Abstract
Kawasaki syndrome (KS) has been reported to be associated with selective expansion of Vβ2+ T cells and either staphylococcal toxic shock syndrome toxin-1 or streptococcal pyrogenic exotoxin C in uncomplicated cases. However, there have been no previous studies on the role of superantigens in KS associated with coronary artery disease, the major complication of this illness. The present study characterized bacteria isolated from three acute KS patients who developed coronary artery disease. Staphylococcus aureus secreting either TSST-1 (n = 3) or exfoliative toxin A(n = 1), both known to stimulate expansion of Vβ2+ T cells, were isolated from all three patients. The percent Vβ2+ T cells was determined in three patients with coronary artery disease. On presentation, one patient demonstrated reduction, whereas the other two showed expansion, of Vβ2+ T cells. Repeat analyses of the latter two children showed their percent Vβ2+ T cells to decrease toward normal. These observations suggest that coronary artery disease in KS may result from superantigenic stimulation of Vβ2+ T cells. This is also the first demonstration of an association of staphylococcal exfoliative toxin with acute KS. The observation that three different bacterial toxins associated with KS are potent activators of Vβ2+ T cells suggests an important role for this T cell subset in the pathogenesis of this autoimmune disease.
Similar content being viewed by others
Main
KS is an acute multisystem vasculitis that affects infants and young children(1–3). Although the symptoms of this illness are generally self-limited, coronary artery abnormalities can develop in up to 25% of untreated patients. The introduction of high dose i.v. immune globulin treatment, within the first 10 d after onset of fever, has significantly reduced the prevalence of coronary artery abnormalities in KS(4). Early recognition and prompt treatment is therefore critical. Unfortunately the current definition of acute KS is based on diagnostic criteria that use clinical features that overlap with other illnesses and create diagnostic dilemmas in atypical cases, which do not completely fulfill the diagnostic criteria of KS but are associated with the development of coronary artery disease(5). The development of an objective diagnostic test as well as more effective therapy for KS requires identification of the etiologic agent.
The clinical symptoms and epidemiology of S are highly suggestive of an infectious disease, overlapping with staphylococcal and streptococcal scarlet fevers and toxic shock syndromes. Several investigators have suggested that both of these genera of bacteria contribute to KS, but this remains controversial(6–9). Of particular note, Leung et al.(10) suggested that staphylococcal TSST-1 and streptococcal pyrogenic exotoxins may contribute to KS. In that blinded controlled study, 13/16 KS patients without coronary artery disease were infected or colonized with TSST-1 (n = 11) or streptocccal pyrogenic exotoxin (n = 2) producing organisms compared with only 1/15 age-matched children with other febrile illnesses. These investigators proposed that TSST-1-producing and progenic exotoxin-producing streptococci could account for the selective expansion of Vβ2-expressing T cells in the blood and tissues of patients with acute KS now reported by three independent groups(11–15).
Although the clinical features of acute KS can overlap with a number of other infectious illnesses, the finding of coronary artery abnormalities is thought to be specific for KS. There have been no prospective studies examining the peripheral blood T cell repertoire or the role of superantigen-producing bacteria in KS complicated by coronary artery disease. Such studies are difficult to do now because treatment with i.v. immune globulin has significantly reduced the prevalence of coronary artery disease caused by KS. The purpose of this report is to provide a detailed clinical, microbiologic, and T cell Vβ2 analysis of several patients with KS complicated by coronary artery abnormalities.
METHODS
Subjects. This study was conducted on three patients with acute KS complicated by coronary artery aneurysms documented by angiography and/or two-dimensional echocardiography (see “Results”). All patients with KS fulfilled the established American Heart Association criteria for diagnosis of acute KS, or atypical KS, as determined by their treating physicians(5, 16).
Isolation and characterization of bacteria. Bacterial cultures were obtained with cotton swabs from the pharynx, rectum, and in one case a tracheal aspirate (see case report 2 below). Swabs from the various sites were cultured overnight at 37 °C on sheep blood agar plates, except for swabs from the rectum, which were also plated on phenylethyl alcohol sheep blood agar. All coagulase-positive Staphylococcus aureus isolates were screened for secretion of TSST-1, exfoliative toxins, and staphylococcal enterotoxins by serial dilution double immunodiffusion as previously described(17, 18).
Assessment of peripheral blood T cell repertoire. Peripheral blood mononuclear cells were isolated from heparinized blood by Ficoll-Hypaque density gradient centrifugation. T cell receptor Vβ repertoire on freshly isolated peripheral blood mononuclear cells were assessed by two- or three-color immunofluorescence on a FACScan flow cytometer (Becton Dickinson immunocytometry systems) using FITC, phycoerythrin, and peridinin chlorophyll protein as the three fluorescent parameters as previously described(11). List mode multiparameter data files (each file with forward scatter, side scatter, and three fluorescent parameters) were analyzed using the LYSIS II Windows program. Negative control reagents were used to verify the staining specificity of antibodies. The percentage of T cells bearing each T cell receptor Vβ phenotype was expressed as a percentage of total T (CD3+) cells.
RESULTS
Patient 1. This was a 7-mo-old black male infant, with a history of multiple arterial aneurysms secondary to KS, readmitted to Wesley Medical Center in Wichita, Kansas, with a diagnosis of recurrent KS. At 2 mo of age, this child was diagnosed as having atypical KS due to the development of arterial aneurysms of the left main (diameter = 5.4 mm), left anterior descending (5.0 mm), and right circumflex (3.0 mm) coronary arteries after suffering 18 d of high fever, conjunctivitis, diffuse maculopapular rash, cracked swollen lips, and oral mucosal lesions. The patient had received i.v. immune globulin therapy and was maintained on aspirin after discharge. He was readmitted at 3 mo of age for management of congestive heart failure due to pericardial effusion with moderate tricuspid and mitral insufficiency. In addition to his various aneurysms involving the left main (diameter = 6.5 mm), left anterior descending (6.0 mm), and right circumflex (5.0 mm) coronary arteries, it was noted at this time that he had developed aneurysms of the iliac, superior mesenteric, axillary, and renal arteries. During this second hospitalization, he was heparinized and treated three times with high dose i.v. immune globulin (2 g/kg). He was discharged on coumadin and aspirin therapy.
During the current admission, at 7 mo of age, this patient presented with a 7-d history of fever up to 103 °F, diffuse maculopapular rash, conjunctivitis, swollen cracked lips, erythema of the pharynx and buccal mucosa, and erythematous induration of the hands and feet. His echocardiogram revealed that his coronary artery aneurysms had enlarged. His left main coronary artery was 8.1 mm in diameter; the left anterior descending, 5.0 mm diameter; and right circumflex coronary artery, 5.0 mm diameter. The physical examination was remarkable for large pulsating femoral and axillary arteries. His echocardiogram also revealed severe tricuspid and mitral regurgitation. The white blood cell count revealed 11 400/mm3 with 36% neutrophils, 23% bands, 29% lymphocytes, and 2% monocytes. His erythrocyte sedimentation rate was 60. He was noted to desquamate the 3rd wk after onset of fever. The patient was treated symptomatically for congestive heart failure.
Blood cultures were negative. However, his pharyngeal and rectal cultures grew out many coagulase-positive S. aureus. He became afebrile after receiving high dose i.v. immune globulin (2 g/kg) therapy and was discharged after 1 mo of hospitalization.
Patient 2. This male infant presented at 6 wk of age to The Children's Hospital of Philadelphia with fever, irritability, and anemia. He received 72 h of i.v. antibiotics pending negative blood, cerebrospinal fluid, and urine cultures. He was discharged only to return 1 wk later with spiking fevers, increased irritability, worsening anemia (Hb 6.5 g/dL), a peripheral eosinophilia, lymphadenopathy, and hepatosplenomegaly. He was noted to have“cherry red” lips by family members. His erythrocyte sedimentation rate was 70. Extensive workup including a bone marrow aspirate, liver biopsy, and a toxoplasmosis, rubella, cytomegalovirus, and herpes simplex titer evaluation were negative.
He was discharged but returned 5 d later at 11 wk of age with increasing irritability, diarrhea, vomiting, fevers, and pneumonia on chest radiograph. A complete blood count revealed 18 500/mm3 white blood cells with 56% neutrophils, 15% bands, 19% lymphocytes, and 10% monocytes. Hb was 9.6 g/dL, and the platelet count was 587 000/mm3. Within 12 h of this admission, he developed cardiovascular collapse due to impaired ventricular function and required mechanical ventilation, dopamine, and dobutamine. He also developed pulseless, white upper extremities. A red evanescent rash was noted on his face and trunk. He did not have any desquamation. Cultures revealed a pure culture of coagulase-positive S. aureus from his initial tracheal intubation and respiratory syncytial virus from a tracheal aspirate. He received antibiotic therapy for his S. aureus. Initial echocardiogram revealed diffusely dilated coronary arteries without pericardial effusion. A repeat echocardiogram the following day revealed fusiform ectasia of right coronary artery (4-5 mm) and dilated left coronary artery 3 mm proximally. A diagnosis of atypical KS was made. The patient received four 2 g/kg doses of i.v. immune globulin and i.v. Solu-Medrol(Upjohn) for recurrent symptoms. His peak platelet count was 711 000/mm3 and his peak C-reactive protein was 9.0 mg/dL. His right forearm and left fifth digit infarcted despite aggressive therapy and required amputation on hospital d 15. He returned at 6 mo of age with hematochezia. He was found to have a stricture which required small bowel resection. Old thrombotic aneurysms were seen histologically. The patient has subsequently been asymptomatic.
Patient 3. At 3 mo of age, this patient developed wheezing and nasal congestion. This was followed immediately by daily fevers for 2 wk. He became pale, irritable, and developed diarrhea. Two weeks into his illness, he developed red conjunctiva and an evanescent rash. A blood culture and urine culture were obtained which were negative. His fevers persisted and he lost weight. Four weeks into his illness a complete blood count was obtained that demonstrated a white blood cell count of 32 000/mm3, Hb of 7.2 g/dL, and platelet count of 878 000/mm3. He was admitted to The Children's Hospital of Philadelphia and an additional blood culture was obtained that was negative. Two days after admission, his hands became dusky and pulseless. An echocardiogram was obtained that showed a moderate pericardial effusion, diffusely dilated right and left coronary arteries (4-5 mm), and normal cardiac function. Atypical KS was diagnosed.
Pharyngeal and rectal cultures grew many colonies of S. aureus. He received 2 g/kg i.v. immune globulin and Solu-Medrol with prompt resolution of fever and irritability. He was also treated with rifampin and cephalexin to eradicate the S. aureus. Three days later an echocardiogram revealed a small pericardial effusion, right main coronary artery diffusely dilated at 7 mm, and left main and circumflex arteries diffusely dilated to 4-5 mm. Six weeks later an echocardiogram revealed persistence of the coronary artery dilatation with the proximal left coronary artery dilated to 3-4 mm and the proximal right coronary artery dilated to 7-8 mm. He has done well subsequently.
Characterization of S. aureus. S. aureus was isolated from each of these three patients with acute KS complicated by coronary artery disease, as well as an additional 6-mo-old hispanic male infant (referred to as patient 4) who had features of KS and multiple coronary artery aneurysms in whom T cell studies were not done. The S. aureus from patients 1, 3, and 4 produced TSST-1 as detected by double immunodiffusion. These organisms were coagulase-positive, off white to white in color, and weakly hemolytic on blood agar plates. The organism from patient 3 also produced enterotoxin C. Of note, S. aureus from patient 2 produced exfoliative toxin type A, also detected by double immunodiffusion. This organism was coagulase-positive, off white in color, and was strongly hemolytic on blood agar plates.
Vβ2+ T cell analysis. It is well established that TSST-1 and exfoliative toxin stimulate the selective expansion of T cells expressing the Vβ2 region of the T cell receptor(19). To determine whether infection with S. aureus secreting TSST-1 or exfoliative toxin was associated with abnormal expression of Vβ2+ T cells we analyzed the T cell repertoire from the peripheral blood of patients 1, 2, and 3 using Vβ-specific MAb and flow cytometry as previously described by our laboratory(11). Due to the small volumes of blood available, we focused on Vβ2 and examined Vβ8.1 and Vβ12 for purposes of comparison.
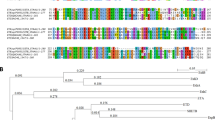
As shown in Figure 1, the percentage of Vβ2+ T cells in patients 2 and 3 during acute KS was higher than the normal range for Vβ2 previously established in peripheral blood lymphocytes from normal children(11), whereas the percentage of Vβ2+ T cells in patient 2 was markedly lower than normal. In contrast, there was no significant difference seen in the percentages of T cells bearing Vβ8.1 or Vβ12 (data not shown). Serial analyses of blood samples from patients 3 and 4 indicated a decrease in percentage of Vβ2+ T cells toward the normal range for Vβ2(see Fig. 1). Of interest, the percent Vβ2 value for patient 3 decreased during convalescence below the normal range.
Serial analysis of Vβ2+ T cells. All determinations were done by using two-color immunofluorescence and flow cytometric analysis with phycoerythrin-conjugated anti-Vβ2 MAb and peridinin chlorophyll protein-conjugated anti-CD3 (Becton Dickinson, Mountainview, CA). Normal range for percentage of Vβ2 is shown in the shaded area.
DISCUSSION
The cases reported here illustrate the clinical challenge in making a prompt diagnosis of acute KS in young infants, particularly those 6 mo of age or younger. Male infants in this age group are at greatest risk for the development of severe coronary artery disease(20). Indeed, in cases 2 and 3, the complete clinical criteria for diagnosis of KS were not fulfilled, and it was only the astute judgment of the child's physician that led to a diagnosis of “atypical KS.” Unfortunately, the diagnosis of atypical KS requires the presence of coronary artery abnormalities, and treatment with i.v. immune globulin can no longer prevent the most devastating complication of this illness. Clearly there is a need for the development of objective laboratory tests for the diagnosis of KS.
In the current study, we demonstrate for the first time that acute KS complicated by coronary artery abnormalities is associated with infection and/or colonization by superantigen-producing S. aureus. Importantly, large numbers or pure cultures of S. aureus could be isolated from all three of these children. In our experience, patients with uncomplicated KS have a lower number of TSST+ S. aureus isolated from either their throat or rectum(10) (P. M. Schlievert and D. Y. M.Leung, unpublished observations). This is consistent with previous observations that patients with KS complicated by coronary artery disease have a higher level of immune activation than patients with uncomplicated KS(21).
TSST-1 was produced by S. aureus from three of the cases, and exfoliative toxin A from the remaining case. The observation that these two different staphylococcal toxins are potent activators of Vβ2+ T cells suggest an important role for this T cell subset in the pathogenesis of this autoimmune disease. Of note, all three of the patients in whom blood was available before i.v. immune globulin treatment had evidence of abnormalities in their Vβ2+ T cell subpopulation. Cases 2 and 3 were associated initially with expansion of Vβ2+ T cells (see Fig. 1). The significance of the Vβ2 expansion was supported by the observation that the Vβ2 values for these two patients decreased during convalescence. Of interest, cases 1 and 3 demonstrated evidence of peripheral blood Vβ2+ T cell depletion or deletion during their course of illness. This is consistent with superantigenic stimulation as studies in animal models have reported that superantigens cause deletion of Vβ-specific circulating T cells after an initial expansion(22). In particular, case 3 appears to have followed this pattern of Vβ2 expansion followed by Vβ2 deletion. An alternative explanation is that reduced Vβ2+ T cells in the peripheral blood may reflect the large-scale homing of these T cells into inflamed tissues(23). Indeed, previous studies have demonstrated increased numbers of Vβ2+ T cells in the small intestinal mucosa as well as cardiac tissue from patients with acute KS(14, 15).
During the past few years, there has been considerable interest in the possibility that acute KS is triggered by bacterial superantigens. This hypothesis is particularly attractive because there is considerable epidemiologic evidence supporting the concept that KS is caused by an infectious agent and the clinical features of KS including the fever, exanthem and desquamation that follows the acute phase of this illness is consistent with a bacterial toxin-mediated disease(6). The strongest immunologic evidence supporting a superantigenic etiology is the observation from three different groups of investigators that peripheral blood- and tissue-infiltrating T cells in acute KS are associated with expansion of Vβ2+ T cells(10–14). However, other investigators have not found a consistent pattern of Vβ2 expansion in KS(24). The reason for this is unclear, but may be due to the existence of several etiologic agents or due to differences in the timing of the blood collection. Indeed, Curtis et al.(13) found increased Vβ2+ T cells only during the 2nd wk of KS.
Our current report also confirms and extends our previous study demonstrating the presence of TSST-1-producing S. aureus in the majority of patients with acute KS(10). Of note, the latter report did not attempt to examine whether patients infected with TSST-1-producing S. aureus had evidence of Vβ2+ T cell stimulation. The lack of reports from other groups confirming an association of TSST-1 S. aureus from patients with KS may relate to the unusual phenotype of the KS S. aureus, which is uniformly nonhemolytic, off-white in appearance, and often grows slowly on blood agar plates(9).
There have also been concerns that the isolation of TSST+ S. aureus from our previously reported patients with KS may simply reflect a variant of staphylococcal toxic shock syndrome, an illness which has many overlapping features with KS. However, coronary artery aneurysms are not generally considered to be a complication of toxic shock syndrome nor have our KS patients been hypotensive due to shock. Our current observations are of potentially great interest because it raises the possibility that microbial superantigens can induce coronary artery disease. Therefore patients with toxic shock syndrome, and other bacterial toxin-mediated diseases, should also be examined for future development of cardiovascular disease. Indeed there have been two previous case reports of children initially diagnosed with toxic shock syndrome, but subsequently found to have KS complicated by coronary artery aneurysms(25, 26). Finally, this is the first report of S. aureus producing exfoliative toxin A in KS. In case 2, a pure culture of S. aureus was isolated from a tracheal aspirate, making it unlikely to be a contaminant. In all, three superantigens,i.e. staphylococcal TSST-1 and exfoliative toxin as well as streptococcal pyrogenic exotoxin C, have now been found to be associated with this illness. Based on these observations, we propose that this illness is not a disease triggered by a single agent, but a syndrome induced by several microbial agents, all of which can induce expansion of Vβ2+ T cells. This illness should therefore be referred to as Kawasaki“syndrome” rather than Kawasaki “disease.” Finally, these data suggest the need for prospective trials of aggressive antibacterial therapy in the treatment of KS particularly in patients who do not respond to i.v. immune globulin therapy.
Abbreviations
- KS:
-
Kawasaki syndrome
- TSST:
-
toxic shock syndrome toxin
References
Tizard EJ, Baguley E, Hughes GR, Dillon MJ 1991 Antiendothelial cell antibodies detected by a cellular based ELISA in Kawasaki disease. Arch Dis Child 66: 189–192.
Meissner HC, Leung DYM 1995 Kawasaki syndrome. Curr Opin Rheumatol 7: 455–458.
Suzuki A, Kamiya T, Kuwahara N, Ono Y, Kohata T, Takahashi O, Kimura K, Takamiya M 1986 Coronary arterial lesions of Kawasaki disease: cardiac catheterization findings of 1100 cases. Pediatr Cardiol 7: 3–9.
Newburger JW, Takahashi M, Beiser AS, Burns JC, Bastian J, Chung KJ, Colan SD, Duffy CE, Fulton DR, Glode MP, Mason WH, Meissner HC, Rowley AH, Shulman ST, Reddy V, Sundel RP, Wiggins JW, Colton T, Melish ME, Rosen FS 1991 A single intravenous infusion of γ globulin as compared with four infusions in the treatment of acute Kawasaki syndrome. N Engl J Med 324: 1633–1639.
Rowley AH, Gonzalez-Crussi F, Gidding SS 1987 Incomplete Kawasaki disease with coronary artery involvement. J Pediatr 110: 409–413.
Leung DYM, Meissner HC, Fulton DR, Quimby F, Schlievert PM 1995 Superantigens in Kawasaki disease. Clin Immunol Immunopathol 77: 119–126.
Abe Y, Nakano S, Nakahar T, Kamezawa Y, Kato I, Ushijima H, Yoshino K, Ito S, Noma S, Okitsu S, Tajima M 1990 Detection of serum antibody by the antimitogen assay against streptococcal erythrogenic toxins. Pediatr Res 27: 11–15.
Terai M, Miwa K, Williams T, Kabat W, Fukuyama M, Okajima Y, Igarashi H, Shulman ST 1995 The absence of evidence of staphylococcal toxin involvement in the pathogenesis of Kawasaki disease. J Infect Dis 172: 558–561.
Todome Y, Ohkuni H, Mizuse M, et al 1995 Superantigenic exotoxin production by isolates of Staphylococcus aureus from the Kawasaki syndrome patients and age-matched control children. J Med Microbiol 42: 91–95.
Leung DYM, Meissner HC, Fulton DR, Murray DL, Kotzin BL, Schlievert PM 1993 Toxic shock syndrome toxin-secreting Staphylococcus aureus in Kawasaki syndrome. Lancet 342: 1385–1388.
Abe J, Kotzin BL, Jujo K, Melish ME, Glode MP, Kohsaka T, Leung DYM 1992 Selective expansion of T cells expressing T cell receptor variable regions Vβ2 and Vβ8 in Kawasaki disease. Proc Natl Acad Sci USA 89: 4066–4070.
Abe J, Kotzin BL, Meissner C, Melish ME, Takahashi M, Fulton D, Romagne F, Malissen B, Leung DYM 1993 Characterization of T cell repertoire changes in acute Kawasaki disease. J Exp Med 177: 791–796.
Curtis N, Zheng R, Lamb JR, Levin M 1995 Evidence for a superantigen mediated process in Kawasaki disease. Arch Dis Child 72: 308–311.
Leung DYM, Giorno R, Kazemi LV, Flynn PA, Bussel JB 1995 Evidence for superantigen involvement in cardiovascular injury due to Kawasaki syndrome. J Immunol 155: 5018–5021.
Yamashiro Y, Nagata S, Oguchi S, Shimizu 1996 Selective increase of Vβ2+ T cells in the small intestinal mucosa in Kawasaki disease. Pediatr Res 39: 264–266.
American Heart Association Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease 1990 Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease 1990 Diagnostic guidelines for Kawasaki disease. JAMA 44: 1218–1219.
Schlievert PM, Osterholm MT, Kelly JA, Nishimura RD 1982 Toxin and enzyme characterization of Staphylococcus aureus isolates from patients with and without toxic shock syndrome. Ann Intern Med 96: 937–940.
Schlievert PM 1988 Immunochemical assays for toxic shock syndrome toxin-1. Methods Enzymol 165: 339–344.
Kotzin BL, Leung DYM, Kappler J, Marrack P 1993 Superantigens and their potential role in human disease. Adv Immunol 54: 99–166.
Burns JC, Wiggins JW, Toews WH, Newburger JW, Leung DYM, Wilson H, Glode MP 1986 The clinical spectrum of Kawasaki syndrome in infants less than six months of age. J Pediatr 109: 759–763.
Matsubara T, Furukawa S, Yabuta K. 1990 Serum levels of tumor necrosis factor, interleukin 2 receptor and interferon-γ in Kawasaki disease involved coronary artery lesions. Clin Immunol Immunopathol 56: 29–36.
McCormack JE, Callahan JE, Kappler J, Marrack PC 1993 Profound deletion of mature T cells in vivo by chronic exposure to exogenous superantigen. J Immunol 150: 3785–3792.
Leung DYM, Gately M, Trumble A, Ferguson-Darnell B, Schlievert PM, Picker LJ 1995 Bacterial superantigens induce T cell expression of the skin-selective homing receptor, the cutaneous lymphocyte-associated antigen (CLA). J Exp Med 181: 747–753.
Pietra BA, De Inocencio J, Giannini EH, Hirsch R 1994 TCR Vβ family repertoire and T cell activation markers in Kawasaki disease. J Immunol 153: 1881–1888.
Wiesenthal AM, Todd JK 1984 Toxic shock syndrome in children aged 10 years or less. Pediatrics 74: 112–117.
Gamillscheg A, Zobel G, Karpf EF, Dacar D, Beitzke A, Stein JI, Suppan C 1993 Atypical presentation of Kawasaki disease in an infant. Pediatr Cardiol 14: 223–226.
Author information
Authors and Affiliations
Additional information
Supported in part by National Institutes of Health Grants HL37260, AR41256, and HL36611, and a Fellowship from the American Heart Association of Colorado.
Rights and permissions
About this article
Cite this article
Leung, D., Sullivan, K., Brown-Whitehorn, T. et al. Association of Toxic Shock Syndrome Toxin-Secreting and Exfoliative Toxin-Secreting Staphylococcus aureus with Kawasaki Syndrome Complicated by Coronary Artery Disease. Pediatr Res 42, 268–272 (1997). https://doi.org/10.1203/00006450-199709000-00004
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199709000-00004