Abstract
During normal pregnancy, the levels of placental GH in the maternal circulation increase significantly until 35 wk of gestation. We have previously shown that these levels are significantly reduced in cases of intrauterine growth retardation (IUGR). To better understand the basis of this observation, we have studied the expression of placental GH in placentas from normal births (n = 6) and births with IUGR (n = 5).In situ hybridization histochemistry was used to determine the mean number of cells per area expressing this message, as well as the mean level of specific mRNA per cell. We have found that the mean mRNA signal level per cell of placental GH did not differ between normal or IUGR placentas. However, the mean number of cells/area expressing this mRNA was significantly greater in normal placentas compared with IUGR placentas (normal 12.8 ± 0.9 cells/unit area, IUGR 4.9 ± 2.4 cells/unit area, analysis of variance:p < 0.004). These data suggest that the decreased levels of placental GH in the maternal circulation in IUGR are not due only to the reduced size of the placenta, but also to changes in the placental tissue which result in a reduced number of cells per area that are capable of producing this peptide.
Similar content being viewed by others
Main
IUGR is of major clinical concern because there is a close relationship between the degree of growth retardation and perinatal morbidity and mortality. Unfortunately, the mechanisms underlying abnormal fetal growth are not well understood. It has recently been shown that levels of placental GH in the maternal circulation are significantly reduced in cases of IUGR(1) and that maternal IGF-1 levels positively correlate with placental GH levels(1, 2). Hence, it is conceivable that placental GH plays a role in the process of IUGR.
Placental GH is encoded by the GH-V gene, which belongs to a gene cluster located on chromosome 17q22-24. This gene cluster consists of 5 loci, beginning 5′ with hGH-N (pituitary GH), and continuing 3′ with hCS-L, hCS-A, hGH-V (placental GH), and hCS-B. These genes have all been cloned and sequenced and have been shown to contain a high degree of sequence and structural homology(3–5).
Placental GH is produced and secreted by the syncytiotrophoblast(6) and during pregnancy progressively replaces pituitary GH in maternal serum(7–10). On the other hand, it is not detectable in the fetus, nor in the cord blood of the newborn. A physiologic role for placental GH is suggested by the fact that it binds to human placental tissues(11). Interestingly, placental GH secretion is inhibited by glucose(12), strongly suggesting a metabolic role of this hormone during gestation. Through its somatogenic activity, placental GH might help to maintain high levels of nutrients in the mother to be transferred to the fetoplacental unit. Hence, an indirect role in fetal growth is implied. In support of this concept, we have previously shown that placental GH is significantly lower in maternal serum in cases of IUGR(1).
To determine whether the source of the decreased in maternal levels of placental GH during IUGR are due to the reduced ability of the placental tissue to produce this peptide, semiquantitative in situ hybridization histochemistry was performed. The number of cells per unit area of tissue producing this peptide, as well as the mRNA levels per cell were determined.
METHODS
Tissue collection and preparation. Placentas from six healthy women with uncomplicated singleton pregnancies, with term delivery (39-41 wk of amenorrhea) and appropriate weight for gestational age infants were used as controls. IUGR was defined as birth weight below the third percentile on Leroy's chart for term (34-41 wk of amenorrhea)(13). The mother's clinical and obstetrical histories and the neonate's clinical characteristics were recorded by obstetricians and pediatricians, respectively. The placentas were macroscopically examined according to Benirschke and Kaufmann(14), and three samples for histologic examination were included in paraffin and stained with hematoxylin-eosin. The placental weights were correlated to the birth weights. Maternal hypertension was noted in two cases of IUGR. Placental vascular lesions were observed in all cases of IUGR.
For in situ hybridization, samples were obtained at the time of birth and taken from areas of the placenta were there was no obvious tissue damage. They were rinsed, immediately frozen on dry ice and stored at-80°C. Cryostat sections were cut at 20 μm and thaw-mounted onto poly-L-lysine (50 μg/mL)-coated slides. Tissue slices were stored at-80°C until hybridization histochemistry was performed.
Labeling of oligonucleotide probes. The probe (Eurogentech, Liège, Belgium) used in these assays was an oligonucleotide probe 30 bases in length and specific for GH-V. It was end-labeled with 35S-dATP by using terminal transferase (TdT; Boehringer Mannheim) and applied to the tissue at a saturating concentration.
In situ hybridization. Tissue sections were fixed in 4% paraformaldehyde, treated with 0.25% acetic anhydride in 0.1 M triethanolamine(pH = 8.0), rinsed in 2 × SSC (300 mM NaCl and 30 mM sodium citrate), dehydrated, and delipidated. The probe was diluted in hybridization buffer and approximately 8 × 105 cpm/slide applied. The slides were then covered with Parafilm, sealed with rubber cement, and incubated overnight in moist chambers at 37°C. The following day, the parafilm coverslips were removed, and the slides washed in 1 × SSC at room temperature for 15 min(twice), 1 × SSC at 48°C for 30 min (twice), and 1 × SSC at room temperature for 30 min (twice). They were then dehydrated and dipped in photographic emulsion (Kodak NBT-2 diluted 1:1 with 600 mM ammonium acetate and heated to 45°C). The slides were then air-dried at room temperature for 15 min, dried in a damp chamber for 1 h, placed in lighttight boxes with dessicant, and exposed at 4°C for 21 d. They were then developed and counterstained with cresyl violet.
Image analysis. Slides were assigned a random three-letter code and analyzed so that the operator was unaware of the experimental group. Twelve tissue sections per placenta were analyzed. To determine the number of GH-V-positive cells, random fields were analyzed (10 fields/tissue section; hence, 120 fields/placenta), and the cells were identified under bright-field illumination (50 × magnification). The number of cresyl violet-stained nuclei associated with a cluster of silver grains was determined in each field. The number of silver grains associated with each nuclei was determined by using an automated image analysis system. This system has previously been described in detail(15). Briefly, the system consisted of a PixelGrabber video acquisition board (Perceptics Corp., Knoxville, TN) attached to a Macintosh IIci computer. Video images were obtained by a Sony camera attached to a Zeiss Axioplan Photomicroscope. An average of 20 positive cells (or nuclei)/section was analyzed (240 readings/placenta). Hence, the“number of positive cells” reflects the number of nuclei in the syncytium associated with a cluster of silver grains. The image analysis readings are reported as mean “grains/cell” and reflect the mean level of specific mRNA signal associated with individual nuclei.
Control experiments. Control experiments for the GH-V probe have previously been reported(6). In addition, a 30-base oligonucleotide probe, whose sequence is not complementary to any known mRNA, was labeled to approximately the same specific activity as the GH-V probe and ran in parallel with all experiments. No specific labeling was seen with this probe. Experiments were also run to determine the saturating concentration of probe. This probe saturated at a concentration of approximately 1.5 fmol/μL(see Fig. 1). All experiments were run at a concentration of 1.75 fmol/μL.
Statistical analysis. The mean level of grains/cell was determined from the analysis of 240 positive cells/placenta. Approximately 120 fields of view were analyzed to determined the mean number of positive cells/area. A t test was used to determine whether there were significant differences between the two groups. The significance level was chosen as p < 0.05.
RESULTS
Figure 1 shows the saturation curve of the oligonucliotide probe used in these experiments. Specific binding saturated at a concentration of approximately 1.5 fmol/μL, whereas, as expected, the nonspecific binding did not saturate with increasing concentrations of probe.
Figure 2 is a darkfield photomicrograph where a positive signal for GH-V mRNA can be seen. The white clusters of silver grains are each specifically associated with a cresyl violet-stained nucleus.
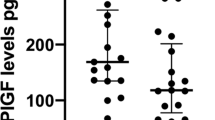
As can be seen in Figure 3A, there was no difference between normal and IUGR placentas in the mean levels of GH-V mRNA/cell. However, the mean number of GH-V-positive cells/area was significantly greater in normal placentas when compared with IUGR placentas (Fig. 3B).
(A) Placental GH mRNA signal in normal and IUGR placentas. The mean level of GH-V mRNA per individual cell (as represented by silver grains/cell) in placentas from normal or IUGR births. There was no significant difference between these two groups in the mean mRNA levels per cell. (B) The mean number of GH-V mRNA-expressing cells per area in placentas from normal or IUGR births. The number of nuclei in the syncytium expressing the mRNA for placental GH was significantly higher in normal placentas compared with that from IUGR births (p < 0.004).
DISCUSSION
It has been established previously that the concentration of placental GH in the maternal circulation is reduced in IUGR(1). Here we present data suggesting that this observation may not be due only to the decreased size of the IUGR placenta, but also to the reduced ability of this tissue to produce placental GH. We show that the number of cells per unit area expressing this peptide is decreased in IUGR placentas compared with normal. Interestingly, the synthetic capacity of the individual nuclei, as expressed in relative levels of placental GH mRNA, does not appear to be modified.
As previously reported, placental GH was found to be expressed within the syncytiotrophoblast(6, 16). Also in accordance with previous studies(6), placental GH-expressing cells tend to be relatively dispersed, but heavily labeled. The fact that in IUGR placentas the relative levels of GH-V mRNA/cell did not differ from that seen in normal placentas suggests that the synthetic capacity for this peptide, at least at the transcriptional level, of individual nuclei is not altered. This may indicate that these cells are functioning normally and are receiving the necessary signals to produce this peptide. However, the reduction in the number of cells expressing this peptide suggests a possible fault in the development or differentiation of the placental tissue.
Although the precise role of placental GH during pregnancy remains to be elucidated, it is not thought to directly influence fetal growth, because it is not detected in the fetal circulation(17). However, both endocrine and paracrine/autocrine functions have been suggested, including modulation of maternal metabolism and regulation of placental development. Maternal IGF-I levels show a positive correlation with placental GH concentrations(1, 2). Although maternal IGF-I is synthesized mainly by the liver(18), some placental IGF-I is secreted into the maternal circulation(19). Placental GH, whose secretion is inhibited by glucose(12), might modulate maternal IGF-I levels by acting on its synthesis in the maternal liver or in the placenta. Indeed, the syncytiotrophoblast is a rich source of IGF-I(20) and also expresses GH receptors(11). Due to the presence of an autocrine regulation of placental GH within the syncytiotrophoblasts, it has also been suggested that placental GH plays a role in placental development. Because a relationship between placental size and fetal growth has been clearly established(21), it is therefore possible that placental GH has an indirect effect on fetal growth. However, whether a reduction in placental GH is the cause of some IUGR or only the result of other underlying causes remains to be elucidated.
In this study we show that the low levels of placental GH in the maternal circulation as a result of IUGR may not be due only to the reduced size of the placenta, but also to the decreased capacity of the existing placental tissue to produce this peptide. This decline in synthetic capacity may be due to a dysfunction in the development of the placenta as there is a decreased number of placental GH producing cells. In contrast, the individual capacity of these cells to produce GH does not appear to be affected in IUGR.
Abbreviations
- IUGR:
-
intrauterine growth retardation
- GH-V:
-
growth hormone variant
References
Mirlesse V, Frankenne F, Alsat E, Poncelet M, Evain-Brion D 1993 Placental growth hormone levels in normal and pregnancies with intrauterine growth retardation. Pediatr Res 34: 439–442.
Caufriez A, Frankenne F, Englert Y, Golstein J, Cantraine F, Hennen G, Copinschi G 1990 Placental growth hormone as a potential regulator of maternal IGF-1 during pregnancy. Am J Physiol 258:E1014–E1019.
Chen EY, Liao YC, Smith DH, Barrere-Saldaña HA, Gelinas RE, Seeburg PH 1989 The growth hormone locus: nucleotide sequence, biology and evolution. Genomics 4: 479–497.
Hirt H, Kimelman J, Binbaum MJ, Chen EY, Seeburg PH, Eberhardt NL, Barta A 1987 The human growth hormone gene locus: structure, evolution and allelic variations. DNA 6: 59–70.
Seeburg PH 1982 The human growth hormone gene family:nucleotide sequences show recent divergence and predict a new polypeptide hormone. DNA 1: 239–249.
Scippo ML, Frankenne F, Hooghe-Peters EL, Igout A, Velkeniers B, Hennen G 1993 Syncytiotrophoblastic localization of the human growth hormone variant mRNA in the placenta. Mol Cell Endocrinol 92:R7–R13.
Hennen G, Frankenne F, Closset J, Gómez F, Pirens G, El Khayat N 1985 A chorionic GH-like antigen: increasing levels during second half of pregnancy with pituitary GH suppression as revealed by monoclonal antibody radioimmunoassays. Int J Fertil 30: 27–33.
Frankenne F, Closset J, Gomez F, Scippo ML, Smal J, Hennen G 1988 The physiology of growth hormones (GHs) in pregnant women and partial characterization of the placental GH variant. J Clin Endocrinol Metab 66: 1171–1180.
Frankenne F, Scippo ML, Van Beeumen J, Igout A, Hennen G 1990 Identification of placental growth hormone as the growth hormone-V gene expression product. J Clin Endocrinol Metab 71: 15–18.
Igout A, Scippo ML, Frankenne F, Hennen G 1988 Cloning and nucleotide sequence of placental hGH-V cDNA. Arch Int Physiol Biochem 96: 63–67.
Frankenne F, Alsat E, Scippo ML, Igout A, Hennen G, Evain-Brion D 1992 Evidences for the expression of growth hormone receptors in human placenta Biochem Biophys Res Commun 182: 481–483
Patel N, Alsat E, Igout A, Baron F, Hennen G, Porquet D, Evain-Brion D 1995 Glucose inhibits human placental GH secretion, in vitro. J Clin Endocrinol Metab 80: 1743–1746.
Leroy B, Lefort F 1971 A propos du poids et de la taille des nouveaux-nés a la naissance. Rev Fr Gynecol Obstet 66: 391–396.
Benirschke K, Kaufmann P 1990 Pathology of the Human Placenta, 2nd Ed. Springer-Verlag, New York, 870
Chowen JA, Steiner RA, Clifton DK 1991 Semiquantitative analysis of cellular somatostatin mRNA levels by in situ hybridization histochemistry. In: Conn PM (ed) Methods in Neurosciences. Academic Press, San Diego, 137–158.
Jara CS, Salud AT, Bryant-Greenwood GD, Pirens G, Hennen G, Frankenne F 1989 Immunocytochemical localization of the human growth hormone variant in the human placenta. J Clin Endocrinol Metab 69: 1069–1072.
DeZeghers F, Vanderschueren-Lodeweyckx M, DeZeghers F, Vanderschueren-Lodeweyckx M, Spitz B, Faijerson Y, Blomberg F, Beckers A, Hennen G, Frankenne F 1990 Perinatal growth hormone (GH) physiology: effect of GH-releasing factor on maternal and fetal secretion of pituitary and placental GH. J Clin Endocrinol Metab 77: 520–522.
Humbel RE 1990 Insulin-like growth factors I and II. Eur J Biochem 190: 445–462.
Challier JC, Frankenne F, Bintein T, Poncelet M, Hennen G 1991 Release of placental growth hormone by perfused human placenta. Placenta 12: 377–378. (abstr)
Wang C-Y, Daimon M, Shen SJ, Engelmann GL, Ilan J 1988 Insulin-like growth factor-I messenger ribonucleic acid in the developing human placenta and in term placenta of diabetics. Mol Endocrinol 2: 217–229.
Sands J, Dobbing J 1985 Continuing growth and development of the third-trimester human placenta. Placenta 6: 13–22.
Acknowledgements
The authors thank Dr. Francis Frankenne for the kind gift of the GH-V oligonucleotide.
Author information
Authors and Affiliations
Additional information
Supported by grants from the EEC (JUTL 91.0004), Fundación de Endocrinología y Nutrición, and la Fondation pour la Recherche Médicale.
Rights and permissions
About this article
Cite this article
Chowen, J., Evain-Brion, D., Pozo, J. et al. Decreased Expression of Placental Growth Hormone in Intrauterine Growth Retardation. Pediatr Res 39, 736–739 (1996). https://doi.org/10.1203/00006450-199604000-00028
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199604000-00028
This article is cited by
-
Insulin-like growth factor axis in pregnancies affected by fetal growth disorders
Clinical Epigenetics (2016)