Abstract
The effects of breathing normal saline, salmeterol, fenoterol, ipratropium bromide, or formoterol, and of i.v. infusion of theophylline on oxygen consumption (˙Vo2), carbon dioxide production (˙Vco2), minute ventilation (˙Ve), heart and respiratory rates, and end-tidal carbon dioxide tension (PETco2) have been defined in 10 anesthetized, intubated rhesus monkeys (mean age 7.0 y, weight 10.2 kg).˙Vo2 increased over control by +17.1% after salmeterol (p< 0.001), +33.3% after fenoterol (p < 0.001), +23.7% after formoterol (p < 0.001), +3.9% after theophylline (p< 0.01), but did not change after ipratropium bromide and normal saline. Ve increased by 63.0% after fenoterol (p < 0.001), 49.8% after formoterol (p < 0.001), 31.7% after salmeterol (p < 0.01), and 29.7% after theophylline (p < 0.001), but not after ipratropium bromide or normal saline. Heart rate response was greatest after fenoterol, formoterol, and salmeterol, respectively. PETco2 dropped dramatically after theophylline (-15.7%, p < 0.001), but not at all with any of the inhaled β2-adrenoceptor agonists. In seven animals, salbutamol (albuterol) caused an increase in ˙Ve and˙Vo2 of 50.1% and 45.9%, respectively, whereas in the presence of aβ2-adrenoceptor antagonist {racemic or (+/-)-propranolol (0.1 mg/kg i.v.)}, inhaled salbutamol (2.5 mg/mL for 10 min) could not increase˙Ve (+6.2%, p > 0.05) and ˙Vo2 (+1.6%, p> 0.05). The increase in ˙Vo2 and ˙Ve after administration of β2-agonists may be partly the result of direct stimulation of the respiratory center and partly a response to increased metabolic rate. The dramatic increase in ˙Vo2 and ˙Ve after salbutamol was suppressed in the presence of propranolol, which is consistent with aβ-receptor-mediated mechanism.
Similar content being viewed by others
Main
Although estimates vary widely, in normal subjects breathing quietly the˙Vo2resp is less than 5% of the total oxygen requirement(˙Vo2)(1). ˙Vo2resp increases with rising levels of ventilation because of the increase in power output of the respiratory muscles. Patients with isolated lung diseases and those with combined cardiorespiratory diseases have been reported with elevated˙Vo2resp in the range from 8 to 24% of total body ˙Vo2(1–4).
Drugs such as β2-agonists may increase total body˙Vo2 (and thus energy requirement) either by their direct effect on other organs through β-stimulation or by increasing the oxygen cost of breathing. The drugs may do this either directly by stimulating skeletal(i.e. respiratory) muscles, or indirectly through stimulating minute ventilation via action on the respiratory center. Thus, in critically ill infants with respiratory compromise treated with inhaledβ2-agonists, the economy of oxygen consumption could deteriorate if the degree of bronchodilatation does not allow ventilation to increase sufficiently to offset the increase in total body ˙Vo2.
We have previously reported the ventilatory and oxygen costs in anesthetized rhesus monkeys of inhaling salbutamol (albuterol), terbutaline, epinephrine, sodium cromoglycate, and methacholine(5). We found that the β-agonists had marked effects on both ˙Ve and˙Vo2, whereas methacholine had a pronounced effect only on the former, suggesting a different mechanism of action. When all β-agonists were reviewed, salbutamol had the most profound effects with 85 and 45% increases in ˙Ve and ˙Vo2, respectively.
In this study, we investigated the influence of fenoterol and two new long acting β2-adrenoceptor agonists, salmeterol and formoterol, on˙Ve and ˙Vo2 when administered by the inhaled route in normal, non-human primates, and of theophylline by the i.v. route. Long acting inhaled bronchodilators are increasingly used for the treatment of asthma and other forms of chronic airway obstruction. Although long acting inhaledβ2-adrenergic drugs are not currently recommended as emergency or intensive care treatment for severe airway obstruction, these drugs are increasingly used in the ambulatory care of patients with asthma or other forms of chronic airway obstruction.
We also examined the effect of i.v. propranolol upon the consistent and marked stimulation of ˙Ve and ˙Vo2 secondary to salbutamol to investigate whether the observed metabolic and ventilatory changes are caused by direct action on β-adrenergic receptors.
METHODS
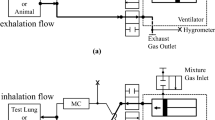
Group A experiments. Ten male rhesus monkeys (Macaca mulatta) with a mean age of 7.0 y (range 6.5 to 8.0 y) and mean weight of 10.2 kg (range 6.5 to 13.0 kg) were investigated using techniques that have been previously described(5). Animals were sedated intramuscularly with ketamine (40 mg/kg) and anesthetized by i.v. infusion of thiopentone sodium (8.0 mg/kg/h) for the duration of the experiment. The larynx, epiglottis, pharynx, and nasal passage were initially anesthetized with 2 mL of topical xylocaine (1% solution) before intubation with a 4.5-mm diameter internal lumen, cuffed endotracheal tube. The cuff was inflated sufficiently to prevent any air leak detectable by auscultation when the lungs were inflated to +50 cm H2O pressure. The animals breathed spontaneously, and the stomach contents were drained via a pediatric feeding tube. Animals were placed in the left lateral recumbent position, and body temperature was monitored continually with an esophageal probe and maintained between 37.8 and 38.2 °C. Three-lead continual electrocardiographic monitoring was done, and the respiratory rate was determined by changes in thoracic electrical impedance (Sirecust model 1281, Siemens, Erlangen, Germany). Sao2 was monitored by pulse oximetry (Nellcor Type B, Hayward, CA). Measurement of PETco2 and mixed expired gases for the determination of functional residual capacity ˙Ve, ˙Vo2, and ˙Vco2 was done with a respiratory mass spectrometer (Airspec MGA 2200, Biggin Hill, UK). ˙Vo2, ˙Vco2, and ˙Ve were determined by the argon dilution technique(6), and the functional residual capacity by a nitrogen washout technique(7) using a computer-based data acquisition system(SensorMedics 2600, Anaheim, CA). In our system, the coefficient of variation for repeated baseline measurements taken over 10 min was less than 3.5% for˙VE, ˙Vo2, and ˙Vco2. After four repeated saline challenges in two monkeys, the intraindividual coefficient of variation for ˙Vo2 was less than 6.0%, and less than 6.1% for ˙Ve.
All test substances were delivered as aerosols using the Cirrhus™ Nebulizer (DHD Medical Products, Canastota, NY) operated at 6 L/min flow of compressed air. The aerosol generated has a mass median aerodynamic diameter of 3.5 μm, determined by laser scatter method, and a mean nebulizer output of 0.307 ± 0.02 mL/min. Seventy percent of the total output has a particle size between 1.2 and 10 μm. The nebulizer was connected to the endotracheal tube by a T-adaptor. Aerosols were delivered by tidal breathing.
After anesthesia, baseline recordings were made of heart and respiratory rates, Sao2, PETco2, temperature, ˙Ve,˙Vo2, and ˙Vco2. Although not reported here, recordings were also taken of respiratory mechanics by single-breath occlusion and forced expiratory flow-volume curves by forced deflation and rapid thoracoabdominal compression. The animals then inhaled nebulized, phosphate-buffered normal saline (0.9%, pH 7.4) for 10 min before all other drugs, except for the theophylline series, in which an i.v. infusion of normal saline was given as the control. Measurements of all variables including ˙Ve, ˙Vo2, and ˙Vco2 were repeated 10 min after the saline challenge.
Challenges with salmeterol, formoterol, fenoterol, and ipratropium bromide were administered for 10 min by inhalation. Ten minutes after cessation of nebulization, all recordings were repeated with ˙Ve, ˙Vo2, and˙Vco2 continuously measured for 5 min to assure baseline stability. Theophylline was infused i.v. for 20 min. At 10 min after the infusion was finished, all recordings were repeated, and at the same time a blood sample for theophylline serum concentrations was taken.
No monkey was studied more than once for each drug, and all studies were performed at the same time of the day. In general, about 2 wk were allowed for recovery after an animal completed any one drug inhalation experiment. At least eight monkeys were studied with each drug, and the order of drug exposure was randomized. The recovery time between experiments, and the limited time available to one investigator (C.J.L.N.) precluded all 10 monkeys being studied with all compounds. All monkeys had stable body weights throughout the study period of about 4 mo.
The numbers of monkeys studied under each condition were: 1) salmeterol, 0.5 mg/mL solution, nine monkeys; 2) fenoterol, 2.5 mg/mL solution, eight monkeys; 3) formoterol, 0.12 mg/mL solution, eight monkeys; 4) ipratropium bromide, 0.125 mg/mL solution, eight monkeys; 5) theophylline, 20 mg/kg solution, nine monkeys; and 6) normal saline, 0.9% solution, 10 monkeys. Commercially available preparations from the same batch were used in all experimental series.
Group B experiments. After it was ascertained that all theβ2-agonists tested caused large increases in ˙Ve,˙Vo2, and ˙Vco2, a further set of experiments was done on another group of monkeys to investigate the pharmacologic mechanism.
Seven monkeys were studied after salbutamol (the β2-agonist causing the greatest increase in ˙Ve and ˙Vo2(5), using the same techniques as for group A. Their mean weight and range were 7.5 and 5.0-10.2 kg, respectively. On the 1st d, the animals inhaled phosphate-buffered normal saline for 10 min after baseline recordings, and then salbutamol solution 2.5 mg/mL for 10 min after a 10-min interval. On the 2nd d, the monkeys received i.v. propranolol 0.1 mg/mL after the baseline recordings and 30 min before the salbutamol challenge at the same dose as previously. All measurements were taken at the same time intervals as the previous (group A) experiments.
Data analysis. A one-way ANOVA was used to compare the measured variables between the different drug groups. A value of p < 0.05 was accepted as significant, the grouping variable being the different study agents. The Bonferroni adjustment was used to determine differences among groups.
Comparisons of physiologic measurements recorded from the monkeys before and after inhalation of each study drug were made using a paired t test. Statistical significance was assumed at a level of 0.05.
Animal welfare and experimental ethics. Animals were maintained in an in-house colony at Sandoz AG; Basel, Switzerland, under the full-time care of an experienced primate veterinarian and his staff. Animals were fed and housed under conditions allowing normal growth, play, and social interactions. All experimental protocols conformed to international standards of animal welfare and were approved and periodically reviewed by the Kantonale Tierversuchs-Kommission von Basel-Stadt und Baselland, the independent external review body for animal experimentation.
RESULTS
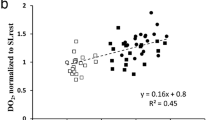
Group A experiments. All raw data are enumerated in detail for each study drug as the mean ± SE in Table 1. Percent changes in ˙Vo2 and ˙Ve after each drug are summarized in Figures 1 and 2, respectively.
Percent changes in oxygen consumption (˙Vo2) after inhaling the study drugs. The results are mean data and are standardized by using percent change from the control (i.e. baseline, no treatment) established for each drug. The statistical differences between drugs were analyzed by ANOVA, whereby bars (drugs) with the same letters show no statistical difference.
Percent changes in minute ventilation (˙Ve) after inhaling the study drugs. The results are mean data and are standardized by using percent change from the control (i.e. baseline, no treatment) established for each drug. The statistical differences between drugs were analyzed by ANOVA, whereby bars (drugs) with the same letters show no statistical difference.
Fenoterol, salmeterol, and formoterol caused marked and significant increases in ˙Ve, ˙Vo2, heart rate, and respiratory rate in the range of 17 to 68% change from baseline. These increases were also significant, but smaller in magnitude, after theophylline infusion. The serum blood levels of theophylline 10 min after infusion were 174.6 ± 6.7μmol/L (therapeutic range 55.5 to 110.0 μmol/L). No significant changes in all parameters studied were observed after the inhalation of ipratropium bromide. We also calculated the oxygen pulse (the ratio of ˙Vo2 to heart rate) for each drug and found significant decreases after the inhalation of fenoterol, formoterol, and theophylline (p < 0.05), but not after ipratropium and salmeterol (p > 0.05).
The baseline value for functional residual capacity corrected for body weight was 15.6 ± 2.1 mL/kg. After saline inhalation, this increased slightly to 16.7 ± 1.0 mL/kg (+7.1%) which was not statistically significant. After salmeterol inhalation, the value changed to 18.8 ± 2.9 mL/kg (+18.8%), which just reached statistical significance (p< 0.05). The Sao2 changed from 98.1 ± 1.0% to 97.7 ± 1.2% after saline, and to 97.3 ± 0.8% after salmeterol (p = NS).
Group B experiments. All raw data are enumerated as mean± SE in Table 2, percent changes for˙Vo2, ˙Ve, heart rate, and respiratory rate with salbutamol before and after propranolol are summarized in Figure 3.
The significant effects of salbutamol on ˙Vo2, ˙Vco2,˙Ve, heart rate, and respiratory rate were completely abolished when the drug was inhaled after i.v. propranolol administration. There was no difference in oxygen pulse (˙Vo2/heart rate) from baseline either after salbutamol alone or salbutamol after propranol, because both variables were equally affected.
DISCUSSION
The present study demonstrates that fenoterol and the long actingβ2-agonists salmeterol and formoterol cause a marked increase in oxygen consumption and spontaneous minute ventilation in the anesthetized rhesus monkey. Similar findings have previously been reported for terbutaline, adrenaline, and salbutamol(5). A small increase in˙Vo2 and a relatively higher increase in ˙Ve also followed the i.v. infusion of theophylline. In contrast, the inhalation of the antimuscarinic agent ipratropium bromide did not result in a significant change in ˙Ve and ˙Vo2. This tends to exclude the possibility that bronchodilatation (with subsequent improvement in ventilation) was responsible for the increase in ˙Vo2.
An increase in energy expenditure and ˙Vo2 upon adrenergic stimulation is a basic mechanism in mammals(8). It has long been recognized that tremor of skeletal muscle occurs in the presence ofβ2-agonist(9, 10) and that adrenaline increases glucose and esterified FFA utilization. Increases in brown fat metabolism and total body ˙Vo2 by β-adrenoceptor agonists have been documented by Holloway and colleagues(11). In our study, the β2-agonists and theophylline, but not ipratropium bromide, caused significant increases in heart rate. Stimulation of cardiac metabolism has been previously demonstrated after β2-agonists administration(12, 13). Cardiacβ2-adrenoceptors are most numerous in the sinu-atrial node and enhance the rate and contractility of the atrium(14). This, along with lowering of systemic vascular resistance by peripheral vasodilatation, could explain the remarkable increase in heart rates after the various β2-agonists administered in our study. However, it is unclear if the observed metabolic effects by the β2-agonist are caused exclusively by a selective action upon the β2-adrenoceptor. We cannot exclude a nonselective stimulation of β1-adrenoceptors or a direct action upon the respiratory center with a subsequent increase in the work of breathing. In addition, a third (i.e. β3) adrenoceptor has recently been identified(15) and could also be responsible for some of the observed effects. It is known thatβ3-receptors determine certain physiologic actions of adrenaline, including increased metabolism in brown fat(16, 17). The presence of the β3-adrenoceptor has also been postulated in the heart(18). Furthermore, theβ2-sympathomimetics studied are mixtures of diasteric isomers, whose dextro-enantiomers are not biologically inert as had been previously presumed, because both dextro-isoprenaline(19) and dextro-salbutamol(20, 21) cause airway hyperreactivity in the guinea pig. Hence, increased oxygen consumption after inhalation of β2-agonists was not unexpected, although this phenomenon has only rarely been reported. Our findings suggest that the increase in ˙Vo2 represents a “class” effect ofβ-adrenergic drugs, because it was observed after allβ2-agonist tested (but not after ipratropium bromide) and because the effects of salbutamol were fully suppressed by the unselectiveβ-blocker (+/-)-propranolol.
The fall in arterial oxygen tension that has been observed after inhalation of β2-agonist bronchodilators in patients with asthma is typically a transient event(22–25). The mechanism of this acute decline in oxygenation has generally been assumed to reflect increased mismatch of ventilation-perfusion due to increased deadspace ventilation and increased cardiac output(26), as well as pulmonary vasodilation and altered tissue oxygen extraction. Whether the increase in ˙Vo2 as a direct effect of these drugs contributes to the fall in arterial oxygen tension does not appear to have been considered. In the present (and also the previous) study(5), it was expected that an increase in ˙Vo2 would have no effect on arterial oxygen saturation in healthy animals. It is possible that the effects on˙Vo2 do not last as long as the bronchodilator effect. During our experiments, we have observed a continued increase in ˙Vo2 over baseline after 2 h in some animals, although we have not formally studied its duration. Ensinger and co-workers(27) described steady elevations in ˙Vo2 during a 4-h infusion of adrenaline. However, their data on adrenoceptor agonist infusions may not be applicable to inhaledβ2-agonists.
Doses of salbutamol, salmeterol, formoterol, and fenoterol were chosen as equivalent bronchodilator doses in asthmatic patients. It is likely that the monkeys received a somewhat higher (but proportionately equivalent) dose of each drug than would spontaneously breathing, nonintubated humans. This was because they had normal airways with no airflow obstruction, and drugs were inhaled directly into the respiratory tract through the endotracheal tube, bypassing any “rain-out” in the mouth. These effects ofβ2-agonists on ˙Ve and ˙Vo2 suggests that a critical level could be reached at which the ability of increasing ventilation to improve oxygenation is overcome by the increased oxygen cost of the respiratory muscle work needed to provide the additional ventilation, along with any other increases in ˙VO2 that β2-agonists may cause (e.g. in the heart, brain, skeletal muscles, and adipose tissue). β2-Adrenoceptors are known to be widely distributed throughout tissues(21). The abolition of the salbutamol effects on heart rate and oxygen uptake by propranolol provides further evidence that the increase in ˙Vo2 by β2-agonists is caused by a widespread action on β-adrenoceptors in organs other than the respiratory muscles.
Theophylline, despite being given in a dose sufficient to achieve supratherapeutic serum concentrations (174.6 ± 6.7 μmol/L){therapeutic range 55.5-110.0 μmol/L} had relatively little effect on˙Vo2 (4% increase), but increased ˙Ve by 30%. It is likely that this increase in ˙Ve (which was similar in magnitude to salmeterol) was caused by a direct action upon the respiratory center. In the absence of significant systemic increases in ˙Vo2, the increase in ˙Ve and the work of breathing may explain the relatively modest increase in˙Vo2, because the oxygen cost of breathing is only a small component of the total ˙Vo2. This adds further evidence to the notion that the much larger increases in ˙Vo2 afterβ2-agonists were related to increases in oxygen demands outside the respiratory system.
There are clinical implications for critically ill patients with respiratory failure and acute exacerbations of chronic lung diseases if the animal data hold true in humans. Bronchodilators are very frequently used in desperation in seriously ill infants with acute compromise of their bronchopulmonary dysplasia, or bronchiolitis(28). Although these patients are often able to respond with some degree of bronchodilatation(28–31), it is small compared with the response usually obtained in asthmatic patients. In addition, critically ill patients have a limited ability to increase their˙Ve (and often their cardiac output as a result of pulmonary hypertension) in response to an increased metabolic load. The magnitude of the observed increase in ˙Vo2 after β2-agonists, if reproduced in humans, is of great importance and implies limits on their use in critically ill patients. Furthermore, the increase in ˙Vco2 could worsen respiratory acidosis in critically ill patients with limited ability to remove CO2 (e.g. severe airway obstruction or fixed mechanical ventilation).
When β2-adrenoceptor agonists such as salbutamol are used chronically, the subsequent increase in ˙Vo2 requires greater energy expenditure. Infants and children with chronic lung diseases often have inadequate caloric intake and can ill afford any additional nutritional burden. These negative nutritional effects have already been predicted indirectly by Vaisman and co-workers(32) with their findings of increased resting energy expenditure (predicted largely from˙Vo2) in both patients with cystic fibrosis and normal subjects, when given salbutamol by inhalation. In infants and children, most acute changes in cardiac output (and hence, systemic oxygen transport) are effected by changes in heart rate rather than stroke volume. Thus, because bronchodilators may affect both heart rate and ˙Vo2, oxygen pulse(the ratio of ˙Vo2 to heart rate) “normalizes” the respective responses and reflects the oxygen extracted by the body tissues from the oxygen carried by each stroke volume, i.e. it gives an estimate of the efficiency of the circulatory system. We found significant declines in oxygen pulse after fenoterol, formoterol, and theophylline (the latter because of its effect on heart rate), with little or no change after ipratropium (neither heart rate nor ˙Vo2 changed), salmeterol, and salbutamol (where both changed but were well matched). Theoretically, the latter two drugs would be preferred if therapy with β2-agonists is required in sick patients.
Perhaps unsurprisingly, ipratropium bromide like saline had no effect on˙Ve, ˙Vo2, heart rate, and respiratory rate. The dose we administered to the monkeys was identical to that used clinically in children of the same weight(33). Therefore, it would appear that ipratropium bromide can be administered to infants with lung disease without any additional metabolic burden or nutritional implications(34). This would imply that anticholinergic bronchodilators may be preferred over β2-agonist when administered to acutely or chronically sick infants with an impaired ability to increase energy requirements, especially if the expected bronchodilatation is small.
In conclusion, we demonstrate that the more selectiveβ2-agonists fenoterol, salmeterol, and formoterol cause an increase in ˙Ve, ˙Vo2, and ˙Vco2 similar to that observed after salbutamol and terbutaline. Our data suggest that these increases in ventilatory and oxygen costs are mediated byβ-adrenoreceptors, because the same response was observed after salbutamol, and its effect could be fully suppressed by propranolol. The magnitude of the oxygen costs of β2-bronchodilators may contraindicate or limit the use of these drugs in critically ill infants. We suggest that ipratropium bromide may be the preferred bronchodilator for acutely ill patients with lung disease in whom the greater energy expenditure caused by β2-adrenergic drugs may be harmful.
Abbreviations
- PETco2:
-
end-tidal carbon dioxide tension
- Vco2:
-
carbon dioxide production;˙Ve, minute ventilation
- ˙Vo2:
-
total body oxygen consumption
- ˙Vo2resp:
-
oxygen cost of breathing
- Sao2:
-
arterial oxygen saturation
References
Field S, Kelly SM, Macklem PT 1982 The oxygen cost of breathing in patients with cardiorespiratory disease. Am Rev Respir Dis 126: 9–13.
Cherniak RM 1959 The oxygen consumption and efficiency of the respiratory muscles in health and emphysema. J Clin Invest 38: 494–499.
Katsardis CV, Desmond KJ, Coates AL 1986 Measuring the oxygen cost of breathing in normal adults and patients with cystic fibrosis. Respir Physiol 65: 257–266.
Donahoe M, Rogers RM, Wilson DO, Pennock BE 1989 Oxygen consumption of the respiratory muscles in normal and in malnourished patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 140: 385–391.
Newth CJL, Amsler B, Anderson GP, Morley J 1991 The ventilatory and oxygen costs in the anesthetized rhesus monkey of inhaling drugs used in the therapy and diagnosis of asthma. Am Rev Respir Dis 143: 766–771.
Davies NJH, Denison DM 1979 The measurement of metabolic gas exchange and minute ventilation by mass spectrometry alone. Respir Physiol 36: 261–267.
Sivan Y, Deakers TW, Newth CJL 1990 An automated bedside method for measuring functional residual capacity by N2 washout in mechanically ventilated children. Pediatr Res 28: 446–450.
Landsberg L, Saville ME, Young J 1984 Sympathoadrenal system and regulation of thermogenesis. Am J Physiol 247:E181–E189.
Jenne JW, Valcarenghi G, Druz WS, Starkey PW, Yu C, Shaughnessy T 1986 Comparison of tremor responses to oral albuterol. Am Rev Respir Dis 134: 708–713.
Svedmyr N, Thiringer G 1971 The effects of salbutamol and isoproterenol on β-2 receptors in patients with chronic obstructive disease. Postgrad Med 44: 33–46.
Holloway BR, Howe R, Rao BS, Stribling D, Mayers RM, Briscoe MG, Jackson JM 1991 ICI D7114 a novel selective beta-adrenoceptor agonist selectively stimulates brown fat and increases whole-body oxygen consumption. Br J Pharmacol 104: 97–104.
Shanahan EA, Wahlqvist ML, Wilmshurst EG 1979 Effects ofβ2-adrenoceptor stimulation on cardiac metabolism in the conscious dog. Br J Pharmacol 66: 229–233.
Tandon MK 1980 Cardiopulmonary effects of fenoterol and salbutamol aerosols. Chest 77: 429–431.
Lemoine H, Schonell H, Kaufmann A 1988 Human cardiac beta-adrenergic receptors: subtype heterogeneity delineated by direct radioligand binding. Br J Pharmacol 95: 55–56.
Emorine LJ, Marullo S, Briend-Sutren MM, Patey G, Tate K, Strosberg DA 1989 Molecular characterization of the humanβ3-adrenergic receptor. Science 245: 1118–1121.
Arch JRS, Ainsworth AT, Cawthorne MA, Piercy V, Sennit MV, Thody VE, Wilson C, Wilson S 1984 Atypical β-adrenoceptor on brown adipocytes as target for anti-obesity drugs. Nature 309: 163–165.
Zaagsma J, Hollenga CH 1991 Distribution and function of atypical β3-adrenoceptors. In: Szabadi E, Bradshaw CM, eds. Adrenoceptors: Structure, Mechanisms, Function. Birkhausverlag, Basle, pp 47–58.
Kaumann AJ 1989 Is there a third heart-adrenoceptor?. Trends Pharmacol Sci 10: 316–320.
Sanjar S, Kristersson A, Mazzoni L, Morley J, Schäublin E 1990 Increased airway reactivity in the guinea-pig follows exposure to intravenous isoprenaline. J Phyiol 425: 43–54.
Hoshiko K, Morley J 1993 Exacerbation of airway hyperreactivity by (+/-)-salbutamol in sensitized guinea-pigs. Jpn J Pharmacol 63: 159–163.
Morley J, Sanjar S, Newth C 1990 Viewpoint: untoward effects of β-adrenoceptor agonists in asthma. Eur Respir J 3: 228–233.
Paterson JW, Clark TJH 1971 Aerosols in asthma. Br Med J 1: 557
Paterson JW, Conolly ME, Davies DS, Dollery CT 1968 Isoprenaline resistance and the use of pressurised aerosols in asthma. Lancet 2: 426–429.
Ingram RH, Krumpe PE, Duffell GM, Maniscalco B 1970 Ventilation perfusion relationships after aerosolized isoproterenol in asthma. Am Rev Respir Dis 101: 364–370.
Tal A, Pesterkamp H, Leahy F 1984 Arterial oxygen desaturation following salbutamol inhalation in acute asthma. Chest 86: 868–869.
Iodice F, Rufolo L, Piscione F, De Michele G 1980 Haemodynamic and ventilatory effects of intravenous salbutamol in patients affected by COLD. Respiration 40: 272–277.
Ensinger H, Weichel T, Lindner KH, Grünert A, Georgieff M 1995 Are the effects of noradrenaline, adrenaline and dopamine infusions on VO2 and metabolism transient. Intensive Care Med 21: 50–56.
Hammer J, Numa A, Newth CJL 1995 Albuterol responsiveness in infants with respiratory failure caused by respiratory syncytial virus infection. J Pediatr 127: 485–490.
Rotschild A, Solimano A, Puterman M, Smyth J, Sharma A, Albersheim S 1989 Increased compliance in response to salbutamol in premature infants with developing bronchopulmonary dysplasia. J Pediatr 115: 984–991.
Motoyama EK, Fort MD, Klesh KW, Mutich RL, Guthrie RD 1987 Early onset of airway reactivity in premature infants with bronchopulmonary dysplasia. Am Rev Respir Dis 136: 50–57.
Mallory GB, Motoyama EK, Koumbourliss AC, Mutich RL, Nakayama DK 1989 Bronchial reactivity in infants in acute respiratory failure with viral bronchiolitis. Pediatr Pulmonol 6: 253–259.
Vaisman N, Levy LD, Pencharz PB, Tan YK, Soldin SJ, Canny GJ, Hahn E 1987 Effect of salbutamol on resting energy expenditure in patients with cystic fibrosis. J Pediatr 111: 137–139.
Brundage KL, Mohsini KG, Froese AB, Fisher JT 1990 Bronchodilator response to ipratropium bromide in infants with bronchopulmonary dysplasia. Am Rev Respir Dis 142: 1137–1142.
Kurzner SI, Garg M, Bautista DB, Sargeant CW, Bowman CM, Keens TG 1988 Growth failure in bronchopulmonary dysplasia: elevated metabolic rates and pulmonary mechanics. J Pediatr 112: 73–80.
Acknowledgements
The authors thank A. Harnist for expert technical assistance, M. Scanlon for help with the statistics, and Dr. J. Morley for valuable advice and support.
Author information
Authors and Affiliations
Additional information
Supported by Sandoz AG, Basel, Switzerland, which allowed us the use of the study animals and the Primate Pulmonary Function Laboratory at no cost. The authors are indebted to the Director of the Preclinical Research Group, Sandoz AG, Basel, Switzerland for this opportunity. The study was undertaken during a Study Leave of C.J.L.N.
Rights and permissions
About this article
Cite this article
Newth, C., Amsler, B., Richardson, B. et al. The Effects of Bronchodilators on Spontaneous Ventilation and Oxygen Consumption in Rhesus Monkeys. Pediatr Res 42, 157–162 (1997). https://doi.org/10.1203/00006450-199708000-00005
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199708000-00005