Abstract
Nitric oxide (NO) relaxes vascular smooth muscle by increasing the intracellular concentration of cGMP. In the pulmonary circulation, cGMP is inactivated by specific phosphodiesterases (PDE5). Dipyridamole, a clinically approved drug, has inhibitory activity against PDE5 and has been reported to augment the response to inhaled NO in persistent pulmonary hypertension of the newborn (PPHN). We wished to determine whether dipyridamole alone, or in combination with NO, can be used to treat a newborn lamb model of PPHN. In newborn lambs with PPHN, dipyridamole infused at 0.02 mg/kg/min for 45 min alone, or in combination with 5 ppm of inhaled NO for the final 15 min, significantly decreased pulmonary and systemic blood pressure, decreased pulmonary vascular resistance, and increased pulmonary blood flow. There was no significant difference between the pulmonary vascular effects of 5 ppm NO alone compared with the effects of NO combined with dipyridamole. In control lambs, the 45-min infusion of dipyridamole did not change pulmonary pressure whereas systemic pressure decreased by 28 ± 3%. These systemic effects in control lambs persisted 90 min after discontinuing the dipyridamole infusion. Systemic arteries isolated from both control and PPHN lambs were significantly more sensitive to dipyridamole than pulmonary arteries. We conclude that dipyridamole has significant hemodynamic effects in both the pulmonary and systemic circulations of newborn lambs with pulmonary hypertension as well as in the systemic circulation of newborn control lambs. The pronounced effects of dipyridamole on the systemic circulation limits its utility as an adjunct to inhaled NO in the treatment of PPHN.
Similar content being viewed by others
Main
PVR falls dramatically at birth as the lung assumes the function of gas exchange. In some newborn infants the normal decrease in pulmonary vascular tone does not occur, resulting in PPHN. This condition complicates at least 1 in 1000 live births and results in high morbidity and mortality rates (1). The failure of standard aggressive therapies results in the transfer of approximately 1200 newborns a year with PPHN to specialized centers for ECMO. Because ECMO is invasive and expensive, there is considerable interest in developing effective alternative therapies.
Inhaled NO is a new therapy for PPHN that improves oxygenation and decreases the need for ECMO (2–4). However, NO is not universally effective in infants with PPHN, and its effects are not always sustained (3–8). Furthermore, because NO and its metabolites can be toxic, therapeutic strategies designed to deliver the lowest effective concentration are needed.
Inhaled NO is believed to diffuse into pulmonary vascular smooth muscle cells where it stimulates soluble guanylate cyclase to produce the second messenger cGMP, which then mediates vascular relaxation of the pulmonary circulation.
Cyclic nucleotide phosphodiesterases, by metabolizing intracellular cyclic nucleotides, play an important role in intracellular cGMP signal transduction. Seven subtypes or families of phosphodiesterases have been described which differ in primary structure, relative affinity for cAMP versus cGMP, responses to specific effectors and inhibitors, and mechanisms of regulation (9). One family (PDE5) both binds and hydrolyzes cGMP with high specificity relative to cAMP. One strategy to enhance the pulmonary vascular effects of inhaled NO could be to inhibit cGMP inactivation by PDE5. Specific experimental inhibitors for PDE5 such as zaprinast and E4021 have been reported to dilate the pulmonary circulation, and enhance the effect of endogenous and exogenous NO in a number of animal species with and without experimentally induced pulmonary hypertension (10–15).
Unfortunately, neither zaprinast nor E4021 is approved for use in humans. In contrast, dipyridamole, which also inhibits PDE5 activity, is approved for use in humans as an antithrombotic agent and coronary vasodilator. Dipyridamole dilates the pulmonary circulation in the ovine fetus (16), and it enhances the pulmonary vascular response to inhaled NO in fetal sheep (17). Furthermore, dipyridamole has been recently reported to augment the pulmonary vascular response to 20 ppm of inhaled NO in a human infant with PPHN due to congenital diaphragmatic hernia, although its effect on systemic blood pressure was not mentioned (18). We investigated the effects of dipyridamole alone, and in combination with inhaled NO, on the pulmonary and systemic circulations in control newborn lambs and in a newborn lamb model of PPHN.
METHODS
Surgical preparation. All procedures and protocols in this study were approved by the Laboratory Animal Care Committee at the State University of New York at Buffalo. The technique for creating pulmonary hypertension by prenatal ligation of the ductus arteriosus has been described previously (19). Pregnant Dorsett ewes were fasted for 24 h before surgery at 126-128 d of gestation (term = 146 d). Anesthesia was induced with sodium thiopental and maintained with 1.5-2.0% halothane. The fetal head and left foreleg were delivered through a hysterotomy. A left lateral thoracotomy was performed in the fourth intercostal space of the fetus, and the ductus arteriosus was ligated. The chest was closed and the fetus returned to the uterus. The uterus and the maternal abdomen were closed, and postoperatively the ewe was treated with intramuscular ampicillin (300 mg/d) and gentamicin (40 mg/d) for 48 h. The ewe was allowed to recover for 10 d.
Isolated vessel experiments (n = 5 control, n = 8 after ductal ligation). At 136-139 d gestation, the pregnant ewe was anesthetized as described above, and the fetus was delivered by cesarean section. The fetus was killed before first breath by rapid exsanguination through a direct cardiac puncture. We have described the subsequent techniques previously (20). Immediately after death, the heart and lungs were removed en bloc from the thorax, and an approximately 30-cm section of small intestine including mesentery was removed from the abdomen and placed in Krebs-Ringer solution (mM: NaC1 118, KC1 4.7, CaC12 2.5, MgSO4 1.2, KH2PO4 1.2, NaHCO3 25.5, glucose 5.6, and calcium disodium EDTA 0.026). Fifth generation intralobar pulmonary arteries (21) with inside diameters of 0.5-1.5 mm were isolated, dissected with care to preserve the integrity of the endothelium, and cut into rings approximately 2 mm wide and 0.8-1.5 mg in weight. Mesenteric arteries of equivalent inside diameters were prepared in a similar fashion. Standard tissue bath techniques were used. A continuous recording of isometric force generation was obtained by tying each vessel ring to a force-displacement transducer (Statham UC 2; Statham Instruments, Hato Rey, PR) that was connected to an oscillographic recorder. The vessel rings were allowed to equilibrate for 20 min in the Krebs-Ringer solution. A micrometer was then used to stretch the tissues repeatedly in small increments over the next 45 min until resting tone remained stable at a passive tension of 1.2 g for pulmonary arteries and 0.8 g for mesenteric arteries. Previous experiments determined that this is the optimal length for generation of active tone in response to exogenous norepinephrine (20). Pharmacological agents were purchased from Sigma Chemical Co. (St. Louis, MO) and dissolved in distilled H2O, with the exception of indomethacin and dipyridamole which were dissolved in 100% ethanol and 95% methanol, respectively. Vessels exposed to alcohol vehicle alone (6 µL in 6 mL) showed no response. All vessels were pretreated with 10-6 M propranolol to block β-adrenergic receptors and with 10-5 M indomethacin to prevent the formation of vasoactive prostaglandins. Vessels were preconstricted with an EC50 concentration of norepinephrine (NE, 10-6 M), as determined from previous studies (20). Vessel rings were exposed to 3 × 10 -5 M dipyridamole or zaprinast, either as a single dose or as part of a cumulative concentration-response curve, and then discarded. Some vessels were incubated with the adenosine receptor antagonist 8-SPT (3 × 10-5 M) before the addition of dipyridamole. In another group of pulmonary arteries, cumulative concentration-response curves to SNP were performed in similarly preconstricted vessels with and without pretreatment with dipyridamole (3 × 10-5 M).
Measurement of cGMP (gestational age 136 d; n = 6 ligated and 6 control). Pulmonary arteries were isolated and suspended in tissue baths using the same methods described above. Vessels were pretreated with 10-5 M indomethacin, 10-6 M propranolol and preconstricted with 10-6 M norepinephrine. Four groups of vessels were studied: norepinephrine alone, dipyridamole alone (3 × 10-5 M), SNP alone (10-6 M), and the combination of dipyridamole and SNP. Preliminary experiments showed that the maximal relaxation response to SNP occurred 2 min after its addition; therefore, this was the time point selected for freeze-clamping vessels rapidly in liquid nitrogen. All groups of vessels were preconstricted and previously described (22) by homogenizing the frozen rings in 2 mL of iced 1 N HCI, centrifuging at 1000 × g for 10 min, lyophilizing the supernatant, and resuspending in 250 µL of 0.1 N HCI. The content of cGMP was determined using a commercially available 125I-cGMP assay kit (cGMP [125I] scintillation proximity dual range assay system, Amersham Corporation, Arlington Heights, IL). The content of cGMP is expressed as femtomoles per milligram of tissue weight.
Intact lamb experiments. At 136-139 d gestation, pregnant ewes were fasted and anesthetized as described above. The fetal head was exposed through a hysterotomy, and the trachea was intubated with a 4.0-mm cuffed endotracheal tube. The carotid artery and jugular vein were exposed in the neck, and polyvinyl catheters were inserted and advanced into the aorta and the right atrium, respectively. The fetal chest was exposed and a left thoracotomy was performed. Polyvinyl catheters were placed in the main pulmonary artery and left atrium, and a 10.0-mm ultrasonic transit time flow transducer (Transonic Systems, Inc., Ithaca, NY) was placed around the main pulmonary artery. In control lambs, the ductus arteriosus was identified and ligated with umbilical tape. The umbilical cord was ligated and the lamb delivered. The lamb was wrapped in a homeothermic servo controlled warming blanket (Harvard Apparatus, Edenbridge, KY) and placed under an infant warmer (Air Shields, Vickers) to maintain temperature at 39°C. Ventilation was initiated with a time cycled pressure control ventilator (Siemens Servo 900C, Solna, Sweden) at FiO2 0.95, ventilator rate, 60 breaths/min; peak inspiratory pressure, 30 cm H2O; peak end expiratory pressure, 4 cm H2O; and inspiratory time, 33%. The rate and inspiratory pressure were adjusted to maintain PaCO2 between 35 and 50 mm Hg. In control lambs, the FiO2 was adjusted to maintain PaO2 between 55 and 80 mm Hg. Tris was used to correct any metabolic acidosis defined as a base deficit greater than 10. Systemic hypotension, defined as a decrease in mean blood pressure by more than 15 mm Hg, or an initial Hb of less than 11 g/dL was corrected by administration of 10 mL/kg maternal blood. The newborn lamb was sedated with 10 mg/kg ketamine hydrochloride as needed. The animal was stabilized for 60-120 min before an experimental protocol was begun. During each protocol, no blood or Tris infusions were given and ventilator settings remained constant.
NO was obtained as 1000 ppm in nitrogen (Matheson Gas Products Inc., Twinsburg, OH) and blended with oxygen to obtain 5 ppm. NO was continuously analyzed from the inspired gas immediately before the endotracheal tube by a chemiluminescence analyzer (Thermoenvironmental Instruments, Model 42 H; Franklin, MA). Medical grade dipyridamole (DuPont Merck Pharmaceutical Co., Billerica, MA) was infused at 0.02 mg/kg/min using a continuous infusion pump (Medfusion Systems Inc, Norcross, GA).
Phasic pulmonary arterial, left atrial, aortic, and airway pressures were measured by Gould Statham physiologic pressure transducers (P-23 XL, Gould Electronics, Cleveland, OH) which were calibrated with a mercury column manometer before each experiment. Pulmonary blood flow was measured by a 10.0-mm ultrasonic transit time flow transducer around the main pulmonary artery and processed by a digital flowmeter (Transonic Systems, Model T 101). These data were recorded continuously on a physiologic amplifier-recorder system (Gould Electronics). Pulmonary vascular resistance was calculated as: PVR = (MPAP-LAP)/Qp and reported in units of (mm Hg/mL/kg) where MPAP is main pulmonary artery pressure, LAP is left atrial pressure, and Qp is pulmonary blood flow. Aortic blood was collected for measurement of pH, PO2, PCO2, Hb, and base status (Acid-Base Laboratory 3; Radiometer Medical A/S, Copenhagen, Denmark).
From preliminary experiments examining the effect of 30-min infusions of 0.1, 0.05, 0.02, and 0.01 mg/kg/min dipyridamole in lambs with PPHN (n = 5, data not shown) we selected 0.02 mg/kg/min dipyridamole as the highest dose that did not produce marked systemic hypotension (> 20% drop in aortic pressure). There were three experimental groups of lambs with PPHN: 1) 30 min of observation followed by inhaled NO at 5 ppm for 15 min (n = 6); 2) infusion of dipyridamole into the right atrial catheter for 45 min (n = 6); or 3) infusion of dipyridamole for 45 min with the addition of 5 ppm of inhaled NO for the final 15 min (n = 6). In addition, there was one group of normal control lambs without PPHN which received an infusion of dipyridamole at 0.02 mg/kg/min into the right atrial catheter for 45 min (n = 5). Dipyridamole has a relatively long half-life (23–24), and our preliminary data showed that pulmonary artery pressure and aortic pressure did not return to baseline 2 h after discontinuing dipyridamole. Therefore, separate groups of animals were used for each protocol. After each study the lambs were killed by a lethal dose of sodium pentobarbital.
Data analysis. All data are expressed as mean ± SEM, with n representing the number of animals studied. Statistical analysis was performed with the Statview 4.5 software package (Abacus Concepts, Berkely, CA). Statistical comparisons within groups were performed using analysis of variance (ANOVA) for repeated measures, followed if necessary by Student-Newman-Keuls post hoc testing for multiple comparisons. A Wilcoxon signed rank test was used to compare groups of data not normally distributed. A one-way ANOVA was performed to determine differences in hemodynamic responses between groups of intact lambs at a given point in time. A p value of less than 0.05 was considered significant.
RESULTS
Isolated vessel experiments. Arteries from lambs with pulmonary hypertension tended to be less sensitive to increasing concentrations of SNP than arteries from control lambs (hypertensive versus control EC50: 2.18 ± 0.9 × 10-7 M versus 4.61 ± 1.10 × 10-8 M; p = 0.07). Pretreatment of pulmonary arteries with dipyridamole increased sensitivity to SNP in both groups of arteries, thus shifting concentration response curves to SNP to the left (Fig. 1). Pretreatment with the adenosine receptor antagonist, 8-SPT, did not alter the increase in sensitivity to SNP produced by dipyridamole in either group of arteries.
Dipyridamole pretreatment significantly enhances cumulative concentration response curves to SNP in pulmonary arteries from control (n = 5) and hypertensive (n = 5) fetal lambs. This enhancement was not altered after pretreatment with the adenosine receptor antagonist 8-SPT. Relaxations (mean ± SEM) are expressed as a percent of plateau constriction with 10-6 M norepinephrine (100%). * p < 0.05 for vessels pretreated with dipyridamole (DIP) or the combination of DIP and 8-SPT compared with SNP alone.
cGMP assays. Figure 2 shows cGMP accumulation in pulmonary arteries from both control and hypertensive lambs after 1) norepinephrine preconstriction alone (control), 2) 10-6 M SNP, 3) 3 × 10-5 dipyridamole, or 4 a combination of the two agents. In arteries from control lambs, cGMP content increased significantly after addition of SNP, dipyridamole, or both compared with the NE alone. In contrast, an increase in cGMP content in hypertensive vessels relative to NE alone did not occur after addition of SNP or dipyridamole alone, but did occur when the two were given together.
cGMP accumulation in preconstricted pulmonary arteries from control lambs (n = 6) increased significantly after addition of 10-6 M SNP, 3 × 10-5 M DIP, and the combination of the two. In pulmonary arteries from hypertensive lambs (n = 6), cGMP accumulation increased significantly only after exposure to dipyridamole and SNP together. * p < 0.05 vs control for same vessel type. † p < 0.05 control vs hypertensive.
Intact animal experiments. Hemodynamic data and blood gas variables for each of the three PPHN groups are shown in Table 1, and the changes in pulmonary and systemic blood pressures are graphed in Figure 3. NO alone significantly decreased pulmonary artery pressure, increased pulmonary blood flow, and decreased PVR without changing aortic pressure. Dipyridamole infused at 0.02 mg/kg/min for 45 min significantly decreased pulmonary artery pressure, PVR, and aortic pressure measured at 30 and 45 min, and significantly increased pulmonary blood flow at both 30 and 45 min.
Changes in pulmonary and aortic blood pressure expressed as a percent of baseline for groups of PPHN lambs receiving NO alone (Panel A), DIP alone (Panel B), or dipyridamole followed by NO (Panel C). The decrease in pulmonary pressure with NO was similar between the groups which did and did not receive dipyridamole. Aortic pressure significantly decreased from baseline at 30 and 45 min in both groups receiving dipyridamole (B and C), but not in the group which received NO alone (A). Data are mean ± SEM. n = 6 hypertensive animals in each treatment group. * p < 0.05 compared with baseline (BL) value, † p < 0.05 compared with preNO (30 min) value.
In the group of animals that received a combination of dipyridamole plus NO, the 30-min infusion of dipyridamole alone increased pulmonary blood flow and decreased PVR and aortic pressure. There was a trend for a decrease in pulmonary artery pressure which was not statistically significant (p = 0.10). Addition of NO to dipyridamole significantly decreased pulmonary artery pressure and PVR and significantly increased pulmonary blood flow. Aortic pressure did not decrease further after the addition of inhaled NO. The pulmonary hemodynamic changes observed during the 15-min period of NO inhalation with dipyridamole were not significantly greater than those observed after inhalation of NO alone (Table 1 and Figure 3).
In the group of control animals that received dipyridamole alone, there was no change in pulmonary hemodynamics or arterial blood gas values. Aortic pressure significantly decreased after 30 and 45 min of dipyridamole (baseline: 65 ± 6 mm Hg; 30 min: 48 ± 4 mm Hg; 45 min: 46 ± 4 mm Hg; Figure 4). The decrease in aortic pressure persisted for 60 min after discontinuation of dipyridamole (46 ± 4 mm Hg).
Changes in pulmonary and aortic blood pressure expressed as a percent of baseline for groups of PPHN and control (CONT) lambs receiving dipyridamole alone. Aortic pressure decreased significantly and similarly from baseline at 30 and 45 min in both groups. Pulmonary pressure significantly decreased in the group of lambs with PPHN. Data are mean ± SEM. n = 6 PPHN animals, n = 5 control animals. * p < 0.05 compared with BL value.
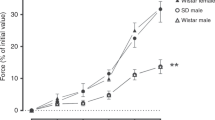
Comparison of pulmonary and mesenteric arteries. Plateau contractile responses to 10-6 M norepinephrine were not statistically different between the groups of pulmonary and mesenteric arteries. The addition of 3 × 10-5 M dipyridamole after norepinephrine preconstriction did not relax pulmonary arteries from lambs with pulmonary hypertension but significantly relaxed pulmonary arteries from control lambs (Fig. 5). Preconstricted mesenteric arteries from both hypertensive and control lambs relaxed similarly, and nearly completely after addition of 3 × 10-5 M dipyridamole. In both control and hypertensive lambs, relaxations to dipyridamole in mesenteric arteries were significantly greater than those observed in pulmonary arteries. Pretreatment with 8-SPT did not alter the response in either group of vessels (data not shown). Preconstricted mesenteric arteries isolated from lambs with PPHN (n = 7) relaxed to a significantly greater degree after addition of increasing concentrations of dipyridamole than zaprinast (Fig. 6).
The addition of 3 × 10-5 M dipyridamole after norepinephrine preconstriction relaxed pulmonary arteries from control lambs and mesenteric arteries from control and hypertensive lambs. In both groups of lambs, relaxations were significantly greater in the mesenteric arteries than in the pulmonary arteries. Data are mean percent relaxations ± SEM. n = 6 for all groups of vessels, * p < 0.05 vs response in pulmonary arteries. † p < 0.05 vs baseline NE constriction.
Preconstricted mesenteric arteries isolated from lambs with PPHN (n = 7) relaxed to a significantly greater degree after addition of increasing concentrations of dipyridamole than zaprinast. Relaxations (mean ± SEM) are expressed as a percent of plateau constriction with 10-6 M norepinephrine (100%). * p < 0.05 vs zaprinast.
DISCUSSION
NO is believed to dilate the pulmonary vasculature by the generation of cGMP. Plasma cGMP concentrations are decreased in human infants with PPHN compared with age-matched controls (25). Our current study demonstrates that cGMP production in response to SNP, an exogenous NO donor, is decreased in pulmonary arteries isolated from lambs with pulmonary hypertension compared with controls (Fig. 2). This finding is similar to previous reports in this and other models of pulmonary hypertension (20,26). We have further reported that responsivity to exogenous cGMP (when delivered as 8-bromo-cGMP) is normal in the ductal ligation model of PPHN (20).
Low cGMP production to exogenous NO may explain why some human infants do not have an adequate or sustained clinical response to inhaled NO (3–5,8). cGMP concentrations are regulated in part by inactivation by specific phosphodiesterases such as PDE5 which are found in high concentrations in bovine lung homogenates (27) and in pulmonary arteries isolated from human patients (28). Therefore, specific PDE5 inhibitors may result in selective pulmonary vasodilation, may allow more infants to adequately respond to inhaled NO, and may decrease the dose of inhaled NO required to improve pulmonary hemodynamics. Dipyridamole, a drug which has been used in humans for many years, has significant activity against PDE5 (29), although it may be less selective for PDE5 than the experimental inhibitor zaprinast (9). Recent data indicate that dipyridamole enhances the pulmonary vascular response to inhaled NO in fetal lambs (17), and it was recently used successfully to augment the response to inhaled NO in an infant with congenital diaphragmatic hernia (18).
In the current study, the effects of dipyridamole in control and hypertensive lambs were greater in the systemic than pulmonary circulations in both intact animal studies (Fig. 4) and isolated vessel protocols (Fig. 5). In lambs with PPHN, a 30-min infusion of 0.02 mg/kg/min dipyridamole decreased pulmonary pressure by 6 ± 2%, but decreased aortic pressure by 18 ± 4%. In control lambs, the same dose of dipyridamole had no effect on pulmonary pressure but decreased aortic pressure by 25 ± 3%. Preliminary experiments (data not shown) suggested that the systemic effects were even greater when higher doses of dipyridamole were used. In the normal fetal lamb, systemic hypotension was only reported at a dose of dipyridamole much higher than we used (4.0 mg/min for 10 min), whereas lower doses of dipyridamole did not decrease systemic arterial pressure (16). The absence of systemic hypotension after dipyridamole in fetal lambs might be explained by the ability of the placental circulation to clear dipyridamole or to provide volume infusion to compensate for systemic vasodilation in the fetus. Both control and pulmonary hypertensive newborn animals experienced significant hypotension in our study, indicating that the mechanism is related to fetal age and not to vascular alterations unique to PPHN. Our data suggest that the dilation of systemic vessels to dipyridamole is independent of adenosine receptor activation. Dipyridamole has been reported to increase cAMP concentrations through inhibition of cAMP-specific phosphodiesterases (30,31) and to enhance prostacyclin production (32,33). Either mechanism could explain the systemic effects we observed.
In contrast, our data indicate that dipyridamole dilates pulmonary arteries from control lambs by a mechanism which is dependent on cGMP. The down-regulation of pulmonary vascular endothelial NO synthase activity and content in the ductal ligation model (34) supports the lack of functional relaxation or increase in cGMP in response to dipyridamole in the pulmonary arteries isolated from PPHN lambs in the current study. Our studies in intact lambs with PPHN showed that dipyridamole had a small, but significant effect on the pulmonary circulation. Other investigators have reported pulmonary vasodilation following dipyridamole in animal models of pulmonary hypertension induced by hypoxia (35,36). Preliminary data suggest that PDE5 activity is increased in the lungs of lambs with PPHN (37,38) which could explain this pulmonary vascular response to dipyridamole. However, we previously reported that a higher dose of zaprinast, a potent inhibitor of PDE5 activity, had no effect by itself on pulmonary hemodynamics of lambs with PPHN (14). We therefore speculate that effects of dipyridamole other than cGMP phosphodiesterase inhibition as described above are a more likely explanation for the pulmonary vascular effects we observed in vivo.
For example, dipyridamole has other potential vasoactive properties including inhibition of phosphodiesterase isozymes which primarily degrade cAMP (30,31), inhibition of adenosine uptake by erythrocytes and endothelial cells (39), and direct enhancement of prostacyclin production (32,33). Exogenous adenosine at low doses is a selective pulmonary vasodilator in newborn lambs but has significant systemic vasodilatory effects at doses greater than 0.3 µmol/kg/min (40). Inhibiting its uptake with dipyridamole might lead to higher extracellular adenosine concentrations and increased endothelial and smooth muscle cell adenosine receptor activation. However, our isolated vessel protocols using the adenosine receptor antagonist 8-SPT support the findings of Skimming et al. (41) in newborn lambs with pharmacologically induced pulmonary hypertension and those of Zeigler et al. (16) from fetal sheep. Both studies found that the vasodilatory effects of dipyridamole are independent of adenosine receptors.
Our study was designed to determine whether dipyridamole would enhance the effect of exogenous NO in PPHN. Our in vitro data show that dipyridamole enhances functional relaxations and cGMP concentrations in response to SNP. In contrast, the combination of i.v. dipyridamole did not enhance the pulmonary vascular effects of inhaled NO in intact lambs with PPHN. Using the same lamb model of pulmonary hypertension, we previously reported a synergistic effect on pulmonary hemodynamics when zaprinast and inhaled NO were delivered together (14). However, we observed only a modest 10% decrease in systemic blood pressure despite using a zaprinast dose which was 5-fold higher than the equimolar equivalent of dipyridamole used in the current study. Our data further show that dipyridamole is a more potent dilator of mesenteric arteries than zaprinast (Fig. 6). Therefore, we conclude that systemic hypotension restricted us from delivering a dipyridamole dose that produced PDE5 inhibition equivalent to that of zaprinast.
Pulmonary hypertension can be produced in many different ways experimentally. The ductal ligation model of pulmonary hypertension is a chronic preparation which results in vascular remodeling similar to that seen in newborns dying from PPHN (42), and this remodeling may alter the expression of critical enzymes in the NO pathway (20,34,38). Because these alterations would not be expected in acute models of pulmonary hypertension not accompanied by remodeling, we speculate that this explains why the combination of dipyridamole with inhaled NO was not effective in our study but was effective in normal fetal lambs (17). We conclude that like many of the other i.v. vasodilators used in the treatment of PPHN, dipyridamole's clinical applicability, alone or in combination with inhaled NO, will be limited by its effects on the systemic circulation.
Abbreviations
- NO:
-
nitric oxide
- PPHN:
-
persistent pulmonary hypertension of the newborn
- PDE5 cGMP-binding:
-
cGMP-specific phosphodiesterase
- ECMO:
-
extracorporeal membrane oxygenation
- PVR:
-
pulmonary vascular resistance
- EC50:
-
estimated concentration producing a 50% constriction or relaxation
- 8-SPT:
-
8-sulfophenyltheophylline
- SNP:
-
sodium nitroprusside [key]perinatal pulmonary circulation, guanylate cyclase, nitric oxide, cGMP
References
Hageman JR, Adams MA, Gardner TH 1984 Persistent pulmonary hypertension of the newborn. Trends in incidence, diagnosis, and management. Am J Dis Child 138: 592–595
Kinsella JP, Truog WE, Walsh WF, Goldberg RN, Bancalari E, Mayock DE, Redding GJ, Delemos RA, Sardesai S, McCurnin DC, Moreland SG, Cutter GR, Abman SH 1997 Randomized, multicenter trial of inhaled nitric oxide and high-frequency oscillatory ventilation in severe persistent pulmonary hypertension of the newborn. J Pediatr 131: 55–62
Roberts JD, Fineman J, Morin FC III, Shaul PW, Rimar S, Schreiber MD, Polin RA, Thusu KG, Zayek M, Zwass MS, Zellers TM, Wylam ME, Gross I, Zapol WM, Heymann MA 1997 Inhaled nitric oxide gas improves oxygenation in PPHN. N Engl J Med 336: 605–610
Neonatal Inhaled Nitric Oxide Study Group 1997 Inhaled nitric oxide in full-term and nearly full-term infants with hypoxic respiratory failure. N Engl J Med 336: 597–604
Barefield ES, Karle VA, Philips JB III, Carlo WA 1996 Inhaled nitric oxide in term infants with hypoxemic respiratory failure. J Pediatr 129: 279–286
Finer NN, Etches PC, Kamstra B, Tierney AJ, Peliowski A, Ryan CA 1994 Inhaled nitric oxide in infants referred for extracorporeal membrane oxygenation: dose response. J Pediatr 124: 302–308
Karamanoukian HL, Glick PL, Zayek M, Steinhorn RH, Zwass MS, Fineman JR, Morin FC III 1994 Inhaled nitric oxide in congenital hypoplasia of the lungs due to diaphragmatic hernia or oligohydramnios. Pediatrics 94: 715–718
Steinhorn RH, Cox PN, Fineman JR, Finer NN, Rosenberg EM, Silver MM, Tyebkhan J, Zwass MS, Morin FC III 1997 Inhaled nitric oxide enhances oxygenation but not survival in infants with alveolar capillary dysplasia. J Pediatr 130: 417–422
Beavo JA 1995 Cyclic nucleotide phosphodiesterases: functional implications of multiple isoforms. Physiol Rev 75: 725–748
Braner DAV, Fineman JR, Chang R, Soifer SJ 1993 M&B 22948, a cGMP phosphodiesterase inhibitor, is a pulmonary vasodilator in lambs. Am J Physiol 264: H252–H258
Ichinose F, Adrie C, Hurford WE, Zapol WM 1995 Prolonged pulmonary vasodilator action of inhaled nitric oxide by zaprinast in awake lambs. J Appl Physiol 78: 1288–1295
McMahon TJ, Ignarro LJ, Kadowitz PJ 1993 Influence of Zaprinast on vascular tone and vasodilator responses in the cat pulmonary vascular bed. J Appl Physiol 74: 1704–1711
Skimming JW, DeMarco VG, Kadowitz PJ, Cassin S 1996 Effects of zaprinast and dissolved nitric oxide on the pulmonary circulation of fetal sheep. Pediatr Res 39: 223–228
Thusu KG, Morin FC III, Russell JA, Steinhorn RH 1995 The cGMP phosphodiesterase inhibitor zaprinast enhances the effect of nitric oxide. Am J Resp Crit Med 152: 1605–1610
Cohen Ah, Hanson K, Morris K, Fouty B, McMurtry IF, Clarke W, Rodman DM 1996 Inhibition of cyclic 3′-5′-guanosine monophosphate-specific phosphodiesterase selectively vasodilates the pulmonary circulation in chronically hypoxic rats. J Clin Invest 97: 172–179
Ziegler JW, Ivy DD, Fox JJ, Kinsella JP, Clarke WR, Abman SH 1994 Dipyridamole, a cGMP phosphodiesterase inhibitor, causes pulmonary vasodilation in the ovine fetus. Am J Physiol 269: H473–H479
Ziegler JW, Ivy DD, Kinsella JP, Clarke WR, Abman SH 1994 Dipyridamole potentiates pulmonary vasodilation induced by acetylcholine and nitric oxide in the ovine fetus. Am J Respir Crit Care Med 157: 1104–1110
Kinsella JP, Torielli F, Ziegler JW, Ivy DD, Abman SH 1995 Dipyridamole augmentation of response to nitric oxide. Lancet 346: 647–648
Morin FC III, Eagan EA 1989 The effect of closing the ductus arteriosus on the pulmonary circulation of the fetal sheep. J Dev Physiol 11: 245–250
Steinhorn RH, Russell JA, Morin F III 1995 Disruption of cyclic GMP production in pulmonary arteries isolated from fetal lambs with pulmonary hypertension. Am J Physiol 268: H1483–H1489
Weibel ER 1991 Design of airways and blood vessels considered as branching trees. In: Crystal RG and West JB eds, The Lung: Scientific Foundations. Raven Press, Ltd, New York, 711
Johns R, Linder J, Peach M 1989 Endothelium-dependent relaxation and cyclic GMP accumulation in rabbit pulmonary artery are selectively impaired by moderate hypoxia. Circ Res 65: 1508–1515
Nielsen-Kudsk F, Pedersen AK 1979 Pharmacokinetics of dipyridamole. Acta Pharmacol Toxicol 44: 391–399
Mahony C, Wolfram KM, Cocchetto DM, Bjornsson TD 1982 Dipyridamole kinetics. Clin Pharmacol Ther 31: 330–338
Christou H, Adatia I, VanMarter LJ, Kane JW, Thompson JE, Stark AR, Wessel DL, Kourembanas S 1997 Effect of inhaled nitric oxide on endothelin-1 and cyclic guanosine 5′-monophosphate plasma concentrations in newborn infants with persistent pulmonary hypertension. J Pediatr 130: 603–611
Crawley DE, Zhao L, Giembycz MA, Liu S, Barnes PJ, Winter RJD, Evans TW 1992 Chronic hypoxia impairs soluble guanylyl cyclase-mediated pulmonary arterial relaxation in the rat. Am J Physiol 263: L325–L332
Thomas MK, Francis SH, Corbine JD 1990 Characterization of a purified bovine lung cGMP-binding cGMP phosphodiesterase. J Biol Chem 265: 14964–14970
Rabe KF, Tenor H, Dent G, Schudt C, Nakashima M, Magnussen H 1994 Identification of PDE isozymes in human pulmonary artery and effect of selective PDE inhibitors. Am J Physiol 266: L536–L543
Lugnier C, Schoeffter P, Lebec A, Strouthou E, Stoclet JC 1986 Selective inhibition of cyclic nucleotide phosphodiesterases of human, bovine, and rat aorta. Biochem Pharmacol 35: 1743–1751
Fitzgerald GA 1987 Drug therapy: dipyridamole. N Engl J Med 316: 1247–1257
Thompson WJ 1991 Cyclic nucleotide phosphodiesterases: pharmacology, biochemistry and function. Pharmacol Ther 51: 13–33
Masotti G, Poggesi L, Galanti G, Serneri GGN 1979 Stimulation of prostacyclin by dipyridamole. Lancet 1: 1412–1414
Van de Velde VJS, Blut H, Weisenberger H, Herman AG 1981 Dipyridamole stimulates prostacyclin production in isolated rat aortic tissue. Arch Int Pharmacodyn Ther 256: 327–328
Shaul PW, Yuhanna IS, German Z, Chen Z, Steinhorn RH, Morin FC III 1997 Pulmonary endothelial NO synthase gene expression is decreased in fetal lambs with pulmonary hypertension. Am J Physiol 272: L1005–L1012
Rosenkrantz JG, Lynch FP, Vogel JHK 1972 Hypoxic pulmonary hypertension: its modification by dipyridamole. J Surg Res 12: 330–333
Mlczoch J, Weir EK, Grover RF 1977 Inhibition of hypoxic pulmonary vasoconstriction by dipyridamole is not platelet mediated. Can J Physiol Pharmacol 55: 447–451
Hanson KA, Abman SH, Clarke WR 1996 Elevation of pulmonary PDE5-specific activity in an experimental fetal ovine perinatal pulmonary hypertension model. Pediatr Res 39: 334A
Sanchez LS, Bloch KD, Morin FC III, Steinhorn RH 1997 Phosphodiesterase 5 enzyme activity and gene expression are altered in newborn lambs with persistent pulmonary hypertension. Pediatr Res 41: 267A
Crutchley DJ, Ryan US, Ryan JW 1980 Effects of aspirin and dipyridamole on the degradation of adenosine diphosphate by cultured derived from bovine pulmonary artery. J Clin Invest 66: 29–35
Konduri GG, Woodard LL, Mukhopadhyaya A, Deshmukh DR 1992 Adenosine is a pulmonary vasodilator in newborn lambs. Am Rev Respir Dis 146: 670–676
Skimming JW, DeMarco VG, Cassin S 1997 Effects of dipyridamole and adenosine infusions on ovine pulmonary and systemic circulations. Am J Physiol H921–H926
Wild LM, Nickerson PA, Morin FC III 1989 Ligating the ductus arteriosus before birth remodels the pulmonary vasculature of the lamb. Pediatr Res 25: 251–257
Acknowledgements
The authors gratefully acknowledge Sylvia Gugino and Daniel Swartz for expert technical assistance in performing these experiments.
Author information
Authors and Affiliations
Additional information
Supported by grants from the National Heart, Lung, and Blood Institute Grant #HL-54705 (R.H.S.), American Heart Association, and the Women and Children's Research Fund of Buffalo.
Presented in part at the 1996 American Pediatric Society-Society for Pediatric Research Annual Meeting, Washington DC, May 6-10, 1996.
Rights and permissions
About this article
Cite this article
Dukarm, R., Morin, F., Russell, J. et al. Pulmonary and Systemic Effects of the Phosphodiesterase Inhibitor Dipyridamole in Newborn Lambs with Persistent Pulmonary Hypertension. Pediatr Res 44, 831–837 (1998). https://doi.org/10.1203/00006450-199812000-00002
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199812000-00002
This article is cited by
-
Increased expression of the cGMP‐inhibited cAMP‐specific (PDE3) and cGMP binding cGMP‐specific (PDE5) phosphodiesterases in models of pulmonary hypertension
British Journal of Pharmacology (2002)