Abstract
The objective of this study was to establish longitudinal normative limits for home memory monitors during early infancy. Eighty-eight healthy infants were monitored overnight at 0.25-19 wk of age using the Healthdyne Smart Monitor. Apnea settings were 14 s for recording and 40 s for alarm; the bradycardia setting was 50 beats/min (5-s delay) for both recording and alarm. Arterial oxygen saturation (Sao2) was documented whenever an event was recorded. The monitor was used 77% of all possible days; median daily use was 8.0 h. Eighty-three percent of all monitor alarms were caused by loose leads, the other 17% by false apnea or false bradycardia. Of all recorded events, 68.9% were caused by false apnea or false bradycardia; the other 31.1% were central apneas that reached the recording threshold of 14 s. The longest apnea was 36 s (wk 1); the 95th percentile for longest apnea was 19.9 s in wk 1 and 18.0 s in wk 17-19 (p < 0.001). Periodic low Sao2 values occurred with periodic breathing; the lowest value was 72%. The 5th percentiles for lowest Sao2 were 82 and 86% in wk 1 and 13-19, respectively (p < 0.001), but the minimum value observed in any week was never >81%. The median duration of Sao2 < 90% was only 5 s but the range was wide (1-183 s), and 39/527 episodes (7.4%) were >10 s. In summary, these longitudinal data provide the first available normal limits for cardiorespiratory pattern and Sao2 during documented home monitoring in early infancy. Utilization of these normative data will improve the diagnostic validity and clinical usefulness of event recordings.
Similar content being viewed by others
Main
The development of memory monitors now permits accurate differentiation of true apnea and true bradycardia events from false alarms(1, 2). Based on the early clinical experiences with documented monitoring, only 8-20% of alarms in the home are indicative of true apnea or bradycardia. Just identifying the number of true or clinically significant alarms, however, is not sufficient; all of the true events recorded need to be interpreted in the context of established age-adjusted normative data, data which has heretofore not existed.
Home monitors are commonly prescribed for the surveillance of infants at risk for a life-threatening event (apnea of infancy). Despite recommendations to the contrary(3), monitors are also prescribed for infants in the hope that SIDS can be prevented. Normative home monitoring data are urgently needed in infants to better understand the boundaries between normal cardiorespiratory occurrences and events of potential clinical significance. Further, although an O2 saturation (Sao2) channel can now be integrated, we have only limited normative Sao2 data in early infancy in the home.
The following study was designed to obtain normative data for apnea, heart rate, and Sao2 events in healthy full-term infants during the first 19 wk of life. Using a state-of-the-art home documented monitoring system, these parameters were monitored longitudinally during nocturnal sleep.
METHODS
Selection of patients. Healthy infants were recruited from prenatal classes and from the Newborn Nursery. The criteria for eligibility included: gestational age 38-42 wk and birth weight 10th-90th percentile; Apgar score >6 at 5 min; absence of any respiratory symptoms in the Nursery and of any medical condition delaying discharge beyond maternal discharge; no congenital anomaly with increased potential for infant mortality; no clinical evidence of congenital heart disease; no history of an unexpected infant sibling death; and no history of maternal substance abuse. Informed consent was obtained. The study protocol was approved by the Institutional Review Board.
Study design. Families were instructed to monitor their infant daily during all nocturnal sleep. No alterations in the protocol were made for immunizations or for routine febrile illness. A home visit occurred within the first 24 h after discharge. Telephone contact with the family occurred 2-3 times during the 1st wk, weekly through the 1st mo, and then twice/mo for the duration of the study.
The memory monitor system used was the Healthdyne 970-S Smart Monitor(Healthdyne Corp,, Atlanta, GA) with the integrated 930 Pulse Oximeter (Nonin Medical, Minneapolis, MN). The five monitor channels included respiration(transthoracic impedance), ECG, ECG-derived heart rate, pulse rate derived from the oximeter, and Sao2. We used black carbon hydrogen patch electrodes (no. 3200B, Special Medical Products, Santa Anna, CA). The pulse oximeter probe was placed on the sole of the foot at the base of the toes and secured with Coban tape. The digital display of Sao2 on the front panel was deactivated to avoid any parental concerns based on the numerical values. To avoid frequent false desaturation alarms, a nontriggering cable was used; consequently, Sao2 was recorded whenever an event was triggered by apparent apnea or bradycardia, but a recorded event could not be triggered by the Sao2 signal. The recorded Sao2 values represent a 4-pulse moving average updating beat-to-beat. The heart rate trend from the ECG signal updates beat-to-beat.
The memory monitor settings for apnea were 14 s for recording and 40 s for alarm. The bradycardia threshold for both recording and alarm was 50 beats/min, with a 5 s delay. Whenever a threshold setting for apnea or bradycardia record was exceeded, the memory monitor stored the five channels of data for the preceding 30 s, during the event, and for 60 s after the event.
The stored data were retrieved from each monitor at monthly intervals and were transferred to hard copy using the Healthdyne computer and recording system. Each download was reviewed to quantify hours of monitor use and to identify any excessive false alarms.
Outcome measures. All recordings were hand scored and reviewed by at least two of the authors. To be scored as a breath, the amplitude had to be >25% of the baseline. Apnea duration was scored as peak-to-peak. LARS was defined as a prolonged period of minimal baseline variation in the respiratory signal without any bradycardia. Each apnea >13 s was scored. A pulse deceleration was scored whenever the heart rate decreased >20 beats/min as part of an event. Sao2 decreases were scored as artifact whenever the oximeter-derived pulse rate was less than the ECG-derived heart rate. All true Sao2 values <90% and <81% were noted, including the total time below the threshold, the minimum value reached, and the duration <90% and <81%.
The downloads from each infant were scored only after discharge from the study. Respiratory events, pulse decelerations, Sao2 events, and any false events (LARS or movement artifact) were tabulated for each day of life monitored. Monitor usage (compliance) was summarized as the percent of total days in the home that the monitor was actually used; for those days used, the hours used/d were determined from the Monitoring Compliance Report.
Statistical analysis. Descriptive statistics (percentages) were calculated on the demographic variables related to family characteristics. Both descriptive statistics and one-way analysis of variances with Bonferroni's post hoc tests were used to analyze the physiologic data. Totals, frequencies, percentages, percentiles, medians, and means were calculated for the different types of events. Because infants were monitored for a variable number of hours/d and days/wk, data were normalized to the median daily duration of 8.0 h and to 7 d/wk, and thus expressed as frequency/56 h. Descriptive statistics were calculated on the normalized data. Graphing techniques were used to visualize the changes in frequency of each type of event. One-way analysis of variances with Bonferroni's post hoc tests were used to determine differences in means for longest apnea and lowest Sao2 level during each week of age. The level of significance was set at p < 0.05.
RESULTS
Characteristics of infants. Study enrollment occurred from August 1990 through May 1993. Of the 146 families initially enrolled, four infants were never monitored (2.7%), 53/141 (37.6%) did not complete the first full week of monitoring, and one infant was later excluded from the study due to symptomatic gastroesophageal reflux. This report is based on the 88 infants who were still being monitored at the end of the 1st wk of age. Seventy-five infants completed the 5th wk of age, 67 the 13th wk, and 42 the 19th wk(Table 1). None of the 88 infants had any observed episode of cyanosis or respiratory distress during infancy, and all 88 infants were alive and healthy at 1 y of age.
The 88 infants included 5 African-American infants (5.7%) and 1 Latino(1.1%). Maternal smoking history was ascertained in the last 68/88; 9% of these 68 mothers smoked. Intended sleep position was ascertained at enrollment in the last 44 subjects; the prone position was intended in 80%. Mean birth weight was 3470 g (SD 440), range 2620-4645 g; 56% were girls.
Compliance. Families used the monitor 77% of all days in the home, resulting in 10 093 d and 78 430 h of memory monitoring. For all days used, median use/d (compliance) was 8.0 h (range 1-24) and mean use was 7.8 h(SD 3.3).
Alarms. There were no true alarms caused by threshold violation in any infant. For the total of 2552 alarms, 2114 (83%) were loose lead alarms. Loose lead alarms have a different sound and do not generate a hard copy event, but are listed in the event log generated with each download. The other 438 alarms (17%) did generate a hard copy recording; the reasons for a false alarm included LARS as well as false apnea or bradycardia caused by movement artifact.
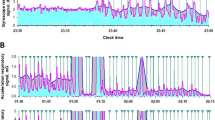
Only 1/63 infants completing 16 wk (1.6%) and 1/42 infants completing 19 wk(2.4%) never had an alarm. Three infants had >100 alarms; the median number of alarms/infant was 16.5 and the maximum was 197. Expressed as the frequency per infant/normalized week of 56 h, the 95th percentiles are summarized for each week of age (Fig. 1A). The ratio of loose lead to other alarms was comparable during all 19 wk. Comparing the 75 infants who were still being monitored at the end of 5 wk of age to the 13 infants who dropped out after the 1st wk but before the end of the 5th wk, there were no differences in the frequency of alarms/normalized week.
Frequencies per infant per normalized week(frequencies/56 h/wk). The 50th percentiles are zero; the top of each solid bar and each open bar represents the 95th percentile. None of these differences across weeks is statistically significant. A, All alarms, subdivided into loose lead and other alarms; 83% of all alarms were loose lead alarms. B, All apneas >13 s subdivided into 14-19 and>19 s. No episodes >19 s occurred after 17 wk of age (seeFig. 3). C, All Sao2 events <90%, subdivided into 81-89% and <81%. All of the events <81% are brief, and most occur within the 1st mo of age.
All recorded events. A total of 5822 events were recorded. The median number of total events/infant was 36 (range 1-320). Of the total 5822 events, 68.9% were false events caused by movement artifact or LARS. Only 1/63 infants completing 16 wk (1.6%) and 1/42 completing 19 wk of home monitoring(2.4%) never had a recorded event. Comparing the 75 infants still being monitored at the end of the 5th wk to the 13 infants who completed the 1st wk but withdrew before the end of the 5th wk, there were no differences in the frequency of 14-19 s or >19 s apnea, or in the frequency of Sao2 values <90% or <81%. We therefore included in our analysis of each week of age all infants completing that week of monitoring.
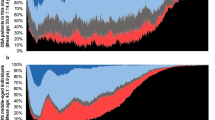
Apnea events. There were no apneas >39 s and therefore no true apnea alarms. However, 1809/5822 recorded events (31.1%) were apnea events >13 s. The median number of all scored apneas >13 s/infant was 8(range 1-272), with 46 infants having <10 and 1 infant having >100 apneas. Of all apneas >13 s 39.5% appeared to be part of a periodic breathing episode (Fig. 2). The 95th percentiles for the frequency of apneas >13 s/normalized week are summarized for each week of age (Fig. 1B).
Thirty-nine of 1809 episodes of apnea >13 s (2.2%) were >19 s. Most occurred in the first 3 wk (Fig. 3), but two apneas 20 s in duration occurred in wk 16 and in wk 17. The three longest episodes of apnea were associated with a single chest wall movement in the middle(Fig 4); if these respiratory efforts were counted as breaths, then the longest apnea would be 25 s occurring in the 2nd and in the 3rd wk. Three hundred and ninety of 1809 apneas >13 s (21.6%) were accompanied by Sao2 values <90% and 19/1809 apneas (1.1%) by Sao2 values <81%. The mean duration of all apneas >13 s in wk 3-4(Table 2) was lower than the mean duration for wk 1(p =.018), but this difference is not clinically significant.
Bradycardia Events. There were no transient heart rates <51 beats/min and no episodes of heart rate <80 beats/min for >5 s. Of the total 1809 apnea events, 691 (38.2%) were accompanied by heart rate deceleration but none by bradycardia. Consequently, all of the apparent bradycardia events were false events.
Sao2 events. There was no measurement of Sao2 unrelated to monitoring and none during monitoring except when an event was triggered by apparent apnea or bradycardia. As part of the scoring of these apparent apnea/bradycardia events, 544 events were identified in which Sao2 decreased to <90%. The median number/infant was 4 (range 0-97), with 30 infants having none and 3 infants having >22. When expressed as frequency per infant per normalized week (Fig. 1C), most occurred in the first 5 wk; as with alarms and apneas, the highest frequency occurred in the 1st wk.
The median duration of Sao2 <90% was 5 s; the range was 1-183 s, with only 50/522 episodes (9.6%) >10 s and 2/522 episodes >100 s (0.4%). Because some of these low Sao2 values were present at the beginning of the recorded event or still present at the end (Fig. 5), these observed durations represent minimum values.
Example of prolonged Sao2 levels <90% in an infant at age 15 d. This is a false apnea event, caused by a LARS. The Sao2 was <90% for at least 183 s; the minimum value was 85%. Because the Sao2 level was already <90% at the onset of the recorded event, the scored duration represents the minimum possible duration.
There were 22/544 desaturation events (4%) in which the lowest Sao2 level was <81%; 14/22 (64%) were <80% (Fig. 1C). The<81% and <80% events occurred in 12 and 9 infants, respectively. One infant had 6 events <81% and 4 events <80%. Most of these saturation values <81% were brief, and 11/14 episodes <80% were periodic and associated with periodic breathing (Fig. 2). Among the 14 episodes <80%, the median duration <80% was 3 s (range 1-7 s), and the 5th percentile for lowest Sao2 was 72% (range 72-78%). For these same 14 episodes <80%, the total median duration <90% was 13 s, and the range was 7-43 s. The lowest Sao2 value observed each week and the 5th and 50th percentiles of the lowest Sao2 value/infant for each week(Table 2) did not differ statistically as the infants matured from 1 to 19 wk of age. There were no parental reports of any dusky or cyanotic episodes, whether related or unrelated to monitor alarms or occurring after discontinuing the home monitor.
DISCUSSION
We provide the first normative data for documented home monitoring, obtained longitudinally through the peak age for SIDS. Before the availability of documented monitoring, normative studies of home monitoring were not feasible; a perception of “disease” would be created whenever a healthy infant had an alarm, and there would be no hard copy of the event to confirm absence of a potentially significant event. Only one family reported concern about one monitor alarm of possible clinical significance, but alarms other than loose lead alarms occurred at all ages (Fig. 1A) and in 97.6% of all infants completing the 19 wk. A perception of disease would thus have been created had we been unable to review a hard copy of each event and to identify artifact as the cause of each event-related alarm. All of the families completing the protocol were comfortable in discontinuing home monitoring at the allotted time.
Compliance. Satisfactory compliance in middle class families can be achieved using state-of-the art documented monitoring technology including Sao2, even in the absence of clinical indication. Because it is not possible to determine the efficacy of home monitoring if the extent of monitor use cannot be quantified, verification of compliance is of critical importance to the more global question of whether home monitor use can reduce the morbidity and/or mortality of life-threatening events. Indeed, in retrospective interviews of SIDS families in whom a monitor was in the home, only 21% reported compliance with the medical regimen(4).
Apnea. Several investigators have published normative pneumogram data for the frequency and duration of central apneas. In four separate studies, the longest apnea in infants did not exceed 14-15 s(5–8), although central apneas as long as 17 s were observed in healthy children at 12-18 mo of age(9). Using different technology for pneumogram recordings, central apneas as long as 21.7 s were observed in the 1st wk, but no apneas>18 s were observed after 7 d of age(10, 11). In contrast, however, a study of breathing patterns in healthy children 2-16 y of age observed apneas as long as 28.8 s(12), which is more consistent with our observations in young infants.
Normative values from different studies cannot be considered interchangeable. Even if the equipment is identical, the scoring algorithms are never standardized and interobserver reliability cannot be assumed. Investigators are divided as to whether single chest wall movements interrupting central apnea should be scored as two separate apneas or one prolonged apnea, in part due to the consideration that such intervening efforts may be obstructive. We have therefore presented the data both ways; the longest apnea is 36 s using our definition (Fig. 4), but would be 25 s if the alternative definition is used and the apneas of 29, 30, and 36 s are thus subdivided (Fig. 3).
Normative data derived from documented home monitoring may be more representative of the full range of normal than data derived from pneumograms. Whereas pneumograms are typically recorded for just 12-24 h, documented monitoring permits substantially longer durations of observation. Compared with a median total of 860 h/infant in this study, the mean observation time in a previous pneumogram study in normal infants(6) was only 20.1 h, a mere 2.2% of the mean time/subject in this documented monitoring study. A final potential explanation for the greater extent of prolonged apnea in healthy infants in this study is that longer apneas may be a normal occurrence after the 1st wk of age; we have significantly more data after the 1st wk and through 4 mo of age than the normative pneumogram studies. Indeed, 31/39 of the apneas >19 s (79%) did occur after the 1st wk of age (Fig. 3). Our normative results are also consistent with two reports of documented monitoring in older infants and young children(to 15 y) monitored for clinical indications(13, 14), in whom apneas >20 s unassociated with any bradycardia or desaturation did occur but did not preclude successful discontinuation of home monitoring.
Bradycardia. Bradycardia has not been studied to the same extent in healthy infants as has apnea. Transient episodes of bradycardia to 60-70 beats/min are common in polysomnogram recordings at 1-6 mo of age(15), but no studies have observed bradycardia episodes of 50 beats/min or less. Similarly, we observed no transient episodes of heart rate <51 beats/min and no heart rates <80 beats/min for >4 s. The absence of bradycardia in healthy infants is especially relevant considering the recent documentation of bradycardia occurring at or before the onset of central apnea in death recordings of SIDS victims(16).
Oxygen saturation (Sao2). Normative longitudinal infant data are very limited in the home setting(12, 17). Overnight pneumogram recordings at 29-54 d of age in healthy infants, using a modified Nellcor pulse oximeter (N100), yielded an Sao2 range of 97-100% (median 99.8%) during regular breathing(17). In 54/67 recordings (81%), however, there was a median of 0.9 episodes/h in which Sao2 transiently decreased to <81%, with the median duration <81% being 2.4 s (range 0.3-8.6 s). Periodic breathing was noted in 49% of infants, and the frequency and duration of Sao2 values <81% were significantly greater in periodic compared with nonperiodic breathing.
It is not technically possible to calibrate pulse oximeters, and systematic differences between different brands have been reported(18). Comparisons of the Healthdyne 930 pulse oximeter with the Nellcor (N) pulse oximeters, however, have not demonstrated any clinically significant differences; saturation values are somewhat lower than either the N-100 and N-200, but the median difference of Healthdyne 930 Sao2 values is only 0.1% above co-oximeter values (range -4.0 to 3.5), whereas the median difference of N-200 Sao2 values is 3.0% higher(range -12.9 to 3.9) than the actual co-oximeter readings(19). There are no previous reports of normative Sao2 values using equipment comparable to ours, and no normative data throughout the first 4 mo of age using any technology. Although the technology and recording algorithms are quite different, our results are similar to previous data(17).
Our observations of periodic lower Sao2 levels associated with periodic breathing (Fig. 2) are consistent with previous data(17). We were surprised, however, by the prolonged durations of Sao2 <90% (Fig. 5). The fact that the longest durations were associated with LARS suggests that LARS may at least in some instances be indicative of hypopnea.
Potential limitations. There are several potential limitations to this study. To explain the longer apnea and lower Sao2 values than anticipated, one potential explanation is that not all infants were truly healthy. Because our subjects were completely healthy by history and examination before enrollment and were consistently healthy by history after study completion, we consider them to be representative of healthy infants. Consequently, we consider our observations to be representative of what occurs in healthy infants undergoing surveillance of this nature and duration. A second potential limitation is related to the absence of nonevent data between the recorded events. Although there is no reason to speculate that any clinically significant apnea or bradycardia was missed, we did not set a record/alarm threshold for Sao2 and therefore cannot make any assumptions as to the occurrence and severity of isolated Sao2 decreases.
A third potential limitation is that these normative data were obtained using only one of the commercially available systems. Because the results might be different using different equipment, our normative data cannot be assumed to be equally valid for other recording technologies. A fourth potential limitation is our protocol decision to restrict monitoring to nocturnal sleep. Because assessment during daytime naps significantly underestimates the cardiorespiratory events occurring during nocturnal sleep(20), however, the inclusion of daytime sleep would not increase the extent of prolonged apnea and lower Sao2 levels.
Our final limitation is a technologic one related to our inability to detect obstructive apnea. Although mixed and obstructive apneas may be important components of clinically significant events, no monitors currently used in the home can detect obstructive apnea because they all depend on transthoracic impedance, detecting small impedance changes as air enters and leaves the lungs, and interpreting these impedance variations as breaths. Impedance monitors are incapable of detecting obstructive apnea because diaphragmatic contraction against a closed upper airway still causes an impedance change that is misinterpreted as a breath. Our normative data thus pertain only to central apnea; normative standards for mixed and obstructive apnea await the availability of a home memory monitor that can detect obstructive as well as central apnea.
In summary, we report normative data for young infants using state-of-the-art technology for home documented monitoring. Eighty-three percent of all alarms were loose lead, and the remaining 17% were false alarms. Sixty-nine percent of all recorded events were false, and apnea >13 s explained the other 31%. Depending on apnea definition, prolonged apneas as long as 25-36 s occur in the 1st mo of age and apneas >19 s occur through the first 17 wk. Heart rates <80 beats/min for >5 s do not occur. Periodic decreases in Sao2 as low as 72% occur with periodic breathing, but no prolonged Sao2 values <85% are evident. Sao2 levels of 85-89% lasting at least 3 min, however, are evident in association with minimal fluctuations in thoracic impedance (LARS). These normative data will be essential for the utilization of documented monitoring as a diagnostic modality and for the interpretation of documented events in patients.
Abbreviations
- LARS:
-
low amplitude respiratory signal
- Sao2,:
-
arterial oxygen saturation (%)
- SIDS:
-
sudden infant death syndrome
REFERENCES
Weese-Mayer DE, Brouillette RT, Morrow AS, Conway LP, Klemka-Walden LM, Hunt CE 1989 Assessing validity of infant monitor alarms with event recording. J Pediatr 115: 702–708
Nathanson I, O'Donnell JO, Commins MF 1989 Cardiorespiratory patterns during alarms in infants using apnea/bradycardia monitors. Am J Dis Child 143: 476–480
National Institutes of Health Consensus Development Conference on Infantile Apnea and Home Monitoring 1987 Pediatrics 79: 292–299
Kelly DH 1992 Home monitoring. In: Beckerman RC, Brouillette RT, Hunt CE (eds) Respiratory Control Disorders in Infants and Children. Williams & Wilkins, Baltimore, pp 400–412
Southall DP, Richards JM, de Swiet M 1983 Identification of infants destined to die unexpectedly during infancy: evaluation of predictive importance of prolonged apnoea and disorders of cardiac rhythm or conduction. First report of a multicentered prospective study into the sudden infant death syndrome. BMJ 286: 1093–1096
Hunt CE, Brouillette RT, Hanson D, David RJ, Stein IM, Weissbluth M 1985 Home pneumograms in normal infants. J Pediatr 106: 551–555
Stein IM, White AQ, Kennedy JL Jr, Merisalo RL, Chernoff H, Gould JB 1979 Apnea recordings of health infants at 40, 44, and 52 weeks postconception. Pediatrics 724–730
Kelly DH, Stellwagen LM, Kaitz E, Shannon DC 1985 Apnea and periodic breathing in normal full-term infants during the first twelve months. Pediatr Pulmonol 1: 215–219
Kelly DH, Riordan L, Smith MJ 1992 Apnea and periodic breathing in healthy full-term infants, 12:18 months of age. Pediatr Pulmonol 13: 169–171
Richards JM, Alexander JR, Shinebourne EA, de Swiet M, Wilson AJ, Southall DP 1984 Sequential 22-hour profiles of breathing patterns and heart rate in 110 full-term infants during their first 6 months of life. Pediatrics 74: 763–777
Poets CF, Stebbens VA, Alexander JR, Southall DP 1991 Breathing patterns and heart rates at ages 6 weeks and 2 years. Am J Dis Child 145: 1393–1396
Poets CF, Stebbens VA, Samuels MP, and Southall DP 1993 Oxygen saturation and breathing patterns in children. Pediatrics 92: 686–690
Silvestri JM, Weese-Mayer DE, Kenny AS, Hauptman SA 1994 Prolonged cardiorespiratory monitoring of children more than twelve months of age: characterization of events and approach to discontinuation. J Pediatr 125: 51–56
Weese-Mayer DE, Morrow AS, Conway LP, Brouillette RT, Silvestri JM 1990 Assessing clinical significance of apnea exceeding fifteen seconds with event recording. J Pediatr 117: 568–574
Hodgman JE, Hoppenbrouwers T, Cabal LA 1993 Episodes of bradycardia during early infancy in the term-born and preterm infant. Am J Dis Child 147: 960–964
Meny RG, Carroll JL, Carbone MT, Kelly DH 1994 Cardiorespiratory recordings from infants dying suddenly and unexpectedly at home. Pediatrics 93: 44–49
Stebbens VA, Poets CF, Alexander JR, Arrowsmith WA . Southall DP 1991 Oxygen saturation and breathing patterns in infancy. I. Full term infants in the second month of life. Arch Dis Child 66: 569–573
West P, Kryger CF George CF 1987 Dynamic in vivo response characteristics of three oximeters: Hewlett-Packard 47201A, Biox III, and Nellcor N-100. Sleep 10: 263–271
ECRI Reports: Health Devices 1989 Pulse oximeters. 18: 185–230( special issue)
Marcus CL, Keens TH, Davidson Ward SL 1992 Comparison of nap and overnight polysomnography in children. Pediatr Pulmonol 13: 16–21
Acknowledgements
The authors thank Dr. Terry Baird for enrolling two infants from Cleveland Metropolitan Hospital; Drs. Bassel Salman and Jim Wallace, and Steve Martindale for assistance in scoring; the Infant Monitor Program staff for assistance in scoring and the overall conduct of the study; and Mary Kesling and Christine Jachimiak for their assistance in preparation of this manuscript.
Author information
Authors and Affiliations
Additional information
Presented in part at the Society for Pediatric Research Annual Meeting, Seattle, WA, May 1994.
Rights and permissions
About this article
Cite this article
Hunt, C., Hufford, D., Bourguignon, C. et al. Home Documented Monitoring of Cardiorespiratory Pattern and Oxygen Saturation in Healthy Infants. Pediatr Res 39, 216–222 (1996). https://doi.org/10.1203/00006450-199602000-00005
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199602000-00005
This article is cited by
-
Inter-hospital cardiorespiratory telemonitoring of newborns and infants: a wellworking example of a hub and spoke network
Italian Journal of Pediatrics (2023)
-
Apparent Life-Threatening Events (ALTE): Italian guidelines
Italian Journal of Pediatrics (2017)
-
Twelve-Month Prospective Study of Oxygen Saturation Measurements among Term and Preterm Infants
Journal of Perinatology (2005)
-
Short-term event recording as a measure to rule out false alarms and to shorten the duration of home monitoring in infants
Wiener Klinische Wochenschrift (2003)
-
Effect of Sleep Position on Apnea and Bradycardia in High-Risk Infants
Journal of Perinatology (2001)