Key Points
-
Deglutition is the act or process of swallowing and is one of the most complex reflex neural activities, involving the highly coordinated interplay of swallowing and breathing
-
By 34 weeks gestational age, most neonates are capable of successful sucking and swallowing if born at this early stage; however, the respiratory system is not yet fully established at this point
-
In healthy preterm neonates, swallow-induced (primary) peristalsis and peristalsis elicited by oesophageal distension (secondary) can be identified as the chief mechanisms of bolus clearance at 26 and 32 weeks gestational age, respectively
-
A swallowing disorder is defined as difficulty swallowing; key symptoms in infancy are excessive regurgitation, food refusal, choking and gagging, and chronic and/or recurrent respiratory symptoms
-
Gastro-oesophageal reflux is predominantly caused by transient relaxation of the lower oesophageal sphincter, which can develop into GERD due to multiple factors (for example, insufficient clearance and buffering of refluxate)
-
Although survival rates in patients with oesophageal atresia are high, surgical complications and long-term oesophageal morbidities, which are mainly related to oesophageal motility disorders, occur in almost all patients
Abstract
Deglutition, or swallowing, refers to the process of propulsion of a food bolus from the mouth into the stomach and involves the highly coordinated interplay of swallowing and breathing. At 34 weeks gestational age most neonates are capable of successful oral feeding if born at this time; however, the maturation of respiration is still in progress at this stage. Infants can experience congenital and developmental pharyngeal and/or gastrointestinal motility disorders, which might manifest clinically as gastro-oesophageal reflux (GER) symptoms, feeding difficulties and/or refusal, choking episodes and airway changes secondary to micro or overt aspiration. These problems might lead to impaired nutritional intake and failure to thrive. These gastrointestinal motility disorders are mostly classified according to the phase of swallowing in which they occur, that is, the oral preparatory, oral, pharyngeal and oesophageal phases. GER is a common phenomenon in infancy and is referred to as GERD when it causes troublesome complications. GER is predominantly caused by transient relaxation of the lower oesophageal sphincter. In oesophageal atresia, oesophageal motility disorders develop in almost all patients after surgery; however, a congenital origin of disordered motility has also been proposed. This Review highlights the prenatal development of upper gastrointestinal motility and describes the most common motility disorders that occur in early infancy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Dodds, W. J. The physiology of swallowing. Dysphagia 3, 171–179 (1989).
Dodds, W. J., Stewart, E. T. & Logemann, J. A. Physiology and radiology of the normal oral and pharyngeal phases of swallowing. Am. J. Radiol. 154, 953–963 (1990).
Rommel, N., De Meyer, A. M., Feenstra, L. & Veereman-Wauters, G. The complexity of feeding problems in 700 infants and young children presenting to a tertiary care institution. J. Pediatr. Gastroenterol. Nutr. 37, 75–84 (2003).
Raju, T. N., Higgins, R. D., Stark, A. R. & Leveno, K. J. Optimizing care and outcome for late-preterm (near-term) infants: a summary of the workshop sponsored by the National Institute of Child Health and Human Development. Pediatrics 118, 1207–1214 (2006).
Michou, E. & Hamdy, S. Cortical in put in control of swallowing. Curr. Opin. Otolaryngol. Head Neck Surg. 17, 166–171 (2009).
Mittal, R. K. Longitudinal muscle of the esophagus: its role in esophageal health and disease. Curr. Opin. Gastroenterol. 29, 421–430 (2013).
Guan, J. et al. Fetal development of regulatory mechanisms for body fluid homeostasis. Braz. J. Med. Biol. Res. 41, 446–454 (2008).
Ross, M. G. & Nijland, M. J. Fetal swallowing: relation to amniotic fluid regulation. Clin. Obstet. Gynecol. 40, 352–365 (1997).
Delaney, A. L. & Arvedson, J. C. Development of swallowing and feeding: prenatal through the first year of life. Dev. Disabil. Res. Rev. 14, 105–117 (2008).
Miller, J. L., Sonies, B. C. & Macedonia, C. Emergence of oropharyngeal, laryngreal and swallowing activity in the developing fetal upper aerodigestive tract: an ultrasound evaluation. Early Hum. Dev. 71, 61–87 (2003).
Lau, C., Alagugurusamy, R., Schanler, R., Smith, E. & Shulman, R. Characterization of the developmental stages of sucking in preterm infants during bottle feeding. Acta Paeditr. 89, 846–852 (2000).
Lau, C. & Kusnierczyk, I. Quantitative evaluation of infant's non-nutritive and nutritive sucking. Dysphagia 16, 58–67 (2001).
Rommel, N. et al. Development of pharyngo-esophageal physiology during swallowing in the preterm infant. Neurogastroenterol. Motil. 23, e401–e408 (2011).
Mizuno, K. & Ueda, A. The maturation and coordination of sucking, swallowing, and respiration in preterm infants. J. Pediatr. 142, 36–40 (2003).
Da Costa, S. P. et al. The development of sucking patterns in preterm, small-for-gestational age infants. J. Pediatr. 157, 603–609 (2010).
Bu'Lock, F., Woolridge, M. W. & Baum, J. D. Development of co-ordination of sucking, swallowing and breathing: ultrasound study of term and preterm infants. Dev. Med. Child. Neurol. 32, 669–678 (1990).
Lau, C. & Hurst, N. Oral feeding in infants. Curr. Probl. Pediatr. 29, 105–124 (1999).
Palmer, M. M. & van den Berg, K. A. A closer look at neonatal sucking. Neonatal Netw. 17, 77–79 (1998).
Qureshi, M. A., Vice, F. L., Taciak, V. L., Bosma, J. F. & Gewolb, I. H. Changes in rhythmic suckle feeding in term infants in the forst month of life. Dev. Med. Child. Neurol. 44, 34–39 (2002).
Jadcherla, S. R., Duong, H. Q., Hoffmann, C., Hoffmann, R. & Shaker, R. Characteristics of upper oesophageal sphincter and oesophageal body during maturation in healthy human neonates compared with adults. Neurogastroenterol. Motil. 17, 663–670 (2005).
Davidson, G. P., Dent, J. & Willing, J. Monitoring of upper oesophageal sphincter pressure in children. Gut 32, 607–611 (1991).
Jadcherla, J. R. et al. Esophageal sensation in premature human neonates: temporal relationships and implications of aerodigestive reflexes and electrocortical arousals. Am. J. Physiol. Gastrointest. Liver Physiol. 302, G134–G144 (2011).
Omari, T. et al. Measurement of upper esophageal sphincter tone and relaxation during swallowing in premature infants. Am. J. Physiol. 277, 862–866 (1999).
Willing, J., Davidson, G. P., Dent, J. & Cook, I. Effect of gastro-esophageal reflux on upper oesophageal sphincter motility in children. Gut 34, 904–910 (1993).
Malinger, G., Levine, A. & Rotmensch, S. The fetal esophagus: anatomical and physiological ultrasonographic characterization using a high-resolution linear transducer. Ultrasound Obstet. Gynecol. 24, 500–505 (2004).
Brugger, P. C., Weber, M. & Prayer, D. Magnetic resonance imaging of the normal fetal esophagus. Ultrasound Obstet. Gynecol. 38, 568–574 (2011).
Bowie, J. D. & Clair, M. R. Fetal swallowing and regurgitation: observation of normal and abnormal activity. Radiology 144, 877–878 (1982).
Omari, T. I. et al. Esophageal body and lower esophageal sphincter function in healthy premature infants. Gastroenterology 109, 1757–1764 (1995).
Hendrix, T. R. Coordination of peristalsis in the pharynx and esophagus. Dysphagia 8, 74–78 (1993).
Omari, T. I. et al. Characterisation of relaxation of the lower oesophageal sphincter in healthy premature infants. Gut 40, 370–375 (1997).
Omari, T. I. et al. Mechanisms of gastroesophageal reflux in healthy premature infants. J. Pediatr. 133, 650–654 (1998).
Jadcherla, S. R., Duong, H. Q., Hoffman, R. G. & Shaker, R. Esophageal body and upper esophageal sphincter motor responses to esophageal provocation during maturation in preterm newborns. J. Pediatr. 143, 31–38 (2003).
Jadcherla, S. R., Hoffmann, R. G. & Shaker, R. Effect of maturation of the magnitude of mechanosensitive and chemosensitive reflexes in the premature human esophagus. J. Pediatr. 149, 77–82 (2006).
Jadcherla, S. R., Gupta, A., Stoner, E., Fernadez, S. & Shaker, R. Pharyngeal swallowing: defining pharyngeal and upper esophageal sphincter relationships in human neonates. J. Pediatr. 151, 597–603 (2007).
Omari, T. et al. Characterization of esophageal body and lower esophageal sphincter motor function in the very premature neonate. J. Pediatr. 135, 517–521 (1999).
Gupta, A. et al. Effect of postnatal maturation on the mechanisms of esophageal propulsion in preterm human neonates: primary and secondary peristalsis. Am. J. Gastroenterol. 104, 411–419 (2009).
Ghosh, S. K., Janiak, P., Schwizer, W., Hebbard, G. S. & Brasseur, J. G. Physiology of the esophageal pressure transition zone: spate contraction waves above and below. Am. J. Physiol. Gastrointest. Liver Physiol. 290, 568–576 (2006).
Staiano, A., Boccia, G., Salvia, G., Zappulli, D. & Clouse, R. E. Development of esophageal peristalsis in preterm and term neonates. Gastroenterology 132, 1718–1725 (2007).
Staiano, A., Boccia, G., Miele, E. & Clouse, R. E. Segemental characteristics of oesophageal peristalsis in paediatric patients. Neurogastroenterol. Motil. 20, 19–26 (2008).
Pena, E. M. et al. Lower esophageal sphincter relaxation reflex kinetics: effects of peristaltic reflexes and maturation in human premature neonates. Am. J. Physiol. Gastrointest. Liver Physiol. 299, 1386–1395 (2010).
Rohof, W. O., Hirsch, D. P. & Boeckxtaens, G. E. Pathophysiology and management of gastroesophageal reflux disease. Minerva Gastroenterol. Dietol. 55, 289–300 (2009).
Thach, B. T. Maturation and transformation of reflexes that protect the laryngeal airway from liquid aspiration from fetal to adult life. Am. J. Med. 111, 69S–77S (2001).
Van der Velde, L. et al. Prolongation of the laryngeal chemoreflex after inhibition of the rostral ventral medulla in piglets: a role in SIDS? J. Appl. Physiol. 94, 1883–1895 (2003).
Dragomir, A., Akay, Y., Curran, A. K. & Akay, M. Investigating the complexity of respiratory patterns during the laryngeal chemoreflex. J. Neuroeng. Rehabil. 5, 17 (2008).
Jadcherla, S. R. Pathophsyiology of aerodigestive pulmonary disorders in the neonate. Clin. Perinatol. 39, 639–654 (2012).
Shaker, R. et al. Pharyngoglottal closure reflex: characterization in healthy young, elderly and dysphagic patients with predeglutitive aspiration. Gerontology 49, 12–20 (2003).
Dua, K. S. et al. Effect of systemic alcohol and nicotine on airway protective reflexes. Am. J. Gastroenterol. 104, 2431–2438 (2009).
Lang, I. M., Dana, N., Medda, B. K. & Shaker, R. Mechanisms of airway protection during retching, vomiting and swallowing. Am. J. Physiol. Gastrointest. Liver Physiol. 283, 529–536 (2002).
Medda, B. K. et al. Relative contribution of various airway protective mechanisms to prevention of aspiration during swallowing. Am. J. Physiol. Gastrointest. Liver Physiol. 284, G933–G939 (2003).
Arvedson, J. C. & Lefton-Greiff, M. A. in Pediatric Videofluoroscopic Swallow Studies: a Professional Manual with Caregiver Guidelines 13–37 (The Psychological Corporation, 1998).
Kramer, S. S. & Monahan-Eicher, P. The evaluation of pediatric feeding abnormalities. Dysphagia 8, 215–224 (1993).
Burklow, K. A., Phelps, A. N., Schultz, J. R., McConnel, K. & Rudolph, C. Classifying complex pediatric feeding disorders. J. Pediatr. Gastroenterol. Nutr. 27, 143–147 (1998).
Cook, I. J. & Kahrilas, P. J. AGA technical review on the management of oropharyngeal dysphagia. Gastroenterology 116, 455–478 (1999).
DeMatteo, C., Matovich, D. & Hjartarson, A. Comparison of clinical and videofluoroscopic evaluation of children with feeding and swallowing difficulties. Dev. Med. Child. Neurol. 47, 149–157 (2005).
Newman, L. A., Keckley, C., Petersen, M. C. & Hamner, A. Swallowing function and medical diagnoses in infants suspected of dysphagia. Pediatrics 108, 106 (2001).
Illingworth, R. S. Sucking and swallowing difficulties in infancy: diagnostic problem of dysphagia. Arch. Dis. Child. 44, 655–665 (1969).
Wolf, L. S. & Glass, R. P. in Feeding and Swallowing Disorders in Infancy: Assessment and Management 336–347 (Therapy Skill Builders, 1992).
Warms, T. & Richards, J. “Wet voice” as a predictor of penetration and aspiration in oropharyngeal dysphagia. Dysphagia 15, 84–88 (2000).
Lee, J. H., Chang, Y. S. & Yoo, H. S., Swallowing dysfunction in very low birth weight infants with oral feeding desaturation. World J. Pediatr. 7, 337–343 (2011).
Gewolb, I. H. & Vice, F. L. Maturational changes in the rhythms, patterning, and coordination of respiration and swallow during feeding in preterm and term infants. Dev. Med. Child. Neurol. 48, 589–594 (2006).
Gewolb, I. H. & Vice, F. L. Abnormalities in the coordination of respiration and swallow in preterm infants with bronchopulmonary dysplasia. Dev. Med. Child. Neurol. 48, 595–599 (2006).
Mizuno, K. et al. Infants with bronchopulmonary dysplasia suckle with weak pressures to maintain breathing during feeding. Pediatrics 120, 1035–1042 (2007).
Nelson, S. P., Chen, E. H., Syniar, G. M. & Christoffel, K. K. Prevalence of symptoms of gastroesophageal reflux during infancy: a pediatric practice-based survey. Pediatric Practice Research Group. Arch. Pediatr. Adolesc. Med. 151, 569–571 (1997).
Vandenplas, Y. et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN). J. Pediatr. Gastroenterol. Nutr. 49, 498–547 (2009).
Newell, S. J., Booth, I. W., Morgan, M. E., Durbin, G. M. & McNeish, A. S. Gastro-oesophageal reflux in preterm infants. Arch. Dis. Child. 64, 780–786 (1989).
El-Mouzan, M. I., Abdullah, A. M., Al-Sanie, A. M. & Al-Khalifah, S. I. Pattern of gastroesophageal reflux in children. Saudi Med. J. 22, 419–422 (2001).
Sherman, P. M. et al. A global, evidence-based consensus on the definition of gastroesophageal reflux disease in the pediatric population. Am. J. Gastroenterol. 104, 1278–1295 (2009).
Hegar, B. et al. Natural evolution of regurgitation in healthy infants. Acta Paediatr. 98, 1189–1193 (2009).
Cresi, F. et al. Prognostic values of multichannel intraluminal impedance and pH monitoring in newborns with symptoms of gastroesophageal reflux disease. J. Pediatrics 162, 770–775 (2013).
Omari, T. I. et al. Mechanisms of gastro-esophageal reflux in preterm and term infants with reflux disease. Gut 51, 475–479 (2002).
Verklan, M. T. Bronchopulmonary dysplasia: its effects upon the heart and lungs. Neonatal Netw. 16, 5–12 (1997).
Franzi, S., Martin, C., Cox, M. & Dent, J. Response of canine lower esophageal sphincter to gastric distension. Am. J. Physiol. 259, 380–384 (1999).
Pouderoux, P., Verdier, E. & Kahrilas, P. J. Patterns of esophageal inhibition during swallowing, pharyngeal stimulation, and transient LES relaxation. Lower esophageal sphincter. Am. J. Physiol. Gastrointest. Liver Physiol. 284, 242–247 (2003).
Trudgill, N. J. & Riley, S. A. Transient lower esophageal sphincter relaxations are no more frequent in patients with gastroesophageal reflux disease than in asymptomatic volunteers. Am. J. Gastroenterol. 96, 2569–2574 (2001).
Scheffer, R. C. et al. Elicitation of transient lower oesophageal sphincter relaxations in response to gastric distension and meal ingestion. Neurogastroenterol. Motil. 14, 647–655 (2002).
Mittal, R. K., Holloway, R. H., Penagini, R., Blackshaw, L. A. & Dent, J. Transient lower esophageal sphincter relaxation. Gastroenterology 109, 601–610 (1995).
Boeckxstaens, G. E. et al. Involvement of cholecystokinin A receptors in transient lower esophageal sphincter relaxations triggered by gastric distension. Am. J. Gastroenterol. 93, 1823–1828 (1998).
Van Wijk, M. P., Benninga, M. A., Davidson, G. P., Haslam, R. & Omari, T. I. Small amounts of feed can trigger TLESR in the right lateral position in infants. J. Pediatr. 156, 744–748 (2010).
Mittal, R. K., Chiareli, C., Liu, J. & Shaker, R. Characteristics of lower esophageal sphincter relaxation induced by pharyngeal stimulation with minute amounts of water. Gastroenterology 111, 378–384 (1996).
Sifrim, D. et al. Composition of the postprandial refluxate in patients with gastroesophageal reflux disease. Am. J. Gastroenterol. 96, 647–655 (2001).
Salvia, G. et al. Effect of intragastric volume and osmolality on mechanisms of gastroesophageal reflux in children with gastroesophageal reflux disease. Am. J. Gastroenterol. 96, 1725–1732 (2001).
Mittal, R. K. & McCallum, R. W. Characteristics and frequency of the lower esophageal sphincter in patients with reflux esophagitis. Gastroenterology 95, 593–599 (1988).
Trudgill, N. J. & Riley, S. A. Transient lower esophageal sphincter relaxations are no more frequent in patients with gastroesophageal reflux disease than in asymptomatic volunteers. Am. J. Gastroenterol. 96, 2569–2574 (2001).
Sifrim, D. et al. Acid, nonacid and gas reflux in patients with gastroesophageal reflux disease during ambulatory 24-hour pH-impedance recordings. Gastroenteroogy 120, 1588–1598 (2001).
Lee, Y. L. & McColl, K. E. L. Pathophysiology of gastroesophageal reflux disease. Best Pract. Res. Clin. Gastroenterol. 27, 339–351 (2013).
Vandenplas, Y. & Hassal, E. Mechanism of gastroesophageal reflux and reflux disease. J. Pediatr. Gastroenterol. Nutr. 35, 117–124 (2002).
Murray, J. A. & Camilleri, M. The fall and rise of the hiatal hernia. Gastroenterology 119, 1779–1781 (2000).
Beaumont, H., Bennink, R. J., de Jong, J. & Boeckxstaens, G. E. The position of the acid pocket as a major risk factor for acidic reflux in healthy subjects and patients with GORD. Gut 59, 441–451 (2010).
Rohof, W. O. et al. Effect of azithromycin on acid reflux, hiatus hernia and proximal acid pocket in the postprandial period. Gut 61, 1670–1677 (2012).
Penagini, R. & Bravi, I. The role of delayed gastric emptying and impaired oesophageal body motility. Best Pract. Res. Clin. Gastroenterol. 24, 831–845 (2010).
Knatten, C. K. et al. Gastric emptying in children with gastroesophageal reflux and in healthy children. J. Pediatr. Surg. 48, 1856–1861 (2013).
Sager, S. et al. Temporal relationship between gastroesophageal reflux and rate of gastric emptying in children. Nucl. Med. Commun. 31, 1059–1062 (2010).
Argon, M. et al. Relationship between gastric emptying and gastroesophageal reflux in infants and children. Clin. Nucl. Med. 31, 262–265 (2006).
Cresi, F. et al. Relationship between gastro-oesophageal reflux and gastric activity in newborns assessed by combined intraluminal impedance, pH metry and epigastric impedance. Neurogastroenterol. Motil. 18, 361–368 (2006).
Di Ciaula, A., Portincasa, P., Di Terlizzi, L., Paternostro, D. & Palasciano, G. Ultrasonographic study of postcibal gastro-esophageal reflux and gastric emptying in infants with recurrent respiratory disease. World J. Gastroenterol. 14, 7296–7301 (2005).
Aktas, A., Ciftçi, I. & Caner, B. The relation between the degree of gastro-oesophageal reflux and the rate of gastric emptying. Nucl. Med. Commun. 20, 907–910 (1999).
Ewer, A. K., Durbin, G. M., Morgan, M. E. & Booth, I. W. Gastric emptying and gastro-oesophageal reflux in preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 75, F117–F121 (1996).
Billeaud, C., Guillet, J. & Sandler, B. Gastric emptying in infants with or without gastro-oesophageal reflux according to the type of milk. Eur. J. Clin. Nutr. 44, 577–583 (1990).
Sistonen, S. J. et al. Esophageal morbitiy and function in adults with repaired esophageal atresia with tracheooesophageal fistula: a population-based long-term follow-up. Ann. Surg. 251, 1167–1173 (2010).
Koziarkiewicz, M., Taczalska, A. & Paiseczna-Piotrowska, A. Long-term follow-up of children with congenital diaphragmatic hernia-observations from a single institution. Eur. J. Pediatr. Surg. http://dx.doi.org/10.1055/s-0033-1357751.
Button, B. M. et al. Gastroesophageal reflux (symptomatic and silent): a potentially significant problem in patients with cystic fibrosis before and after lung transplantation. J. Heart Lung Transplant. 24, 1522–1529 (2005).
Jadcherla, S. R. et al. Practice variance, prevalence, and economic burden of premature infants diagnosed with GERD. Hosp. Pediatr. 3, 335–341 (2013).
Akinola, E., Rosenkrantz, T. S., Pappagallo, M., McKay, K. & Hussain, N. Gastroesophageal reflux in infants <32 weeks gestational age at birth: lack of relationship to chronic lung disease. Am. J. Perinatol. 21, 57–62 (2004).
Quitadamo, P. et al. Total and abdominal obesity are risk factors for gastroesophageal reflux symptoms in children. J. Pediatr. Gastroenterol. Nutr. 55, 72–75 (2012).
Lightdale, J. R. & Gemse, D. A. Gastroesophageal reflux: management guidance for the paediatrician. Pediatrics 131, e1684–e1695 (2013).
Vandenplas, Y. Management of paediatric GERD. Nat. Rev. Gastroenterol. Hepatol. 11, 147–157 (2013).
Hegar, B. & Vandenplas, Y. Gastroesophageal reflux: natural evolution, diagnostic approach and treatment. Turk J. Pediatr. 55, 1–7 (2013).
Van der Pol, R. J. et al. Diagnostic accuracy of tests in pediatric gastroesophageal reflux disease. J. Pediatr. 162, 983–987 (2013).
Rode, H., Stunden, R. J., Millar, A. J. & Cywes, S. Esophageal pH assessment of gastroesophageal reflux in 18 patients and the effect of two prokinetic agents: cisapride and metoclopramide. J. Pediatr. Surg. 22, 931–934 (1987).
Tolia, V., Calhoun, J., Kuhns, L. & Kauffman, R. E. Randomized, prospective double-blind trial of metoclopramide and placebo for gastroesophageal reflux in infants. J. Pediatr. 115, 141–145 (1989).
Van der Pol, R. J. et al. Efficacy of proton-pump inhibitors in children with gastroesophageal reflux disease: a systematic review. Pediatrics 127, 925–935 (2011).
Chicella, M. F. et al. Prokinetic drug therapy in children: a review of current options. Ann. Pharmacother. 39, 706–711 (2005).
Hill, D. J. et al. Role of food protein intolerance in infants with persistent distress attributed to reflux esophagitis. J. Pediatr. 136, 641–647 (2000).
Nielsen, R. G., Bindslev-Jensen, C., Kruse-Andersen, S. & Husby, S. Severe gastroesophageal reflux disease and cow milk hypersensitivity in infants and children: disease association and evaluation of a new challenge procedure. J. Pediatr. Gastroenterol. Nutr. 39, 383–391 (2004).
Iacono, G. et al. Gastroesophageal reflux and cow's milk allergy in infants: a prospective study. J. Allergy Clin. Immunol. 97, 822–827 (1996).
Goyal, A. et al. Esophageal atresia and tracheoesphageal fistula. Arch. Dis. Child. Fetal Neonatal Ed. 91, 381–384 (2000).
Koivusalo, A. I., Pakarinen, M. P. & Rintala, R. J. Modern outcomes of oesophageal atresia: single centre experience over the last twenty years. J. Pediatr. Surg. 48, 297–303 (2013).
Taylor, A. C. et al. Gastroesophageal reflux and related pathology in adults who were born with esophageal atresia: a long-term follow-up study. Clin. Gastroenterol. Hepatol. 5, 702–706 (2007).
Deurloo, J. A. & Aronson, D. C. Possibility that esophageal atresia (EA) carries an increased risk for esophageal carcinoma. J. Pediatr. Surg. 41, 876–877 (2006).
Deurloo, J. A., Klinkenberg, E. C., Ekkelkamp, S., Heij, H. A. & Aronson, D. C. Adults with corrected oesophageal atresia: is oesophageal function associated with complaints and/or quality of life? Pediatr. Surg. Int. 24, 537–541 (2008).
Koivusalo, A., Pakarinen, M. P. & Rintala, R. J. The cumulative incidence of significant gastroesophageal reflux in patients with oesophageal atresia with a distal fistula: a systematic clinical, pH-metric and endoscopic follow-up study. J. Pediatr. Surg. 42, 370–374 (2007).
Kovesi, T. & Rubin, S. Long-term complications of congenital esophageal atresia and/or tracheooesophageal fistula. Chest 126, 915–925 (2004).
Lemoine, C. et al. Characterization of esophageal motility following esophageal atresia repair using high-resolution esophageal manometry. J. Pediatr. Gastroenterol. Nutr. 56, 609–614 (2013).
Dutta, H. H., Grover, V. P., Dwivedi, S. N. & Bhatnagar, V. Manometric evaluation of postoperative patients of esophageal atresia and trachea-esophageal fistula. Eur. J. Pediatr. Surg. 11, 371–376 (2001).
Orringer, M. B., Kirsh, M. M. & Sloan, H. Long-term esophageal function following repair of esophageal atresia. Ann. Surg. 186, 436–443 (1997).
Duranceau, A. et al. Motor function of the esophagus after repair of esophageal atresia and tracheoesophageal fistula. Surgery 82, 116–123 (1977).
Tomaselli, V. et al. Long-term evaluation of oesophageal function in patients treated at birth for esophageal atresia. Pediatr. Surg. Int. 19, 40–43 (2003).
Mittal, R. K. & Bhalla, V. Oesophageal motor functions and its disorders. Gut 53, 1536–1542 (2004).
Hoffman, I., DeGreef, T., Haesendonck, N. & Tack, J. Esophageal motility in children with suspected gastroesophageal reflux disease. J. Pediatr. Gastroenterol. Nutr. 50, 601–608 (2010).
Di Pace, M. R. et al. Evaluation of esophageal motility and reflux in children treated for esophageal atresia with the use of combined multichannel intraluminal impedance and pH monitoring. J. Pediatr. Surg. 46, 443–451 (2011).
Cheng, W. et al. Abnormalities of neuropeptides and neural markers in the esophagus of fetal rats with Adriamycin-induced esophageal atresia. J. Pediatr. Surg. 32, 1420–1423 (1997).
Cheng, W., Bishop, A. E., Spitz, L. & Polak, J. M. Abnormal enteric nerve morphology in atretic esophagus of fetal rats with Adriamycin-induced esophageal atresia. Pediatr. Surg. Int. 15, 8–10 (1999).
Deurloo, J. A., Smit, B. J., Ekkelkamp, S. & Aronson, D. C. Oesophageal atresia in premature infants: an analysis of morbidity and mortality over a period of 20 years. Acta Pediatr. 93, 394–399 (2004).
Qi, B. Q., Uemura, S., Farmer, P., Myers, N. A. & Hutson, J. M. Intrinsic inntervation of the oesophagus in fetal rats with oesophageal atresia. Pediatr. Surg. Int. 15, 2–7 (1999).
Nakazato, W., Landing, B. H. & Wells, T. R. Abnormal Auerbach plexus in the esophagus and stomach of patients with esophageal atresia and tracheoesophageal fistula. J. Pediatr. Surg. 21, 831–837 (1986).
Boleken, M. et al. Reduced neuronal innervation in the distal end of the proximal esophageal atretic segment in cases of esophageal atresia with distal tracheoesophageal fistula. World J. Surg. 31, 1512–1517 (2007).
Midrio, P., Alaggio, R. & Stojna, A. Reduction of interstitial cells of Cajal in esophageal atresia. J. Pediatr. Gastroenterol. Nutr. 51, 610–617 (2010).
Davies, M. R. Anatomy of the intrinsic motor nerve supply to mobilized segments of the oesophagus disrupted by dissection during repair of oesophageal atresia with distal fistula. Br. J. Surg. 83, 1268–1270 (1996).
Guo, W., Fonkalsrud, E. W. & Swaniker, F. Relationship of esophageal anastomotic tension to the development of gastroesophageal reflux. J. Pediatr. Surg. 32, 1337–1340 (1997).
Aspirot, A. & Faure, C. Esophaeal dysmotility: characterization and pathophysiology. Dis. Esophagus 26, 405–409 (2013).
Author information
Authors and Affiliations
Contributions
M.M.J.S. researched data for the article, provided substantial contribution to discussion of the content, wrote the article and reviewed/edited the manuscript before submission. N.R. wrote and reviewed/edited the manuscript before submission. T.I.O., M.A.B. and M.P.v.W. provided substantial contributions to discussion of the content and reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Singendonk, M., Rommel, N., Omari, T. et al. Upper gastrointestinal motility: prenatal development and problems in infancy. Nat Rev Gastroenterol Hepatol 11, 545–555 (2014). https://doi.org/10.1038/nrgastro.2014.75
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2014.75
This article is cited by
-
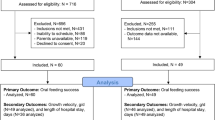
Characterization of Esophageal and Sphincter Reflexes across Maturation in Dysphagic Infants with Oral Feeding Success vs Infants requiring Gastrostomy
Dysphagia (2022)
-
Oesophageal dysphagia: manifestations and diagnosis
Nature Reviews Gastroenterology & Hepatology (2015)