Abstract
Our objective was the study of the renal phosphate threshold(TP/GFR) in very low birth weight infants with increasing post-menstrual (pm) age (gestational age plus postnatal age). The case notes of 62 very low birth weight infants were reviewed. Plasma and urine phosphate concentrations (PP, UP) determined on the same day together with the corresponding creatinine concentrations (PCrea, UCrea) built up a data set. Data sets obtained from 29 to 36 wk of pm age were included in the study. UP ≥ 1 mmol/L was defined as phosphaturia. TP/GFR= PP - (UP × PCrea/UCrea). In infants without phosphaturia, maximum PP is a lower limit of TP/GFR and was used as a censored TP/GFR value. We found that in phosphaturic infants, maximum PP (median and range) decreased from 2.8 (1.2-4.6) to 2.0 (1.4-2.7) mmol/L from 29-30 to 35-36 wk of pm age (p < 0.001), and censored TP/GFR (median and 95% confidence interval) decreased from 2.13 (1.95-2.33) to 1.57 (1.31-1.77) mmol/L (p < 0.001). We speculate that the renal phosphate threshold declines with increasing postmenstrual age because tubular reabsorption capacity increases more slowly than GFR.
Similar content being viewed by others
Main
In VLBW infants sufficiently substituted with phosphorus (UP ≥ 1 mmol/L) for preventing postnatal bone demineralization(1), we observed decreasing PP with increasing pm age. This decrease in PP did not result from a decreasing phosphate supplementation, because UP did not decrease. Therefore we concluded that the renal phosphate threshold decreases with increasing pm age. The following investigation was carried out to study this hypothesis.
METHODS
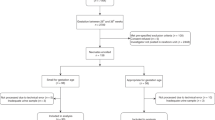
The case notes of 62 VLBW infants admitted to our intensive care unit from October 1984 to December 1987 were reviewed retrospectively. Daily vitamin D(cholecalciferol) intake was 1000 U (0.025 mg). All urinary measurements of phosphate and creatinine (morning spot urinary specimens) were recorded in cases where plasma concentrations of the same morning were available. PCa and UCa were recorded as well. Data sets of infants younger than 3 d of age were omitted because of possible transitional changes during this early time after birth. For each data set the pm age (gestational age plus postnatal age) of the individual child was calculated. Data sets obtained from 29 to 36 wk of pm age (study period) were included in the study.
Measured data. Phosphate, creatinine, and calcium were measured in plasma and urine by standard methods during the daily routine(2–4). The sensitivity of urine phosphate measurement was 0.4 mmol/L. Phosphaturia was defined as UP ≥ 1.0 mmol/L. The sensitivity of urine calcium measurement was 1.2 mmol/L.
Calculated data. For calculation of the renal phosphate threshold TP/GFR, the following formula was used.

Assuming that creatinine clearance equals GFR, the formula can be transformed as follows. Equation

The excreted fraction of the filtered phosphate load is equal to the ratio of phosphate clearance to creatinine clearance, indicated as CP/CCrea. Equation

The study period was divided into four 2-wk periods. The number of data sets per infant varied from 1 to 19. Every infant contributed, if available, only one value to every calculation in every 2-wk period. These values were selected as follows. 1) In phosphaturic infants (UP ≥ 1 mmol/L): (a) the maximum PP and its corresponding UP, PCa, UCa and (b) the maximum TP/GFR and its corresponding CP/CCrea (PCrea and UCrea available) or the minimum PP with phosphaturia (PCrea or UCrea not available); and 2) in nonphosphaturic infants (UP < 1 mmol/L) the maximum PP.
The maximum PP without phosphaturia is a lower limit of TP/GFR in infants insufficiently substituted with phosphate. The minimum PP with phosphaturia (UP ≥ 1 mmol/L) is an upper limit of TP/GFR in phosphaturic infants.
Statistics. Data are shown as median and range or as median and 95% confidence interval. Exploratory statistical tests were calculated without correction for multiple testing. The level of significance was set top = 0.01. The following hypotheses were tested by analysis of variance: 1) H10: there is no difference between the PP concentrations of the four groups and 2) H20: there is no difference between the UP concentrations of the four groups.
The hypothesis 'H30: there is no difference between the TP/GFR concentrations of the four groups was tested by the Log-Rank test. At first this test was done with all available TP/GFR values. In a second step, median censored TP/GFR was calculated. The method of calculating censored median values and their 95% confidence interval was taken from life table analysis (Kaplan Meier)(5, 6). In life table analysis it happens sometimes that a patient, who survived a certain time, moves away and his outcome is not known. This time can be used as censored survival time for estimation of the survival probability of the whole population over a period of time. In the present study the maximum PP of nonphosphaturic infants must be below the renal phosphate threshold and therefore is a lower limit of TP/GFR. These lower limits of TP/GFR were used as censored TP/GFR values. Including this information it was possible to calculate a censored median TP/GFR. Finally, in phosphaturic infants in whom TP/GFR could not be calculated because PCrea or UCrea were not available, the minimum PP with phosphaturia (UP ≥ 1 mmol/L) was used instead of TP/GFR because it was an upper limit of TP/GFR. It was now possible to calculate an upper limit of the censored median TP/GFR of the whole group.
RESULTS
Gestational age of the study population ranged from 25 to 32 wk with a median of 29. Median postnatal age was 21 (3-82) d (Table 1), and 395 data sets were included in the study. The number of data sets per patient ranged from 1 to 19 with a median of 6. Significant phosphaturia was present in 265 of 395 data sets. TP/GFR could be calculated in 201 data sets.
In phosphaturic infants (Table 2) the median PP decreased (p < 0.001) with increasing pm age and UP did not decrease (p > 0.7). Neither PCa nor the proportion of infants with UCa ≥ 1.2 mmol/L and their median UCa changed within the study period. Median CP/CCrea values varied between 0.17 and 0.25 in the four pm age groups. The median maximum PP of infants without phosphaturia (UP < 1 mmol/L) varied between 1.9 and 2.1 mmol/L, and the minimum PP in phosphaturic infants (UP ≥ 1 mmol/L) in whom TP/GFR could not be calculated varied between 2.7(1.8-3.1) and 2.0 (1.7-2.4) mmol/L (Table 3). TP/GFR, censored TP/GFR, and the censored upper limit of TP/GFR decreased with increasing pm age (p < 0.001)(Table 4).
DISCUSSION
This is the first study concerned with the development of the renal phosphate threshold in preterm infants between 29 and 32 wk of pm age. In infants sufficiently substituted with phosphorus (UP ≥ 1 mmol/L), the PP decreased with increasing pm age, whereas UP did not decrease. We concluded that the renal phosphate threshold decreases with increasing pm age.
The kidney plays a key role in regulating PP(7, 8). Plasma inorganic phosphate concentration is largely determined by the renal tubular reabsorption capacity, which is best described by TmP/GFR, the maximum rate of tubular phosphate reabsorption divided by the GFR(9). TmP/GFR is known as the theoretical renal phosphate threshold. In adults, TmP/GFR equals TP/GFR, the actual tubular phosphate reabsorption divided by GFR, as long as the excreted fraction of the filtered phosphate load(CP/CCrea) is equal or above 0.2(7). If CP/CCrea is lower than 0.2, derivation of TmP/GFR requires a mathematical correction of TP/GFR. In children, there is a close correlation and no significant difference between TP/GFR and its maximum TmP/GFR(10, 11). In infants, 0.5-12 mo of age, TmP/GFR and TP/GFR were equal with CP/Cinulin values above 0.1, and there was an excellent agreement between TmP/Cinulin and TP/GFR = PP -(UP × PCrea/UCrea)(11). Regarding preterm infants there are no data available. In the present study, median CP/CCrea varied between 0.17 and 0.25. Therefore, the reported TP/GFR values are thought to be a good approximation to TmP/GFR. The median TP/GFR at 33-36 wk of pm age is in agreement with the data of Brodehl et al.(12) who calculated TP/GFR using classical clearance techniques in newborn infants 0-3 mo of age. Slightly higher mean TP/GFR values (2.0 mmol/L) have been reported in preterm infants of about 36-37 wk of pm age(13).
It was possible to calculate Tp/GFR in only 19-35 of the infants'(Table 2) each 2-wk period. To use all available information, the time course of the median censored upper limit of TP/GFR of the whole group was calculated. As shown inTable 4 it was now possible to include the data for 31-52 of the 62 infants studied in each 2-wk period. This upper limit of TP/GFR also decreased with increasing pm age, supporting our hypothesis.
The decrease in TP/GFR with increasing pm age requires an explanation. In the first place, renal function might be impaired by exogenous factors like repeated episodes of ischemia and hypoxemia or nephrotoxic drugs. For example, all but three of our infants received antibiotic therapy with aminoglycosides, which might have affected renal tubular function in spite of regular drug level monitoring. The effect of aminoglycosides on the renal phosphate threshold in preterm infants has not yet been investigated. Second, it is well known that PTH does have a phosphaturic effect by decreasing renal phosphate threshold. But PTH levels were not measured in this study. However, the median PCa (2.4 mmol/L), the number of infants with an UCa≥ 1.2 mmol/L and the vitamin D supplementation (1000 IU/d) did not change within the study period. Therefore an increasing secondary hyperparathyroidism is unlikely the cause of this postnatal change in the phosphate threshold. Finally there is an imbalance in maturation of glomerular and tubular function in the preterm kidney. In VLBW infants, GFR is related to pm age and increases exponentially from 26 to 33 wk of pm age(14). By usingβ2-microglobulin as a marker for tubulus maturation, glomerular functional development precedes tubular functional development until the 34th pm wk(15). These results concur with our data because an exponentially increasing GFR in combination with a slower increasing tubular phosphate reabsorption capacity gives rise to a decreasing renal phosphate threshold.
Abbreviations
- VLBW:
-
very low birth weight
- pm age:
-
postmenstrual age (gestational age plus postnatal age)
- TP/GFR:
-
actual tubular phosphate reabsorption divided by GFR
- TmP/GFR:
-
maximum rate of tubular phosphate reabsorption divided by GFR = renal phosphate threshold
- Cinulin:
-
inulin clearance
- CP/CCrea:
-
excreted fraction of the filtered phosphate load = ratio of phosphate clearance to creatinine clearance
- PP:
-
plasma phosphate concentration
- PCrea:
-
plasma creatinine concentration
- UP:
-
urine phosphate concentration
- UCrea:
-
urine creatinine concentration
- UVol:
-
urine volume
- PCa:
-
plasma calcium concentration
- UCa:
-
urine calcium concentration
References
Pohlandt F 1994 Prevention of postnatal bone demineralization in very low-birth-weight infants by individually monitored supplementation with calcium and phosphorus. Pediatr Res 35: 125–129
Greiling H, Gressner AM 1989 Lehrbuch der Klinischen Chemic und Pathobiochemie, Schattauer, Stuttgart, pp 578–580
Henry RJ 1974 Clinical Chemistry, Harper & Row, New York, pp 639–756
Ginder EM, King JD 1972 Rapid colorimetric determination of calcium in biological fluids. Am J Clin Pathol 58: 376–382
Armitage P, Berry G 1987 Statistical Methods in Medical Research, 2nd EdBlackwell Scientific Publications, Oxford, pp 31–51
Lawless JF 1982 Statistical Models and Methods for Lifetime Data. Wiley, New York, pp 31–43
Bijvoet OLM 1977 Kidney function in calcium and phosphate metabolism. In: Avioli LV, Krane SM (eds) Metabolic Bone Disease. Academic Press, New York, pp 50–83
Senterre J, Salle B 1988 Renal aspects of calcium and phosphorus metabolism in preterm infants. Biol Neonate 53: 220–229
Bijvoet OLM 1969 Relation of plasma phosphate concentration to renal tubular reabsorption of phosphate. Clin Sci 37: 23–36
Stark H, Eisenstein B, Tieder M, Rachmel A, Alpert G 1986 Direct measurement of TP/GFR: a simple reliable parameter of renal phosphate handling. Nephron 44: 125–128
Brodehl J, Krause A, Hoyer PF 1988 Assessment of maximum tubular phosphate reabsorption: comparison of direct measurement with the nomogram of Bijvoet. Pediatr Nephrol 2: 183–189
Brodehl J, Gellissen K, Weber H-P 1982 Postnatal development of tubular phosphate reabsorption. Clin Nephrol 17: 163–171
Langhendries JP, Francois A, Chedid F, Battisti O, Bertrand JM, Senterre J 1992 Phosphorus intake in preterm babies and variation of tubular reabsorption for phosphate per litre glomerular filtrate. Biol Neonate 61: 345–350
Wilkins BH 1992 Renal function in sick very low birthweight infants: 1. Glomerular filtration rate. Arch Dis Child 67: 1140–1145
Aperia A, Broberger O, Broberger U, Herin P, Zetterström R 1983 Glomerular tubular balance in preterm and fullterm infants. Acta Paediatr Scand Suppl 305: 70–76
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Mihatsch, W., Muche, R. & Pohlandt, F. The Renal Phosphate Threshold Decreases with Increasing Postmenstrual Age in Very Low Birth Weight Infants. Pediatr Res 40, 300–303 (1996). https://doi.org/10.1203/00006450-199608000-00018
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199608000-00018
This article is cited by
-
Urinary excretion of calcium and phosphate in preterm infants
Pediatric Nephrology (2004)