Abstract
Owing to poor reliability of laboratory tests, diagnosis of food allergy is based on clinical response to double-blind placebo-controlled food challenge. The aim of the present study was to assess the value of duodenal IgE-positive cells in the diagnosis of food allergy. Thirty-one children with a history of possible food allergy underwent duodenal biopsies, skin prick tests, and measurement of serum IgE antibodies, and were put on an elimination diet followed by food challenge. Open food challenges were performed in patients under 12 mo of age, and double-blind placebo-controlled challenges were for suspected foods. On the basis of clinical food hypersensitivity, patients were divided into two groups. Group 1 consisted of 13 children with food allergy. Thirteen of 20 positive provocations elicited reactions within 12 h from the end of the challenge, seven later. Group 2 was the control group and included 18 patients with negative food challenges. The number of IgE-positive cells in biopsy specimens was significantly more elevated in group 1 with respect to group 2 (153.24 ± 83.13 versus 18.4 ± 18.9; p < 0.01). Total serum IgE levels were elevated compared with that of the control group (p < 0.01) and correlated with the number of IgE-positive cells (p < 0.001, r = 0.62). Enhanced IgE-containing cells were found in all delayed reactors, but about one-third had negative skin prick tests or specific serum IgE antibodies to the offending foods. Our results showed that systemic reactions to foods are associated with an IgE-mediated response in the duodenal mucosa. Larger studies would be required to assess the predictive value of an increased number of IgE-positive cells in the diagnosis of allergy to food, especially in children with delayed reactions.
Similar content being viewed by others
Main
Elimination diet followed by double-blind placebo-controlled food challenge is considered the gold standard for the diagnosis of food allergy in infants and children (1). Immediate reactions after food challenge can be easily identified, whereas delayed reactions can be difficult to recognize (2). Therefore, nonclinical criteria for diagnosing food allergy are required. Among proposed diagnostic tests, SPTs and measurement of serum-specific IgE antibodies to foods are commonly performed in children with suspected food allergy. However, these tests should be regarded as only suggestive of food allergy (3,4).
IgE-positive cells have been demonstrated in the intestinal mucosa by immunoelectron microscopy (5). However, conflicting results have been reported on the presence of IgE-containing cells in the mucosa of the small intestine and on their relation to serum-specific IgE antibodies in uncontrolled studies in patients with food allergy (6–11). So far, no comparative data are available on the diagnostic accuracy of SPT to foods versus positive IgE cells in the intestinal mucosa, and on the correlation between duodenal IgE-containing cells and the total serum IgE level.
We were therefore interested first, in clearly ascertaining the value of duodenal IgE-positive cells in the diagnosis of food allergy in children, and second, in comparing the finding of duodenal mucosal IgE-containing cells with SPT results and serum IgE levels.
METHODS
Patients. Thirty-one children with a history of symptoms which could be caused by food allergy were consecutively enrolled in the study. Complaints were vomiting in 24 cases, eczema in 14, diarrhea in 5, abdominal pain in 3, asthma in 2, urticaria in 2, angioedema in 1, failure to thrive in 1.
All children underwent endoscopy of the intestinal upper tract (Olympus GIF-XP 20) before beginning an elimination diet. Duodenal biopsies were taken in all children. The children were investigated while having symptoms or within 24 h from the last appearance of clinical signs of allergy. Immunologic studies were carried out in all patients.
To ascertain the presence of clinical food hypersensitivity, children were put on a 14-d restricted diet. During this period, patients were allowed to eat only soy milk, tea, water, sucrose, rice, carrots, lettuce, potatoes, rabbit's meat, pears, and olive oil, if none of these foods was suspected of eliciting clinical reactions and SPT results were negative (12). None of these infants was breast-fed. Calcium supplements were given. If symptoms improved on this diet, oral challenges to common foods were performed. Each food was given for 4 d at home. Children were visited before and after the challenge and if reactions occurred. Challenges for foods suspected of eliciting adverse reactions, on the basis of positive immunologic tests or if a suggestive history was present, were performed at the hospital (12). Open challenge tests were performed in infants under 12 mo of age, and double-blind placebo-controlled food challenges in children over 1 y of age (1). Briefly, children were administered increasing doses of food or placebo every 20 min. The total amount of food was equal to the average daily intake, e.g. one egg. Patients were observed for 5 h. If no symptom occurred, parents gave the food at home for 4 d. As a placebo, a soy formula (Humana SL, Humana Italia, Milan, Italy) was used in the children who were tolerant. In the children with suspected soy allergy and in soy challenge, an amino acid-derived formula (Nutri-junior, Nutricia, Milan, Italy) was used. Positive responses to placebo were never found. In one case provocation was not performed because the child had a convincing history of a severe anaphylactic reaction and a positive SPT result. All children who improved after the elimination diet had at least one positive food challenge. No children were on antihistamines, oral steroids, or β-agonists at the time of the study.
According to the presence or absence of clinical reactions to oral food challenge, children were included in the food-allergic patient or the control group, respectively. The food-allergic patient group consisted of 13 children (8 boys and 5 girls; age range, 2 mo to 4 y, mean 15 ± 13 mo) with positive food challenge (see Table 1). Thirteen of 20 positive provocation tests elicited reactions within 12 h from the end of the challenge. These early reactors presented the following symptoms: vomiting in 8 cases, urticaria in 5, rash in 5, angioedema in 4, diarrhea in 4, eczema in 1, asthma in 1, rhinitis in 1. Seven single delayed reactions which started more than 12 h after challenge occurred: eczema in 6 cases and diarrhea in 1. Two children had early reactions and then developed delayed symptoms: eczema in 2 cases and diarrhea in 1. Eleven children were found to be allergic to cow's milk, 5 to egg, 3 to wheat, and 1 to lamb's meat.
The control group consisted of 18 patients (12 boys and 6 girls; age range, 5 mo to 10 y, mean, 44 ± 41 mo) who did not have food allergy (negative oral food challenge results). The age of the control group was significantly higher than that of the patient group (p < 0.001). Control patients were referred with the following symptoms: vomiting in 17 cases, eczema in 3, diarrhea in 2, abdominal pain in 2, asthma in 1, failure to thrive in 1. Parents of all patients gave written consent.
Immunologic studies. All children were given SPTs with food extracts (1:20, w:v) (Bayropharm, Milan, Italy) of hen's egg, cow's milk, goat's milk, pea, wheat, oat, corn, barley, rice, bean, peanut, pear, peach, apple, banana, tomato, potato, carrot, soy, cod, tuna, salmon, beef, pork, lamb's meat, chicken, and rabbit's meat. The size of the skin test wheal was compared with histamine chloride, 1 mg/mL, and the diluent. SPTs were considered positive if the diameter of the wheal was greater than 3 mm, after subtracting the diameter of the wheal of the diluent (12) and was graded in comparison with the histamine wheal: + + + + if greater than twice the area of the histamine standard, + + + if twice the area of the histamine standard, + + if equal to the area of the histamine standard, and + if half the area of the histamine standard (13). Serum circulating IgE antibodies to foods were measured by Phadebas RAST (radioallergosorbant test) (Pharmacia, Uppsala, Sweden). Total serum IgE was measured by Phadebas PRIST (Pharmacia, Uppsala, Sweden).
Immunofluorescent study. Duodenal biopsies were immediately fixed in periodate-lysine-paraformaldehyde, which can preserve antigenicity better than conventional fixative (14). The periodate-lysine-paraformaldehyde solution was prepared as follows: 0.1 M dibasic sodium phosphate was added to 0.2 M lysine-HC1 in distilled water until a pH of 7.4 was achieved. The solution was then diluted to 0.1 M lysine with 0.1 M sodium phosphate buffer, pH 7.4 (resulting phosphate concentration was 0.05 M). After the fixation with the paraformaldehyde solution, solid sodium m-periodate was added. Then, the tissues were washed with three changes of cacodylate 0.1 M buffer solution for 30 min each, and then overnight at 4°C with cacodylate 0.1 M buffer solution to which 7% sucrose had been added. Excess washing solution was removed, and the specimens were rinsed with four changes of acetone for 10 min each. Dehydrated specimens were treated with xylol for 30 min and embedded in paraffin. Serial sections were cut at about 2-3 µm on a sliding microtome (LKBF, Sweden). The specimens were dried on a plate at 37°C. For histology, adjacent tissue sections were subjected to conventional mast cell staining procedures with toluidine blue or were stained with hematoxylin and eosin. For immunohistochemistry, adjacent sections were treated with xylol for 15 min, then with ethanol, and washed with water. After treatment with PBS buffer, the specimens were incubated overnight with commercially prepared fluorescent antisera specific for human IgE (Dako, Copenhagen, Denmark) at 4°C. The sections were washed with three changes of PBS buffer. The specimens were examined under a Leitz Ortholux incident-light fluorescent microscope. The lamina propria cells with IgE fluorescence were counted by a observer unaware of the clinical data. Counting was performed with a ×40 objective. In each case the number of cells in 10 different adjacent areas of the mucosa above the muscularis mucosae was counted, giving the number of cells/10 visual fields. Nasal polyps were used as a positive control tissue (15), whereas negative controls were carried out by the absence of staining in positive sections after blocking antigenic binding sites with nonconjugated antisera. The specificity of the anti-IgE antiserum was confirmed by lack of cytoplasmic immunofluorescence on monoclonal bone marrow preparations using antisera detected against IgA, IgG, IgM, and IgD.
Adjacent tissue sections stained with toluidine blue or with hematoxylin and eosin were examined by conventional transmission microscopy to identify IgE-positive cells (4). Furthermore, the number of mast cells/10 visual fields was counted.
Data analysis. Data are presented as mean ± SD. ANOVA was used to compare continuous variables. Logarithmically transformed serum IgE levels showed a normal distribution. We considered 95% of the number of duodenal IgE-positive cells in control subjects as the normal value. Sensitivity, specificity, and predictive accuracy of diagnostic tests were calculated using standard formulas (16). Differences in the ability of diagnostic tests to discriminate children with food allergy were compared by McNemar's test with Yates continuity correction. A χ2 test with Yates continuity correction was used to compare differences in percentages of food-allergic and control children who had elevated total serum IgE. Correlations were examined by linear regression analysis and by Spearman rank correlation coefficient (rS).
RESULTS
Immunologic studies. The mean logarithmic total serum IgE levels in the food-allergic children (2.12 ± 0.62) were significantly elevated compared with that of the control group (1.44 ± 0.23) (p < 0.01). Total serum IgE were elevated for age (17) in 10 out of 13 (76%) children with food allergy and in 2 out of 18 control subjects (11%) (p < 0.001).
Positive SPT reactions to at least one food were found in 10 of 13 (76%) children in the food-allergic group and in 4 of 18 (22%) children in the control group (p < 0.01). In the food-allergic group, 8 children had positive SPT reactions to cow's milk, 6 to egg, 4 to wheat, 3 to pea, 3 to peanut, 2 to oat, 2 to barley, 2 to potato, 2 to pork, 2 to beef, 1 to soy, 1 to pear, 1 to carrot, 1 to bean, 1 to lamb's meat, and 1 to tomato. SPT reactions were positive to 16 of the 20 (80%) offending foods. Eight children were positive to cow's milk, 4 to egg, 3 to wheat, and 1 to lamb's meat (Table 1). In the control group, SPT reactions were positive to cow's milk in 2 cases, to egg in 2, and to pear in 1.
Specific serum IgE antibodies to one or several foods were found in 11 (84%) children in the food-allergic group and in 3 (16%) children in the control group (p < 0.001). In the food-allergic group, 7 children had specific serum IgE antibodies to cow's milk, 7 to egg, 3 to wheat, 2 to rice, 2 to potato, 2 to soy, 2 to pea, 2 to peanut, 2 to lamb's meat, 1 to beef, 1 to pork, 1 to pear, 1 to barley, and 1 to oat. Specific serum IgE antibodies to 14 of the 20 (70%) offending foods were found. Seven children had IgE antibodies to cow's milk, 4 to egg, and 3 to wheat (Table 1). In the control group, specific serum IgE antibodies to egg were found in 2 cases, to cow's milk in 1, and to wheat in 1. Among the early reactors group, one child was SPT-negative and 3 food-specific IgE antibody-negative. Two children who had isolated delayed reactions to cow's milk had both negative SPT and food-specific IgE antibodies. Results of both SPTs and specific serum IgE antibodies for the antigens most frequently associated with clinical reactions were found to have poor positive predictive accuracy and sensitivity, but high specificity and negative predictive accuracy. Total serum IgE level gave similar values of sensitivity, specificity, and predictive accuracy (Table 2).
There was no significant difference between results of SPT and allergen-specific serum IgE antibodies in identifying children with egg or cow's milk allergy. Furthermore, no significant differences was found between total serum IgE level and results of SPT, or food-specific IgE antibodies, or SPT-positive food-specific IgE antibodies in identifying allergic subjects. Positive SPT and RAST reactions were not associated with the time of onset of symptoms.
Patients 3 and 11 (Table 1) who had only atopic dermatitis after challenge were followed up in the outpatient clinic to have confirmation of the positive cow's milk challenge. No eczematous lesion appeared on a cow's milk-free diet during a 1-y follow-up.
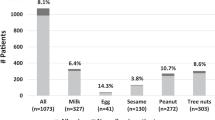
IgE-containing cells in the duodenal mucosa. The distribution of the number of IgE-positive cells in the biopsy specimens from the food-allergic children (153.24 ± 83.13) was significantly elevated compared with that of the control group (18.4 ± 18.90) (p < 0.01) (Fig. 1). The number of IgE-positive cells was significantly more elevated in children who developed isolated delayed reactions (82.66 ± 23.69) than in control subjects (p < 0.01). This number was not significantly different between children who developed isolated delayed reactions and the remaining food-allergic children. The prevalence of elevated numbers of IgE-containing cells in food-allergic children was 92%. The number of duodenal IgE-positive cells correlated with the total serum IgE level (r = 0.62; p < 0.001) (Fig. 2) (rS = 0.64; p < 0.001). Age (17 children under 18 mo versus 14 children over 18 mo), sex (11 female versus 20 male), or symptoms did not significantly influence the number of IgE-positive cells or the total IgE concentrations in serum.
Values of sensitivity, specificity, and positive and negative predictive accuracy calculated for the number of duodenal IgE-containing cells and total serum IgE level for clinical hypersensitivity to at least one food are listed in Table 3. In general, the diagnostic accuracy of IgE-containing cells was high. However, there was no significant difference between the number of IgE- containing cells and total serum IgE level in identifying children with food allergy.
Among 12 food-allergic children with an elevated number of duodenal IgE-positive cells, two had negative SPTs and specific IgE antibodies to the offending foods, and one of them had a normal serum IgE level. Both children had isolated delayed clinical reactions after food challenges (Table 1).
The number of duodenal IgE-containing cells in children with clinical reactions to cow's milk was found to have a high but not absolute diagnostic accuracy. Sensivity and negative predictive accuracy of duodenal IgE-positive cells in children with clinical hypersensitivity to egg were high, but positive predictive accuracy and specificity were poor (Table 2). There was no significant difference between the number of IgE-containing cells and the results of SPT, or food-specific serum IgE antibodies, or SPT-positive allergen-specific IgE antibodies or serum IgE levels in identifying children with clinical hypersensitivity to cow's milk and egg.
In children with food allergy, a marked inflammatory cell infiltration which includes lymphocytes, mostly plasma cells, polymorphs, and some eosinophils was observed in the duodenal mucosa. The number of mast cells was 3.6 per 10 visual fields. In the control group, mast cells were virtually absent and the infiltrate poor. IgE-positive cells were judged to be principally mononuclear cells. Most of them were recognized as plasma cells; mast cells represented 2.3% of IgE-positive cells.
DISCUSSION
The results of this study showed that IgE-positive cells in the duodenal mucosa are significantly increased in children with food allergy. These findings were consistent with previous reports describing an association of duodenal IgE-containing cells with cow's milk allergy (7–9). Uncontrolled Finnish studies (6,10,11) found different results in terms of IgE-positive cells at the site of the intestinal mucosa. However, it is not easy to make a comparison between our results and theirs because of the different experimental design and immunohistochemical techniques used and because of the lack of antisera specificity, especially before 1980 (18). These differences may also explain our observation of IgE-positive cells being mainly plasma cells. This finding is in accordance with some previous studies (5,8), but at variance with the results of others (19) which showed predominantly mast cells.
Further, our data show that sensitivity, specificity, and predictive indices of duodenal IgE-positive cells are similar to those of SPTs and specific serum IgE antibodies to foods. The diagnostic accuracy of SPTs and specific serum IgE antibodies to cow's milk and egg was comparable to that reported in previous studies (3,4). The measurement of mucosal duodenal IgE-positive cells provided no diagnostic advantage over total serum IgE in predicting clinical food allergy. As the prevalence of food allergy in our population was higher than in the general population (20), normal numbers of IgE-containing cells should be considered useful to rule out clinical food hypersensitivity. Increased numbers of IgE immunoreactive cells should be regarded only as suggestive of a reaction to foods (21).
Schrander et al. (8) determined in 16 children with cow's milk intolerance the diagnostic value of duodenal mucosal IgE-positive cells, stained by the immunoperoxidase technique, and of specific serum IgE antibodies in comparison to cow's milk challenge. The specificity and positive predictive accuracy of the number of IgE-positive cells were comparable to ours, but sensitivity was lower. However, these authors did not describe how the food challenge was performed and which symptoms were induced. They carried out a qualitative rather than a quantitative evaluation of the immunohistochemical stainings. SPTs were not studied.
In children who have delayed clinical reactions to foods, immunologic tests are considered to have no diagnostic value (22,23). Interestingly, we found that delayed reactors had a significantly elevated number of mucosal duodenal IgE-positive cells, even in the absence of elevated total serum IgE levels, specific serum IgE antibodies, or positive SPT to the offending food. Thus, our findings suggest that not only acute onset reactions but also delayed reactions, occurring at least 12 h after food exposure, are IgE-mediated (24). However, the diagnostic value of this observation needs to be further clarified.
In some delayed reactors, symptoms cannot be easily related to the reintroduction of a food, because of a long time lag or the variable course of the disease. Therefore, we followed up patients 3 and 11 (Table 1) to confirm the positive cow's milk challenge. During a 1-y follow-up, no eczematous lesion appeared in children given a cow's milk-free diet.
In our study population, children with food allergy were significantly younger than were control children. This is in agreement with studies (25,26) which reported a higher prevalence of adverse reactions to food in infancy and early childhood. Total serum IgE levels increase during childhood (17), but were found to be lower in the control group. Therefore, we think that the different age of the two groups did not influence our results.
Previous studies have offered evidence of intestinal mucosal damage in some patients with food allergy, by documenting 1) minor morphologic changes in the mucosa of the small intestine (27–30), 2) an increased gastrointestinal permeability (31–34), and 3) reactions on the gastric mucosa after intragastric food challenge under endoscopy (35). However, the mechanisms responsible for intestinal alterations in food-allergic patients are poorly understood (36). Several studies indicate that immediate hypersensitivity reactions are involved. In children with food allergy, elevated IgE levels have been found both in feces (37) and intestinal washings (38), and the fecal eosinophil cationic protein concentration is enhanced (39). Our results extend these previous observations by showing a significant correlation between clinical food hypersensitivity and an increased number of duodenal mucosal IgE-positive mast cells as well as IgE-producing plasma cells.
The detection of allergen-specific IgE antibodies in intestinal washings in food-intolerant patients with both negative SPTs and food-specific serum IgE antibodies has been interpreted as the result of a strictly local IgE synthesis (38). In contrast, there is some support for the view that the whole mucosal immune system is involved in patients with atopic diseases (40). Moreover, local intestinal IgE production was found to be unlikely involved to any large extent, because IgE-positive B cells represented less than 2% of intestinal Ig-producing cells (41). Further, serum IgE concentrations have been found to be associated with the number of basophil IgE-receptors (42). In agreement with these observations, we found that the number of duodenal mucosal IgE-positive cells was correlated with IgE levels in blood, suggesting a systemic IgE production. This is true also in the patients with gastrointestinal complaints. Our data of IgE immunoreactive cells in the duodenal mucosa in the absence of positive SPT or allergen-specific IgE antibodies do not exclude a strictly local production of IgE. Alternatively, these findings may be explained by the poor accuracy of immunologic tests.
Our study indicates that occurrence of cutaneous, gastrointestinal, and respiratory symptoms after food intake is associated with IgE-mediated reactions in the duodenal mucosa. We found that duodenal IgE-positive cells had a high but imperfect diagnostic accuracy which was comparable to that of total serum IgE, SPT, and food-specific IgE antibodies. Thus, our results confirm that an allergen elimination diet followed by food challenge is the most accurate means of diagnosing food allergy. However, we found increased IgE-containing cells in all delayed reactors despite the fact that one-third had negative immunologic tests. Baehler et al. (22) found that no patients with delayed reactions to cow's milk challenge had positive SPTs or specific serum IgE antibodies. A larger study is required to establish whether our findings in the delayed reactor group may be of diagnostic value.
Abbreviations
- SPT:
-
skin prick test
REFERENCES
Niggemann B, Wahn U, Sampson HA 1994 Proposals for standardization of oral food challenge tests in infants and children. Pediatr Allergy Immunol 5: 11–13
Hill DJ, Hosking CS 1996 Cow milk allergy in infancy and early childhood. Clin Exp Allergy 26: 243–246
Bock SA, Atkins FM 1990 Patterns of food hypersensitivity during sixteen years of double-blind placebo-controlled food challenge. J Pediatr 17: 561–567
Bahna SL, Gandhi MD 1987 Reliability of skin testing and RAST in food allergy diagnosis. In: Chandra RK (ed) Food Allergy. Nutrition Research Foundation, St. John's Newfoundland, Canada, 139–147.
Patterson S, Roebuck P, Platts-Mills TAE, Shiner M, Kingston D, Pearson JR 1981 IgE plasma cells in human jejunum demonstrated by immunoelectron microscopy. Clin Exp Immunol 46: 301–304
Savilahti E 1973 Immunohistochemical study of the malabsorption syndrome with cow's milk intolerance. Gut 4: 491–501
Rosekrans PCM, Meijer CJLM, Cornelisse CJ, Udwall AM, Lindeman J 1980 Use of morphometry and immunohistochemistry of small intestinal biopsy specimens in the diagnosis of food allergy. J Clin Pathol 33: 125–130
Schrander JJP, Dellevoet JJPF, Arends JW, Forget PP, Kuijten R 1992 Small intestinal mucosa IgE plasma cells and anti-cow milk IgE in children with cow milk protein intolerance. Ann Allergy 70: 406–409
Shiner M, Ballard J, Smith ME 1975 The small-intestinal mucosa in cow's milk allergy. Lancet 1: 136–139
Perkkio M 1980 Immunohistochemical study of intestinal biopsies from children with atopic eczema due to food allergy. Allergy 35: 573–580
Perkkio M, Savilahti E, Kuitunen P 1981 Morphometric and immunohistochemical study of jejunal biopsies from children with intestinal soy allergy. Eur J Pediatr 137: 63–69
Burks WA, Sampson HA 1992 Diagnostic approaches to the patient with suspected food allergies. J Pediatr 121: S64–S71
Consensus Conference 1989 Interpretazione delle indagini immuno-allergologiche per la diagnosi delle allergopatie respiratorie infantili da inalanti. Riv Immunol Allergy Pediatr 2: 37–49
McLean IW, Nakane PK 1974 Periodate-lysine-paraformaldehyde fixative. A new fixation for immunoelectron microscopy. J Histochem Cytochem 22: 1077–80
Feltkamp-Vroom TM, Stallman PJ, Aalberse RC, Reerink-Brongers EE 1975 Immuofluorescence studies on renal tissue, adenoids, nasal polyps and skin of atopic and non-atopic patients with special reference to IgE. Clin Immunol Immunopathol 4: 392–404
Galen RS, Gambino SR 1975 Beyond Normality: The Predictive Value and Efficiency of Medical Diagnoses. John Wiley & Sons, New York
Cavagni G, Capra T, Suzzani L, Nori G, Lapetina F, Deriu FM, Dusi R, Bernasconi S 1980 Valori di IgE in bambini sani non atopici. Folia Allergol Immunol Clin 27: 273–280
Brandtzaeg P, Baklien K 1976 Inconclusive immunohistochemistry of human IgE in mucosal pathology. Lancet 1: 1297–1298
Rognum TO, Brandtzaeg P 1989 IgE-positive cells in human intestinal mucosa are mainly mast cells. Int Arch Allergy Appl Immunol 89: 256–260
Young E, Stoneham MD, Petruckevitch A, Barton J, Rona A 1994 A population study of food intolerance. Lancet 343: 1127–1130
Sampson HA, Ho DG 1997 Relationship between food-specific IgE concentrations and the risk of positive food challenges in children and adolescents. J Allergy Clin Immunol 100: 444–451
Baehler P., Chad Z, Gurbindo C, Bonin AP, Bouthillier L, Seidman EG 1996 Distinct patterns of cow's milk allergy in infancy defined by prolonged, two-stage double-blind, placebo-controlled food challenges. Clin Exp Allergy 26: 254–261
Hill DJ, Duke AM, Hosking CS, Hudson IL 1988 Clinical manifestations of cow's milk allergy in childhood. The diagnostic value of skin test and RAST. Clin Allergy 5: 481–490
Niggemann B, Beyer K, Wahn U 1994 The role of eosinophils and eosinophil cationic protein in monitoring oral challenge tests in children with food-sensitive atopic dermatitis. J Allergy Clin Immunol 94: 963–971
Kaiosaari M 1982 Food allergy in Finnish children aged 1 to 6 years. Acta Paediatr Scand 71: 815–819
Bock SA 1987 Prospective appraisal of complaints of adverse reactions to foods in children during the first 3 years of life. Pediatrics 79: 683–688
McCalla R, Savilahti E, Perkkio M, Kuitunen P, Backman A 1980 Morphology of the jejunum in children with atopic eczema due to food allergy. Allergy 35: 563–571
Kuitunen P, Visakorpi JK, Savilahti E, Pelkonen P 1975 Malabsorption syndrome with cow's milk intolerance. Clinical findings and course in 54 cases. Arch Dis Child 50: 351–356
Walker-Smith J, Harrison M, Kilby A, Phillips A, France N 1973 Cow's milk-sensitive enteropathy. Arch Dis Child 53: 375–380
Fontaine JL, Navarro J 1975 Small intestinal biopsy in cow's milk protein allergy in infancy. Arch Dis Child 50: 357–362
Paganelli R, Levinsky RJ, Brostoff J, Wraith DG 1979 Immune complexes containing food proteins in normal and atopic subjects after oral challenge and effect of sodium cromoglycate on antigen absorption. Lancet 1: 1270–1272
Paganelli R, Atherton DJ, Levinsky RJ 1983 Differences between normal and milk allergic subjects in their immune responses after milk ingestion. Arch Dis Child 58: 201–206
Dupont C, Barau E, Molkhou P, Raynaud F, Barbet JP, Dehennin L 1989 Food-induced alterations of intestinal permeability in children with cow's milk-sensitive enteropathy and atopic dermatitis. J Pediatr Gastroenterol Nutr 8: 459–465
Caffarelli C, Cavagni G, Menzies IS, Bertolini P, Atherton DJ 1993 Elimination diet and intestinal permeability in atopic eczema: a preliminary study. Clin Exp Allergy 23: 28–31
Reimann HJ, Lewin J 1988 Gastric mucosal reactions in patients with food allergy. Am J Gastroenterol 83: 1212–1219
Crowe SE, Perdue MH 1992 Gastrointestinal food hypersensitivity: basic mechanisms of pathophysiology. Gastroenterology 103: 1075–1095
Sasai K, Furukawa S, Sugarawa T, Kaneko K, Baba M, Yabuta K 1992 IgE levels in faecal extracts of patients with food allergy. Allergy 47: 594–598
Marcucci F, Sensi LG, Bizzarri G 1985 Specific IgE to food and inhalant allergens in intestinal washings of children affected by atopic eczema. Clin Allergy 15: 195–202
Majamaa H, Miettinen A, Laine S, Isolauri E 1996 Intestinal inflammation in children with atopic eczema: faecal eosinophil cationic protein and tumour necrosis factor-α as non-invasive indicators of food allergy. Clin Exp Allergy 26: 181–187
Wallaert B, Desremaux P, Copin MC, Tillie I, Bernard A, Colombel JF, Gosselin B, Tonnel AB, Janin A 1995 Immunoreactivity for interleukin 3 and 5 and granulocyte/Macrophage colony-stimulating factor of intestinal mucosa in bronchial asthma. J Exp Med 182: 1897–1904
Brown WR, Borthistle BK, Chen ST 1975 Immunoglobulin E (IgE) and IgE-containing cells in human gastrointestinal fluids and tissues. Clin Exp Immunol 20: 227–237
Malvaux FJ, Conroy MC, Adkinson NF Jr, Lichtenstein LM 1978 IgE receptors on human basophils. J Clin Invest 62: 176–181
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Caffarelli, C., Romanini, E., Caruana, P. et al. Clinical Food Hypersensitivity: The Relevance of Duodenal Immunoglobulin E-Positive Cells. Pediatr Res 44, 485–490 (1998). https://doi.org/10.1203/00006450-199810000-00004
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199810000-00004
This article is cited by
-
Potential effector and immunoregulatory functions of mast cells in mucosal immunity
Mucosal Immunology (2015)
-
Intestinal allergic inflammation in birch pollen allergic patients in relation to pollen season, IgE sensitization profile and gastrointestinal symptoms
Clinical and Translational Allergy (2014)
-
Clinical Spectrum of Food Allergies: a Comprehensive Review
Clinical Reviews in Allergy & Immunology (2014)
-
Food-induced anaphylaxis: mast cells as modulators of anaphylactic severity
Seminars in Immunopathology (2012)