritance of the FAS gene cannot be excluded. A biallelic defect in the FAS gene is another possibility for ALPS. The mutation found in the patient studied here clearly demonstrated recessive inheritance of ALPS. The syndrome can also be found in patients lacking a FAS mutation. The severity of the syndrome as determined by the presence of the typical ALPS characteristics and the age of onset is dependent on the type of mutation. Decreased levels of trimer Fas expression seem to result in milder ALPS forms, whereas complete absence of the Fas protein as observed in our patient induces the severe ALPS phenotype.
Abbreviations
- ALPS:
-
autoimmune lymphoproliferative syndrome
- TCR:
-
T cell receptor
- PB:
-
peripheral blood
- MNC:
-
mononuclear cells
- TCRB:
-
TCRβ gene
- RT-PCR:
-
reverse transcriptase PCR
- RQ-PCR:
-
real-time quantitative PCR
- GAPDH:
-
glyceraldehyde-3-phosphate dehydrogenase
- CT:
-
cycle number in which the fluorescent signal exceeds the threshold value
References
Fisher GH, Rosenberg FJ, Straus SE, Dale JK, Middleton LA, Lin AY, Strober W, Lenardo MJ, Puck JM 1995 Dominant interfering Fas gene mutations impair apoptosis in a human autoimmune lymphoproliferative syndrome. Cell 81: 935–946
Sneller MC, Straus SE, Jaffe ES, Jaffe JS, Fleisher TA, Stetler-Stevenson M, Strober W 1992 A novel lymphoproliferative/autoimmune syndrome resembling murine lpr/gld disease. J Clin Invest 90: 334–341
Watanabe-Fukunaga R, Brannan CI, Copeland NG, Jenkins NA, Nagata S 1992 Lymphoproliferation disorder in mice explained by defects in Fas antigen that mediates apoptosis. Nature 356: 314–317
Takahashi T, Tanaka M, Brannan CI, Jenkins NA, Copeland NG, Suda T, Nagata S 1994 Generalized lymphoproliferative disease in mice, caused by a point mutation in the Fas ligand. Cell 76: 969–976
Adachi M, Suematsu S, Kondo T, Ogasawara J, Tanaka T, Yoshida N, Nagata S 1995 Targeted mutation in the Fas gene causes hyperplasia in peripheral lymphoid organs and liver. Nat Genet 11: 294–300
Adachi M, Suematsu S, Suda T, Watanabe D, Fukuyama H, Ogasawara J, Tanaka T, Yoshida N, Nagata S 1996 Enhanced and accelerated lymphoproliferation in Fas-null mice. Proc Natl Acad Sci USA 93: 2131–2136
Itoh N, Yonehara S, Ishii A, Yonehara M, Mizushima S, Sameshima M, Hase A, Seto Y, Nagata S 1991 The polypeptide encoded by the cDNA for human cell surface antigen Fas can mediate apoptosis. Cell 66: 233–243
Takahashi T, Tanaka M, Inazawa J, Abe T, Suda T, Nagata S 1994 Human Fas ligand: gene structure, chromosomal location and species specificity. Int Immunol 6: 1567–1574
Gulbins E, Bissonnette R, Mahboubi A, Martin S, Nishioka W, Brunner T, Baier G, Baier-Bitterlich G, Byrd C, Lang F, Kolesnick R, Altman A, Green D 1995 FAS-induced apoptosis is mediated via a ceramide-initiated RAS signaling pathway. Immunity 2: 341–351
King LB, Ashwell JD 1994 Thymocyte and T cell apoptosis: is all death created equal?. Thymus 23: 209–230
Osborne BA 1996 Apoptosis and the maintenance of homeostasis in the immune system. Curr Opin Immunol 8: 245–254
Singer GG, Abbas AK 1994 The Fas antigen is involved in peripheral but not thymic deletion of T lymphocytes in T cell receptor transgenic mice. Immunity 1: 365–371
Rathmell JC, Cooke MP, Ho WY, Grein J, Townsend SE, Davis MM, Goodnow CC 1995 CD95 (Fas)-dependent elimination of self-reactive B cells upon interaction with CD4+ T cells. Nature 376: 181–184
Lynch DH, Ramsdell F, Alderson MR 1995 Fas and FasL in the homeostatic regulation of immune responses. Immunol Today 16: 569–574
Cheng J, Zhou T, Liu C, Shapiro JP, Brauer MJ, Kiefer MC, Barr PJ, Mountz JD 1994 Protection from Fas-mediated apoptosis by a soluble form of the Fas molecule. Science 263: 1759–1762
Behrmann I, Walczak H, Krammer PH 1994 Structure of the human APO-1 gene. Eur J Immunol 24: 3057–3062
Cheng J, Liu C, Koopman WJ, Mountz JD 1995 Characterization of human Fas gene: exon/intron organization and promoter region. J Immunol 154: 1239–1245
Inazawa J, Itoh N, Abe T, Nagata S 1992 Assignment of the human Fas antigen (FAS) to 10q 24: 1. Genomics 14: 821–822
Rieux-Laucat F, Le Deist F, Hivroz C, Roberts IA, Debatin KM, Fischer A, de Villartay JP 1995 Mutations in Fas associated with human lymphoproliferative syndrome and autoimmunity. Science 268: 1347–1349
Le Deist F, Emile JF, Rieux-Laucat F, Benkerrou M, Roberts I, Brousse N, Fischer A 1996 Clinical, immunological, and pathological consequences of Fas-deficient conditions. Lancet 348: 719–723
Bettinardi A, Brugnoni D, Quiros-Roldan E, Malagoli A, La Grutta S, Correra A, Notarangelo LD 1997 Missense mutations in the Fas gene resulting in autoimmune lymphoproliferative syndrome: a molecular and immunological analysis. Blood 89: 902–909
Sneller MC, Wang J, Dale JK, Strober W, Middelton LA, Choi Y, Fleisher TA, Lim MS, Jaffe ES, Puck JM, Lenardo MJ, Straus SE 1997 Clinical, immunologic, and genetic features of an autoimmune lymphoproliferative syndrome associated with abnormal lymphocyte apoptosis. Blood 89: 1341–1348
Infante AJ, Britton HA, DeNapoli T, Middelton LA, Lenardo MJ, Jackson CE, Wang J, Fleisher T, Straus SE, Puck JM 1998 The clinical spectrum in a large kindred with autoimmune lymphoproliferative syndrome caused by a Fas mutation that impairs lymphocyte apoptosis. J Pediatr 133: 629–633
Lim MS, Straus SE, Dale JK, Fleisher TA, Stetler-Stevenson M, Strober W, Sneller MC, Puck JM, Lenardo MJ, Elenitoba-Johnson KS, Lin AY, Raffeld M, Jaffe ES 1998 Pathological findings in human autoimmune lymphoproliferative syndrome. Am J Pathol 153: 1541–1550
Chomczynski P, Sacchi N 1987 Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem 162: 156–159
Holland PM, Abramson RD, Watson R, Gelfand DH 1991 Detection of specific polymerase chain reaction product by utilizing the 5′-3′ exonuclease activity of Thermus aquaticus DNA polymerase. Proc Natl Acad Sci USA 88: 7276–7280
Langerak AW, Szczepanski T, van der Burg M, Wolvers-Tettero ILM, van Dongen JJM 1997 Heteroduplex PCR analysis of rearranged T cell receptor genes for the diagnosis of suspected T cell proliferations. Leukemia 11: 2192–2199
van Dongen JJM, Wolvers-Tettero ILM 1991 Analysis of immunoglobulin and T cell receptor genes: I. Clin Chim Acta 198: 1–91
Nagata S, Suda T 1995 Fas and Fas ligand:lpr and gld mutations. Immunol Today 16: 39–43
Stanger BZ, Leder P, Lee TH, Kim E, Seed B 1995 RIP: a novel protein containing a death domain that interacts with Fas/APO-1 (CD95) in yeast and causes cell death. Cell 81: 513–523
Grimm S, Stanger BZ, Leder P 1996 RIP and FADD: two “death domain”-containing proteins can induce apoptosis by convergent, but dissociable, pathways. Proc Natl Acad Sci USA 93: 10923–10927
Muzio M, Chinnaiyan AM, Kischkel FC, O'Rourke K, Shevchenko A, Ni J, Scaffidi C, Bertz JD, Zhang M, Gentz R, Mann M, Krammer PH, Peter ME, Dixit VM 1996 FLICE, a novel FADD-homologous ICE/CED-3-like protease, is recruited to the CD95 (Fas/Apo-1) death-inducing signaling complex. Cell 85: 817–827
Muzio M, Salvesen GS, Dixit VM 1997 FLICE induced apoptosis in a cell-free system: cleavage of caspase zymogens. J Biol Chem 272: 2952–2956
Dianzani U, Bragardo M, DiFranco D, Alliaudi C, Scagni P, Buonfiglio D, Redoglia V, Bonissoni S, Correra A, Dianzani I, Ramenghi U 1997 Deficiency of the Fas apoptosis pathway without Fas gene mutations in pediatric patients with autoimmunity/lymphoproliferation. Blood 89: 2871–2879
Acknowledgements
The authors thank Professor Dr. R. Benner for providing continuous support, Professor Dr. B. A. Oostra for critical reading of the manuscript, and T.M. van Os for preparation of the figures. We also thank Sandra de Bruin-Versteeg for technical assistance.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
van der Burg, M., de Groot, R., Comans-Bitter, W. et al. Autoimmune Lymphoproliferative Syndrome (ALPS) in a Child from Consanguineous Parents: A Dominant or Recessive Disease?. Pediatr Res 47, 336–343 (2000). https://doi.org/10.1203/00006450-200003000-00009
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200003000-00009
This article is cited by
-
ALPS, FAS, and beyond: from inborn errors of immunity to acquired immunodeficiencies
Annals of Hematology (2022)
-
Incomplete penetrance in primary immunodeficiency: a skeleton in the closet
Human Genetics (2020)
-
The Autoimmune Lymphoproliferative Syndrome with Defective FAS or FAS-Ligand Functions
Journal of Clinical Immunology (2018)
-
A FAS-ligand variant associated with autoimmune lymphoproliferative syndrome in cats
Mammalian Genome (2017)
-
A Missense Mutation in the Extracellular Domain of Fas: The Most Common Change in Argentinean Patients with Autoimmune Lymphoproliferative Syndrome Represents a Founder Effect
Journal of Clinical Immunology (2012)