Abstract
The study was peformed to assess the utility of the Morris water maze (MWM) and acoustic startle reflex (ASR) for evaluating neurologic outcome in a rat model of asphyxial cardiac arrest. Rats were anesthetized, intubated, and chemically paralyzed. Control animals were decannulated and, after awakening, were extubated and returned to their housing. Experimental animals were asphyxiated by disconnecting the ventilator. Approximately 3.5 min after the disconnection, there was no measurable pulse. After 7 min of asphyxia, they were then resuscitated with resumed ventilation, chest compressions, epinephrine, and sodium bicarbonate. All animals were assigned to either MWM or ASR testing. The MWM is a 6-ft diameter tank filled with opaque water. In a fixed location of the tank, a 4-inch diameter escape platform is submerged just below the surface. MWM animals were tested on post-injury d 16-21 by recording the path and time taken to escape from three randomly assigned locations per d. ASR animals had s.c. leads placed over the right triceps and tibialis anterior muscles. The latency and rectified amplitude of the ASR was measured by recording the electromyographic impulse generated when the animal was startled by an acoustic stimulus. Animals were tested on post-injury d 6 and 7. After the last test session for each group, the animals' brains were removed for histopathologic examination. Asphyxiated MWM animals took longer to find the platform, and their paths were less direct than control animals(analysis of variance p < 0.05). The ASR of asphyxiated ASR animals had greater amplitude and shorter latency compared with controls(analysis of variance p < 0.05). Histologic examination revealed no abnormalities in control animals, but 80% of asphyxiated brains showed hippocampal neuronal injury and/or reactive gliosis in the CA1 segment. Abnormalities were more commonly detected in animals killed 7 d post-injury(ASR protocol) compared with animals killed 21 d post-injury (MWM protocol). We conclude that the MWM and ASR are useful for detecting neuronal injury in asphyxiated rats.
Similar content being viewed by others
Main
Most experimental research investigating hypoxic/ischemic cerebral injury has focused on models of partial ischemia (mimicking cerebral vascular disease), global ischemia (mimicking cerebral ischemia secondary to cardiac arrest), or pure hypoxia (an uncommon clinical event). Comparatively little work has been performed using asphyxial models of cerebral insult(1–6). Asphyxia, as a cause of cardiac arrest and CNS injury, deserves further study because of its distinct pathophysiology. Compared with other insults, asphyxia exposes the brain to lower tissue pH and higher tissue CO2 and results in greater edema, parenchymal hemorrhage, and disruption of the blood-brain barrier(6–9). These pathophysiologic attributes may result in an altered response to cerebroprotective interventions (compared with the response of other hypoxic/ischemic injuries)(6). Lastly, asphyxial cardiac arrest is of particular importance in the pediatric population, in which 75% of cardiac arrests are respiratory in origin(10–12).
This project was designed to develop a model for assessing neurologic outcome of rats resuscitated from asphyxial cardiac arrest. Neurologic outcome was assessed using the MWM, the ASR, and histopathology. The MWM was chosen as an outcome measure because of its ability to assess memory impairment (a common sequelae of human cardiac arrest) and its close relationship with the hippocampus (an area of the brain particularly sensitive to hypoxic/ischemic injury). The ASR was chosen as an outcome measure because it is a quantifiable and reproducible reflex arc which is relatively resistent to changes in emotional/motivational state. Outcomes of instrumented, asphyxiated animals were compared with instrumented, nonasphyxiated controls.
METHODS
This study was approved by an Institutional Animal Care and Use Committee. Sprague-Dawley rats weighing 450 g were used in this experiment. Each rat was adapted to the university vivarium for at least 1 wk before instrumentation.
Instrumentation
Anesthesia was initiated by placing the animal in a bell jar with 4% halothane in a 50:50 mixture of N2O/O2. Once a sufficient plane of anesthesia was achieved, the rat was transferred to a nose cone providing 3% halothane. When the animal became flaccid it was intubated with a 16-gauge angiocatheter, and the halothane was decreased to 1.5%. The angiocatheter was connected to a Harvard rodent ventilator with a piston volume of 10 mL/kg, peak end-expiratory pressure = 2 cm H2O, and a respiratory rate of 38 cycles/min. The animal was then placed on a warmed gel pack, and ECG leads and a rectal temperature probe were placed. Rectal temperature was maintained at 37.5 ± 0.5°C. The left femoral artery and vein were cannulated with PE50 tubing.
After cannulation, 0.5 mg of vecuronium was given through the femoral vein, and the halothane was decreased to 0.5%. Five minutes after paralysis a blood sample for determining arterial blood gas was drawn, and the ventilator frequency was adjusted to maintain the partial pressure of arterial CO2 at 30-45 mm Hg and the pHa 7.32-7.5. When the arterial blood gas fell within these parameters, the anesthetic gases were washed out with 1 min of ventilation with 100% O2 followed by 4 min of room air. Previous experience with this model demonstrated that the washout period diminished the hemodynamic effects of the anesthetics while still allowing the animal to be anesthetized to the point of unconsciousness(2). At the beginning of the washout period and 4 min later, 0.75-mg doses of vecuronium were administered. The vecuronium was given to prevent the brain stem-mediated agonal respirations (autoresuscitation) found in asphyxiated animals.
Asphyxia
After the washout period, 35 experimental animals were asphyxiated by disconnecting the respiratory tubing from the ventilator for a duration of 7 min. After 7 min, the ventilator was reconnected at a rate of 60 breaths/min with 100% O2, and the animals were resuscitated with 0.01 mg/kg epinephrine, 1 mEq/kg NaHCO3, and manual extrathoracic compressions at a rate of approximately 300 compressions/min. After the return of spontaneous circulation, a 2-mL bolus of normal saline was administered.
Control animals were not asphyxiated; they were decannulated and extubated after the washout period. They were returned to their housing with no further interventions except for routine care until the beginning of testing.
Post-injury
Asphyxiated animals were ventilated at 60 breaths/min for the first 10 min, 50 breaths/min for the subsequent 10 min, and 40 breaths/min for the next 10 min. Blood gases were obtained at 5 and 15 min post-asphyxia. At 15 min post-asphyxia, the femoral catheters were removed, and the wounds were closed with nylon sutures. The animals were extubated at 30 min post-injury or before if they began breathing spontaneously. Their eyes were coated with Lacri-lube(Allergen Pharmacetuicals, Irvine, CA), and they were given blow-by oxygen for approximately 1 h before being placed back in their cages. Ten milliters of normal saline (s.c.) and 1 mL Nutrical (IGI, Inc., Buena, NJ) (p.o.) were administered daily until the animals were observed to be eating and drinking spontaneously. They were also given 0.5 mL of trimethaprim-sulfazoxazole suspension daily for 3 d. All control and experimental animals were assigned to either the MWM or ASR group. Animals could not be assigned for testing with both measures because the duration of survival differed between the groups.
MWM
The MWM is a 6-ft diameter metal tank filled to a depth of 20 cm with water rendered opaque with nontoxic white tempura paint(13). An escape platform (a solid column 11 cm in diameter and 19 cm tall) was placed in the northern sector of the maze. Because the platform was submerged 1 cm below the opaque water, it was not visible to the rat. Throughout the experiment the location of the escape platform was kept constant. Four large, brightly colored, geometric shapes were placed around the inside of the tank to help orient the animals to their surroundings.
All rats were handled daily, beginning 4 d before the insult, to acclimate them to the investigators' touch. On post-injury d 13, the animals were acclimated to the MWM by allowing them to swim freely in the tank (without the escape platform) for 2 min. MWM trials were performed daily on post-injury d 16-21. A trial consisted of placement in the tank from one of three locations(east, west, or south). On each test day, all three locations were tested in a randomized sequence. The path taken to find the platform and the time elapsed were recorded for each trial. The path taken by the animals was hand-traced onto a scaled-down, paper replica of the maze. Times were recorded with a stopwatch. Trial tracings were later retraced with a map chronometer for determination of swimming speed. Once the platform was found, the animal was allowed to remain on the platform for 1 min to orient to the visual clues and spatial relationships of the maze. To prevent fatigue, animals were removed from the water and placed on the platform if the platform was not located within 3 min of swimming.
ASR
The ASR is a series of fore- and hindlimb stereotypical responses involving several muscle masses that is produced by an intense auditory stimulus(14, 15). A less intense auditory stimulus delivered just before the intense stimulus modifies the ASR by prolonging the latency and decreasing the amplitude of the reflex (prestimulus inhibition)(16–18). The latency and magnitude of the ASR and ASR modulated with prestimulus inhibition were measured in both asphyxiated and control animals using bipolar electrode leads placed s.c. at polar ends of the right triceps and right tibialis anterior muscles.
All rats were handled daily, beginning 4 d before the insult, to acclimate them to the investigators' touch and the acoustic startle chamber. The startle chamber was a 75 × 33 × 60-cm soundproof box containing a fan, two speakers, and a 17 × 7 × 6-cm containment cage. The fan delivered a continuous background noise of 70 dB (white noise). The speakers delivered the main tone and pretone stimuli. The main tone was a 115 dB, 5-ms tone in the medium frequency range, and the pretone was a 90 dB, 1-ms tone in the high frequency range. The containment cage was a plastic fenestrated cage that limited the motion of the animals, facilitated placement of the leads, and regulated the animals' posture. The animals were habituated with 10 min in the containment cage with white noise on the 1st d, 20 min of similar confinement on the 2nd d, and 30 min of white noise on the 3rd and 4th d with main tones generated every 30 s for the final 10 min.
The day after the 4-d habituation period, the animals were anesthetized, instrumented, and either exposed to asphyxia or prepared as controls. During anesthesia each animal had metal staples placed through the skin overlying the right triceps and right anterior tibialis muscles. These staples were later used to attach leads for ASR testing. The staples were fashioned from 23-gauge needles which were inserted s.c. and then bent 90° four times to form a 4× 7-mm rectangle. Two staples were placed at each location 8 mm parallel to each other. Another staple, used for grounding, was placed in the lumbosacral area approximately 2 cm cephalad to the tail.
ASR testing was performed on post-injury d 6 and 7. After placing the animals in the containment cage, insulated electrical wires (0.9-mm outer diameter) were attached to the staples via miniclips. These wires were connected to the data analyzer (model DR-484, Neuro Data Corp.) through a differential AC amplifier (×100, 20 Hz-20 kHz model 1700, A-M System). All data were transferred from the data analyzer to an IBM-compatible computer by the data acquisition program Neuro Lab (Neuro Data Instruments Corp., 1992).
Once the leads were connected, the animal was isolated inside the acoustic startle chamber. A series of main tones was delivered every 30 s for 10 min. One-half of the main tones were randomly paired with pretones delivered 60 ms before the main tone. The tone sequence was controlled by a digital stimulator(PG-4000 digital stimulator, Neuro Data Corp., New York). On each of the two testing days, 20 responses were generated (10 main tone and 10 pretone-main tone pairs). The latency (interval from main tone to start of startle), and the rectified integrated amplitude for each response was determined by the waveset analysis functions of the Neuro Lab.
Histopathology of the Brain
Fixation. Animals in the MWM group were killed and perfused after the final swimming test on post-injury d 21. Animals in the ASR group were killed and perfused after the final ASR testing session on post-injury d 7. Tissue perfusion was performed under halothane anesthesia by exposing the heart and placing an 18-gauge needle into the left ventricle. The pulmonary artery was severed, and normal saline was perfused into the left ventricle at a pressure of 100 mm Hg. When the effluent from the pulmonary artery was clear, the perfusant was changed to 10% buffered paraformaldehyde. Perfusion was continued with paraformaldehyde for 10 min beyond the first fasciculations. The heads were then removed and stored in paraformaldehyde until processed for histopathology.
Histologic examination. Brains were extracted from the cranial vaults and weighed after the olfactory bulbs were removed and the brain stem cut at the level of the sulcus medianus dorsalis. The entire brain was imbedded for histologic sections, and representative areas of the cerebral cortex, hippocampus, basal ganglia, thalamus, cerebellum, and three levels of brain stem were examined by light microscopy. The brain was cut coronally into four sections. The first cut was done at the level of the infundibulum, the second at the level of the cerebral peduncles, the third at the level of the exit of the fifth cranial nerve in the pons, and the fourth at the level of the inferior vermis. To maximize midbrain examination, the anterior side of the cerebral tissue blocks and the posterior side of the brain stem blocks were marked with India ink; the opposite side was used for histologic sections. The sections were stored in 70% alcohol until they were processed into paraffin blocks, cut, and stained.
Two brains from control rats were not examined because of technical mishaps. The brains of all other animals surviving until completion of the protocol were processed with H&E stain. Staining with GFAP immunoperoxidase, which specifically stains astrocytes and highlights lesions of foci associated with reactive gliosis, was performed on approximately one-third of control and two-thirds of asphyxiated brains. Because of cost constraints, GFAP staining could not be performed on all brains. The neuropathologist (G.d.C.-M.) examining the sections was blinded to the assignment of the animals.
Statistics
Analysis of variance with repeated measures was used to compare MWM performance and ASR characteristics within and between groups. p values < 0.05 were considered to be statistically significant.
RESULTS
Before the insult, there was no difference in weight, temperature, blood pressure, Hb, serum glucose, and blood gas values when control and experimental groups were compared (t test). A total of 35 animals were asphyxiated. Three animals were unable to be resuscitated and another 10 died after resuscitation (0.5, 3, 24, 24, 48, 48, 72, 120, 144, and 144 h post-asphyxia). Gross examination of the thoracic and abdominal cavities in these animals revealed diffuse hemorrhage into the lungs. The asphyxiated animals were severely obtunded for several hours after the event; their motor activity consisted of yawning and, rarely, lifting their heads. During the initial hours they developed marked flexion of the upper extremities and extension of the lower extremities. The upper limb spasticity resolved over the next several days. The lower limb spasticity resolved after the upper limb spasticity, in general, over 1-2 wk.
MWM. There were 11 asphyxiated animals assigned to the MWM group that survived the duration of the MWM protocol (21 d). Two of these animals had mild, persistent hindlimb spasticity and were excluded from MWM testing. There were nine asphyxiated and nine control animals tested in the MWM.
Asphyxiated animals took significantly longer to find the platform compared with control animals. The poor performance of asphyxiated animals was not due to differences in the mean swimming speed of the two groups of rats(asphyxiated rats 2.38 ± 0.82 cm/s, control rats 2.72 ± 0.82 cm/s). The performance times are shown in Table 1 andFigure 1. ANOVA with repeated measures demonstrated a significant difference between groups and over time for both the individual site times and the total daily times (Table 2). However, there was no interaction between the groups; in other words, the groups showed a parallel learning curve and did not act differently from each other with respect to the direction and magnitude of their change over time. Although there was no interaction between groups, the performance of control animals appeared to asymptote on d 4 and 5, whereas performance of the experimental animals did not. When experimental animals without histologic evidence of brain injury were compared with experimental animals with evidence of brain injury, there was no difference in performance (ANOVA, p = 0.68). However, when the experimental animals without histologic evidence of brain injury were compared with control animals, the difference in performance was preserved (ANOVA, p = 0.02). Sample tracings of maze performance are shown in Figure 2. The paths of control animals were more direct than the paths of asphyxiated animals.
ASR. There were 11 asphyxiated animals assigned to the ASR group that survived the duration of the ASR protocol (7 d). There were 10 animals assigned as ASR controls.
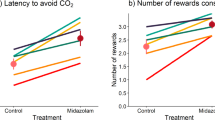
A typical ASR wave form is shown in Figure 3. In general, recordings from the lower extremity were of better quality than those from the upper extremity. The rectified integral of the ASR amplitude, with and without prestimulus inhibition, is shown in Figure 4. The latency of the ASR, with and without prestimulus inhibition, is shown inFigure 5. Because the results from d 6 and 7 did not differ (ANOVA), they were combined for statistical analyses. p values obtained from ANOVA with repeated measures are shown inTable 3. Asphyxiated animals had responses with greater amplitudes and shorter latencies compared with control animals. Both groups had prolonged latency and diminished rectified integral in response to the pretone (prestimulus inhibition). The ANOVA test for interaction, which examines the relative sensitivity to prestimulus inhibitionbetween groups, revealed a significant p value for lower extremity latencies; signifying that control animals were more susceptible to prestimulus inhibition of latency than asphyxiated animals. The p value for interaction in the lower extremity rectified integral values approached, but did not reach, significance (p = 0.065). The tests for interactions in the upper extremity were not significant; however, the sample size of upper extremity values was limited because the wave form quality from several animals was inadequate for analysis.
The rectified and integrated amplitude of the triceps(TR) and tibialis anterior (TA) responses with and without the pretone (Pre). Vertical bars represent the 95% confidence intervals. The asphyxiated animals had greater values compared with controls. Note the inhibition of the response after the pretone.
The duration of the interval from the start of the upper extremity response to the lower extremity response was longer in the controls (1.45 ms) than in asphyxiated animals (1.15 ms). However, the difference was not statistically significant.
Histopathology. All brains were examined with H&E. There were no abnormalities detected in the 17 control animals. The H&E stain revealed irreversible ischemic neuronal changes in 4 of the 9 MWM and 10 of the 11 ASR experimental animals. The majority of injury was limited to the hippocampus, with the CA1 region of the hippocampus being most vulnerable to injury. Four brains had lesions in the seventh cranial nerve nucleus and four had minimal injury to the cerebellar Purkinje cells.
Thirteen experimental and five control animals were examined with GFAP stain. No abnormalities were detected in control animal brains. Three of seven MWM and two of six ASR experimental animals had reactive gliosis detected with GFAP stain. The reactive gliosis, consisting of enlarged astrocytes, was present only in the CA1 region of the hippocampus. The 13 experimental brains examined with GFAP included all 6 of the experimental animals with normal H&E stains: 4 were normal, 2 had reactive gliosis. Moreover, staining for reactive gliosis highlighted inconspicuous H&E lesions that could easily be overlooked.
In all, 16 of 20 experimental brains had focal pathology. The lesions consisted of either pyramidal neuronal death (best seen with H&E) and/or reactive gliosis with enlarged astrocytes (best seen with GFAP). Brains obtained from animals in the ASR protocol, which were examined 7 d after the insult, were more likely to reveal abnormalities than brains obtained from animals in the MWM protocol, which were examined 21 d after the insult (11/11versus 5/9, Fisher exact p < 0.05). The CA1 lesions involved less than half of the structures in all but two cases and was often restricted to a few pyramidal perikarya.
DISCUSSION
MWM. The MWM was successful in detecting neurologic impairment in asphyxiated animals. Asphyxiated animals took longer than controls to escape the maze.
The MWM is well suited for evaluating the neurologic outcome of rats after asphyxial cardiac arrest. It is a versatile and robust tool for evaluating learning and memory(19, 20). It is resilient to motivational state (all rats are relatively equally motivated to escape water) and to the effects of circadian rhythm (rats are equally motivated to escape the water during the day or night). Although the maze is not a pleasurable experience, it is not so noxious as pain and is, therefore, less likely to result in a sustained hyperanxious state. The use of water eliminates the problem of scent which can confound the results of other maze tests. And lastly, because food is not used as positive reinforcement, the results are not confounded by the degree of hunger.
The validity of the MWM as a test of CNS function, specifically hippocampal function, is supported by studies demonstrating impaired performance after surgical or chemical ablation of the hippocampus(20). Impaired maze performance after hippocampal injury is consistent with the primary functions of the hippocampus: short-term and spatial memory. The hippocampus and its function are of particular relevance to postresuscitation brain injury because the hippocampus has been shown to be “selectively vulnerable” to hypoxia/ischemia(21). Histopathologic changes in the hippocampus, especially in the CA1 sector, have been demonstrated post-resuscitation in both animals(22, 23) and humans(24, 25). In addition, clinical studies reveal that the predominant cognitive deficit after cardiac arrest in humans is difficulty with short-term memory and spatial ability(26–32). The selective vulnerability of the hippocampus and the frequency of memory deficits (presumably the expression of hippocampal injury) in human survivors of cardiac arrest were the basis for using the MWM as an outcome measure in this model.
The finding of ischemic changes in the CA1 sector of the hippocampus after 7 min of asphyxia is in agreement with Katz et al.'s(23) work in which rats were asphyxiated for 8 min. The lower frequency of detected abnormalities in the MWM group compared with the ASR group may reflect a progression of lesions with resorption of dead neurons and resolution of reactive gliosis occurring between d 7 and 21. Therefore, the four asphyxiated animals without detected neuronal injury most likely did have injuries, but the injuries were below the threshold of detection for the histopathologic techniques used. Likewise, the presence of impaired MWM performance in animals without overt hippocampal injury is likely due to injury that is below the threshold of detection for the methods and timing used in this experiment.
Although we postulate that the impaired performance on the MWM is related to the hippocampal injury seen with histology, we have no proof of causality. Other possible explanations include: 1) impaired motor skills causing increased swim times, 2) impaired sensory input causing the water to be less adverse, 3) impaired visual acuity causing difficulty selecting and orienting to spatial clues, and 4) impaired ability to attend to visual clues. The unimpaired speed of swimming and the sometimes frenetic appearance of the experimental animals when placed in the tank make the first two alternative explanations unlikely. Although the visual acuity of the animals was not directly tested, the animals had at least some visual ability or they would have been unable to learn the task. The last possibility is the most plausible alternative. In fact, in the early trials, asphyxiated animals would leave the platform in search of another escape route with more frequency than controls. This (hyperactive?) behavior would result in less rearing time on the platform which could result in less time spent orienting to visual clues.
ASR. Asphyxiated animals demonstrated a hyperreflexic ASR with increased amplitude and decreased latency. The augmented response suggests that the auditory input of the animals was intact. The shortened latency and the shortened time interval from upper to lower extremity activation in asphyxiated animals suggest that the descending motor tracts were also intact. One plausible explanation of the hyperreflexia is an alteration in the normal balance of inhibitory and excitatory input from interneurons. Either a selective loss of inhibitory input or an increase in excitatory input could result in the hyperreflexia of asphyxiated animals. Of these two possibilities, a loss of inhibitory input is favored; in addition to creating a hyperreflexic ASR, a diminished inhibitory pool would have less“recruitable” input and, therefore, would provide less inhibition in response to a prestimulus. Support for the phenomenon of decreased inhibitory input resulting in hyperreflexia and diminished reflex inhibition is found elsewhere. Thompson et al.(33) foundγ-aminobutyric acid receptor dysfunction correlating with the hyperreflexia and diminished reflex inhibition of rats with spinal cord injury. Alternatively, the increased rectified integral of the ASR in asphyxiated animals could be secondary to alterations of the neuromuscular junction resulting in recruitment of a greater number of muscle fibers. However, this latter explanation does not account for the shortened latency intervals in asphyxiated animals.
The relationship of the histologic changes to the observed changes in the ASR requires further clarification. The ASR is routed primarily through the brain stem, and the locus of ASR-prestimulus inhibition is in the lateral tegmentum. No significant histopathologic changes were detected in these areas, indicating that, if the injury is secondary to neuronal drop-out, the losses are subtle (consistent with the loss of sparse modulating interneurons) or possibly due to failure of synaptic transmission. Regardless, the alteration of the ASR response in asphyxiated animals indicates that a more extensive brain injury exists which is below the threshold of detection for the histologic techniques used in this experiment. The possibility of a more extensive pattern of injury which includes deeper brain stuctures is supported by Katz's(40) work examining the histopathology of rats after a longer duration (8 min) of asphyxia.
Limitations. A possible limitation of this study is the absence of monitoring for secondary events which could result in altered neurologic outcome. Specifically, any hypotension and/or hypoxia occurring after removal of the femoral artery catheter would not have been detected. Hypotension status post-resuscitation has been shown to alter the extent and pattern of neuronal injury(34, 35). In addition, unobserved or subclinical seizures occurring during the recovery period could alter the neurologic outcome of survivors. Nonetheless, the neurologic and neuropathologic outcome is quite uniform in this model, suggesting that uncontrolled post-exposure events are either inconsequential or evenly distributed so as to affect outcome uniformly and thus enable testing of neuroprotective therapies with relatively few animals.
The use of adult (versus juvenile) rats is another limitation of this study. Ultimately, we are interested in neurologic injury secondary to asphyxial cardiac arrest because of its importance to the pediatric population. Specifically, we are interested in respiratory-induced cardiac arrest beyond the newborn period. Therefore, it would have been preferable to study immature rats. Unfortunately, the difficulties of instrumenting smaller animals and managing their post-injury airway secretions limited our investigation to adult animals. Another limitation of studying adult animals is the relative maturity of their behavioral paradigms and lack of cerebral plasticity compared with immature animals. The cerebral response to injury in rats is likely to differ at varying ages, just as the cerebral response of a 1-y-old human may differ from a 10-y-old.
Context. Investigations of the physiologic response to hypoxic/ischemic injury have led to the development of potential neuroprotective therapies(8, 36). Models for the evaluation of neurologic injury status post asphyxial cardiac arrest are necessary to test these therapies. Excluding perinatal asphyxia research, however, CNS injury secondary to asphyxia has not been well studied. Compared with the more commonly studied global complete ischemia (as occurs during sudden cardiac arrest), asphyxia results in lower tissue pH, higher tissue Pco2, greater edema, greater parenchymal hemorrhage, and increased disruption of the blood-brain barrier(6–9). In addition, before cardiovascular collapse and complete cessation of cerebral perfusion, asphyxia results in a period of low flow cerebral perfusion. This “trickle flow” continues to deliver substrate (glucose), which is anaerobically metabolized to lactic acid, thereby exacerbating the tissue acidosis and worsening cerebral injury(7, 22, 37). This combination of pathophysiologic characteristics occurring with asphyxia results in a different and more severe pattern of central nervous injury compared with other oxygen deprivation states(6, 34, 38, 39). Furthermore, there is evidence that the response to neuroprotective therapy after asphyxia may differ from the response after other causes of the hypoxic/ischemic injury(6). These considerations support development of asphyxial cardiac arrest models for the evaluation of neuroprotective strategies. Lastly, the investigation of asphyxial injury is particularly important for the pediatric population in which respiratory compromise is the most frequent cause of cardiopulmonary arrest(10–12).
CONCLUSION
The rat asphyxial arrest/neurologic outcome model described is attractive because the insult is easily administered, the animal is inexpensive, and the quantitative outcome measures enable assessment of statistically significant treatment effects. Another advantage is the large amount of information already available regarding rat behavior, neurochemistry, and neurohistology. Further work with this model is desirable to establish additional causal relationships, to define secondary insults, and to validate the model under different metabolic circumstances. This model promises rapid, inexpensive, and quantitative testing of the efficacy of neuroprotective agents in need ofin vivo assessment.
Abbreviations
- MWM:
-
Morris water maze
- ASR:
-
acoustic startle reflex
- H&E:
-
hematoxylin-eosin
- GFAP:
-
glial fibrillary acidic protein
- ANOVA:
-
analysis of variance
References
Kaasik AE, Nilsson L, Siesjo BK 1970 The effect of asphyxia upon the lactate, pyruvate and bicarbonate concentrations of brain tissue and cisternal CSF, and upon the tissue concentrations of phosphocreatine and adenine nucleotides in anesthetized rats. Acta Physiol Scand 78: 433–447
Hendrickx HH, Rao GR, Safar P, Grisvold SE 1984 Asphyxia, cardiac arrest and resuscitation in rats: short term recovery. Resuscitation 12: 97–116
Hendrickx HH, Safar P, Miller A 1984 Asphyxia, cardiac arrest and resuscitation in rats: long term behavioral changes. Resuscitation 12: 117–128
Hendrickx HH, Safar P, Baer BP, Basford RE 1984 Brain lactate and alanineglutamate ratios during and after asphyxia in rats. Resuscitation 12: 129–140
Thiringer K, Hrbek A, Karlsson K, Rosen KG, Kjellmer I 1987 Post-asphyxial cerebral survival in newborn sheep after treatment with oxygen free radical scavengers and a calcium antagonist. Pediatr Res 22: 62–66
Vaagenes P, Safar P, Moossy J, Rao G, Diven W, Cantadore R 1988 Differences in the effects of CNS treatments after ventricular fibrillation (VF) vs. asphyxiation (A) cardiac arrest (CA) in dog models. Crit Care Med 16: 447( abstr)
Safar P 1985 Long-term animal outcome models for cardiopulmonary-cerebral resuscitation research. Crit Care Med 13: 936–940
Kochanek PM 1988 Novel pharmacologic approaches to brain resuscitation after cardiorespiratory arrest in the pediatric patient. Crit Care Clin 4: 661–677
Lindner KH, Ahnefeld FW, Bowdler IM 1990 Cardiopulmonary resuscitation with interposed abdominal compression after asphyxial or fibrillatory cardiac arrest in pigs. Anesthesiology 72: 675–681
Eisenberg M, Bergner L, Hallstrom A 1983 Epidemiology of cardiac arrest and resuscitation in children. Ann Emerg Med 12: 672–674
Safranek DJ, Eisenberg MS, Larsen MP 1992 The epidemiology of cardiac arrest in young adults. Ann Emerg Med 21: 1102–1106
Hickey RW, Cohen DM, Strausbaugh S, Dietrich A 1995 Pediatric patients requiring CPR in the prehospital setting. Ann Emerg Med 25: 495–501
Brandeis R, Brandys Y, Yehuda S 1989 The use of the morris water maze in the study of memory and learning. Int J Neurosci 48: 29–69
Leitner DS, Powers AS, Hoffman HS 1980 The neural substrate of the startle response. Physiol Behav 25: 291–297
Davis M 1989 Neural systems involved in fear-potentiated startle. Ann NY Acad Sci 563: 165–183
Ison JR, McAdam DW, Hammond GR 1973 Latency and amplitude changes in the acoustic startle reflex of the rat produced by variation in auditory pre-stimulation. Physiol Behav 10: 1035–1039
Leitner DS, Powers AS, Stitt CL, Hoffman HS 1981 Midbrain reticular formation involvement in the inhibition of acoustic startle. Physiol Behav 26: 259–268
Hoffman HS, Ison JR 1980 Reflex modification in the domain of startle: I. Some empirical findings and their implications for how the nervous system processes sensory input. Psychol Rev 87: 175–189
Morris R 1984 Development of a water-maze procedure for studying spatial learning in the rat. J Neurosci Methods 11: 47–60
Morris RG, Garrud P, Rawlins JNP, O'Keefe J 1982 Place navigation impaired in rats with hippocampal lesions. Nature 297: 681–683
Weisfeldt ML, Halperin HR 1986 Cardiopulmonary resuscitation: beyond cardiac massage. Circulation 74: 443–448
Myers RE, Yamaguchi S 1977 Nervous system effects of cardiac arrest in monkeys. Arch Neurol 34: 65–74
Katz L, Sim KM, Radovsky A, Neumar R, Ubmeyer U, Safar P 1992 Asphyxial cardiac arrest survival model in rats with quantitative brain histopathologic evaluation. Ann Emerg Med 21: 633( abstr)
Vogel FS 1979 The morphologic consequences of cerebral hypoxia. Adv Neurol 26: 147–154
Petito CK, Feldmann E, Pulsinelli WA, Plum F 1987 Delayed hippocampal damage in humans following cardiorespiratory arrest. Neurology 37: 1281–1286
Bengtsson M, Holmberg S, Jansson B 1969 A psychiatric-psychological investigation of patients who had survived circulatory arrest. Acta Psychiatr Scand 45: 327–346
Bergner L, Hallstrom AP, Bergner M, Eisenberg MS, Cobb LA 1985 Health status of survivors of cardiac arrest and myocardial infarction controls. Am J Public Health 75: 1321–1323
Zola-Morgan S, Squire LR, Amaral DG 1986 Human amnesia and the medial temporal region: enduring memory impairment following a bilateral lesion limited to field CA1 of the hippocampus. J Neurosci 6: 2950–2967
Volpe BT, Holtzman JD, Hirst W 1986 Further characterization of patients with amnesia after cardiac arrest: preserved recognition of memory. Neurology 36: 408–411
Bertini G, Giglioli C, Giovannini F, Bartoletti A, Cricelli F, Margheri M, Russo L, Taddei T, Taiti A 1990 Neuropsychological outcome of survivors of out-of-hospital cardiac arrest. J Emerg Med 8: 407–412
Roine RO, Kajaste S, Kaste M 1993 Neuropsychological sequelae of cardiac arrest. JAMA 269: 237–242
Morris RD, Krawiecki NS, Wright JA, Walter LW 1993 Neuropsychological, academic, and adaptive functioning in children who survive in-hospital cardiac arrest and resuscitation. J Learn Disabil 26: 46–51
Thompson FJ, Parmer R, Fessler RG 1993 Is spinal cord injury induced frequency-hyperreflexia related to intraspinal GABAb receptor dysfunction? Eleventh Annual Neurotrauma Symposium (abstr)
Miller JR, Myers RE 1972 Neuropathology of systemic circulatory arrest in adult monkeys. Neurology 22: 888–904
de Courten-Myers GM, Fogelson HM, Kleinholz M, et al 1989 Hypoxic brain and heart injury thresholds in piglets. Biomed Biochim Acta 48:S143–S148
Kochanek PM 1993 Ischemic and traumatic brain injury: pathobiology and cellular mechanisms. Crit Care Med 21:S333–S335
Siesjo BK 1988 Mechanisms of ischemic brain damage. Crit Care Med 16: 954–963
de Courten-Myers G, Kleinholz M, Wagner KR, Myers RE 1991 Asphyxia- compared to cardiac arrest-induced brain damage is more extensive and uniquely involves thalamus and brainstem. Neurology 41: 337( abstrt)
Morimoto Y, Kemmotsu O, Kitami K, Matsubara I, Tedo I 1993 Acute brain swelling after out-of-hospital cardiac arrest: pathogenesis and outcome. Crit Care Med 21: 104–110
Katz L, Ebmeyer U, Safar P, Radovsky A, Neumar R 1995 J Cereb Blood Flow Metab (in press)
Acknowledgements
The authors are grateful to Dr. Jean Powers and John Hayes for their help with statistical analysis, and Drs. Bradford Stokes and Charles Brown for their review of the manuscript. We are especially indebted to Drs. Larry Katz and Robert Neumar for their help and advice with the asphyxial model of cardiac arrest in rats.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hickey, R., Akino, M., Strausbaugh, S. et al. Use of the Morris Water Maze and Acoustic Startle Chamber to Evaluate Neurologic Injury after Asphyxial Arrest in Rats. Pediatr Res 39, 77–84 (1996). https://doi.org/10.1203/00006450-199601000-00011
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199601000-00011
This article is cited by
-
Brain Resuscitation in the Drowning Victim
Neurocritical Care (2012)