Abstract
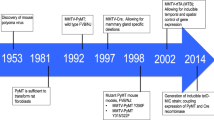
Elevated expression of the cysteine protease cathepsin B (CTSB) has been correlated with a poor prognosis for cancer patients. In order to model high CTSB expression in mammary cancer, transgenic mice expressing human CTSB were crossed with transgenic polyoma virus middle T oncogene breast cancer mice (mouse mammary tumor virus-PymT), resulting in a 20-fold increase in cathepsin B activity in the tumors of double-transgenic animals. CTSB expression did not affect tumor onset, but CTSB transgenic mice showed accelerated tumor growth with significant increase in weight for end-stage tumors, as well as an overall worsening in their histopathological grades. Notably, the lung metastases in the CTSB transgenic animals were found to be both significantly larger and to occur at a significantly higher frequency. Ex vivo analysis of primary PymT tumor cells revealed no significant effects from elevated CTSB levels on tumor cell characteristics, that is, the formation of tumor cell colonies and the sprouting of invasive strands from PymT cell spheroids. However, tumors from CTSB-overexpressing mice showed increased numbers of tumor-associated B cells and mast cells. In addition, more CD31+ endothelial cells were detected in these tumors, correlating with higher levels of vascular endothelial growth factor (VEGF) being present in the tumor and serum. We conclude that elevated proteolytic CTSB activity facilitates progression and metastasis of PymT-induced mammary carcinomas, and is associated with increased immune cell infiltration, enhanced VEGF levels and the promotion of tumor angiogenesis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Allavena P, Sica A, Solinas G, Porta C, Mantovani A . (2008). The inflammatory micro-environment in tumor progression: the role of tumor-associated macrophages. Crit Rev Oncol Hematol 66: 1–9.
Andreu P, Johansson M, Affara NI, Pucci F, Tan T, Junankar S et al. (2010). FcRgamma activation regulates inflammation-associated squamous carcinogenesis. Cancer Cell 17: 121–134.
Barrett AJ . (1992). Cellular proteolysis. An overview. Ann NY Acad Sci 674: 1–15.
Berdowska I . (2004). Cysteine proteases as disease markers. Clin Chim Acta 342: 41–69.
Brix K, Dunkhorst A, Mayer K, Jordans S . (2008). Cysteine cathepsins: cellular roadmap to different functions. Biochimie 90: 194–207.
Buck MR, Karustis DG, Day NA, Honn KV, Sloane BF . (1992). Degradation of extracellular-matrix proteins by human cathepsin B from normal and tumour tissues. Biochem J 282 (Part 1): 273–278.
Caglic D, Kosec G, Bojic L, Reinheckel T, Turk V, Turk B . (2009). Murine and human cathepsin B exhibit similar properties: possible implications for drug discovery. Biol Chem 390: 175–179.
Chang SH, Kanasaki K, Gocheva V, Blum G, Harper J, Moses MA et al. (2009). VEGF-A induces angiogenesis by perturbing the cathepsin-cysteine protease inhibitor balance in venules, causing basement membrane degradation and mother vessel formation. Cancer Res 69: 4537–4544.
Coulibaly S, Schwihla H, Abrahamson M, Albini A, Cerni C, Clark JL et al. (1999). Modulation of invasive properties of murine squamous carcinoma cells by heterologous expression of cathepsin B and cystatin C. Int J Cancer 83: 526–531.
Coussens LM, Raymond WW, Bergers G, Laig-Webster M, Behrendtsen O, Werb Z et al. (1999). Inflammatory mast cells up-regulate angiogenesis during squamous epithelial carcinogenesis. Genes Dev 13: 1382–1397.
Crivellato E, Nico B, Ribatti D . (2008). Mast cells and tumour angiogenesis: new insight from experimental carcinogenesis. Cancer Lett 269: 1–6.
de Visser KE, Korets LV, Coussens LM . (2005). De novo carcinogenesis promoted by chronic inflammation is B lymphocyte dependent. Cancer Cell 7: 411–423.
Del Rosso M, Fibbi G, Pucci M, D'Alessio S, Del Rosso A, Magnelli L et al. (2002). Multiple pathways of cell invasion are regulated by multiple families of serine proteases. Clin Exp Metastasis 19: 193–207.
DeNardo DG, Coussens LM . (2007). Inflammation and breast cancer. Balancing immune response: crosstalk between adaptive and innate immune cells during breast cancer progression. Breast Cancer Res 9: 212.
Dennemarker J, Lohmuller T, Mayerle J, Tacke M, Lerch MM, Coussens LM et al. (2010). Deficiency for the cysteine protease cathepsin L promotes tumor progression in mouse epidermis. Oncogene 29: 1611–1621.
Du R, Lu KV, Petritsch C, Liu P, Ganss R, Passegue E et al. (2008). HIF1alpha induces the recruitment of bone marrow-derived vascular modulatory cells to regulate tumor angiogenesis and invasion. Cancer Cell 13: 206–220.
Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG et al. (2010). NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature 464: 1357–1361.
Egeblad M, Werb Z . (2002). New functions for the matrix metalloproteinases in cancer progression. Nat Rev Cancer 2: 161–174.
Elston CW, Ellis IO . (1991). Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19: 403–410.
Folkman J . (2002). Role of angiogenesis in tumor growth and metastasis. Semin Oncol 29: 15–18.
Gocheva V, Wang HW, Gadea BB, Shree T, Hunter KE, Garfall AL et al. (2010). IL-4 induces cathepsin protease activity in tumor-associated macrophages to promote cancer growth and invasion. Genes Dev 24: 241–255.
Gocheva V, Zeng W, Ke D, Klimstra D, Reinheckel T, Peters C et al. (2006). Distinct roles for cysteine cathepsin genes in multistage tumorigenesis. Genes Dev 20: 543–556.
Gondi CS, Lakka SS, Yanamandra N, Olivero WC, Dinh DH, Gujrati M et al. (2004). Adenovirus-mediated expression of antisense urokinase plasminogen activator receptor and antisense cathepsin B inhibits tumor growth, invasion, and angiogenesis in gliomas. Cancer Res 64: 4069–4077.
Green KA, Lund LR . (2005). ECM degrading proteases and tissue remodelling in the mammary gland. Bioessays 27: 894–903.
Guy CT, Cardiff RD, Muller WJ . (1992). Induction of mammary tumors by expression of polyomavirus middle T oncogene: a transgenic mouse model for metastatic disease. Mol Cell Biol 12: 954–961.
Halle A, Hornung V, Petzold GC, Stewart CR, Monks BG, Reinheckel T et al. (2008). The NALP3 inflammasome is involved in the innate immune response to amyloid-beta. Nat Immunol 9: 857–865.
Hanahan D, Weinberg RA . (2000). The hallmarks of cancer. Cell 100: 57–70.
Hawinkels LJ, Zuidwijk K, Verspaget HW, de Jonge-Muller ES, van Duijn W, Ferreira V et al. (2008). VEGF release by MMP-9 mediated heparan sulphate cleavage induces colorectal cancer angiogenesis. Eur J Cancer 44: 1904–1913.
Houseweart MK, Pennacchio LA, Vilaythong A, Peters C, Noebels JL, Myers RM . (2003). Cathepsin B but not cathepsins L or S contributes to the pathogenesis of unverricht-lundborg progressive myoclonus epilepsy (EPM1). J Neurobiol 56: 315–327.
Jedeszko C, Sloane BF . (2004). Cysteine cathepsins in human cancer. Biol Chem 385: 1017–1027.
Joyce JA, Pollard JW . (2009). Microenvironmental regulation of metastasis. Nat Rev Cancer 9: 239–252.
Katz HR, Lobell RB . (1995). Expression and function of Fc gamma R in mouse mast cells. Int Arch Allergy Immunol 107: 76–78.
Lin EY, Jones JG, Li P, Zhu L, Whitney KD, Muller WJ et al. (2003). Progression to malignancy in the polyoma middle T oncoprotein mouse breast cancer model provides a reliable model for human diseases. Am J Pathol 163: 2113–2126.
Mai J, Finley Jr RL, Waisman DM, Sloane BF . (2000). Human procathepsin B interacts with the annexin II tetramer on the surface of tumor cells. J Biol Chem 275: 12806–12812.
Mantovani A, Allavena P, Sica A, Balkwill F . (2008). Cancer-related inflammation. Nature 454: 436–444.
Mohamed MM, Sloane BF . (2006). Cysteine cathepsins: multifunctional enzymes in cancer. Nat Rev Cancer 6: 764–775.
Nagy JA, Dvorak AM, Dvorak HF . (2007). VEGF-A and the induction of pathological angiogenesis. Annu Rev Pathol 2: 251–275.
Orimo A, Gupta PB, Sgroi DC, Arenzana-Seisdedos F, Delaunay T, Naeem R et al. (2005). Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell 121: 335–348.
Pollard JW . (2004). Tumour-educated macrophages promote tumour progression and metastasis. Nat Rev Cancer 4: 71–78.
Premzl A, Zavasnik-Bergant V, Turk V, Kos J . (2003). Intracellular and extracellular cathepsin B facilitate invasion of MCF-10A neoT cells through reconstituted extracellular matrix in vitro. Exp Cell Res 283: 206–214.
Rawlings ND, Barrett AJ, Bateman A . (2010). MEROPS: the peptidase database. Nucleic Acids Res 38: D227–D233.
Ribatti D, Vacca A, Nico B, Crivellato E, Roncali L, Dammacco F . (2001). The role of mast cells in tumour angiogenesis. Br J Haematol 115: 514–521.
Rozhin J, Sameni M, Ziegler G, Sloane BF . (1994). Pericellular pH affects distribution and secretion of cathepsin B in malignant cells. Cancer Res 54: 6517–6525.
Sevenich L, Schurigt U, Sachse K, Gajda M, Werner F, Muller S et al. (2010). Synergistic antitumor effects of combined cathepsin B and cathepsin Z deficiencies on breast cancer progression and metastasis in mice. Proc Natl Acad Sci USA 107: 2497–2502.
Shin M, Kadowaki T, Iwata J, Kawakubo T, Yamaguchi N, Takii R et al. (2007). Association of cathepsin E with tumor growth arrest through angiogenesis inhibition and enhanced immune responses. Biol Chem 388: 1173–1181.
Takai T . (2005). Fc receptors and their role in immune regulation and autoimmunity. J Clin Immunol 25: 1–18.
Tummalapalli P, Spomar D, Gondi CS, Olivero WC, Gujrati M, Dinh DH et al. (2007). RNAi-mediated abrogation of cathepsin B and MMP-9 gene expression in a malignant meningioma cell line leads to decreased tumor growth, invasion and angiogenesis. Int J Oncol 31: 1039–1050.
Turk V, Kos J, Turk B . (2004). Cysteine cathepsins (proteases)—on the main stage of cancer? Cancer Cell 5: 409–410.
Van Damme J, Struyf S, Opdenakker G . (2004). Chemokine-protease interactions in cancer. Semin Cancer Biol 14: 201–208.
Vasiljeva O, Korovin M, Gajda M, Brodoefel H, Bojic L, Kruger A et al. (2008). Reduced tumour cell proliferation and delayed development of high-grade mammary carcinomas in cathepsin B-deficient mice. Oncogene 27: 4191–4199.
Vasiljeva O, Papazoglou A, Kruger A, Brodoefel H, Korovin M, Deussing J et al. (2006). Tumor cell-derived and macrophage-derived cathepsin B promotes progression and lung metastasis of mammary cancer. Cancer Res 66: 5242–5250.
Vasiljeva O, Reinheckel T, Peters C, Turk D, Turk V, Turk B . (2007). Emerging roles of cysteine cathepsins in disease and their potential as drug targets. Curr Pharm Des 13: 387–403.
Werb Z, Vu TH, Rinkenberger JL, Coussens LM . (1999). Matrix-degrading proteases and angiogenesis during development and tumor formation. Apmis 107: 11–18.
Acknowledgements
The Tg(CTSB)+/0 mice were kindly provided by Dr L Pennacchio, Genomics Division, Lawrence Berkeley Laboratory. We thank Anne Schwinde, Ulrike Reif, Lisa Christiansson and Anna Heisswolf for excellent technical assistance. This work was supported by European Commission FP7 Grant 201279 (Microenvimet), Deutsche Forschungsgemeinschaft SFB 850 Project B7, and by the Excellence Initiative of the German Federal and State Governments (EXC 294 and GSC-4, Spemann Graduate School).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Oncogene website
Rights and permissions
About this article
Cite this article
Sevenich, L., Werner, F., Gajda, M. et al. Transgenic expression of human cathepsin B promotes progression and metastasis of polyoma-middle-T-induced breast cancer in mice. Oncogene 30, 54–64 (2011). https://doi.org/10.1038/onc.2010.387
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/onc.2010.387
Keywords
This article is cited by
-
Expression signature, prognosis value and immune characteristics of cathepsin F in non-small cell lung cancer identified by bioinformatics assessment
BMC Pulmonary Medicine (2021)
-
The secreted inhibitor of invasive cell growth CREG1 is negatively regulated by cathepsin proteases
Cellular and Molecular Life Sciences (2021)
-
A bi-directional dialog between vascular cells and monocytes/macrophages regulates tumor progression
Cancer and Metastasis Reviews (2021)
-
Lysosomal trafficking mediated by Arl8b and BORC promotes invasion of cancer cells that survive radiation
Communications Biology (2020)
-
Lysosomal quality control of cell fate: a novel therapeutic target for human diseases
Cell Death & Disease (2020)