Abstract
Background
Ascribing food allergy diagnosis to patients who are not allergic is well described, but its implications on oral immunotherapy (OIT) have not been studied. The aim was to study non-allergic patients referred for OIT.
Methods
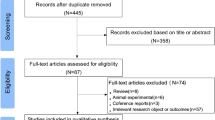
All patients who began OIT at Shamir Medical Center between November 2015 and August 2020 were included. Medical records were reviewed, and skin prick tests (SPT) and/or specific IgE were measured. Patients were challenged to the index food. Allergic and non-allergic patients were compared.
Results
A total of 1073 patients were studied (milk, n = 327; egg, n = 41; peanut, n = 272; sesame, n = 130; and tree nuts, n = 303) and 87 (8.1%) were found non-allergic (milk, n = 21; egg, n = 6; sesame, n = 5; peanut, n = 29; tree nuts, n = 26). Predictors of being not allergic were no previous reaction to the index food (OR = 3.3, p = 0.001), not having asthma (OR = 2.4, p = 0.001), or HDM sensitization (OR = 2.0, p = 0.007), male sex (OR = 2.3, p = 0.004), and a smaller SPT wheal size (OR = 1.5, p < 0.001).
Conclusions
A substantial number of patients referred for OIT are mislabeled with food allergy, suffer from unjustly food limitations and impairments in quality of life, and “take up” OIT places of true allergic patients. Awareness of OIT centers to this phenomenon is important.
Impact
-
A significant number (8.1%) of patients referred for OIT are found not allergic to the food they intended to treat.
-
This study characterizes non-allergic patients referred for OIT (a lack of previous reaction to the index food, a smaller or negative SPT wheal size, and less atopic co-morbidities) and discusses the implications of such referrals.
-
Increased awareness by OIT centers to potential non-allergic patients referred for OIT is required, including screening of patients before treatment initiation, to minimize unnecessary treatments of non-allergic patients.
Similar content being viewed by others
Introduction
Food allergy is a worldwide major public health problem, having a detrimental effect on both patients and society on a personal, social, and economic level.1,2,3 Oral immunotherapy (OIT) has become an effective alternative treatment for food allergic patients.4,5,6,7 In many areas of the world, OIT is largely provided by specialists in the field of food allergy, and its availability is far from matching the high demand for the treatment, leading to long waiting times. In light of the recent approval of a peanut OIT product by the Food and Drug Administration, OIT is likely to be offered by an increasing number of centers.7,8 With the lack of unifying guidelines, criteria for patient selection might vary between centers, increasing the odds of non-allergic patients entering OIT.
An OIT treatment program was initiated at the Institute of Allergy, Immunology and Pediatric Pulmonology at Shamir (formerly Assaf-Harofeh) Medical Center in 2010. The Center provides OIT to patients with allergies to milk, egg, peanuts, sesame, and tree nuts (walnut–pecan, cashew–pistachio, hazelnut, and almond), as previously described.9,10,11,12 The OIT program functions as a referral center for patients from all over Israel with an average waiting time of 3 years. Most patients arriving for OIT are diagnosed and followed by local allergists and are referred to our center specifically for the treatment. All patients undergo an oral food challenge (OFC) at the beginning of OIT, and those who pass the challenge are excluded. Systematic documentation of non-allergic patients began in 2015. The aim of the current study was to identify patients who were referred for OIT, but who were subsequently found to be non-allergic to that particular food, describe the rate of this phenomenon, and patient characteristics, and to identify factors distinguishing them from allergic patients.
Methods
Patients
All patients who began OIT at Shamir Medical Center between November 2015 and August 2020 were included. Patients arriving for OIT were required to provide an updated referral letter (within the past year) from their allergist, including documentation of previous reactions and OFCs performed, and the results of skin prick tests (SPTs) and/or serum immunoglobulin E (sIgE) to the respective foods. Medical records were reviewed, and data were collected on demographics, allergic co-morbidities (including atopic dermatitis, asthma, and house dust mite (HDM) sensitization), previous allergic reactions, and results of SPT and/or specific sIgE measurements. Patients referred for the treatment of milk, egg, peanut, or sesame allergy underwent their evaluation during the first week of OIT. Patients who were referred for the treatment of tree nut allergy were invited for an evaluation, including SPTs and OFCs, before starting OIT, to diagnose allergy vs. sensitization to the various tree nuts and to determine which tree nut is to be treated first. Approval for the documentation and publication of all patient data was obtained from the Helsinki institutional review board committee.
Patient evaluation
Patients were evaluated in our clinic by a specialized allergist and underwent SPTs to the index food. A graded OFC is performed during the first week of OIT regardless of sensitization level or a history of previous reactions (Supplementary Methods, Table S1). In the case of tree nuts, patients are evaluated prior to OIT with multiple OFCs to the different tree nuts (walnut–pecan, cashew–pistachio, hazelnut, and almonds), based on their medical history, sensitization level, and previous reactions, to elucidate the allergic status of each nut (Table S2). Patients with pecan and pistachio allergy were all allergic to their cross-reactive nuts (walnut and cashew, respectively) and these pairs of nuts were thus included together. Patients with no reaction to the final dose of the OFC (milk, 3600 mg protein; peanut, 3000 mg; egg, 6000 mg; sesame, 4000 mg; and tree nuts, 2500–4200 mg) are considered non-allergic.13 These patients are instructed to consume the index food at home for a at least a month before their OIT slot is canceled. In the case of tree nuts, only patients who completed all tree nut challenges without an allergic reaction were considered non-allergic to tree nuts.
Skin prick tests
SPTs were performed on the volar surface of the forearm and read after 15–20 min (Supplementary Methods). A “highly positive” SPT was defined as either a wheel diameter ≥95% positive predictive value (PPV) (milk 8 mm, egg 7 mm, peanut 8 mm, walnut 8 mm, cashew 8 mm) or, in the absence of a 95% PPV value, as the optimal cutoff on receiver operating characteristic (ROC) curve, based on Youden’s index (hazelnut 8 mm) for the respective food.14,15,16,17 A cutoff of 8 mm was used for sesame as well. SPT values ≥3 mm and less than the level providing 95% PPV were defined as an intermediate range. Almond SPT values ≥3 mm were defined as an intermediate range.
Statistical analysis
Statistical analysis was done using the SPSS-20 software. Comparisons were made between allergic and non-allergic patients using the chi-square test (or Fisher’s exact test) for categorical variables and Mann–Whitney test for continuous variables. Variables found to differ significantly between allergic and non-allergic patients on univariate analysis were inserted into a multivariable logistic regression analysis. Significance was determined when p value was <0.05.
Results
Study population
A total of 1073 patients performed OFCs to various foods before starting OIT and were included in the analysis. The foods challenged were milk, n = 327; egg, n = 41; peanut, n = 272; sesame, n = 130; and tree nuts, n = 303 (walnut–pecan, n = 194; cashew–pistachio, n = 82; hazelnut, n = 23; almond, n = 4). Median (interquartile range (IQR)) patients’ age was 7 (5.5–10) years and 657 patients (61.2%) were males. Asthma was diagnosed in 512 (47.7%) and 776 patients (72.3%) were sensitized to HDM. While an anaphylactic reaction to the index food, or to a cross-reactive nut (walnut–pecan or cashew–pistachio) in the case of tree nuts, was reported by most patients (n = 601, 56%), and while 375 (34.9%) reported a previous use of injectable epinephrine for such reactions, 83 (7.7%) patients had no history of a previous reaction to the index food. Seventeen patients had a negative SPT upon arrival to OIT (Table 1).
Allergic vs. non-allergic patients
Eighty-seven patients (8.1%) concluded their OFCs without an allergic reaction and were deemed non-allergic (milk, n = 21; egg, n = 6; sesame, n = 5; peanut, n = 29; tree nuts, n = 26 (walnut–pecan, n = 11; cashew–pistachio, n = 8; hazelnut, n = 5; almond, n = 2)). The median age of allergic and non-allergic patients was comparable (Table 1). More males were represented in the non-allergic group (p = 0.004). The rate of non-allergic patients for the different foods ranged from 3.8% for sesame to 14.3% for egg (Fig. 1) and, in tree nuts, from 5.7% for walnut–pecan to 50% for almond (Fig. S1). The rate of non-allergic patients in foods considered to have high spontaneous resolution rates (milk and egg) vs. those with low spontaneous resolution (sesame, peanut, tree nuts) was not significantly different (p = 0.29). Both asthma and HDM sensitization were less common in non-allergic patients compared to allergic ones.
A history of previous reactions in allergic and non-allergic patients
A previous reaction to the index food was reported in all patients referred for milk OIT, but no reaction was documented in 7.3% of patients in the case of egg, 3.7% of peanut, 4.6% of sesame, and 21.1% of tree nuts-challenged patients (walnut–pecan 21.1%, cashew–pistachio 17.1%, hazelnut 30.4%, and almond 50%, (Figs. 2 and S2). A previous reaction (p = 0.005), anaphylactic reactions (p = 0.006), and reactions treated with injectable epinephrine (p = 0.002) were significantly less frequent in non-allergic patients (Table 1). In seven of these patients, the reaction described was either on skin contact with the index food or involved minor perioral symptoms. All patients referred for milk, egg, and sesame OIT, who were found to be non-allergic, had a history of previous reactions to these foods. In contrast, 13.8 and 38.5% of those found not allergic to peanut or tree nuts, respectively, had no previous reactions (Fig. 2). These rates for the various tree nuts are shown in Fig. S2. The median age of last reaction to each food in non-allergic patients ranged from 2 years (egg) to 13 years (sesame) and included patients whose last reaction occurred at age ≤1 year for each of the foods studied (Tables S3 and S4). The characteristics of previous reactions (age at first and last reactions and organ system involved) in these patients are shown in Tables S3 and S4.
SPTs in allergic and non-allergic patients
SPTs were significantly smaller in the non-allergic group (p < 0.001) (Table 1). Seventeen patients who arrived for OIT had a negative SPT to the target food (milk, n = 1; egg, n = 4; sesame, n = 1; peanut, n = 4; tree nuts, n = 7). Of those, 16 were non-allergic and 1 was allergic to sesame. Additional 448 patients had SPTs in the mid-range, and 608 had highly positive SPTs for their respective foods (Figs. 3 and S3). Of the group of patients with highly positive SPTs, 3.9% were found to be non-allergic (milk, 5.1%; egg, 7.7%; sesame, 1.4%; peanut, 5.1%; and tree nuts, 2.6% (walnut–pecan, 2.7%; cashew–pistachio, 1.5%; hazelnut, 8.3%)). Of the patients with SPTs in the mid-range, 10.5% were non-allergic (milk, 7.1%; egg, 4.2%; sesame, 6.8%; peanut, 17.8%; and tree nuts, 13.2%, (walnut–pecan, 8.8%; cashew–pistachio, 23.1%; hazelnut, 30%; almond, 33.3%). An algorithm demonstrating the breakdown of allergic and non-allergic patients based on a history of previous reaction and sensitization level is shown in Fig. 4. Most patients with a highly positive SPT, regardless of a positive or negative history of a previous reaction (96.9 and 94.5%, respectively) were allergic. Nearly all patients with a negative SPT, regardless of a history of a previous reaction, were non-allergic. In patients with intermediate SPT, the rate of non-allergic patients was 10.2% in cases where a history of a previous reaction was documented and reached 32% if no such history was present (Fig. 4).
Allergic vs. non-allergic patients on multivariate analysis
Comparing allergic and non-allergic patients using a logistic regression analysis, no history of a previous reaction to the index food was the strongest predictor for no allergy (odds ratio (OR) = 3.3), followed by lack of asthma (OR = 2.4), male sex (OR = 2.3), no HDM sensitization (OR = 2.9), and a smaller SPT wheal size (OR = 1.5), (Table 2). Twenty-nine patients in the non-allergic group had a food allergy to a different food from the one they intended to treat, and 16 started OIT for that food.
Discussion
In the current study, 8.1% of patients who were referred by allergists for OIT to a specific food allergy following a recent evaluation by an allergist were found to be non-allergic to that food. While there were differences in the rate of non-allergic patients between the various foods, there was no significant difference between food allergies that typically resolve (milk and egg) and those that typically persist (sesame, peanut tree nuts). Characteristics of non-allergic patients included fewer cases of previous reactions to the suspected food, particularly for peanut and tree nuts, a smaller SPT wheal size, less atopic co-morbidities (asthma and HDM sensitization), and male sex.
While several practice guidelines for OIT have been published, significant differences exist between centers.6,18,19,20,21 For example, in a recent European review, 98% of centers reported that they challenge patients before starting OIT.22 In contrast, in a US survey, only 52.6% of academic centers and 47.3% of non-academic centers reported challenging patients before OIT.23 With its growing demand, and increased availability of commercial products, OIT will likely be offered by an increasing number of centers in the near future. While not having to challenge every patient might simplify the treatment and increase its availability, confirming the diagnosis of food allergy before OIT is important from several aspects (Table S5). First, OIT is challenging, requiring daily dose consumption under specific limitations, associated with adverse reactions, some severe, and may temporarily impair quality of life.24,25 Second, OIT in many centers is not covered by health care insurances.22 Third, treating a food that a multiple food allergic patient is not actually allergic to would delay treatment of a true food allergy. Fourth, non-allergic individuals take up places of allergic patients awaiting OIT. The current study demonstrates that the rate of non-allergic patients referred by allergists for OIT is not negligible, despite a specialist follow-up visit in proximity to OIT. Ideally, these patients should be identified before entering OIT.
Surprisingly, a previous reaction to the target food was not experienced by 7.7% of our patients and those were referred for OIT, rather than an OFC. Patients who had no history of a previous reaction to the suspected food were diagnosed based on sensitization only. Those who were ultimately found to be not allergic might have not been allergic at all and perhaps suffered from unnecessary elimination diet. Potentially, some allergic patients with no history of a previous reaction might not have been allergic initially but rather developed allergy following elimination diet.26,27 All those who were found not allergic to milk, egg, and sesame reported previous reactions, likely representing natural food allergy resolution, which was missed. A remote last reaction, particularly in food allergies with high spontaneous resolution rates, should prompt such investigation.
Another predictor of non-allergic patients was the SPT. Seventeen patients were referred for OIT with a negative SPT (sIgE is not routinely obtained in Israel). This could suggest that allergists prefer that the evaluation be made at the OIT center, even when an OFC is clearly indicated. Many patients referred to treatment had SPTs that were intermediate in size. Moreover, commercially available SPTs for certain foods (tree nuts, sesame) have no published 95% PPV values.16,17 The rate of patients with intermediate size SPT who were found not allergic was 10.5%, ranging from as low as 4.2% for egg to 30% for hazelnut. The decision on whether or not to challenge these patients before starting OIT depends on the specific food, the patient’s age, and the interval from the previous reaction, but should not be overlooked.
Asthma and HDM sensitization were significantly less common in non-allergic patients, similar to previous reports.28 In addition, while several studies reported a male sex preponderance in food allergic patients, male sex in our study was more representative in those who were non-allergic.29,30 Importantly, nearly a third of the non-allergic patients in our study did have a food allergy to a different food, limiting these observations.
This study has several limitations. First, being a retrospective study, the information collected was limited to the data available in the medical records. As a result, data regarding atopic dermatitis was unattainable for a considerable number of our patients. Second, our patients reflect a selected group, enrolled from a single center, and may not necessarily represent food allergic patients referred for OIT in other centers or countries.
In summary, many patients referred for OIT are found not allergic to the food they intended to treat. While food allergy mislabeling is a well-known entity, the current study emphasizes that this phenomenon occurs even in patients followed regularly by allergists and referred for OIT. Some of these patients likely represent spontaneous resolution of food allergy while others potentially were not allergic to begin with. These patients unjustly suffer from food limitations and quality-of-life impairments associated with food allergy and will be unnecessarily subjected to the challenges of OIT if not challenged before. Also, these patients take up OIT places of truly allergic patients. Allergists should be aware of this phenomenon and be proactive in the evaluation of patients prior to OIT referral.
Data availability
Additional data regarding the current study are available from the corresponding author on reasonable request.
References
Gupta, R. et al. The economic impact of childhood food allergy in the United States. JAMA Pediatr. 167, 1026–1031 (2013).
Allen, C. W., Bidarkar, M. S., vanNunen, S. A. & Campbell, D. E. Factors impacting parental burden in food-allergic children. J. Paediatr. Child Health 51, 696–698 (2015).
Cummings, A. J., Knibb, R. C., King, R. M. & Lucas, J. S. The psychosocial impact of food allergy and food hypersensitivity in children, adolescents and their families: a review. Allergy 65, 933–945 (2010).
Anagnostou, K. et al. Assessing the efficacy of oral immunotherapy for the desensitization of peanut allergy in children (STOP II): a phase 2 randomized controlled trial. Lancet 383, 1297–1304 (2014).
Nurmatov, U. et al. Allergen immunotherapy for IgE-mediated food allergy: a systematic review and meta-analysis. Allergy 72, 1133–1147 (2017).
Pajno, G. B. et al. EAACI guidelines on allergen immunotherapy: IgE-mediated food allergy. Allergy 73, 799–815 (2018).
Vickery, B. P. et al. AR101 oral immunotherapy for peanut allergy. PALISADE Group of Clinical Investigators. N. Engl. J. Med. 379, 1991–2001 (2018).
Traister, R. S., Green, T. D., Mitchell, L. & Greenhawt, M. Community opinions regarding oral immunotherapy for food allergies. Ann. Allergy Asthma Immunol. 109, 319–323 (2012).
Elizur, A. et al. Clinical and laboratory 2-year outcome of oral immunotherapy in patients with cow’s milk allergy. Allergy 71, 275–278 (2016).
Nachshon, L., Goldberg, M. R., Katz, Y., Levy, M. B. & Elizur, A. Long-term outcome of peanut oral immunotherapy – real life experience. Pediatr. Allergy Immunol. 29, 519–526 (2018).
Nachshon, L. et al. Efficacy and safety of sesame oral immunotherapy - a real-world, single center study. J. Allergy Clin. Immunol. Pract. 7, 2775.e2–2781.e2 (2019).
Elizur, A. et al. Single walnut oral immunotherapy for desensitizing walnut and additional tree-nut allergies: a prospective cohort study (Nut CRACKER study). Lancet Child Adolesc. Health 3, 312–321 (2019).
Niggemann, B. When is an oral food challenge positive? Allergy 65, 2–6 (2010).
Appel, M. Y. et al. Evaluation of the basophil activation test and skin prick testing for the diagnosis of sesame food allergy. Clin. Exp. Allergy 48, 1025–1034 (2018).
Elizur, A. et al. NUT Co Reactivity - ACquiring Knowledge for Elimination Recommendations (NUT CRACKER) study. Allergy 73, 593–601 (2018).
Sporik, R., Hill, D. J. & Hosking, C. S. Specificity of allergen skin testing in predicting positive open food challenges to milk, egg and peanut in children. Clin. Exp. Allergy 30, 1540–1546 (2000).
McWilliam, V. et al. Skin prick test predictive values for the outcome of cashew challenges in children. J. Allergy Clin. Immunol. Pract. 8, 141.e2–148.e2 (2020).
Bégin, P. et al. CSACI guidelines for the ethical, evidence-based and patient-oriented clinical practice of oral immunotherapy in IgE-mediated food allergy. Allergy Asthma Clin. Immunol. 16, 20 (2020).
Martorell, A. et al. Immunotherapy Egg and Milk Spanish Guide (ITEMS Guide). Part I: cow milk and egg oral immunotherapy: introduction, methodology, rationale, current state, indications, contraindications, and oral immunotherapy build-up phase. J. Investig. Allergol. Clin. Immunol. 27, 225–237 (2017).
Ebisawa, M. et al. Japanese guidelines for food allergy 2020. Allergol. Int. 69, 370–386 (2020).
Pajno, G. B. et al. Allergen-specific Immunotherapy panel of the Italian Society of Pediatric Allergy and Immunology (SIAIP). Clinical practice recommendations for allergen-specific immunotherapy in children: the Italian consensus report. Ital. J. Pediatr. 43, 13 (2017).
Rodríguez Del Río, P. et al. Food immunotherapy practice: nation differences across Europe, The FIND project. Allergy https://doi.org/10.1111/all.15016 (2021).
Greenhawt, M. J. & Vickery, B. P. Allergist-reported trends in the practice of food allergen oral immunotherapy. J. Allergy Clin. Immunol. Pract. 3, 33–38 (2015).
Rigbi, N. E. et al. Changes in patient quality of life during oral immunotherapy for food allergy. Allergy 72, 1883–1890 (2017).
Nachshon, L. et al. Patient characteristics and risk factors for home epinephrine-treated reactions during oral immunotherapy for food allergy. J. Allergy Clin. Immunol. Pract. 9, 185.e3–192.e3 (2021).
Elizur, A., Bollyky, J. B. & Block, W. M. Elimination diet and the development of multiple tree-nut allergies. Pediatr. Res. 82, 671–677 (2017).
Du Toit., G. et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N. Engl. J. Med. 372, 803–813 (2015).
Hill, D. A., Grundmeier, R. W., Ram, G. & Spergel, J. M. The epidemiologic characteristics of healthcare provider-diagnosed eczema, asthma, allergic rhinitis, and food allergy in children: a retrospective cohort study. BMC Pediatr. 16, 133 (2016).
Nachshon, L. et al. The prevalence of food allergy in young Israeli adults. J. Allergy Clin. Immunol. Pract. 7, 2782.e4–2789.e4 (2019).
Liu, A. H. et al. National prevalence and risk factors for food allergy and relationship to asthma: results from the National Health and Nutrition Examination Survey 2005-2006. J. Allergy Clin. Immunol. 126, 798.e13–806.e13 (2010).
Acknowledgements
We would like to thank Hasia Duani and Tehila Abargil for coordinating the patient clinical visits and to Keren Golobov, Mor Carmel, and Michal Noah Tal for assisting with OFC performance.
Funding
This study was self-supported. M.R.G. is funded by a Kamea grant from the Ministry of Health, Israel.
Author information
Authors and Affiliations
Contributions
All authors have met the Pediatric Research authorship requirements. Y.K.: conceptualization (equal); investigation (lead); writing original draft (equal); review and editing (equal). L.N.: investigation (supporting); review and editing (equal). M.R.G.: investigation (supporting); review and editing (equal). M.B.L.: investigation (supporting); review and editing (equal). N.E.-R.: investigation (supporting); review and editing (equal). A.E.: conceptualization (equal); investigation (supporting); formal analysis (lead); writing original draft (equal); review and editing (equal).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Patients’ consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Koren, Y., Nachshon, L., Goldberg, M.R. et al. Characteristics of patients diagnosed as non-allergic following food allergy oral immunotherapy referral. Pediatr Res 93, 643–648 (2023). https://doi.org/10.1038/s41390-022-02119-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02119-3