Abstract
Postpartum changes in the concentrations of IL-1β, IL-6 tumor necrosis factor-α (TNF-α), transforming growth factor-β1 (TGF-β1), TGF-β2, and prostaglandin E2 in 257 human milk samples collected longitudinally from 49 healthy mothers during the first 12 wk of lactation were determined by ELISA or RIA. The proinflammatory cytokines IL-1β, IL-6, and TNF-α were present in only a proportion of samples, and there was a wide range of concentrations detected at each time in the present study (IL-1β, <15-400 pg/mL; IL-6, <15-1032 pg/mL; TNF-α, <15-2933 pg/mL). Concentrations of prostaglandin E2 increased after the first week and remained elevated for the remainder of the study (range, <10-9966 pg/mL). The antiinflammatory cytokines TGF-β1 (range, 43-7108 pg/mL) and TGF-β2 (range, 208-57935 pg/mL) were present in substantial quantities in all samples, and there was little change in the mean concentration during 12 wk of lactation. The present study shows that immunomodulating agents are normally present in human milk in physiologically relevant quantities for at least the first 3 mo of the breast-fed infant's life.
Similar content being viewed by others
Main
Breast-feeding is associated with a reduction in the incidence of gastrointestinal illness(1–3), respiratory illness(3), and otitis media(1,3). Long-term epidemiologic studies suggest a link between breast-feeding and a lower incidence of some diseases appearing later in life such as type I diabetes(4), allergies(2,3), and Crohn's disease(5). This supports the concept that breast milk contains immunomodulating agents that not only may act directly to neutralize the detrimental effects of pathogens encountered by the infant but also may influence the maturation of the infant's own developing immune system.
Among the many potentially active immunologic components identified in human breast milk are the polypeptide cytokines that often act in femtomolar concentrations to regulate the behavior or properties of cells associated with the immune system. A range of both proinflammatory and antiinflammatory cytokines have been detected by a variety of methodologies in breast milk collected at various stages of lactation. These include IL-1β(6–9), IL-6(8–15), TNF-α(6,8,9,14–18), and TGF-β(8,19–22). Many of these studies had small sample sizes and most looked for the presence of cytokines in colostrum or "early" milk only.
Another family of substances present in human milk that has the capacity to influence physiologic functions of the newborn infant are the lipid eicosanoids such as PGE2(23–25). Prostaglandins are derived from essential fatty acids supplied in the diet and are involved in the modulation of gastric acid and mucous secretion, homeostasis, smooth muscle contraction, cytoprotection, and leukocyte function. More recently, PGE2 has been shown to be associated with the regulation of proinflammatory cytokine production by monocytes and macrophages(26,27).
In this longitudinal study, we used a sensitive and specific ELISA method to determine the concentration of IL-1β, IL-6, TNF-α, TGF-β1, and TGF-β2 in samples obtained sequentially over 12 wk from a large cohort of healthy mothers delivering at term. In addition, we determined the concentration of PGE2 by RIA during this period.
METHODS
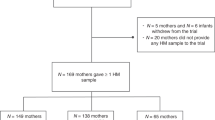
Subjects. Forty-nine mothers who planned to breast-feed for at least 12 wk and who had delivered healthy term infants were recruited from the postnatal ward at Flinders Medical Centre. All women were healthy, aged 18 y or more, and were not taking antiinflammatory medication at the time of enrollment. The present study was approved by the Flinders Medical Centre Committee on Clinical Investigation (Ethics) and written informed consent was obtained from all participants.
Sample collection. In this longitudinal study, milk samples (2-5 mL) were collected from each mother by manual expression into sterile polypropylene containers on d 1-6 and at 2, 4, 6, 8 and 12 wk postpartum either at home or at the hospital. All samples were stored at 4°C and processed within 2 h of collection. After centrifugation at 690 × g for 20 min, the aqueous phase was collected and stored at -80°C until analyzed for cytokine/eicosanoid content. All samples were analyzed for IL-1β, IL-6, and TNF-α within 16 wk of collection and for TGF-β1, TGF-β2, and PGE2 after storage for 20-30 wk. Information regarding recent illnesses or infections and the use of any medications was collected from each mother at each collection time.
Immunoassays for IL-1β, IL-6, TNF-α. ELISA for IL-1β, IL-6, and TNF-α were established using matched antibody pairs (IL-1β, Endogen, Inc., Cambridge, MA; IL-6 and TNF-α, R&D Systems, Minneapolis, MN). Briefly, 96-well flat-bottomed plates (Nalge Nunc International, Naperville, IL) were incubated with 2 µg/mL mouse anticytokine MAb in carbonate/bicarbonate buffer (50 mM, pH 9.6) overnight at room temperature. Each well was washed 3 times with wash buffer (PBS/0.05% Tween 20) and the blocked with PBS/2.5% BSA for 1 h at 37°C. Test samples or cytokine standards (in duplicate) diluted in assay buffer (PBS/0.05% Tween 20/1% BSA) were added to washed wells and incubated for 2 h at 37°C. After washing, biotinylated mouse anti-IL-1β MAb (500 ng/mL) or biotinylated goat anticytokine antibody (IL-6, 25 ng/mL and TNF-α, 200 ng/mL) diluted in assay buffer was added to each well for 2 h at 37°C. Washed wells were incubated with ExtrAvidin alkaline phosphatase (Sigma Chemical Co. BioSciences, St. Louis, MO) at 1:5000 dilution in assay buffer for 1 h at 37°C. After a further three washes, the substrate solution (p-nitrophenyl phosphate in diethanolamine buffer) was added to each well, and the color reaction was allowed to proceed until read on an automatic plate reader at OD 405 nm. The limit of detection for each ELISA was 15 pg/mL. Complete recovery of added recombinant cytokine standards was obtained from expressed breast milk aqueous-phase samples, indicating a lack of interfering substances in these assays.
Immunoassays for TGF-β1 and TGF-β2. ELISA for TGF-β1 and TGF-β2 were established using matched antibody pairs (R&D Systems, Minneapolis, MN) as described above with the following modifications. After coating with MAb, the wells were blocked with PBS/0.05% Tween 20/5% sucrose/0.05% sodium azide for 1 h. Samples (100 µL) were acidified by the addition of 1N HCl (20 µL) for 10 min at room temperature followed by neutralization with 20 µL 1.2N NaOH/0.5 M HEPES. Standards and acidified samples were diluted in 100 mM Tris-HCl/150 mM NaCl/0.05% Tween 20/0.1% essential fatty acid-free BSA, pH 9.6 as required followed by a 1:2 dilution in PBS/0.05% Tween 20/1.4% essential fatty acid-free BSA assay buffer and were incubated for 30 min on a shaker at room temperature followed by 90 min at 37°C. Biotinylated goat anti-TGF-β antibody was used at a concentration of 100 ng/mL. The limit of detection for each ELISA was 30 pg/mL. The recovery of recombinant TGF-β1 and TGF-β2 added to appropriately diluted breast milk samples ranged from 75-85%. According to the manufacturer, there is <1% cross-reactivity between the two isoforms of TGF-β when the appropriate antibody combinations are used.
Immunoassay for PGE2. Aqueous-phase samples were diluted 1:2 in Tris/NaCl buffer and PGE2 concentrations were measured in triplicate by RIA as described previously(28). The limit of detection for the assay was 10 pg/mL.
Data analysis. Cytokine/eicosanoid data are presented as mean ± SEM. For calculations of mean concentrations of groups of all data, those samples below the level of detection were assigned a value of half the limit of detection, i.e. 7.5 pg/mL for IL-1β, IL-6, and TNF-α and 5 pg/mL for PGE2. Because the point of left truncation is very small when compared with the mean, this manipulation of the data introduces only a small error, i.e. there is little change in the calculated mean whether those samples below the level of detection are assigned a value of 15, 7.5, or 0 pg/mL. The relationships between immune factors at each time were determined by Pearson correlation using SPSS for Windows 6.0 (SPSS Inc., Chicago, IL), as were the associations between subject characteristics and cytokine/eicosanoid concentration.
RESULTS
Subject characteristics. Forty-nine women between 18-38 y of age and parity 1-5 were recruited into the study. Twelve (24%) of the participants smoked cigarettes, 78% had delivered vaginally, and, at each collection time, a maternal illness or infection was reported by 11-27% of mothers who provided a sample. Each mother provided a colostral sample 1-6 d after delivery. Additional milk samples were obtained from 48 of these mothers at wk 2 (d 11-17), 45 at wk 4 (d 24-33), 42 at wk 6 (d 39-47), 37 at wk 8 (d 53-60), and 36 at wk 12 (d 80-88). Ninety-seven percent (250/257) of samples were collected from mothers who reported that they were exclusively breast-feeding their infants.
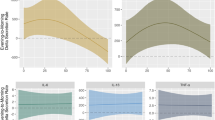
Postpartum changes in cytokine/eicosanoids. Cytokine/eicosanoid levels in human milk samples collected at each time postpartum are presented in Figures 1–3 (individual data points) and Tables 1 and 2 (mean ± SEM, range). At each time, the mean concentration of each cytokine/eicosanoid was compared with all other cytokines/eicosanoid. No associations were found. There was no correlation between smoking, birth type, or maternal illness/infection and cytokine or PGE2 concentration.
IL-1β, IL-6, and TNF-α (Table 1 and Fig. 1,A-C) were detected in 5-51% of samples collected at each time in the study. Overall, mean levels seemed to be higher in early milk and then decreased as lactation continued. With each of these cytokines, there was a wide range of concentrations detected at each time in the study (Fig. 1,A-C).
After acidification, TGF-β1 and TGF-β2 (Fig. 2 and Table 2) were detected in all samples tested throughout the study. TGF-β2 was present in approximately 10-fold higher amounts than TGF-β1, and there was a wide range of values at each time of lactation. There was little change in the mean concentration of either isoform of TGF-β present in milk samples during the first 12 wk of lactation.
PGE2 (Fig. 3 and Table 2) was detected in the aqueous phase of 47/49 (96%) colostral samples, 41/42 (98%) milk samples collected at wk 6, and all remaining samples tested. PGE2 content increased from early lactation and then remained steady for the period of the study.
Cytokine profile of milk from individual mothers over 12 wk lactation. The longitudinal design of the study enabled us to investigate the relationship between different breast milk cytokines of individuals from delivery to 12 wk postpartum. Of 36 mothers who provided a sample at every time, seven did not have detectable levels of any of the proinflammatory cytokines (IL-1β, IL-6, TNF-α) at any stage of lactation. In some other individuals, these proinflammatory cytokines seemed to track together over time; however, overall no consistent pattern of association between the cytokines measured was observed. There was no relationship between the appearance of the proinflammatory cytokines and maternal reports of an infection or illness immediately preceding or at the time of milk collection. The postpartum changes in TGF-β1 and TGF-β2 seemed to follow each other in some individuals, although there was no statistically significant association between the two. High levels of proinflammatory cytokines were not statistically associated with low levels of immunosuppressive cytokines in any individual.
DISCUSSION
The composition of human milk is subject to change during lactation; however, there is little known about postpartum changes in its immunologic constituents. This is the first comprehensive study investigating a range of cytokines in colostrum and milk samples obtained from delivery to 3 mo postpartum from a single large cohort of women. Our results clearly show the extensive heterogeneity in the concentration of all cytokines measured as well as PGE2 in milk among subjects at each collection time.
There is diversity in the reported values for the proinflammatory cytokines in human breast milk (Table 3). Our finding of IL-1β present in a small proportion of samples is in contrast with the data described by both Srivastava et al.(8) and Basolo et al.(15) who were unable to detect any IL-1β and Munoz et al.(6) who reported IL-1β at high concentrations in all colostral samples tested (Table 3). Similarly, our data for IL-6 contrast with reports of low amounts of colostral and mature milk IL-6 (maximum 34 and 42 pg/mL, respectively) by one group(8) but are comparable to data for colostrum from other authors(9,13) (Table 3). Although IL-6 shares many proinflammatory functions with IL-1β and TNF-α, it has also been associated with the local production of IgA in the breast(10), which may be an important function in the breast-fed infant.
The presence of substantial amounts of two soluble TNF receptors (sTNFRI and sTNFRII) in colostrum and milk has been described(18). These receptors can bind TNF-α and thus reduce the amount of "free" antigen available for detection by an ELISA that is unable to recognize both free and bound antigen. However, the matched antibody pairs purchased for the establishment of the TNF-α ELISA used in the present study have been shown to have no significant cross-reactivity or interference with either soluble receptor and, hence, measure total TNF-α (R&D Systems, Technical Service, personal communication). Indeed, our results are in the ranges reported by Buescher and Malinowska(18) who used an enzyme-amplified sensitivity immunoassay based on multiple MAb that enabled recognition of total (free plus bound) antigen and Na et al.(14), rather than the extremely low concentrations (<2-26 pg/mL) that had also been reported(8) (Table 3).
TGF-β is synthesized and secreted as a biologically inactive complex associated with a precursor molecule that is designated the latency-associated peptide. Active TGF-β can be released from the latency-associated peptide by a variety of treatments, the most common being acidification, which is a possible mechanism of activation in the infant gut. In the present study, free TGF-β was not detected in any samples; however, after acidification, all colostrum/milk samples contained considerable amounts of TGF-β1 and TGF-β2. In general, both isoforms of TGF-β seem to have overlapping biologic activities in vitro; however, TGF-β2 was present at approximately 10-fold greater concentrations than TGF-β1 throughout our study. It is likely that each isoform has specific roles, as suggested by studies with TGF-β1 null mice in which the TGF-β1 "knockout" offspring develop an excessive inflammatory response leading to cellular infiltration of vital organs and death at 3-5 wk of age(29). The null newborn pups survive initially, apparently due to maternal sources of TGF-β1 via both placental transfer and then milk while suckling(30). These studies indicate that the immunosuppressive properties of TGF-β are both conserved after ingestion by the neonatal pup and are vital for immune regulation. In addition to the immunosuppressive properties of the TGF-β family, other functions likely to be of significance to the breast-fed infant are involvement in the induction of oral tolerance(21,31,32), stimulation of IgA isotype switching in B cells(33), and maintenance of intestinal epithelium barrier function(34).
The role of PGE2 in breast milk is unclear. Although synthesis of IL-1β and TNF-α by monocytes/macrophages can be inhibited by PGE2 in vitro(26,27), which may account for some of its down-regulating effects on lymphocyte proliferation, there was no statistical association between cytokine and PGE2 concentrations in our study.
The broad range of concentrations of IL-1β, IL-6, TNF-α, TGF-β1, TGF-β2, and PGE2 in milk samples collected during the first 12 wk of lactation and the lack of correlation among them makes interpretation difficult. Analysis of our data indicates that factors such as smoking, birth type, and maternal illness/infection did not contribute to the wide variation in values. Time since last feed and whether the sample was fore milk, hind milk, or a complete expression may, however, be confounding variables. Samples from individual mothers did not contain consistently high (or low) levels of either proinflammatory or antiinflammatory cytokines, although there was a trend for both isoforms of TGF-β to follow a parallel pattern of change throughout lactation. It is apparent from the existing literature that whereas TGF-β and PGE2 are consistently present in human milk samples in readily detectable quantities(8,25), there are huge discrepancies in reported values (and incidence) of cytokines such as IL-1β, IL-6, and TNF-α (Table 3). These differences are not readily explained by differences in methodology, stage of lactation, or maternal characteristics.
Our data support the accumulating evidence that immunomodulating agents are normally present throughout lactation in quantities that have the potential to exert in vivo effects on the recipient infant. For most in vitro applications, cytokines exert their biologic activity in the concentration range of 1 pg/mL to 10 ng/mL. A newborn infant consumes 400-500 mL of breast milk per day, and consumption increases to approximately 800 mL/d by 3 mo of age(35). Therefore, although the mean concentration of some of the cytokines measured decreased as lactation continued, many infants would be consuming nanogram or microgram amounts per day throughout the first 3 mo of life. The specific immunologic effects of cytokines in human breast milk are likely to be determined by the balance between a number of bioactive factors with complementary and competing activities. Breast milk clearly contains components with immunosuppressive properties that provide a mechanism for evolving immune tolerance and thus protect against the development of overt inflammation and immunologically mediated diseases. On the other hand, the presence of proinflammatory cytokines in breast milk may be important in activating the developing neonatal immune system and in providing immunologic protection in the infant with an immature cytokine network.
Abbreviations
- IL-1β:
-
interleukin-1β
- IL-6:
-
interleukin-6
- TNF-α:
-
tumor necrosis factor-α
- TGF-β:
-
transforming growth factor-β
- PGE2:
-
prostaglandin E2
References
Dewey KG, Heinig MJ, Nommsen-Rivers LA 1995 Differences in morbidity between breast-fed and formula-fed infants. J Pediatr 126: 696–702
Howie PW, Forsyth JS, Ogston SA, Clark A, Florey CD 1990 Protective effect of breast feeding against infection. BMJ 300: 11–16
Beaudry M, Dufour R, Marcoux S 1995 Relation between infant feeding and infections during the first six months of life. J Pediatr 126: 191–197
Metcalfe MA, Baum JD 1992 Family characteristics and insulin-dependent diabetes. Arch Dis Child 67: 731–736
Koletzko S, Sherman P, Corey M, Griffiths A, Smith C 1989 Role of infant feeding practices in development of Crohn's disease in childhood. BMJ 298: 1617–1618
Munoz C, Endres S, van der Meer J, Schlesinger L, Arevalo M, Dinarello C 1990 Interleukin-1 beta in human colostrum. Res Immunol 141: 505–513
Soder O 1987 Isolation of interleukin-1 from human milk. Int Arch Allergy Appl Immunol 83: 19–23
Srivastava MD, Srivastava A, Brouhard B, Saneto R, Groh-Wargo S, Kubit J 1996 Cytokines in human milk. Res Commun Mol Pathol Pharmacol 93: 263–287
Sone S, Tsutsumi H, Takeuchi R, Matsuda K, Imai S, Ogra PL, Chiba S 1997 Enhanced cytokine production by milk macrophages following infection with respiratory syncytial virus. J Leukoc Biol 61: 630–636
Saito S, Maruyama M, Kato Y, Moriyama I, Ichijo M 1991 Detection of IL-6 in human milk and its involvement in IgA production. J Reprod Immunol 20: 267–276
Rudloff HE, Schmalstieg FC Jr, Palkowetz KH, Paszkiewicz EJ, Goldman AS 1993 Interleukin-6 in human milk. J Reprod Immunol 23: 13–20
Bocci V, von Bremen K, Corradeschi F, Franchi F, Luzzi E, Paulesu L 1993 Presence of interferon-gamma and interleukin-6 in colostrum of normal women. Lymphokine Cytokine Res 12: 21–24
Eglinton BA, Roberton DM, Cummins AG 1994 Phenotype of T cells, their soluble receptor levels, and cytokine profile of human breast milk. Immunol Cell Biol 72: 306–313
Na HR, Daniels LC, Seelig LL Jr 1997 Preliminary study of how alcohol consumption during pregnancy affects immune components in breast milk and blood of postpartum women. Alcohol Alcohol 32: 581–589
Basolo F, Conaldi PG, Fiore L, Calvo S, Toniolo A 1993 Normal breast epithelial cells produce interleukins 6 and 8 together with tumor-necrosis factor: defective IL6 expression in mammary carcinoma. Int J Cancer 55: 926–930
Rudloff HE, Schmalstieg FC Jr, Mushtaha AA, Palkowetz KH, Liu SK, Goldman AS 1992 Tumor necrosis factor-alpha in human milk. Pediatr Res 31: 29–33
Mushtaha AA, Schmalstieg FC Jr, Hughes TK Jr, Rajaraman S, Rudloff HE, Goldman AS 1989 Chemokinetic agents for monocytes in human milk: possible role of tumor necrosis factor-alpha. Pediatr Res 25: 629–633
Buescher ES, Malinowska I 1996 Soluble receptors and cytokine antagonists in human milk. Pediatr Res 40: 839–844
Noda K, Umeda M, Ono T 1984 Transforming growth factor activity in human colostrum. Gann 75: 109–112
Saito S, Yoshida M, Ichijo M, Ishizaka S, Tsujii T 1993 Transforming growth factor-beta (TGF-beta) in human milk. Clin Exp Immunol 94: 220–224
Ishizaka S, Kimoto M, Tsujii T, Saito S 1994 Antibody production system modulated by oral administration of human milk and TGF-beta. Cell Immunol 159: 77–84
Palkowetz KH, Royer CL, Garofalo R, Rudloff HE, Schmalstieg FC Jr, Goldman AS 1994 Production of interleukin-6 and interleukin-8 by human mammary gland epithelial cells. J Reprod Immunol 26: 57–64
Le Deist F, de Saint Basile G, Angeles Cano E, Griscelli C 1986 Prostaglandin E2 and plasminogen activators in human milk and their secretion by milk macrophages. Am J Reprod Immunol Microbiol 11: 6–10
Lucas A, Mitchell MD 1980 Prostaglandins in human milk. Arch Dis Child 55: 950–952
Chappell JE, Clandinin MT, Barbe GJ, Armstrong DT 1983 Prostanoid content of human milk: relationships to milk fatty acid content. Endocrinol Exp 17: 351–358
Hart PH, Whitty GA, Piccoli DS, Hamilton JA 1989 Control by IFN-gamma and PGE2 of TNF-alpha and IL-1 production by human monocytes. Immunology 66: 376–383
Haynes DR, Whitehouse MW, Vernon-Roberts B 1992 The prostaglandin E1 analogue, misoprostol, regulates inflammatory cytokines and immune functions in vitro like the natural prostaglandins E1, E2, and E3. Immunology 76: 251–257
Caughey GE, Mantzioris E, Gibson RA, Cleland LG, James MJ 1996 The effect on human tumor necrosis factor α and interleukin 1β production of diets enriched in n-3 fatty acids from vegetable oil or fish oil. Am J Clin Nutr 63: 116–122
Kulkarni AB, Karlsson S 1993 Transforming growth factor-beta 1 knockout mice. Am J Pathol 143: 3–9
Letterio JJ, Geiser AG, Kulkarni AB, Roche NS, Sporn MB, Roberts AB 1994 Maternal rescue of transforming growth factor-beta 1 null mice. Science 264: 1936–1938
Gray JD, Hirokawa M, Horwitz DA 1994 The role of transforming growth factor-beta in the generation of suppression: an interaction between CD8+ T and NK cells. J Exp Med 180: 1937–1942
Strober W, Kelsall B, Fuss I, Marth T, Ludviksson B, Ehrhardt R, Neurath M 1997 Reciprocal IFN-gamma and TGF-β responses regulate the occurrence of mucosal inflammation. Immunol Today 18: 61–64
van Vlasselaer P, Punnonen J, De Vries JE 1992 Transforming growth factor-beta directs IgA switching in human B cells. Immunol 148: 2062–2067
Planchon SM, Martins CA, Guerrant RL, Roche JK 1994 Regulation of intestinal epithelial barrier function by TGF-beta 1. J Immunol 153: 5730–5739
Department of Nutrition, Dietetics, and Food Science, Curtin University of Technology (ed) 1992 Dietitian's Pocket Book. Curtin University of Technology, Perth
Acknowledgements
The authors thank Mark Neumann, Kieran McCaul, and Brett Jeffrey for statistical analysis and data management; Jenny Osmond, Jane Armstrong, and Lyn Pullen for nursing and administrative assistance; and Ela Zielinski and Maryanne Demasi for technical assistance.
Author information
Authors and Affiliations
Additional information
Supported in part by the Flinders University of South Australia, University Research Budget Project Grant.
Rights and permissions
About this article
Cite this article
Hawkes, J., Bryan, DL., James, M. et al. Cytokines (IL-1β, IL-6, TNF-α, TGF-β1, and TGF-β2) and Prostaglandin E2 in Human Milk during the First Three Months Postpartum. Pediatr Res 46, 194–199 (1999). https://doi.org/10.1203/00006450-199908000-00012
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199908000-00012
This article is cited by
-
The immune response to sub-clinical mastitis is impaired in HIV-infected women
Journal of Translational Medicine (2018)
-
Maternal breast milk transforming growth factor-beta and feeding intolerance in preterm infants
Pediatric Research (2014)
-
Changes in immunomodulatory constituents of human milk in response to active infection in the nursing infant
Pediatric Research (2012)
-
Probiotics and dietary counselling targeting maternal dietary fat intake modifies breast milk fatty acids and cytokines
European Journal of Nutrition (2012)
-
The Effects of Formula Feeding on Physiological and Immunological Parameters in the Gut of Neonatal Rats
Digestive Diseases and Sciences (2009)