Abstract
This study was designed to determine indirectly if the changes in ovine fetal pulmonary vascular tone caused by i.v. injections of nitric oxide-containing solutions are mediated by cGMP. We first characterized the dose-response relationship of bolus intrapulmonary injections of zaprinast (a cGMP-selective phosphodiesterase inhibitor) and nitric oxide solutions. Injections of nitric oxide solutions as well as zaprinast solutions resulted in dose-dependent decreases in pulmonary arterial pressure that were greater than reductions in systemic arterial pressure. We also evaluated the effects of simultaneous infusions of zaprinast and U46619 (a thromboxane mimetic) on the response to bolus injections of 1.0 μg of acetylcholine, 100 ng of endothelin-1, and 10.0 μL of ethanol saturated with nitric oxide. Zaprinast was infused at a rate of 1.5 mg/min, and the concentration of U46619 was titrated to raise mean left pulmonary arterial pressure (LPAP) to the steady state level that was present before infusing zaprinast. All bolus injections reduced left pulmonary arterial pressure more than they reduced mean systemic arterial pressure. However, neither the response magnitudes nor the response durations were affected by simultaneous infusions of zaprinast and U46619. We therefore suggest that modulation of fetal pulmonary vascular tone by endogenously produced nitric oxide may involve mechanisms other than raising smooth muscle cytoplasmic cGMP concentrations.
Similar content being viewed by others
Main
Fetal pulmonary circulation is characterized by high pulmonary vascular resistance and low blood flow. Mechanisms that maintain pulmonary vascular resistance high in utero and then low postnatally are incompletely understood. However, some mechanisms involved in the transition to postnatal circulation have been elucidated. Mechanical airway distension(1), uncoiling of peripheral pulmonary blood vessels(2), elevation of arterial Po2(3, 4), and release of endogenous vasodilators(5–7) have all been suggested to augment the pulmonary vasodilation that occurs at birth.
Pulmonary vascular dilation undoubtedly involves interaction of many vasoactive compounds. Changes in vascular smooth muscle cGMP concentrations caused by endothelial production of nitric oxide modulate vascular tone(8–12). Hydrolysis of cGMP to guanosine 5′-monophosphate by cyclic nucleotide phosphodiesterases is believed to limit the duration of cGMP's vasodilating effects. Evidence to support this idea comes from studies showing smooth muscle relaxation caused by inhibition of the cGMP phosphodiesterases. Phosphodiesterase inhibitors such as zaprinast(13, 14), MY-5445(14, 15), and vinpocetine(14, 15) have been shown to relax vascular smooth muscle in isolated tissue preparations. In vivo infusions of zaprinast have been shown to cause vascular dilation in lambs(16), cats(17), and rats(18). Zaprinast has also been shown to potentiate drug-induced vascular smooth muscle relaxation caused by nitrovasodilators(19) and by endothelial-dependent vasodilators such as acetylcholine(12, 16) and ATP(16).
Modulation of fetal pulmonary vascular resistance has recently been suggested to involve endogenous production of nitric oxide(20–24). Abman and Accurso(25) indirectly supported this idea by showing that exogenous administration of a cGMP analog (8-bromo-cGMP) decreases fetal pulmonary vascular resistance. Although this finding suggests the presence of an intact signal transduction system for cGMP in the fetal pulmonary vascular bed, elevation of fetal vascular smooth muscle cGMP has not been directly linked to endogenous nitric oxide production.
The purpose of this study was to evaluate indirectly the role of cGMP in mediating nitric oxide-induced vasodilation of an intact fetal preparation. To accomplish this purpose, fetal sheep were given agonists believed to cause vasodilation, at least in part, by the following mechanisms: 1) directly increasing intracellular smooth muscle cGMP concentrations by activating guanylate cyclase (nitric oxide solutions), 2) indirectly increasing smooth muscle cGMP concentrations by increasing the endogenous endothelial release of nitric oxide (acetylcholine, endothelin-1), and3) indirectly increasing smooth muscle cGMP concentrations by decreasing its rate of hydrolysis (zaprinast). We anticipated that all these drugs would decrease fetal pulmonary vascular resistance. We further expected that zaprinast would potentiate these decreases in fetal pulmonary vascular resistance.
METHODS
Animals and surgical preparation. The University of Florida Animal Research Committee approved the following procedures before the study began. Fetuses ranging in age from 136 to 143 d of gestation were exteriorized from the uterus by cesarean section while the ewe received i.v. chloralose anesthesia (initial dose 50 mg/kg followed by 10 mg/kg/h). Exposure of the umbilical cord was minimized by suturing the fetal chest and abdomen to the maternal skin. A tracheostomy was performed on the fetus, and the trachea was connected to a bag of saline so that air could not enter the lungs. A 1.0-mm internal diameter polyvinylchloride catheter was placed in the left femoral artery to allow systemic arterial pressure and heart rate monitoring. A 2.0-mm internal diameter polyvinylchloride catheter was placed through the femoral vein and the inferior vena cava so that the tip rested near the right atrial-inferior vena caval junction. Through a left lateral thoracotomy, a 1.0-mm internal diameter polyvinylchloride catheter was placed directly into the left atrium for left atrial pressure monitoring. The left pulmonary artery was cannulated with a 3.5-mm internal diameter polyethylene catheter. The proximal end of the left pulmonary artery was ligated and the ductus arteriosus was left intact.
After completing the instrumentation, the animal was given 200 U/kg heparin i.v. Maternal blood was used to fill 3.1-mm internal diameter silicone tubing connected to a Cole-Parmer Masterflex pump. One limb of this pump perfusion apparatus was connected to the catheter in the inferior vena cava, and the other limb was connected to a catheter in the left pulmonary artery. Blood from the inferior vena cava was then pumped into the left pulmonary artery. LPAP was measured through a side port in the left pulmonary artery catheter. The left pulmonary arterial inflow was adjusted during the first hour so that the LPAP was approximately 2-3 mm Hg above the SAP. The left pulmonary arterial inflow was thereafter maintained constant and measured using an in-line 4-mm diameter Transonic Systems (Ithaca, NY) flow probe. The animal's colonic temperature was maintained between 38 and 40°C using a heating pad and an infrared lamp.
Preparation of chemical agents. Chloralose(α-D-(+)-glucochloralose, Calbiochem, La Jolla, CA) was prepared as a 0.75% solution containing sodium chloride (0.58%) and sodium bicarbonate(0.42%). Solutions of 10 μg/mL acetylcholine were prepared by dissolving the crystalline salt (Sigma Chemical Co., St. Louis, MO) in 0.9% saline. Solutions of 1000 ng/mL endothelin-1 were prepared by dissolving the lyophilized powder (Peptides International, Louisville, KY) in 0.9% saline. Zaprinast (2-o-propoxyphenyl-8-azapurin-6-one; Rhône Poulenc, Essex, UK) was dissolved initially in 0.15 N sodium hydroxide to make a 3000μg/mL stock solution and then diluted as necessary with 0.9% saline. Nitric oxide solutions were prepared immediately before each experiment using a modification of the technique described by Feelisch(26). First, the solvents (0.9% saline and 95% ethanol) were chilled to 0°C. Then, pure nitrogen was bubbled through the solvents for 30 min. Finally, pure nitric oxide (Alphagaz, LaPorte, TX) was bubbled through the solvents for 10 min. Storage tubes for the nitric oxide solutions were filled to capacity, tightly sealed, and chilled until use.
Experimental procedure. The hemodynamic measurements were continuously monitored using a Gould 8 channel polygraph. The polygraph was connected to a personal computer using a Kiethley 570 data acquisition system permitting real time data analysis and subsequent data storage. Arterial blood pH, Pco2, and Po2 were measured hourly using a model 288 Ciba-Corning blood gas system. Hb and oxygen saturation measurements were also obtained hourly using a model OSM2 Radiometer Hemoximeter.
Experimental protocol . Dose-response to dilators. Fetuses were given, in random order, i.v. bolus injections of ethanol, normal saline, nitric oxide in ethanol, nitric oxide in saline, and zaprinast. All boluses were injected directly into the left pulmonary arterial circulation via the pump perfusion tubing. Ethanol, saline, and nitric oxide solutions ranged in volume from 3 to 300 μL. Doses of zaprinast ranged from 20 to 2000 μg. The number of injections given to the same animal was dependent upon the hemodynamic stability of the preparation; however, no animal received more than 10 injections. Injections were separated by at least a 5-min steady state after return of hemodynamic values to their respective baselines. The magnitudes of change in both LPAP and SAP were recorded. The time from the point of injection to the point when the LPAP response attenuates to half the peak response (LPAP t1/2) was also recorded.
Constant infusion of zaprinast and U46619. In a separate group of fetuses, nitric oxide in ethanol (10.0 μL), acetylcholine (1.0 μg), and endothelin-1 (100 ηg) were injected in random order into the lumen of the pump perfusion tubing. Eight fetuses were used for testing. Control injections of nitric oxide in ethanol and control injections of endothelin-1 were given to all fetuses. Control injections of acetylcholine were given to five of the fetuses. After the control injections were given to the animals, zaprinast(1.5 mg/min) was infused into the lumen of the pump perfusion tubing. This infusion dose was chosen because our prior experience suggested that it would produce a decrease in LPAP that was less than maximal. A continuous i.v. infusion of U46619 was started when the reduction in LPAP was observed to reach a steady state. The U46619 infusion rate was adjusted as necessary to return the LPAP to the steady state level that was recorded before infusing the zaprinast. Nitric oxide in ethanol (10.0 μL), acetylcholine (1.0μg), and endothelin-1 (100 ηg) were again injected in random order into the lumen of the pump perfusion tubing. The LPAP change, SAP change, and LPAPt1/2 were recorded during each bolus injection.
Statistical analysis. All data are presented as mean ± SEM. The LPAP change and SAP change versus the log10 dose for nitric oxide in saline, ethanol, nitric oxide in ethanol, and zaprinast were fitted to regression lines using the method of least squares. The LPAP dose-response regression line slopes and y intercepts were compared with the respective SAP dose-response regression line slopes and y intercepts using both a standard comparison of multiple regression lines and a Bonferroni correction. Using the same method, the LPAP dose-response regression line slope and y intercept for each of the following drugs-nitric oxide in saline, ethanol, and nitric oxide in ethanol-was compared with the regression line slope and y intercept for each other drug. Using paired t tests, the LPAP change, the SAP change, and the LPAP t1/2 for each drug injected during the constant zaprinast and U46619 infusions was compared with the respective values recorded before starting the infusions. A p value <0.05 was considered statistically significant.
RESULTS
Thirty-two fetal sheep (4.3 ± 0.2 kg; gestational age 141 ± 0.5 d) served as study subjects. The mean left pulmonary arterial inflow used was 80.6 ± 5.3 mL/min. Mean left atrial pressure and heart rate were unaffected by drug injections. Mean left atrial pressure measured 2.5 ± 0.1 mm Hg, and mean heart rate measured 212.7 ± 3.0 beats/min. Changes in femoral arterial blood pH, Pco2, Po2, and Hb were not noticeably affected by the bolus injections or by the constant infusions. Overall mean values for these parameters were as follows: pH 7.23 ± 0.01, Pco2 8.21 ± 0.11 kPa, Po2 3.03 ± 0.05 kPa, Hb 12.1 ± 0.1 mg/dL.
Dose response to dilators. The change in LPAP and SAP after injections of 3-300-μL aliquots of nitric oxide in saline, ethanol, and nitric oxide in ethanol are shown in Figure 1. LPAP decreased in a dose-dependent fashion after injections of nitric oxide in saline (LPAP change = -16.0 log10 dose +8.18, r2 = 0.96) and injections of nitric oxide in ethanol (LPAP change = -8.67 log10 dose -18.9, r2 = 0.93). Although LPAP decreased after injections of ethanol (LPAP change = 0.58 log10 dose -19.8,r2 = 0.035), the change was not dose-dependent in the range of volumes that was used. No change in LPAP or SAP was detected after injections of 3-300-μL aliquots of 0.9% saline. The changes in LPAP and SAP after injections of various doses of zaprinast are shown inFigure 2. LPAP decreased in a dose-dependent fashion using zaprinast (LPAP change = -11.2 log10 dose +14.4, r2 = 0.97). The LPAP dose-response regression line slopes for nitric oxide in saline and zaprinast were significantly different from their respective SAP dose-response regression line slopes (nitric oxide in saline: SAP change =-5.10 log10 dose +4.1, r2 = 0.61; zaprinast: SAP change = -1.40 log10 dose -1.9, r2 = 0.98). The LPAP dose-response regression line y intercepts for ethanol and nitric oxide in ethanol were significantly different from their respective SAP dose-response regression line y intercepts (ethanol: SAP change =-0.93 log10 dose +0.18, r2 = 0.56; nitric oxide in ethanol: SAP change = -6.52 log10 dose +4.63, r2 = 0.79). The LPAP t1/2 recorded after injections of nitric oxide in saline, ethanol, nitric oxide in ethanol, and zaprinast are shown inTable 1. The LPAP t1/2 was dose-dependent for each drug. For volumes greater than 10 μL, the LPAPt1/2 for nitric oxide in ethanol was longer than that for nitric oxide in saline. For each volume used, the LPAP t1/2 for both nitric oxide in ethanol and nitric oxide in saline was longer than that for ethanol.
Regression lines for nitric oxide in saline (NO Sal) dose, ethanol (Alc) dose, and nitric oxide in ethanol(NO Alc) dose vs change from baseline LPAP(circles) and change from baseline SAP (squares) are shown. Changes in LPAP are more than changes in SAP for all drugs. Changes in LPAP for NO Alc appear to reflect a summation of responses to Alc and responses to NO Sal. The number of injections is represented byn.
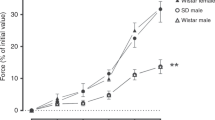
Constant infusion of zaprinast and U46619. The average U46619 dose required to return LPAP to the steady state level recorded before the zaprinast infusion was 1.4 μg/min. The LPAP immediately before infusing zaprinast was 61.9 ± 3.0 mm Hg, after infusing zaprinast for 10 min was 37.5 ± 2.7 mm Hg, and after infusing U46619 for 10 min was 64.3± 2.4 mm Hg. The SAP immediately before infusing zaprinast was 56.2± 3.6 mm Hg, after infusing zaprinast for 10 min was 48.1 ± 2.9 mm Hg, and after infusing U46619 for 10 min was 55.6 ± 3.6 mm Hg. The LPAP change, SAP change, and LPAP t1/2 after bolus injections of nitric oxide in ethanol, acetylcholine, and endothelin-1 are shown inFigure 3. For all drugs tested, the changes in LPAP and SAP during the zaprinast and U46619 infusions were not different from values recorded before the infusions. Similarly, the mean LPAP t1/2 values during the zaprinast and U46619 infusions were not different from values recorded before the infusions.
DISCUSSION
The decreases in pulmonary arterial pressure that occurred in response to bolus injections of zaprinast suggest that the resting fetal pulmonary vessels produce cGMP. These results support the finding of Abman and Accurso(25) that a cGMP signal transduction system is present in the fetus. These results also support the idea that cGMP modulates fetal pulmonary vascular tone. Although several investigators(13, 14) have shown that zaprinast is a highly selective inhibitor of cGMP phosphodiesterase, the possibility that zaprinast caused pulmonary vasodilation in our experiments by a mechanism other than cGMP modulation cannot be excluded.
A greater effect of the various bolus injections on pulmonary arterial pressure compared with the effect of bolus injections on systemic arterial pressure can be explained by a variety of mechanisms. These mechanisms include: drug target tissue specificity, short drug half-life, drug dilution by blood flowing across the foramen ovale and ductus arteriosus, and various placental circulation influences.
A comparison of nitric oxide pulmonary vasodilatory responses to zaprinast pulmonary vasodilatory responses reveals that equipotent doses of nitric oxide and zaprinast have different response durations. For example, the mean LPAP decrease caused by 600 μg of zaprinast injections (-18.7 mm Hg) was slightly less than the mean LPAP decrease caused by 3 μL of nitric oxide in ethanol injections (-20.7 mm Hg) and by 100 μL of nitric oxide in saline injections (-21.3 mm Hg). The mean LPAP t1/2 caused by 600-μg zaprinast injections (3.00 min) was markedly longer, however, than the mean LPAP t1/2 caused by both 3 μL of nitric oxide in ethanol injections (0.72 min) and 100 μL of nitric oxide in saline injections (1.40 min). These findings are consistent with both an inhibitory effect of zaprinast on cGMP hydrolysis and a cGMP-dependent vasodilatory mechanism for nitric oxide. If fetal responses to nitric oxide injections are caused by increased cGMP concentrations and if zaprinast and nitric oxide response magnitudes are proportional to the respective increases in sarcoplasmic cGMP concentrations, then the vasodilatory response to an injection of zaprinast should (as our findings suggest) last longer than the vasodilatory response to an equipotent injection of nitric oxide.
We were unable to demonstrate that zaprinast affects the responses to bolus injections of nitric oxide in ethanol, acetylcholine, and endothelin-1. The inability to potentiate responses to nitric oxide in ethanol with zaprinast was surprising, because we found that nitric oxide in ethanol injections cause fetal pulmonary vasodilation by at least two mechanisms. The inability to potentiate acetylcholine-induced pulmonary vasodilatory responses with zaprinast was also surprising because this potentiation has been shown in cats(17) and lambs(16). Because transduction of endothelin-1-induced fetal pulmonary vascular dilation partly involves enhanced endogenous synthesis of nitric oxide(27), we were again surprised because zaprinast did not augment the vasodilator response to endothelin-1.
Because the responses to ethanol alone were maximal over the entire range of used volumes and because solubilized nitric oxide augmented the responses to ethanol suggests the presence of more than one fetal pulmonary vasodilatory mechanism. Response magnitudes for nitric oxide dissolved in ethanol seem to reflect an additive effect estimated from ethanol dose-response curves and from nitric oxide in saline dose-response curves. Nitric oxide in ethanol response durations clearly resulted from more than simply the sum of ethanol response durations and nitric oxide in saline response durations. Responses to nitric oxide in ethanol were expected to be greater than the sum of the independent effects of ethanol and nitric oxide in saline because nitric oxide is more soluble in ethanol (13.7 mM/L at 0°C) than it is in saline (2.05 mM/L at 0°C). At volumes ranging from 30 to 300 μL, the ratios of the nitric oxide in ethanol response durations to the nitric oxide in saline response durations (6.58/1.08, 10.29/1.40, and 17.07/3.22) resemble the ratio of the nitric oxide solubility coefficient for ethanol to the nitric oxide solubility coefficient for saline (13.7/2.05). This finding suggests that the duration of the response to injections of nitric oxide solubilized in saline and ethanol is directly proportional to the amount of delivered nitric oxide.
cGMP-independent mechanisms that may be involved in fetal pulmonary vasodilator responses to nitric oxide in ethanol, acetylcholine, and endothelin-1 include the following: selective cAMP modulation, sarcolemmal hyperpolarization, and electron transport inhibition. Nitric oxide, for example, can increase both cAMP and cGMP concentrations in gut smooth muscle cytoplasm(28). Some studies have shown that nitric oxide-releasing compounds, such as nitrovasodilators, cause nonselective increases in cAMP concentrations(29, 30). Potassium channel activation causes hyperpolarization of the sarcolemma which in turn causes vasodilation, at least in some instances, by cyclic nucleotide-independent mechanisms. Nitric oxide(31–34), other nitrovasodilators(34–38), acetylcholine(39, 40), and endothelin-1(41, 42) have all been shown to activate potassium channels. Recently, Bolotina and et al.(43) reported that nitric oxide activates potassium channels of isolated smooth muscle cells by cGMP-independent mechanisms. That potassium channel activation mechanisms are at least partially responsible for fetal pulmonary vasodilation with injections of nitric oxide in ethanol, acetylcholine, and endothelin-1 seems plausible. Furthermore, in vitro studies revealed that heme prosthetic groups of electron transport chain cytochromes reversibly bind nitric oxide(44) and that this binding of nitric oxide to the cytochromes reversibly inhibits electron transport activity(45). We propose, therefore, that nitric oxide may even attenuate vascular smooth muscle contraction by simply inhibiting mitochondrial electron transport activity.
We conclude that late gestation fetal sheep tonically produce cGMP in their pulmonary vascular bed. We further conclude that modulation of their pulmonary vascular tone by exogenously administered acetylcholine, endothelin-1, and nitric oxide at least partially involves cGMP-independent mechanisms. Therefore, we believe that late gestation fetal sheep (and possibly human) pulmonary vasodilation by endogenously produced nitric oxide may involve cGMP-independent mechanisms.
Abbreviations
- LPAP:
-
mean left pulmonary arterial pressure
- SAP:
-
mean systemic arterial pressure
- LPAPt1/2,:
-
time from point of injection to point when LPAP response attenuates to half peak response
References
Enhorning G, Adams FH, Norman A 1966 Effect of lung expansion on fetal lamb circulation. Acta Paediatr Scand 55: 441–451
Reynolds SR 1956 The fetal and neonatal pulmonary vasculature in the guinea pig in relation to hemodynamic changes at birth. Am J Anat 98: 97–127
Cook CD, Drinker PA, Jacobson HN, Levinson H, Strang LB 1963 Control of pulmonary blood flow in the foetal and newly born lamb. J Physiol 169: 10–29
Lauer RM, Evans JA, Aoki H, Kittle CF 1965 Factors controlling pulmonary vascular resistance in fetal lambs. J Pediatr 67: 568–577
Cassin S 1981 Prostaglandins and the perinatal pulmonary circulation. In: Mehta J, Mehta P (eds) Platelets and Prostaglandins in Cardiovascular Disease. Futura Publishing, New York, pp 219–249
Leffler CW, Hessler JR, Green RS 1984 The onset of breathing at birth stimulates pulmonary vascular prostacyclin synthesis. Pediatr Res 18: 938–942
Davidson D 1988 Pulmonary hemodynamics at birth: effect of acute cyclooxygenase inhibition in lambs. J Appl Physiol 64: 1676–1682
Griffith TM, Edwards DH, Lewis MJ, Henderson AH 1985 Evidence that cyclic guanosine monophosphate (cGMP) mediates endothelium-dependent relaxation. Eur J Pharmacol 112: 195–202
Waldman SA, Murad F 1988 Biochemical mechanisms underlying vascular smooth muscle relaxation: the guanylate cyclase-cyclic GMP system. J Cardiovasc Pharmacol 12( suppl 5): S115–S118
Arnold WP, Mittal CK, Katsuki S, Murad F 1977 Nitric oxide activates guanylate cyclase and increases guanosine 3,5-cyclic monophosphate levels in various tissue preparations. Proc Natl Acad Sci USA 74: 3203–3207
Ignarro LJ, Kadowitz PJ 1985 The pharmacological and physiological role of cyclic GMP in vascular smooth muscle relaxation. Annu Rev Pharmacol Toxicol 25: 171–191
Holzman S 1982 Endothelium-induced relaxation by acetylcholine associated with larger rises in cyclic GMP in coronary arterial strips. J Cyclic Nucleotide Res 8: 409–419
Martin W, Furchgott RF, Villani GM, Jothianandan D 1986 Phosphodiesterase inhibitors induce endothelium-dependent relaxation of rat and rabbit aorta by potentiating the effects of spontaneously released endothelium-derived relaxing factor. J Pharmacol Exp Ther 237: 539–547
Souness JE, Brazdil R, Diocee BK, Jordan R 1989 Role of selective cyclic GMP phosphodiesterase inhibition in the myorelaxant actions of MB 22948, MY-5445, vinpocetine and 1-methyl-3-isobutyl-8-(methylamino)xanthine. Br J Pharmacol 98: 725–734
Hidaka H, Tanaka T, Itoh H 1984 Selective inhibitors of three forms of cyclic nucleotide phosphodiesterases. Trends Pharmacol Sci 5: 237–239
Braner DAV, Fineman JR, Chang R, Soifer SJ 1993 MB 22948, a cGMP phosphodiesterase inhibitor is a pulmonary vasodilator in lambs. Am J Physiol 264:H252–H258
McMahon TJ, Ignarro LJ, Kadowitz PJ 1993 Influence of Zaprinast on vascular tone and vasodilator responses in the cat pulmonary vascular bed. J Appl Physiol 74: 1704–1711
Trapani AJ, Smits GJ, McGraw DE, McMahon EG, Blaine EH 1991 Hemodynamic basis for the depressor activity of zaprinast, a selective cGMP phosphodiesterase inhibitor. J Pharmacol Exp Ther 258: 269–274
Kukovetz WR, Holzmann S, Wurm A, Poch G 1979 Evidence for cyclic GMP-mediated relaxant effects of nitro-compounds in coronary smooth muscle. Naunyn-Schmiedebergs Arch Pharmacol 310: 129–138
Tiktinsky MH, Morin FC 1993 Increasing oxygen tension dilates fetal pulmonary circulation via endothelium-derived relaxing factor. Am J Physiol 265:H376–H380
McQueston JA, Cornfield DN, McMurtry IF, Abman SH 1993 Effects of oxygen and exogenous L-arginine on EDRF activity in fetal pulmonary circulation. Am J Physiol 264:H865–H871
Abman SH, Chatfield BA, Rodman DM, Hall SL, McMurtry IF 1991 Maturational changes in endothelium-derived relaxing factor activity of ovine pulmonary arteries in vitro. Am J Physiol 260: L280–L285
Chang JK, Moore P, Fineman JR, Soifer SJ, Heymann MA 1992 K+ channel pulmonary vasodilation in fetal lambs: role of endothelium-derived nitric oxide. J Appl Physiol 73: 188–194
Shaul PW, Farrar MA, Zellers TM 1992 Oxygen modulates endothelium-derived relaxing factor production in fetal pulmonary arteries. Am J Physiol 262: H355–H364
Abman SH, Accurso FJ 1991 Sustained fetal pulmonary vasodilation with prolonged atrial natriuretic factor and GMP infusions. Am J Physiol 260:H183–H192
Feelisch M 1991 The biochemical pathways of nitric oxide formation from nitro vasodilators: appropriate choice of exogenous NO donors and aspects of preparation and handling of aqueous NO solutions. J Cardiovasc Pharmacol 17( suppl 3): S25–S33
Tod ML, Cassin S 1992 Endothelin-1-induced pulmonary arterial dilation is reduced by N-nitro-L-arginine in fetal lambs. J Appl Physiol 72: 1730–1734
Chakder S, Rattan S 1993 Involvement of cAMP and cGMP in relaxation of internal anal sphincter by neural stimulation, VIP, and NO. Am J Physiol 264:G702–G707
Maurice DH, Haslam RJ 1990 Nitroprusside enhances isoprenaline-induced increases in cAMP in rat aorta smooth muscle. Eur J Pharmacol 191: 471–475
Maurice DH, Haslam RJ 1990 Molecular basis of the synergistic inhibition of platelet function by nitrovasodilators and activators of adenylate cyclase: inhibition of cAMP breakdown by cGMP. Mol Pharmacol 37: 671–681
Miyoshi H, Nakaya Y, Moritoki 1994 Nonendothelial-derived nitric oxide activates the ATP-sensitive K+ channel of vascular smooth muscle cells. FEBS Lett 345: 47–49
Tare M, Parkington HC, Coleman HA, Neild TO, Dusting GJ 1990 Hyperpolarization and relaxation of arterial smooth muscle caused by nitric oxide derived from the endothelium. Nature 346: 69–71
Krippeit-Drews P, Morel N, and Godfraind T 1992 Effect of nitric oxide on membrane potential and contraction of rat aorta. J Cardiovasc Pharmacol 20( suppl 12): S72–S75
Williams DL, Katz GM, Roy-Contancin L, Reubin JP 1988 Guanosine 5-monophosphate modulates gating of high-conductance Ca2+-activated, K+ channels in vascular smooth muscle cells. Proc Natl Acad Sci USA 85: 9360–9364
Fujino K, Nakaya S, Wakatsuki T, Miyoshi Y, Nakaya Y, Mori H, Inoue I 1991 Effects of nitroglycerin on ATP-induced Ca2+-mobilization, Ca2+-activated K channels and contraction of cultured smooth muscle cells of porcine coronary artery. J Pharmacol Exp Ther 256: 371–377
Itoh Y, Suzuki H, and Kuriyama H 1978 Effects of sodium nitroprusside on smooth muscle cells of rabbit pulmonary artery and portal vein. J Pharmacol Exp Ther 207: 1022–1031
Cheung DW, MacKay MJ 1985 The effects of sodium nitroprusside and 8-bromocyclic GMP on electrical and mechanical activities of the rat tail artery. Br J Pharmacol 86: 117–124
Itoh Y, Kitamura K, and Kuriyama H 1978 Actions of nitroglycerine on the membrane and mechanical properties of smooth muscles of the coronary artery of the pig. Br J Pharmacol 70: 197–204
Brayden JE, Large WA 1986 Electrophysiological analysis of neurogenic vasodilatation in the isolated lingual artery of the rabbit. Br J Pharmacol 89: 163–171
Kitamura K, Kuriyami H 1979 Effects of acetylcholine on the smooth muscle of isolated main coronary artery of the guinea-pig. J Physiol 293: 119–133
Lippton HL, Cohen GA, McMurtry IF, Hyman AL 1991 Pulmonary vasodilation to endothelin isopeptides in vivo is mediated by potassium channel activation. J Appl Physiol 70: 947–952
Hasunuma K, Rodman DM, O'Brien RF, McMurtry IF 1990 Endothelin 1 causes pulmonary vasodilation in rats. Am J Physiol 259:H48–H54
Bolotina VM, Najibi S, Palacino JJ, Pagano PJ, Cohen RA 1994 Nitric oxide directly activates calcium-dependent potassium channels in vascular smooth muscle. Nature 368: 850–853
Blokzijl-Homan MF, Van Gelder BF 1971 Biochemical and biophysical studies in cytochrome aa3. III. The EPR spectrum of NO-ferrocytochrome a3. Biochim Biophys Acta 234: 493–498
Cleeter MW, Cooper JM, Darly-Usmar VM, Moncada S, Schapira AH 1994 Reversible inhibition of cytochrome c oxidase, the terminal enzyme of the mitochondrial respiratory chain, by nitric oxide: implications for neurodegenerative diseases. FEBS Lett 345: 50–54
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Skimming, J., DeMarco, V., Kadowitz, P. et al. Effects of Zaprinast and Dissolved Nitric Oxide on the Pulmonary Circulation of Fetal Sheep. Pediatr Res 39, 223–228 (1996). https://doi.org/10.1203/00006450-199602000-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199602000-00006