Abstract
This study was designed to determine the effects of a membrane permeant phosphodiesterase-resistant analog of cGMP on lung liquid production and pulmonary blood flow at the time of birth. Experiments were performed on seven fetal sheep prepared for chronic measurements of lung liquid production (Jv), pulmonary blood flow (Qp) and pressure, as well as systemic pressure. Injection of either 8-bromo-cGMP or saline were made via a catheter inserted in the left pulmonary artery. Experiments consisted of 1 h of control, 1 h of infusion, and 2 h of recovery. Data were analyzed by ANOVA and Newman-Keuls test. After infusion of 8-bromo-cGMP, Jv was decreased by 70 and 44% from control in h 3 and 4, respectively. Qp was elevated by 100 mL/min in h 2 and 3 and continued to be elevated by 50 mL/min in h 4. Saline infused animals showed no significant changes in Qp and Jv. This study demonstrates that 8-bromo-cGMP decreases lung liquid production and increases pulmonary blood flow in near term fetal sheep. Although blood flow increased in h 2, lung liquid production did not decrease at this time, suggesting a time dissociation between changes in pulmonary blood flow and lung liquid production. Thus, it is possible that a common transduction pathway involving cGMP may be responsible for lung liquid reduction and elevation of pulmonary blood flow at birth. However, Qp and Jv may not be causally related.
Similar content being viewed by others
Main
Fetal lungs normally produce large volumes of fluid (≈4.5 mL/h per kg of body weight) which are important for proper lung growth and development(1–3). It is essential, however, that this fluid production is terminated and the lungs cleared of fluid at birth. Reabsorption of lung liquid is concurrent with circulatory adjustments occurring at birth in the transformation of the mammalian fetus to a newborn. These changes include a decrease in PVR, with a 4-5-fold increase in pulmonary blood flow, constriction of the umbilical vessels, and closure of the ductus arteriosus(4).
The adaptations occurring at birth have been attributed to a variety of endogenous and exogenous factors. Investigators have shown that epinephrine(5) and vasopressin in the presence of cortisol and thyroid hormones decrease lung liquid production or actually cause reabsorption of the fluid(6). Additionally, EDRF-NO as well as ventilation and eicosanoids were found to play an important role in the alteration of the fetal circulation from a high PVR with low flow to a low resistance with high flow(7–9).
The exact mechanisms responsible for these physiologic alterations in fetal lung physiology at the time of birth are not completely understood. Evidence has been presented that the reabsorption of lung liquid at birth is caused by the β adrenergic stimulation of epinephrine, which by conventional understanding, would elevate cAMP production. The latter in turn has been shown to activate pulmonary epithelial Na+ channels(6, 10, 11). In addition, several vasoactive substances including acetylcholine, bradykinin, and PGD2 have been shown simultaneously to decrease lung liquid production(12) and increase pulmonary blood flow in fetal sheep close to term(13, 14). PGD2 behaves like epinephrine in that it stimulates production of cAMP, which not only affects sodium channels, but is also a potent vasodilator(15). Acetylcholine and bradykinin stimulate production of NO, which in turn elevates smooth muscle cGMP, another cyclic nucleotide that is also a vasodilator(13, 15, 16). Recent studies using two isolated cell lines, Calu-3 and CFT43, as models of normal and cystic fibrosis airway epithelial cells, respectively, have provided evidence that 8-bromo-cGMP can mediate changes in chloride permeability(17). Also, studies by Geary et al.(18) have suggested that there are similar mechanisms in cultured human airway epithelial cells to synthesize and export cGMP and cAMP. Studies have shown interaction and similarities in action between cAMP and cGMP(19, 20). Thus, both intracellular messengers(cAMP and cGMP) may be important in mediating changes occurring in fetal lungs at birth.
Because cAMP is an important mediator in the process of lung liquid reabsorption as well as pulmonary vasodilation(12, 15, 21, 22), we decided to study the effects of cGMP on lung liquid production and pulmonary blood flow in near term fetal lambs. The specific aim of our study is to determine whether the increase in pulmonary blood flow and lung liquid reabsorption occurring at birth are caused by a common transduction mechanism(s) that may involve elevation of the intracellular messenger cGMP. This could occur as a result of elevation of EDRF-NO at the time of birth. Thus, we studied the effects of a cGMP analog (8-bromo-cGMP) on lung liquid production and pulmonary blood flow in seven fetal lambs at 129-140 d of gestation.
METHODS
Surgical procedure for chronic animal preparation. The following procedures were approved by the University of Florida Animal Research Committee, Gainesville, FL. Pregnant ewes (n = 7) carrying fetuses 128-140 d of gestation, with a mean gestational age of 133 ± 1.1 d (term is 145-148 d), were premedicated with ketamine (12 mg/kg) followed by endotracheal intubation and general anesthesia with halothane (1.5-2.0%) in 95% oxygen. Using aseptic surgical techniques described previously(16, 23, 24), a small portion of the uterus was carefully delivered through a midline abdominal wall incision. Via a small incision in the uterine wall, the fetal head and left forearm were delivered. Through a small incision in the fetal neck, polyvinyl cannulas were placed in the fetal carotid artery and jugular vein. In addition, the fetal trachea was exposed, and a loop of saline-filled silicone tubing (length, 230 cm; inside diameter, 0.264 cm; volume, 15.0 mL) was inserted 3 cm below the larynx into the central and distal ends of the cut trachea and tied in place. To monitor amniotic fluid pressure, a catheter with multiple luminal holes at the end was sewn to the fetal skin. An incision between ribs 4 and 5 of the fetus allowed access to the left pulmonary artery and left atrium. After opening the pericardium, the left pulmonary artery was isolated, and a Transonic flow probe (4-6 mm) was placed around it and secured in place with ligatures. Catheters were inserted directly into the left pulmonary artery, main pulmonary artery, and left atrium. The catheters were secured by purse-string sutures. The fetal chest wall was then closed, and catheters were stitched to the skin. All vascular catheters were filled with heparin (1000 IU/mL), and the ends were sealed with tightly fitting brads. The amniotic fluid and lung liquid circuit catheters were filled with saline. The amniotic membranes and uterine wall were sutured to prevent fluid loss; the uterine wall was then imbricated. All catheters were tunneled under the maternal skin to exit via a lateral abdominal incision for insertion into a cloth pouch attached to the maternal flank. The maternal midline abdominal incision was closed with sutures and the skin incision with stainless steel wound clips. Beginning the day before surgery, ampicillin (15 mg/kg) and gentamicin (2-4 mg/kg) were given to the mother intramuscularly and for the next 4 d after surgery. The abdominal incision and the amniotic fluid received a total of 600 mg of Polyflex (Bristol) at surgery. Ewes were allowed no less than 4 d to recover from surgery before experiments were carried out. When multiple experiments were carried out, ewes were allowed 2 d to recover from prior procedures.
Protocol. Two procedures were performed in these studies:1) 8-bromo-cGMP infusion for 1 h and 2) saline infusion for controls. One hour of impermeant tracer mixing and equilibration was carried out at the start of each experiment. Then in each study 1 h of control lung liquid production was followed by administration, in random order, of either saline or the cGMP analog for 1 h during which lung liquid was mixed and samples were collected every 10 min. Lung liquid samples were collected for an additional 2 h for estimation of lung liquid production. We performed total of 14 experiments; 6 of them were control saline infusion.
Mean fetal heart rate, left pulmonary arterial blood flow, and systemic arterial pressure, referenced to amniotic pressure, were monitored throughout the experiment with a Gould recorder using a Keithly analog to digital converter and an IBM computer. Blood gases and pH, corrected for normal ovine body temperature (39 °C), were measured in the middle of each hour of each experiment using a Corning blood gas analyzer model 288. Data for otherwise“normal” fetal sheep were not accepted if pH < 7.30; Po2< 16 mm Hg or Pco2 > 55 mm Hg. Maternal blood pressure and heart rate were monitored continuously, whereas blood gases and pH were measured every hour throughout the experimental protocol.
Drug preparation. 8-Bromo-cGMP (Sigma Chemical Co. St. Louis, MO) was prepared by dissolving (3-5 mg/mL) in saline. The compound was given by continuous infusion over 1 h into the left pulmonary artery at 0.3-0.5 mg/min.
Measurements of lung liquid secretion rate. Measurements of rates of lung liquid production were based on the dye dilution techniques of Normand et al.(25) and Olver et al.(26). Similar methods(15, 19) have been reported in detail by Cassin and co-workers previously(23, 27). During experiments, the oral side of the tracheal tubing was clamped to permit lung liquid to drain by gravity into a warmed 100-mL reservoir, which was open to air via a bacterial filter. The fluid contents of the reservoir were maintained at 39 °C by applying an adjustable heating pad around the reservoir. This technique allows withdrawal of fluid directly from the lungs for mixing and sampling. Secretion rates were calculated from the rate of dilution of an impermeant tracer blue dye dextran(molecular mass 2 000 000 Da) mixed in the lung liquid. In prior experiments in which we used both 125I and blue dye dextran, identical results were obtained with the two tracers(6, 23). Samples of lung liquid (0.5 mL) were taken every 10 min after the addition of 10 mL of blue dye (50 mg/mL) to fluid in the reservoir. Mixing of the dye with lung liquid was carried out by repeatedly withdrawing liquid into the reservoir and returning it between samples. The decline in concentration of dye in consecutive samples, which were used to estimate the rate of lung liquid secretion, was measured with a Beckman DU-50 spectrophotometer at 620 nm.
Quantitation of results. Rates of lung liquid production were calculated from the slopes of regression lines of 1-h periods from plots of total fluid volume versus time (method of least squares)(23, 27). Differences between rates of liquid production were analyzed by repeated measures one-way ANOVA and Newman-Keuls test(28). Because production must involve bidirection movement of ions and fluid, positive slopes of volume on time were taken to indicate net secretion, whereas negative slopes indicate net reabsorption. In this report we have used the terms secretion and reabsorption to describe net processes. In all experiments, appropriate sequential adjustments were made for gain or loss of fluid due to removal of samples or addition of drugs. All data are presented as means ± SEM. p values of <0.05 are accepted as significant.
RESULTS
All fetuses and ewes were in apparent good health at the time of study. There were no significant differences between values of fetal blood gases and pH at the beginning and the end of the experiment. Average fetal pH, Po2, and Pco2 in the saline control group were pH 7.36 ± 0.01, 25 ± 1 mm Hg, and 50 ± 2 mm Hg, respectively. In the cGMP group the average pH, Po2, and Pco2 values were pH 7.35 ± 0.01, 23 ± 1 mm Hg, and 51 ± 2 mm Hg, respectively.
Lung liquid production in saline control group. In six fetal sheep, infusion of isotonic saline at a rate equivalent to the rate of infusion of 8-bromo-cGMP did not result in significant changes in lung liquid production rate over 4 h (Fig. 1A). Fetuses varied in age from 129 to 140 d gestation, and had a mean body weight of 3.52 ± 0.28 kg. The average secretion rate in the control animals for 4 h was 13.6± 1.7 mL/h.
Lung liquid production in 8-bromo-cGMP-infused group. The infusion of 8-bromo-cGMP at a rate of 0.3-0.5 mg/min in eight fetal sheep(129-140 d of age) consistently reduced the lung liquid secretion rate significantly from an average value of 13.4 ± 1.4 mL/h in h 1 and 2, to an average value of 4.3 ± 2.2 and 7.9 ± 1.4 mL/h in h 3 and 4, respectively. The change in secretion rate was statistically significant when compared with the saline control group (p < 0.05). The lung liquid secretion in the 3rd and 4th h was decreased by 70 and 44%, respectively, from that in the control period (Fig. 1B).Table 1 provides a summary of data on lung liquid secretion rates in the saline control group and the cGMP-infused group.
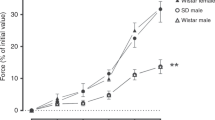
Pulmonary blood flow in saline control group. Infusion of saline in the control group causes no significant change in pulmonary blood flow. Average mean pulmonary blood flow during 4 h was 53 ± 5 mL/min (Fig. 2A).
Pulmonary blood flow in 8-bromo-cGMP-infused group. Pulmonary blood flow averaged 56 ± 2 mL/min during the control hour. After the cGMP analog infusion, flow increased to 167 ± 20 and 187 ± 22 mL/min in h 2 and 3, respectively (approximately by 2.5-fold). The flow returned slowly toward preinfusion rate during the 4th h, although it was still elevated (117 ± 21 mL/min) by approximately two times above the control rate. The difference in the mean pulmonary blood flow between the treatment and the control group was significant (p < 0.05) during h 2, 3, and 4 (Fig. 2B). Table 1 provides a summary of data on fetal pulmonary blood flow in saline control group and cGMP-infused group.
Fetal heart rate and systemic blood pressure. Infusion of 8-bromo-cGMP did not cause significant changes in mean systemic blood pressure. However, fetal heart rates increased significantly during h 2 and continued to be elevated during h 3 and 4 after infusion (p < 0.05). Significant changes in fetal heart rate or blood pressure were not observed in the control group. Table 2 provides a summary of data on fetal heart rate and systemic blood pressure in saline-infused group and cGMP analog group.
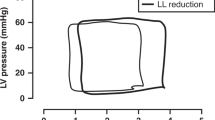
Fetal PAP and PVR. Infusion of 8-bromo-cGMP causes negligible changes in mean fetal PAP. Average fetal PVR {(PAP - left atrial pressure)/flow} decreased from 0.76 ± 0.08 (mm Hg·kg·min·mL-1) during the control hour to 0.29± 0.06, 0.23 ± 0.02, and 0.47 ± 0.09 in h 2, 3, and 4, respectively. Changes in fetal PVR during h 2, 3, and 4 were significantly different from the control h 1 (p < 0.05) (Fig. 3A).
Infusion of saline into left pulmonary artery of six fetal control sheep did not change PVR (A). After cGMP infusion(B), PVR decreased by approximately 60 and 70% during infusion and the following hour. The resistance returned slowly toward baseline in h 4; however, it was still below baseline (*p < 0.05).
No significant changes were noticed in PVR or PAP after saline infusion in the control group (Fig. 3B). Table 2 illustrates a summary of data collected on PVR and PAP in both the cGMP and saline control groups.
DISCUSSION
In this study, we have demonstrated that infusion of 8-bromo-cGMP increases pulmonary blood flow and decreases lung liquid production in near term fetal sheep. These alterations are essential in the transition of the fetus from a liquid-breathing to an air-breathing status. Exact mechanisms involved in rearrangement of fetal pulmonary circulation and lung liquid balance are still not clear. In the fetal state, lungs are fluid-filled, and gas exchange must occur via the placenta. Fetal pulmonary blood flow is low (35-50 mL·min-1·kg-1 of body weight)(29), and pulmonary vascular tone is high. At birth, many factors including gaseous expansion of the lungs, increase in Pao2, decrease in Pco2, and increase in arterial pH contribute to decreasing pulmonary vascular tone. These changes may stimulate synthesis and/or release of multiple vasoactive substances, including prostacyclin, PGE2, bradykinin, endothelin, and platelet activating factor(8, 29, 30). Investigators have shown that in the fetal state bradykinin, acetylcholine, and endothelin work, at least in part, to cause pulmonary vasodilation via the release of EDRF-NO(7, 8, 12, 23, 24, 31, 32). EDRF-NO in turn stimulates guanylate cyclase to produce cGMP, leading to vascular smooth muscle relaxation(33). Eicosanoids released by endothelial cells exert their effects via release of cAMP(15). The suggestion has been made that platelet-activating factor may release PGE2 which in turn could produce vasodilation via cAMP(34). Recently, studies have demonstrated that there are maturational changes in EDRF-NO production by ovine fetal pulmonary arteries(35).
In our study, infusion of 8-bromo-cGMP into the left pulmonary artery of near term fetal sheep increases pulmonary blood flow by 2.5-fold shortly after onset of infusion, and during the following hour. This flow diminished in h 4; but it was still above baseline. The increase in flow was associated with decreases in PVR without significant changes in PAP, and mimics the changes which occur normally in the fetal lung at the time of birth. Our findings support the hypothesis that EDRF-NO and cGMP have a role in modulating the PVR close to term. Lung liquid production decreased from the baseline value by approximately 70% and 45% in h 3 and 4, respectively, after cGMP infusion. Although increases in pulmonary blood flow occur during the 2nd h of cGMP infusion, a parallel decrease in lung liquid production rate was not observed. An approximately 1-h delay was noted between the change in Qp, which started in h 2, and the change in Jv, which started later in h 3. This dissociation in the effects of cGMP on pulmonary blood flow and lung liquid production rate during h 2 suggests that the two processes may be independent of each other. Recently, a great deal of interest has been directed at a possible link between the increase in pulmonary blood flow and lung liquid clearance at the time of birth. Studies with vasoactive agents (acetylcholine and PGE1) in near term fetal lambs have revealed a concurrent increase in pulmonary blood flow and decrease in lung liquid production(12). Our observation of the dissociation between the pulmonary blood flow and lung liquid production is not in accord with the hypothesis that the elevation in pulmonary blood flow causes a decrease in lung liquid production. However, the exact role of cGMP in preparing the fetal lung for alveolar gas ventilation is not completely clear. It appears that a variety of stimuli at birth elevate endogenous NO synthesis, which increases intracellular cGMP with a resultant increase in pulmonary blood flow and suppression of lung liquid production.
Acetylcholine, which stimulates NO synthase and increases endogenous NO production, has been shown to cause a concurrent increase in fetal pulmonary blood flow and decrease in lung liquid production(12). In our experiments cGMP infusion to near term fetal sheep diminished lung liquid production and dilated the pulmonary circulation. Although the changes we demonstrated in lung liquid production and pulmonary blood flow were not to the same extent normally seen at the time of birth, our results were comparable. Our observation strengthens the hypothesis that the pulmonary vasodilation and drying the lungs at the time of birth are caused, at least in part, by several birth-related stimuli that lead to elevation in EDRF-NO with subsequent increase in intracellular messenger cGMP.
The role of cyclic nucleotides in regulating fetal pulmonary blood flow and lung liquid production is not well understood. Investigators have shown that forskolin, 8-bromo-cAMP, and cAMP suppress lung liquid production(21, 36, 37). Furthermore, Gryglewski et al.(15) showed that cAMP has potent vasodilator effects. In these studies we showed that the effects of cGMP on lung liquid and pulmonary blood flow were similar to the effects of cAMP. Thus, it appears that both cyclic nucleotides may play a role in the regulation of fetal lung circulation and lung liquid clearance close to term.
It is not clear how EDRF-NO and cGMP suppress lung liquid production. There have been suggestions that elevation of cGMP may activate cGMP-dependent protein kinase and stimulate smooth muscle K+ channels, resulting in hyperpolarization and smooth muscle relaxation(38). It is also possible that cGMP-sensitive protein kinase may be involved in opening Na+ channels to allow reabsorption of alveolar fluid Na+ and water(39). Recently, interest has been directed toward the interaction and “cross activation” between cGMP and cAMP(40). cGMP-dependent protein kinase has been shown to mediate the effects of both cGMP as well as cAMP on aortic smooth muscle relaxation(41). Furthermore, Harrison et al.(42) identified a cAMP phosphodiesterase which in vitro can be inhibited by cGMP. This isoenzyme was found to play a significant role in pulmonary vascular tone regulation(43). It is also possible that cGMP causes lung liquid reabsorption by cross activation of cAMP via phosphodiesterase III inhibition(cGMP-inhibited cAMP phosphodiesterase)(43). This would certainly agree with the mechanism of epinephrine-induced lung liquid reabsorption via elevated cAMP as proposed by Olver et al.(10) and Strang(11).
It is also possible that the lung liquid production rate is diminished as a result of toxic effects of cGMP. However, we think this is unlikely, because measurements made of fetal blood pressures and blood gases and pH did not suggest stress of this nature. The elevation in heart rate could be due to release of epinephrine as a result of drug administration. Alternatively, the cardiac acceleration could be due to elevation of cAMP as a result of cGMP inhibition of phosphodiesterase. Fetal lung liquid production represents a balance between Cl- secretion and Na+ reabsorption from alveolar spaces. Thus, it is possible that the decrease in lung liquid production in these studies was due to an effect of cGMP in inhibiting Cl- transport into the lung lumen. As indicated previously, there are data to indicate that epithelial cells in vitro: 1) display mechanisms for synthesis and export of cAMP and cGMP, and 2) can mediate changes in chloride permeability in response to elevated cGMP(17, 18). However, because the above studies were carried out in vitro using cells from adult lung carcinoma and adult primary cultures of human airway, some caution is required in comparing these data with results obtained from intact unanesthetized fetal sheep in utero.
Although we considered the possibility that the increased reabsorption of lung fluid is caused by the increase in pulmonary blood flow, we do not think the hypothesis is tenable. Our studies have demonstrated a temporal dissociation between these two events. Also in preliminary studies, we have investigated the effects of nitrendipine on fetal pulmonary blood flow and lung liquid modulation. This dihydropyridine type Ca2+ channel blocker to our knowledge has no effect on cyclic nucleotides. Our preliminary studies demonstrated that nitrendipine infusion to near term fetal lambs (n= 3) causes a significant increase in pulmonary blood flow with no effect on lung liquid production rate. Furthermore, investigators have demonstrated lung liquid reabsorption in isolated nonperfused in vitro fetal lungs(21, 44). Their observations as well as ours are in agreement and are better explained by the theory that lung liquid reabsorption and pulmonary blood flow may be independent processes.
In summary, postnatal survival of the fetus depends on an appropriate balance between pulmonary blood flow and alveolar ventilation. There is a transition from a liquid breathing fetus to an air breathing newborn with a marked increase in pulmonary blood flow. EDRF-NO and cGMP play an important role in dilating the pulmonary circulation at birth and may also be involved in clearing liquid from the lungs at the same time. Both cGMP, as shown by these experiments, and cAMP as demonstrated previously appear to be important in changes of fetal lung physiology close to term.
Abbreviations
- Jv:
-
net lung liquid production
- Qp:
-
pulmonary blood flow
- EDRF:
-
endothelium-derived relaxing factor
- NO:
-
nitric oxide
- PVR:
-
pulmonary vascular resistance
- PAP:
-
pulmonary arterial pressure
- PG:
-
prostaglandin
References
Strang LB 1997 Neonatal Respiration. Blackwell Scientific, Oxford, UK, 20–46
Alcorn D, Adamson TA, Lambert TF, Maloney JM, Richie BC, Robinson PM 1997 Morphological effects of chronic tracheal ligation and drainage in the fetal lamb lung. J Anat 123: 649–660
Moessinger AC, Harding R, Adamson TM, Singh M, Ku GT 1990 Role of lung fluid volume in growth and maturation of the fetal sheep lung. J Clin Invest 86: 1270–1277
Cassin S, Dawes GS, Mott JC, Ross BB, Strang LB 1964 The vascular resistance of the foetal and newly ventilated lung of the lamb. J Physiol 171: 61–79
Walters DV, Olver RE 1978 The role of catecholamines in lung liquid absorption at birth. Pediatr Res 12: 239–242
Cassin S, Demarco V, Perks AM, Kuck H, Ellis TM 1994 Regulation of lung liquid secretion in immature fetal sheep: hormonal interaction. J Appl Physiol 77: 1445–1450
Abman SH, Chatfield BA, Hall SL, McMurthy IF 1990 Role of endothelium-derived relaxing factor during transition of pulmonary circulation at birth. Am J Physiol 259:H1921–H1927
Cassin S 1993 The role of eicosanoids and endothelium-dependent factors in regulation of the fetal pulmonary circulation. J Lipid Mediators 6: 477–485
Iwamoto HS, Teitel D, Rudolph AM 1987 Effects of birth-related events on blood flow distribution. Pediatr Res 22: 634–640
Olver RE, Ramsden CA, Strang LB, Walters DV 1986 The role of amiloride-blockable sodium transport in adrenaline-induced lung liquid reabsorption in the fetal lamb. J Physiol 376: 334–340
Strang L B 1991 Fetal lung liquid: secretion and reabsorption. Physiol Rev 71: 991–1016
Cummings JJ 1995 Pulmonary vasodilator drugs decrease lung liquid production in fetal sheep. J Appl Physiol 79: 1212–1218
Ignarro LJ, Harbison RG, Wood KC, Kadowitz PJ 1986 Activation of purified soluble guanylate cyclase by endothelium-derived relaxing factor from intrapulmonary artery and vein: stimulation by acetylcholine, bradykinin and arachidonic acid. J Pharmacol Exp Ther 237: 893–900
Ignarro LJ, Burke TM, Wood KS, Wolin MS, Kadowitz PJ 1984 Association between cyclic GMP accumulation and acetylcholine-elicited relaxation of bovine intrapulmonary artery. J Pharmacol Exp Ther 228: 682–690
Gryglewski RJ, Botting RM, Vane JR 1988 Mediators produced by the endothelial cell. Hypertension 12: 530–548
Griffith TM, Edwards DH, Lewis MJ, Henderson AH 1985 Evidence that cyclic GMP mediates endothelium-dependent relation. Eur J Pharmacol 112: 195–202
Kelley TJ, Al-Nakkash L, Drumm ML 1997 C-type natriuretic peptide increases chloride permeability in normal and cystic fibrosis airway cells. Am J Respir Cell Mol Biol 16: 464–470
Geary GA, Goy MF, Boucher RC 1993 Synthesis and vectorial export of cGMP in airway epithelium: expression of soluble and CNP specific guanylate cyclases. Am J Physiol 265:L598–L605
Jiang H, Colbran JL, Francis SH, Corbin JD 1992 Direct evidence for cross activation of cGMP-dependent protein kinase by cAMP in pig coronary arteries. J Biol Chem 267: 1015–1019
Jin JG, Murthy KS, Grider JR, Makhlouf GM 1993 Activation of distinct cAMP- and cGMP-dependent pathways by relaxant agents in isolated gastric muscle cells. Am J Physiol 264:G470–G477
Kindler PM, Ziabakhsh S, Perks AM 1992 Effect of cAMP, its analogues, and forskolin on lung liquid production by in vitro lung preparations from fetal guinea pits. Can J Physiol Pharmacol 70: 330–338
Cassin S, Dawes GS, Ross BB 1964 Pulmonary blood flow and vascular resistance in immature foetal lambs. J Physiol 171: 80–89
Davis TA, Gause G, Perks AM, Cassin S 1992 Effect of intravenous saline infusion on fetal ovine lung liquid secretion. Am J Physiol 262:R1117–R1120
Perks AM, Cassin S 1985 The rate of production of lung liquid in fetal goats and the effect of expansion of the lungs. J Dev Physiol 7: 149–160
Normand ICS, Olver RE, Reynolds EOR, Strang LB 1971 Permeability of lung capillaries and alveoli to non-electrolytes in foetal lamb. J Physiol 219: 303–320
Olver RE, Ramsden CA, Strang LB, Walters DV 1986 The role of amiloride blockable sodium transport in adrenaline-induced lung liquid reabsorption in the fetal lamb. J Physiol 376: 334–340
Cassin S, Perks AM 1982 Studies of factors which stimulate lung liquid secretion in fetal goats. J Dev Physiol 4: 311–325
Winer BJ 1971 Statistical Principles in Experimental design. McGraw-Hill, New York, pp 205–260
Heymann MA, Soifer JS 1989 Control of the fetal and neonatal pulmonary circulation. Lung Biol Health Dis 38: 33–50
Accurso FJ, Abman SH, Wilkoning RB, Worthen GS, Henson P 1991 Fetal pulmonary vasodilation after exogenous platelet-activating factor. J Appl Physiol 70: 778–787
Tiktinski MH, Cummings JJ, Morin FC 1992 Acetylcholine increases pulmonary blood flow in intact fetuses via endothelium-dependent vasodilation. Am J Physiol 262:H406–H410
Bellan JA, Minkes RK, McNamara DB 1991 Nω-Nitro-L-arginine selectively inhibits vasodilator responses to acetylcholine and bradykinin in cats. Am J Physiol 260:H1025–H1029
Zapol WM, Rimar S, Gillis N, Marletta M, Bosken C 1994 Nitric oxide and the lung. Am J Respir Crit Care Med 149: 1375–1380
Webber SE, Morikawa T, Widdicombe JG 1992 Platelet-activating factor relaxes ferret tracheal smooth muscle and reduces transepithelial potential differences in vitro. Br J Pharmacol 105: 223–229
Kinsella JP, MaQuerton JA, Rosenberg AA, Abman SA 1992 Hemodynamic effects of exogenous nitric oxide in ovine transitional pulmonary circulation. Am J Physiol 263:H875–H880
Barker PM, Brown MJ, Ramsden CA, Strang LB, Walters DV 1988 The effect of thyroidectomy in the fetal sheep on lung liquid reabsorption induced by adrenaline. J Physiol 407: 373–383
Walters DV, Ramsden CA, Olver RE 1990 Dibutyryl cAMP induces a gestation-dependent absorption of fetal lung liquid. J Appl Physiol 68: 2054–2059
Cook NS 1988 The pharmacology of potassium channels and their therapeutic potential. Trends Pharmacol Sci 9: 21–28
Archer SL, Huang JMC, Hampl V, Nelson DP, Schultz PJ 1994 Nitric oxide and cGMP cause vasorelaxation by activation of a charybdotoxin-sensitive K channel by cGMP dependent protein kinase. Proc Natl Acad Sci USA 91: 7583–7587
Smith JA, Francis SH, Walsh KA, Kumar S, Corbin JD 1996 Auto-phosphorylation of type Iβ cGMP-dependent protein kinase increases basal catalytic activity and enhances allosteric activation by cGMP or cAMP. J Biol Chem 271: 20756–20762
Komalavilas P, Lincoln TM 1996 Phosphorylation of the inositol 1,4,5-triphosphate receptor. J Biol Chem 271: 21933–21938
Harrison S, Reifsnyder DH, Gallis B, Cadd GG, Beavo JA 1986 Isolation and characterization of bovine cardiac muscle cGMP-inhibited phosphodiesterase: a receptor for new cardiotonic drugs. Mol Pharmacol 29: 506–514
Haynes JJ, Kithas PA, Taylor AE, Strada SJ 1991 Selective inhibition of cGMP-inhibitable cAMP phosphodiesterase decreases pulmonary vasoreactivity. Am J Physiol 261:H487–H492
Perks AM, Ruiz T, Chua B, Vonder Muhl LI, Kindler PM, Blair W 1993 Reabsorption of lung liquid produced by 2,4-Dinitrophenol inin-vitro lungs from fetal guinea pigs. Can J Physiol Pharmacol 71: 1–11
Acknowledgements
The authors thank Hilken Kuck for his excellent technical assistance.
Author information
Authors and Affiliations
Additional information
Supported in part by National Heart, Lung, and Blood Institute Grant HL-10834, Children's Miracle Network, and from Division of Sponsored Research.
Rights and permissions
About this article
Cite this article
Kabbani, M., Cassin, S. The Effects of cGMP on Fetal Sheep Pulmonary Blood Flow and Lung Liquid Production. Pediatr Res 43, 325–330 (1998). https://doi.org/10.1203/00006450-199803000-00003
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199803000-00003