Abstract
Background
Effort of Breathing (EOB) calculations may be a reliable alternative to Work of Breathing (WOB) calculations in which Respiratory Inductance Plethysmography (RIP) replaces spirometry. We sought to compare EOB and WOB measurements in a nonhuman primate model of increasing extrathoracic inspiratory resistance simulating upper airway obstruction (UAO).
Methods
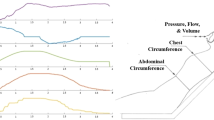
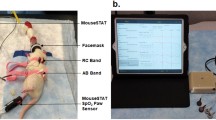
RIP, spirometry, and esophageal manometry were measured in spontaneously breathing, intubated Rhesus monkeys utilizing 11 calibrated resistors randomly applied for 2-min. EOB was calculated breath-by-breath as Pressure Rate Product (PRP) and Pressure Time Product (PTP). WOB was calculated from the Pressure-Volume curve based on spirometry (WOBSPIR) or RIP flow (WOBRIP).
Results
WOB, PRP and PTP showed similar linear increases when exposed to higher levels of resistive loads. When comparing WOBSPIR to WOBRIP, a similar strong correlation was seen for both signals as resistance increased and there were no statistically significant differences.
Conclusion
EOB and WOB parameters utilizing esophageal manometry and RIP, independent of spirometry, showed a strong correlation as a function of increasing inspiratory resistance in nonhuman primates. This allows several potential monitoring possibilities for non-invasively ventilated patients or situations where spirometry is not available.
Impact
-
EOB and WOB parameters showed a strong correlation as a function of increasing inspiratory resistance in nonhuman primates.
-
There was a strong correlation between spirometry-based WOB versus RIP-based WOB.
-
To date, it has remained untested as to whether EOB is a reliable alternative for WOB and if RIP can replace spirometry in these measurements.
-
Our results enable additional potential monitoring possibilities for non-invasively ventilated patients or situations where spirometry is not available.
-
Where spirometry is not available, there is no need to apply a facemask post extubation to a spontaneously breathing, non-intubated infant to make objective EOB measurements.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Argent, A. C., Newth, C. J. L. & Klein, M. The mechanics of breathing in children with acute severe croup. Intensive Care Med. 34, 324–332 (2008).
Graham, A. S., Chandrashekharaiah, G., Citak, A., Wetzel, R. C. & Newth, C. J. L. Positive end-expiratory pressure and pressure support in peripheral airways obstruction. Intensive Care Med. 33, 120–127 (2006).
Willis, B. C., Graham, A. S., Yoon, E., Wetzel, R. C. & Newth, C. J. L. Pressure-rate products and phase angles in children on minimal support ventilation and after extubation. Intensive Care Med. 31, 1700–1705 (2005).
Khemani, R. G. et al. Evaluating Risk Factors for Pediatric Post-extubation Upper Airway Obstruction Using a Physiology-based Tool. Am. J. Resp. Crit. Care. 193, 198–209 (2016).
Klein, M. & Reynolds, L. G. Relief of sleep-related oropharyngeal airway obstruction by continuous insufflation of the pharynx. Lancet 1, 935–939 (1986).
Argent, A. C., Hatherill, M., Newth, C. J. L. & Klein, M. The effect of epinephrine by nebulization on measures of airway obstruction in patients with acute severe croup. Intensive Care Med. 34, 138–147 (2007).
Khemani, R. G. et al. Respiratory inductance plethysmography calibration for pediatric upper airway obstruction: an animal model. Pediatr. Res. 77, 75–83 (2015).
Harrison, V. C., Heese Hde, V. & Klein, M. The significance of grunting in hyaline membrane disease. Pediatrics 41, 549–559 (1968).
Asher, M. I., Coates, A. L., Collinge, J. M. & Milic-Emili, J. Measurement of pleural pressure in neonates. J. Appl Physiol. 52, 491–494 (1982).
Coates, A. L., Davis, G. M., Vallinis, P. & Outerbridge, E. W. Liquid-filled esophageal catheter for measuring pleural pressure in preterm neonates. J. Appl. Physiol. 67, 889–893 (1989).
Hammer, J. & Newth, C. Influence of endotracheal tube diameter on forced deflation flow-volume curves in rhesus monkeys. Eur. Respir. J. 10, 1870–1873 (1997).
Cabello, B. & Mancebo, J. Work of breathing. Intensive Care Med. 32, 1311–1314 (2006).
Khemani, R. G. et al. Pediatric extubation readiness tests should not use pressure support. Intensive Care Med. 42, 1214–1222 (2016).
Sivan, Y., Deakers, T. W. & Newth, C. J. L. Thoracoabdominal asynchrony in acute upper airway obstruction in small children. Am. Rev. Respir. Dis. 142, 540–544 (1990).
Stocks, J. Respiratory physiology during early life. Monaldi Arch. Chest Dis. 54, 358–364 (1999).
Verma, R. P. Respiratory Distress Syndrome of the Newborn Infant. Obstet. Gynecol. Surv. 50, 542–555 (1995).
de Vries, H., Jonkman, A., Shi, Z. H., Spoelstra-de Man, A. & Heunks, L. Assessing breathing effort in mechanical ventilation: physiology and clinical implications. Ann. Transl. Med. 6, 387 (2018).
Acknowledgements
The authors acknowledge the financial support of the National Institutes of Health/National Institutes of Child Health and Development 1K23HL103785 (R.G.K.), Bethesda, MD, and Novartis Pharmaceutical Grant-in-Aid for facilities (C.J.L.N.), Basel, Switzerland.
Author information
Authors and Affiliations
Contributions
Conception and design: R.F., R.K., C.N. Analysis and interpretation: R.F., J.H., M.K., F.d.J., C.N., A.v.K., R.K. Drafting the paper for important intellectual content: R.F., A.v.K., F.d.J., M.K., C.N., R.K.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Flink, R.C., Newth, C.J.L., Hotz, J.C. et al. Effort and work-of-breathing parameters strongly correlate with increased resistance in an animal model. Pediatr Res 94, 944–949 (2023). https://doi.org/10.1038/s41390-023-02576-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02576-4