Abstract
Dexamethasone is widely used in the postnatal period. Its impact on retinopathy of prematurity (ROP) is extremely controversial; published studies have found a detrimental, protective, or no effect on ROP. The goal of this study was to test the hypothesis that use of dexamethasone during the injury phase (oxygen exposure) reduces the severity of oxygen-induced retinopathy (OIR) in a mouse model. C57BL6 mice pups were exposed to either room air or hyperoxia (75% FiO2) from postnatal d 7 through 12 (PN7-12) with or without dexamethasone (0.5 mg/kg/d s.c.) and killed on PN17-21. Retinopathy was assessed by a scoring system of retinal flat mount preparations and periodic acid-Schiff (PAS) staining of retinal sections. Pups exposed to dexamethasone and oxygen had a lower median retinopathy score of 5 (4,6) [median (25th, 75th quartile)] compared with animals exposed to oxygen alone with median score of 9 (6,10) with p < 0.001. PAS staining for extra retinal neovascularization in the dexamethasone and oxygen treated animals showed a significant reduction in number of nuclei extending beyond the inner limiting membrane when compared with oxygen exposed alone (p = 0.04). Animals treated with dexamethasone had decreased weight gain compared with control animals. Dexamethasone did not appear to affect the normal development of retinal vasculature as assessed by the scoring system when compared with control animals. Thus, dexamethasone decreases severity of OIR without having an adverse effect on normal retinal vascular development in the mouse model. We speculate that dexamethasone decreases the injury response that occurs during the hyperoxic phase, thus protecting the developing vasculature and improving the subsequent retinopathy.
Similar content being viewed by others
Main
Retinopathy of prematurity (ROP), previously termed "retrolental fibroplasia," is a serious vasoproliferative disorder of the retina(1) affecting premature infants. Although many infants have complete resolution of their ROP, some infants progress to develop myopia, poor visual acuity, and blindness(2). With the past and present improvements in neonatal intensive care, the number of extremely low birth weight infants surviving has increased dramatically, resulting in a new generation of children severely visually impaired or blind as a result of ROP(3,4). Their number will probably rise as the neonatal care is expected to improve further in the future. In spite of the advances in neonatal medicine in recent years, no measures are available yet to prevent or to reduce the severity of ROP. Once threshold ROP is established, cryotherapy(5) or laser surgery(6–8) are used to treat the more severe forms of ROP that lead to unfavorable visual outcomes of blindness or severe visual impairment. Even with cryotherapy, 47% of these premature babies had unfavorable visual outcome at 5½ years of age(2).
ROP has a multifactorial etiology. The leading risk factors are birth weight, gestational age, and the number of days on supplemental oxygen. Prolonged mechanical ventilation is associated with bronchopulmonary dysplasia, a severe debilitating chronic lung disease of tiny babies. Corticosteroids are used during the postnatal period in premature babies in two different regimens: the "early" (≤2 wk of age) and "late" (≥2 wk of age) regimen(9–16) for prevention of chronic lung disease (CLD) and for weaning from mechanical ventilation and oxygen supplementation, respectively.
La Motte(17) speculated in 1952 on the potential beneficial effect of adrenal corticotropin hormone on retrolental fibroplasia based on the observation that hyperadrenalism in the post-operative period inhibits the growth of capillaries. In recent years, several clinical studies attempted to assess the effect of postnatal corticosteroids on ROP. The conclusions of these studies are varied(9,11,14–15,17–26). Some have found that use of corticosteroids is associated with an increase in severity of ROP, but others found a protective or no effect at all. The effect of steroids on ROP is controversial as there are no controlled prospective randomized human studies to assess this effect. Recent reports describe a protective effect of antenatal corticosteroids on the development of ROP(27–29). The purpose of this study was to assess the effects of dexamethasone in a mouse model of retinopathy and to test the hypothesis that early use of postnatal corticosteroids during the "critical period" of injury, defined as the period of oxygen exposure, will protect against the development of oxygen-induced retinopathy (OIR) in the mouse.
METHODS
Animal model and dexamethsone experiments. The protocol was approved by the Georgetown University Animal Care and Use Committee. C57BL6 mice were obtained from Taconic Laboratories (Germantown, NY). Mice exposed to oxygen treatment were placed with their nursing dam in an infant incubator (Ohmeda, Inc., Columbia, MD) from PN7 (postnatal d 7) through PN12 as previously described(30). The oxygen flow was adjusted to keep the concentration in the incubator at 75 ± 2% FiO2. Oxygen concentration was measured using a Hudson Oxygen Analyzer (Hudson Ventronics, Temecula, CA) and was checked at least twice daily during the period of exposure. Animals assigned to dexamethasone treatment group were given a single dose of 0.5 mg/kg/d of dexamethasone (American Reagent Laboratories, Inc., Shirley, NY) s.c. in the nape of the neck for 5 d beginning at PN7. This dose is comparable to that used in clinical settings for prevention of CLD or weaning from mechanical ventilation. On PN12 animals were removed from the oxygen and placed in room air. From PN12 through PN17-20 all animal groups were kept in room air and then killed by a lethal intraperitoneal injection of sodium pentobarbital (Abbott Laboratories, North Chicago, IL). The greatest neovascular response occurred in this model from PN17 to 21(30), and thus all animals were killed at PN17-20 in these studies. Animal weights were recorded on PN7, PN12, and PN17-20. A log of animal death was kept throughout the experiment.
Fluorescein dextran perfusion of the retinal blood vessels. To study the retinal vascular pattern, systemic perfusion was performed(31) using high molecular weight (MW = 2 000 000) fluorescein-conjugated dextran (Sigma Chemical Co., St. Louis, MO) in PBS (GIBCO, Grand Island, NY). Briefly, animals were given a lethal dose of sodium pentobarbital and a median sternotomy was performed. The left ventricle was identified and perfused with fluorescein-conjugated dextran (50 mg/mL in 4% PBS) using a 1-mL tuberculin syringe with a 27-gauge needle. Eyes were then enucleated and placed in 4% paraformaldehyde (Sigma Chemical Co.) in PBS for 4 to 24 h. Using a dissecting microscope, the retina was removed and a flat mount was prepared by making radial cuts. A coverslip was applied over the retinae after placing a drop of 2% gelatin (Sigma Chemical Co.). The edge of the coverslip was sealed with transparent nail polish. The scoring of retinal whole mounts was performed using fluorescent microscopy. Each retina was scored by at least two independent observers in a masked fashion using the retinopathy scoring system(32) as shown in Table 1 and the average retinopathy score for each animal was used for statistical analysis.
Periodic acid-Schiff (PAS) stain of retinal sections. Mice were killed on PN17-20 using sodium pentobarbital. After midline sternotomy was performed, the left ventricle was injected with 4% paraformaldehyde in PBS. The eyes were enucleated, placed immediately in optimum cutting temperature embedding compound (Sakura Fine Tek, Inc., Torrence, CA), and frozen at -70°C. Serial sections (8-9 microns thick) over a minimum of 450 microns were cut in a sagittal plane through the cornea, parallel to the optic disc. Tissue sections were stained with periodic acid-Schiff (PAS) reagent and hematoxylin(33). Multiple sections from individual eyes were scored in a masked fashion using light microscopy counting all nuclei extending beyond the inner limiting membrane into the vitreous as previously described(30). A minimum of six sections at least 50 microns apart were evaluated and counted per eye and then averaged. The average number of neovascular nuclei for each eye was used in the statistical analysis.
Animal growth and death. To assess the effect of dexamethasone and 5 d of oxygen exposure on animal well being, a log of animal death was kept throughout the experiment. Weights were recorded on PN7, PN12, and PN17-20 using a laboratory balance.
Statistical analyses. Each retina was scored by two independent observers. The scores were averaged for the two eyes and each animal had one retinopathy score, which was used for statistical analysis. Analysis of variance using the Kruskal-Wallis test was performed to test for differences among the various treatment groups. Mann-Whitney tests were used to compare the total retinopathy scores and the retinopathy subscores between groups. t tests were used to compare nuclei count and animal weight. Statistical significance was defined as p < 0.05. Interobserver variability for the retinal scoring system was assessed by using the Kendall's tau-b correlation coefficient test.
RESULTS
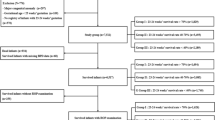
Total retinopathy scores and subscores. Dexamethasone significantly decreased the total retinopathy scores as shown in Figure 1. Control animals (n = 11) had a median total retinopathy score [median (25th, 75th quartile)] of 1 (0.5, 1.5). Animals treated with dexamethasone only (n = 17) had a total retinopathy score of 0.5 (0,1). Oxygen exposed animals (n = 14) had a median total retinopathy score of 9(6,10) versus oxygen and dexamethasone treated animals (n = 12) with median total retinopathy score of 5(4,6). The correlation between the observers' retinopathy scores was significant at the 0.01 level by the Kendall's tau-b (Fig. 2) demonstrating concordance of the independently obtained scores.
Total retinopathy scores - control and oxygen treated animals with and without dexamethasone. Animals exposed to 75% oxygen had median retinopathy score of 9. Animals exposed to oxygen and dexamethasone had median retinopathy score of 5 (p < 0.001). There is no difference (p = 0.31) in retinopathy scores between control animals and those treated only with dexamethasone. Data are shown as median ± 25th-75th quartile. Oxygen exposed animals are indicated by (○) and control animals by (·).
Animals treated with dexamethasone and oxygen compared with animals treated with oxygen only had a significant reduction in the subscores of blood vessel tufts, extra retinal neovascularization, and blood vessel tortuosity (p < 0.001) as shown in Table 2. Figure 3 shows retinal whole mounts from the various groups. Animals treated with dexamethasone, compared with control group, did not show any difference in the total retinal scores or subscores (Fig. 1, Table 2), hence dexamethasone does not have an effect on the normal retinal development as measured by the retinopathy scoring system.
Retinal whole mounts from various treatment groups. Note the decrease in severity of OIR, as measured by decrease in the number of tufts, severity of extra retinal neovascularization, and blood vessel tortuosity, in the animals treated with dexamethasone and oxygen (B) compared with oxygen treated animals (A). (A) Hyperoxia group: Retina from oxygen treated animal shows an abundance of blood vessel tufts, extraretinal neovascularization, central loss of blood vessels or vasoconstriction, and severe blood vessel tortuosity. (B) Oxygen and dexamethasone group: Retina from oxygen and dexamethasone treated animal, compared with (A) shows significant reduction in the number of vascular tufts, extra retinal neovascularization, and blood vessel tortuosity. (C) Control group: The vessels have a fine pattern throughout. Note the absence of blood vessel tufts, extra retinal neovascularization, central vasoconstriction, and blood vessel tortuosity.
Retinal sections. To corroborate on the finding of extra-retinal neovascularization on flat retinal mounts, retinal sections were performed(30). Control and dexamethasone only group had an average of 3.1 ± 1.1 and 4.4 ± 2.7 (average ± SD) nuclei per section, respectively (p = 0.3). Oxygen compared with oxygen and dexamethasone treated animals had an average of 43.4 ± 13.1 and 27.3 ± 17.1 neovascular nuclei per section, respectively (p = 0.04), as shown in Figure 4.
Effect of dexamethasone on neovascular nuclei. Oxygen treated animals had 43.4 ± 13 (mean ± SD) nuclei extending beyond the inner limiting membrane. Oxygen and dexamethasone treated animals had 27.3 ± 17 nuclei (p = 0.04). There is no difference between control and dexamethasone treated animals (p = 0.3). Oxygen treatment appears as (○) and control treatment as (·).
Animal growth and death. Animal weight and death was monitored to assess the effect of 5 d of oxygen and dexamethasone exposure on animal health. Weights were recorded on PN7, PN12, and PN17-20. Animals exposed to dexamethasone had a slower rate of growth while exposed to the drug (Table 3). This finding was previously described in literature(13,15–16,25,34–36). After discontinuation of the drug on PN12, growth in the dexamethasone treated animals was similar to the control animals as assessed by average weight gain per day from PN12 until the day the animals were killed. Animals still had statistically lower weights on PN17-20. There were no deaths in the control group and one death in each of the other groups of animals. The deaths were excluded from the weight analysis.
DISCUSSION
The results demonstrate a clear beneficial effect of dexamethasone, when given concurrently with oxygen exposure, on OIR in the mouse. There was a significant reduction in the total retinopathy scores in the dexamethasone and oxygen treated animals when compared with oxygen treated animals. The specific subscore categories showing improvement were blood vessels tufts, extra retinal neovascularization, and blood vessel tortuosity. Dexamethasone and oxygen treated animals have a significantly lower number of neovascular nuclei on PAS-stained retinal sections when compared with animals treated with oxygen only. Although a beneficial effect was observed in the development of retinopathy in the mice, dexamethasone did cause growth impairment.
The mouse model of OIR is not a true representation of human ROP. Hyperoxic injury followed by retinal hypoxia produces an aggressive retinopathy in the mouse. Human ROP is characterized by an initial delay in vascular development and vasoconstriction/vaso-obliteration with subsequent hypoxia-driven retinal neovascularization. The dexamethasone used in these mice pups was given during the exposure to 75% oxygen and retinopathy was evaluated at the peak of vasoproliferation (PN17-20). Seventy-five percent oxygen is not routinely clinically used; the lowest amount of supplemental oxygen (if any) to maintain arterial oxygen tension in a normal range is used for premature infants. In addition, mice have retinal vasculature that normally matures ex utero at term; human infants do not. Premature infants have retinal vasculature that must mature in a developmentally abnormal (ex utero as opposed to in utero) environment where arterial oxygen tensions are higher than in utero. ROP is characterized by neovascularization at the developing vessel front. Mice develop retinal neovascular blood vessel tufts at the end of the area of central vasoconstriction. This model has been used to study down-regulation of vascular endothelial growth factor by hyperoxia(37) and modulation of vasoconstriction with calcium channel blockade(32), both of which target the injury produced in this model by 75% oxygen exposure for 5 d. The mouse model has been used extensively to study retinal neovascularization, which occurs after room air recovery of the animals(38–43). Injury and healing occur in both the mouse model of OIR and ROP, but there are species differences.
Although the precise mechanism by which dexamethasone exerts its protective effect is unknown, we speculate that the protective effect may by mediated, at least in part, by reduction in inflammation and/or injury caused by 75% oxygen exposure. Oxygen promotes synthesis and secretion of TNF(44–47). TNF is a macrophage, monocyte, or endothelial cell-derived proinflammatory polypeptide cytokine(48). Jensen(47) showed that the lungs of mice exposed to high-dose oxygen (greater than 95%) for 3 d demonstrated an increased expression of the gene for TNF. Daily treatment of these animals with anti-TNF antibodies improved their survival. These findings suggest that oxygen exposure induces TNF, which explains part of the toxicity of oxygen. O'Brien-Lander(45) showed that hyperoxia exposure enhances TNF production by posttranscriptional mechanism in LPS-stimulated human alveolar macrophages. Many investigators have documented that dexamethasone inhibits TNF production(49–53). Joyce(49) showed that dexamethasone suppresses both spontaneous and LPS-stimulated release of soluble forms of receptors for TNF from monocytes and suppresses the release of bioactive TNF from peripheral blood mononuclear cells. Brenner(50) used astrocytes derived from fetal rat brain and triggered by mycoplasmas to produce TNF. Preincubation of these cells with dexamethasone markedly inhibited the secretion of TNF. Waage(51) demonstrated that the production of TNF by LPS-stimulated human monocytes was significantly inhibited in a time and a dose-dependent fashion by dexamethasone.
TNF is found in the retina(54–57) and has been implicated in proliferative vitreoretinopathy(56,57). Modulation of TNF by dexamethasone may explain the improvement in retinopathy observed in the mouse model. Dexamethasone may inhibit inflammation via a TNF mediated macrophage infiltration thus protecting fragile capillaries from injury during the hyperoxic exposure.
Intravitreal administration of steroids has been shown to inhibit preretinal neovascularization in a pig model(58) and subretinal neovascularization in a primate model(59). The mechanism of inhibition of blood vessel proliferation is unclear, but is postulated that steroids have anti-inflammatory properties. Inhibition of macrophage infiltration to an area of injury has been proposed as a protective mechanism of action(58,59).
Dexamethasone may stabilize retinal capillary endothelial cells making them less susceptible to the injurious effects of 75% oxygen in the mouse model. Dexamethasone has been shown to stabilize human umbilical vein endothelium(60). Perhaps the dexamethasone treated animals are protected from the injury of the 75% oxygen more than their control counter-parts.
Timing of dexamethasone dosing may be critically important as pointed out by Ehrenkrantz(24). Dexamethasone administered to infants earlier (median d 23 versus 38) for pulmonary indications showed significantly lower rates of cryosurgery(21). The timing of the dexamethasone used in our experiments was most likely equivalent to early postnatal dexamethasone exposure. The developmental stage of the blood vessels in the newborn mouse retina approximates 4 to 5 mo gestation in the preterm infant(61). Antenatal corticosteroids have recently been shown to protect against the development of severe ROP(27–29). It has been speculated that antenatal corticosteroids may accelerate the maturation of the retinal vasculature, thus placing the infant at lower risk of developing serious ROP(29). The steroids may decrease the response of the developing blood vessels to the injurious extra uterine environment perhaps through TNF-mediated mechanisms. Dexamethasone in the mice may protect the retinal vasculature by an unknown or undescribed mechanism rendering by an unknown or undescribed mechanism rendering them less susceptible to retinal neovascularization when removed from 75% oxygen on d 12 of the experiment. The dexamethasone used in these animal experiments may be acting by a similar mechanism that renders antenatal steroids protective.
In conclusion, the retinopathy scoring system and quantification of neovascular nuclei on retinal sections show a beneficial effect of dexamethasone on OIR. Further studies are needed to establish the exact mechanism of action by which dexamethasone exerts its protective effect and to establish the best timing for dexamethasone exposure.
Abbreviations
- ROP:
-
retinopathy of prematurity
- OIR:
-
oxygen-induced retinopathy
- PAS:
-
periodic acid-Schiff
- CLD:
-
chronic lung disease
- PN:
-
postnatal
References
Terry TL 1942 Extreme prematurity and fibroplastic overgrowth of persistent sheath behind each crystalline lens. Am J Ophthalmol 25: 203–204
Casey Eye Institute 1996 Multicenter trial of cryotherapy for retinopathy of prematurity: snellen visual acuity and structural outcome at 5:1/2 years after randomization. Arch Ophthalmol 114: 417–424
Gilbert C, Rahi J, Eckstein M, O'Sullivan J, Foster A 1997 Retinopathy of prematurity in middle-income countries. Lancet 350: 12–14
Kennedy J, Todd DA, Watts J, John E 1997 Retinopathy of prematurity in infants less than 29 weeks gestation: 3½ years pre- and postsurfactant. J Pediatr Ophthalmol Strabismus 34: 289–292
Cryotherapy for retinopathy of prematurity cooperative group 1988 Multicenter trial of cryotherapy for retinopathy of prematurity: preliminary results. Arch Ophthalmol 106: 471–479
McNamara JA, Tasman W, Brown GC, Federman JL 1991 Laser photocoagulation for stage 3+ retinopathy of prematurity. Ophthalmology 98: 576–580
Preslan MW 1993 Laser therapy for retinopathy of prematurity. J Pediatr Ophthalmol Strabismus 30: 80–83
Landers MB, Toth CA, Semple HC, Morse LS 1992 Treatment of retinopathy of prematurity with argon laser photocoagulation. Arch Ophthalmol 110: 44–47
Cummings JJ, D'Eugenio DB, Gross SJ 1989 A controlled trial of dexamethasone in preterm infants at high risk for bronchopulmonary dysplasia. N Engl J Med 320: 1505–1510
Collaborative dexamethasone trial group 1991 Dexamethasone therapy in neonatal chronic lung disease: an international placebo-controlled trial. Pediatrics 88: 421–427
Durand M, Sardesai S, McEvoy C 1995 Effects of early dexamethasone therapy on pulmonary mechanics and chronic lung disease in very low birth weight infants: a randomized, controlled trial. Pediatrics 95: 584–590
Avery GB, Fletcher AB, Kaplan M, Brudno DS 1985 Controlled trial of dexamethasone in respiratory-dependent infants with bronchopulmonary dysplasia. Pediatrics 75: 106–111
Harkavy KL, Scanlon JW, Chowdhry PK, Grylack LJ 1989 Dexamethasone therapy for chronic lung disease in ventilator and oxygen-dependent infants: a controlled trial. J Pediatr. 115: 979–983
Kazzi NJ, Brans YW, Poland RL 1990 Dexamethasone effects on the hospital course of infants with bronchopulmonary dysplasia who are dependent on artificial ventilation. Pediatrics 86: 722–727
Yeh TF, Torre JF, Rastogi A, Anyebuno MA, Pildes RS 1990 Early postnatal dexamethasone therapy in premature infants with severe respiratory distress syndrome: a double-blind, controlled study. J Pediatr 117: 273–282
Papile LA, Tyson JE, Stoll BJ, Wright LL, Donovan EF, Bauer CR, Krause-Steinrauf H, Verter J, Korones SB, Lemons JA, Fanaroff AA, Stevenson DK 1998 A multicenter trial of two dexamethasone regiments in ventilator-dependent premature infants. N Engl J Med 338: 1112–1118
La Motte W, Tyner GS, Scheie HG 1952 Treatment of retrolental fibroplasia with vitamin E, Corticotropin (ACTH), and cortisone. Arch Ophthalmol 47: 556–569
Batton DG, Roberts C, Trese M, Maisels J 1992 Severe retinopathy of prematurity and steroid exposure. Pediatrics 90: 534–536
Reese AB, Blodi FC, Locke KC, Silverman WA, Day RL 1952 Results of use of corticotropin (ACTH) in treatment of retrolental fibroplasia. Arch Ophthalmol 47: 551–555
Ramanathan R, Siassi B, deLemos RA 1995 Severe retinopathy of prematurity in extremely low birth weight infants after short-term dexamethasone therapy. J Perinatol 15: 178–182
Sobel DB, Philip AG 1992 Prolonged dexamethasone therapy reduces the incidence of cryotherapy for retinopathy of prematurity in infants less then 1 kilogram birth weight with bronchopulmonary dysplasia. Pediatrics 90: 529–533
Todd DA, Kennedy J, Roberts S, Watts J, Psaila K, John E 1994 Retinopathy of prematurity in infants less than 29 wk' gestation at birth. Aust N Z J Ophthalmol 22: 19–23
Wright K, Wright SP 1994 Lack of association of glucocorticoid therapy and retinopathy of prematurity. Arch Pediatr Adolesc Med 148: 848–852
Ehrenkrantz R 1992 Steroids, chronic lung disease, and retinopathy of prematurity. Pediatrics 90: 647–648
Rastogi A, Akintorin SM, Bez ML, Morales P, Pildes R 1996 A controlled trial of dexamethasone to prevent bronchopulmonary dysplasia in surfactant-treated infants. Pediatrics 98: 204–210
Valkova Z 1986 Administration of corticoids in the treatment of retinopathy of prematurity. Cesk Oftalmol 42: 267–269
Kennedy JE, Todd DA, John E 1997 Premature birth and retinopathy of prematurity. In: Reibaldi A, Di Pietro M, Scuderi, Malerba E (eds) Progress in Retinopathy of Prematurity. Kugler Publications, Amsterdam, pp 25–29
The Italian ROP study group. 1997 ROP study group 1997 Italian multicenter study on retinopathy of prematurity: the Italian ROP study group. Eur J Pediatr 156: 939–943
Higgins RD, Mendelsohn AL, DeFeo MJ, Ucsel R, Hendricks-Munoz KD 1998 Antenatal dexamethasone and decreased severity of retinopathy of prematurity. Arch Ophthalmol 116: 601–605
Smith LEH, Wesolowski E, McLellan A, Kostyk SK, D'Amato R, Sullivan R, D'Amore PA 1994 Oxygen-Induced retinopathy in the mouse. Invest Ophthalmol Vis Sci 35: 101–111
D'Amato R, Wesolowski E, Smith LEH 1993 Microscopic visualization of the retina by angiography with high molecular weight fluorescein labeled dextrans in the mouse. Microvasc Res 46: 135–142
Higgins RD, Yu K, Sanders RJ, Nandgaonkar BN, Rotschild T, Rifkin DB 1999 Diltiazem reduces retinal neovascularization in a mouse model of oxygen induced retinopathy. Curr Eye Res 18: 20–27
Bancroft JD, Cook HC, Sterling RW, Turner DP 1994 Manual of Histological Techniques and Their Diagnostic Application. Churchill Livingstone, Edinburgh, pp 134–136
Yeh TF, Lin YJ, Huang CC, Chen YJ, Lin CH, Lin HC, Hsieh WS, Lien YJ 1998 Early dexamethasone therapy in preterm infants: a follow-up study. Pediatrics 101( 5): E7
Gregoire MC, Lefebvre F, Glorieux J 1998 Health and development outcomes at 18 months in very preterm infants with bronchopulmonary dysplasia. Pediatrics 101: 856–860
Barks JDE, Post M, Tuor UI 1991 Dexamethasone prevents hypoxic-ischemic brain damage in the neonatal rat. Pediatr Res 29: 558–563
Pierce EA, Foley ED, Smith LEH 1996 Regulation of vascular endothelial growth factor by oxygen in a model of retinopathy of prematurity. Arch Ophthalmol 114: 1219–1228
Pierce EA, Avery RL, Foley ED, Aiello LP, Smith LEH 1995 Vascular endothelial growth factor/vascular permeability factor expression in a mouse model of retinal neovascularization. Proc Natl Acad Sci USA 92: 905–909
Aiello LP, Pierce EA, Foley ED, Takagi H, Chen H, Riddle L, Ferrara N, King GL, Smith LE 1995 Suppression of retinal neovascularization in vivo by inhibition of vascular endothelial growth factor (VEGF) using soluble VEGF- receptor chimeric proteins. Proc Natl Acad Sci USA 92: 1045–1061
Robinson GS, Pierce EA, Rook SL, Foley E, Webb R, Smith LE 1996 Oligodeoxynucleotides inhibit retinal neovascularization in a murine model of proliferative retinopathy. Proc Natl Acad Sci USA 93: 4851–4856
Hammes HP, Brown Lee M, Jonczyk A, Sutter A, Preissner KT 1996 Subcutaneous injection of a cyclic peptide antagonist of vitronectin receptor-type integrins inhibits retinal neovascularization. Nat Med 2: 529–533
Smith LEH, Kopchick JJ, Chen W, Knapp J, Kinose F, Daley D, Foley E, Smith RG, Schaeffer JM 1997 Essential role of growth hormone in ischemia-induced retinal neovascularization. Science 276: 1706–1709
Suzuma K, Takagi H, Otani A, Suzuma I, Honda Y 1998 Increased expression of KDR/Flk-1 (VEGFR-2) in murine model of ischemia-induced retinal neovascularization. Microvasc Res 56: 183–191
Lahat N, Bitterman H, Yaniv N, Kinarty A, Bitterman N 1995 Exposure to hyperbaric oxygen induces tumor necrosis factor-alpha (TNF-alpha) secretion from rat macrophages. Clin Exp Immunol 102: 655–659
O'Brien-Lander AR, Nelson ME, Cowley BD Jr, Bailey K, Wesselius LJ 1995 Hyperoxia amplifies TNF-alpha production in LPS-stimulated human alveolar macrophages. Am J Respir Cell Mol Biol 12: 275–279
Shea LM, Beehler C, Schwartz M, Shenkar R, Tuder R, Abraham E 1996 Hyperoxia activates TNF - Kappa B and increases TNF-alpha and IFN-gamma gene expression in mouse pulmonary lymphocytes. J Immunol 157: 3902–3908
Jensen JC, Pogrebnic HW, Pass HI, Buresh C, Merino MJ, Kauffman D, Venzon D, Langstein HN, Norton JA 1992 Role of tumor necrosis factor in oxygen toxicity. J Appl Physiol 72: 1902–1907
Yoshida S, Ono M, Shono T, Izumi H, Ishibashi T, Suzuki H, Kuwano M 1997 Involvement of interleukin-8, vascular endothelial growth factor, and basic fibroblast growth factor in tumor necrosis factor alpha-dependent angiogenesis. Mol Cell Biol 17: 4015–4023
Joyce DA, Kloda A, Steer JH 1997 Dexamethasone suppresses release of soluble TNF receptors by human monocytes concurrently with TNF-alpha suppression. Immunol Cell Biol 75: 345–350
Brenner T, Yamin A, Abramsky O, Gallily R 1993 Stimulation of tumor necrosis factor- alpha production by mycoplasmas and inhibition by dexamethasone in cultured astrocytes. Brain Res 608: 273–279
Waage A, Bakke O 1988 Glucocorticoids suppress the production of tumor necrosis factor by lipopolysaccharide-stimulated human monocytes. Immunology 63: 299–302
Brattsand R, Linden M 1996 Cytokine modulation by glucocorticoids: mechanisms and actions in cellular studies. Aliment Pharmacol Ther 1 Suppl 2: 81–90
Pan M, Wasa M, Ruan U, Souda W 1996 Lipopolysaccharide and tumor necrosis factor stimulate lung microvascular arginine uptake, a response attenuated by dexamethasone. JPEN J Parenter Enteral Nutr 20: 50–55
La Vail MM, Unoki K, Yasumura D, Matthes MT, Yancopoulos GD, Steinberg RH 1992 Multiple growth factors, cytokines, and neurotrophins rescue photoreceptors from the damaging effects of constant light. Proc Natl Acad Sci USA 89: 11249–11253
Behar-Cohen FF, Parel JM, Pouliquen Y, Thillaye-Goldenberg B, Goureau O, Heydolph S, Courtois Y, De Kozak Y 1997 Iontophoresis of dexamethasone in the treatment of endotoxin-induced-uveitis in rats. Exp Eye Res 65: 533–554
Limb GA, Alam A, Earley O, Green W, Chignell AH, Dumonde DC 1994 Distribution of cytokine proteins within epiretinal membranes in proliferative vitreoretinopathy. Curr Eye Res 13: 791–798
Limb GA, Chignell AH, Green W, LeRoy F, Dumonde DC 1996 Distribution of TNF alpha and its reactive vascular adhesion molecules in fibrovascular membranes of proliferative diabetic retinopathy. Br J Ophthalmol 80: 168–173
Danis RP, Bingaman DP, Yang Y, Ladd B 1996 Inhibition of preretinal and optic nerve head neovascularization in pigs by intravitreal triamcinolone acetonide. Ophthalmology 103: 2099–2104
Ishibashi T, Miki K, Sorgente N, Patterson R, Ryan SJ 1985 Effects of intravitreal administration of steroids on experimental subretinal neovascularization in the subhuman primate. Arch Ophthalmol 103: 708–711
Jarvelainen H, Pelliniemi TT, Ronnemaa T 1985 The stabilizing effect of glucocorticoids on human endothelial cells in culture. Scand J Clin Lab Invest 45: 223–228
Gyllenstein LJ, Hellstrom BE 1955 Experimental approach to the pathogenesis of retrolental fibroplasia: II. the influence of the developmental maturity in oxygen-induced changes in the mouse eye. Am J Pathol 39: 475–488
Author information
Authors and Affiliations
Additional information
Supported in part by National Institutes of Health Grants EY00330 (RDH) and Fight For Sight, Research Division of Prevent Blindness America (RDH).
Rights and permissions
About this article
Cite this article
Rotschild, T., Nandgaonkar, B., Yu, K. et al. Dexamethasone Reduces Oxygen Induced Retinopathy in a Mouse Model. Pediatr Res 46, 94–100 (1999). https://doi.org/10.1203/00006450-199907000-00016
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199907000-00016
This article is cited by
-
Oxygen-induced retinopathy: a model for vascular pathology in the retina
Eye (2010)
-
Treatment of Retinopathy of Prematurity with topical ketorolac tromethamine: a preliminary study
BMC Pediatrics (2004)
-
Effect of Dexamethasone Therapy on Serum Vitamin E Concentrations in Premature Infants with Bronchopulmonary Dysplasia
Journal of Perinatology (2003)