Key Points
-
Genomic technologies have had a greater impact on paediatrics than on many other fields of medicine, and this discipline is leading the way in the implementation of clinical genomics.
-
Appropriate use of whole-exome sequencing (WES) or whole-genome sequencing (WGS) has the potential to curtail the diagnostic process for patients with rare and ultra-rare paediatric disorders, often avoiding the need for invasive and expensive investigations.
-
Although WES and WGS have enormous diagnostic power, data interpretation remains very challenging because of a high incidence of novel and ultra-rare benign variants, incomplete knowledge, false assignment of variant pathogenicity and even false association of genes with disease in the literature.
-
An accurate genetic diagnosis benefits a child by enabling a better understanding of their prognosis, more personalized treatment and tailored management and surveillance. A precise genetic diagnosis also enables accurate genetic advice for individuals and their relatives with increased reproductive choice and improved access to information and support from patient support groups, education, health and social care.
-
WES and WGS require considerable computational resources to process, analyse and store the vast data sets generated by these technologies. For clinicians, the issue of data storage and access is linked to the question of whether their duty of care is limited to finding a diagnosis for the child's immediate problems or whether it extends beyond the scope of the initial investigation.
-
In the future, stratified therapy for rare paediatric disease based on the specific genetic diagnosis is likely to be possible, and effective and affordable therapies are likely to become available through drug repurposing and innovation.
Abstract
The majority of rare diseases affect children, most of whom have an underlying genetic cause for their condition. However, making a molecular diagnosis with current technologies and knowledge is often still a challenge. Paediatric genomics is an immature but rapidly evolving field that tackles this issue by incorporating next-generation sequencing technologies, especially whole-exome sequencing and whole-genome sequencing, into research and clinical workflows. This complex multidisciplinary approach, coupled with the increasing availability of population genetic variation data, has already resulted in an increased discovery rate of causative genes and in improved diagnosis of rare paediatric disease. Importantly, for affected families, a better understanding of the genetic basis of rare disease translates to more accurate prognosis, management, surveillance and genetic advice; stimulates research into new therapies; and enables provision of better support.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Change history
19 February 2018
In Figure 2a of the above article, the resolution of microarrays was originally stated to be 50–100 Mb. The actual resolution is 50–100 kb. In addition, the key for Figure 2b referred to 30,000 coding variants instead of 20,000. These errors have been corrected online. Nature Reviews Genetics apologizes for these errors.
References
European Organisation for Rare Diseases. Rare Diseases: Understanding this Public Health Priority. (Eurodis, 2005).
Boycott, K. M. et al. International cooperation to enable the diagnosis of all rare genetic diseases. Am. J. Hum. Genet. 100, 695–705 (2017).
Quintana-Murci, L. Understanding rare and common diseases in the context of human evolution. Genome Biol. 17, 225 (2016).
Amberger, J., Bocchini, C. A., Scott, A. F. & Hamosh, A. Mckusick's online mendelian inheritance in man (OMIM). Nucleic Acids Res. 37, D793–D796 (2009).
Amberger, J. S., Bocchini, C. A., Schiettecatte, F., Scott, A. F. & Hamosh, A. OMIM.org: Online Mendelian Inheritance in Man (OMIM®), an online catalog of human genes and genetic disorders. Nucleic Acids Res. 43, D789–D798 (2015).
Yoon, P. W. et al. Contribution of birth defects and genetic diseases to pediatric hospitalizations. A population-based study. Arch. Pediatr. Adolesc. Med. 151, 1096–1103 (1997).
Dodge, J. A. et al. The importance of rare diseases: from the gene to society. Arch. Dis. Child 96, 791–792 (2011).
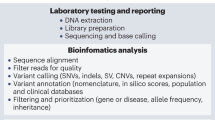
Wright, C. F. et al. Genetic diagnosis of developmental disorders in the DDD study: a scalable analysis of genome-wide research data. Lancet 385, 1305–1314 (2015). This is an important paper outlining a prototype clinical bioinformatics pipeline for the diagnosis of developmental disorders.
Deciphering Developmental Disorders Study. Prevalence and architecture of de novo mutations in developmental disorders. Nature 542, 433–438 (2017). This is a landmark paper highlighting the major contribution of de novo mutation to developmental disorders.
Austin, C. P. et al. Future of rare diseases research 2017-2027: an IRDiRC perspective. Clin. Transl Sci. https://doi.org/10.1111/cts.12500 (2017).
Grozeva, D. et al. Targeted next-generation sequencing analysis of 1,000 individuals with intellectual disability. Hum. Mutat. 36, 1197–1204 (2015).
Kochinke, K. et al. Systematic phenomics analysis deconvolutes genes mutated in intellectual disability into biologically coherent modules. Am. J. Hum. Genet. 98, 149–164 (2016).
Torgerson, P. R. & Mastroiacovo, P. The global burden of congenital toxoplasmosis: a systematic review. Bull. World Health Organ. 91, 501–508 (2013).
Del Campo, M. & Jones, K. L. A review of the physical features of the fetal alcohol spectrum disorders. Eur. J. Med. Genet. 60, 55–64 (2017).
Chavali, P. L. et al. Neurodevelopmental protein Musashi-1 interacts with the Zika genome and promotes viral replication. Science 357, 83–88 (2017).
Firth, H. V. & Wright, C. F. & DDD Study. The Deciphering Developmental Disorders (DDD) study. Dev. Med. Child Neurol. 53, 702–703 (2011).
Baynam, G. et al. The rare and undiagnosed diseases diagnostic service — application of massively parallel sequencing in a state-wide clinical service. Orphanet J. Rare Dis. 11, 77 (2016).
Doherty, E. S. et al. Muenke syndrome (FGFR3-related craniosynostosis): expansion of the phenotype and review of the literature. Am. J. Med. Genet. A 143A, 3204–3215 (2007).
Posey, J. E. et al. Resolution of disease phenotypes resulting from multilocus genomic variation. N. Engl. J. Med. 376, 21–31 (2017). This interesting paper focuses on diagnosing individuals with several independent rare genetic conditions.
Henn, B. M., Botigué, L. R., Bustamante, C. D., Clark, A. G. & Gravel, S. Estimating the mutation load in human genomes. Nat. Rev. Genet. 16, 333–343 (2015).
Boycott, K. M., Vanstone, M. R., Bulman, D. E. & MacKenzie, A. E. Rare-disease genetics in the era of next-generation sequencing: discovery to translation. Nat. Rev. Genet. 14, 681–691 (2013).
Samocha, K. E. et al. A framework for the interpretation of de novo mutation in human disease. Nat. Genet. 46, 944–950 (2014). This is a useful paper outlining a model for predicting the number of de novo mutations expected by chance across the genome, which is essential for robust discovery of genes that cause novel dominant de novo disorders.
Weiner, D. J. et al. Polygenic transmission disequilibrium confirms that common and rare variation act additively to create risk of autism spectrum disorders. Nat. Genet. 49, 978–985 (2017).
The 1000 Genomes Project Consortium. A map of human genome variation from population-scale sequencing. Nature 467, 1061–1073 (2010).
The 1000 Genomes Project Consortium. An integrated map of genetic variation from 1,092 human genomes. Nature 491, 56–65 (2012).
The 1000 Genomes Project Consortium. A global reference for human genetic variation. Nature 526, 68–74 (2015). This study presents a comprehensive account of the wealth of variation in the genomes of normal individuals.
Katsanis, S. H. & Katsanis, N. Molecular genetic testing and the future of clinical genomics. Nat. Rev. Genet. 14, 415–426 (2013).
Brewington, J. & Clancy, J. P. Diagnostic testing in cystic fibrosis. Clin. Chest Med. 37, 31–46 (2016).
Aartsma-Rus, A., Ginjaar, I. B. & Bushby, K. The importance of genetic diagnosis for Duchenne muscular dystrophy. J. Med. Genet. 53, 145–151 (2016).
Speicher, M. R. & Carter, N. P. The new cytogenetics: blurring the boundaries with molecular biology. Nat. Rev. Genet. 6, 782–792 (2005). This is a useful Review of microarray technologies and their use for the diagnosis of rare paediatric syndromes.
Shaw-Smith, C. et al. Microarray based comparative genomic hybridisation (array-CGH) detects submicroscopic chromosomal deletions and duplications in patients with learning disability/mental retardation and dysmorphic features. J. Med. Genet. 41, 241–248 (2004).
Crespi, B. J. & Procyshyn, T. L. Williams syndrome deletions and duplications: genetic windows to understanding anxiety, sociality, autism, and schizophrenia. Neurosci. Biobehav. Rev. 79, 14–26 (2017).
Sagoo, G. S. et al. Array CGH in patients with learning disability (mental retardation) and congenital anomalies: updated systematic review and meta-analysis of 19 studies and 13,926 subjects. Genet. Med. 11, 139–146 (2009).
Mardis, E. R. The impact of next-generation sequencing technology on genetics. Trends Genet. 24, 133–141 (2008).
Ansorge, W. J. Next-generation DNA sequencing techniques. N. Biotechnol. 25, 195–203 (2009).
Moorthie, S., Mattocks, C. J. & Wright, C. F. Review of massively parallel DNA sequencing technologies. Hugo J. 5, 1–12 (2011).
Vissers, L. E. L. M. et al. A clinical utility study of exome sequencing versus conventional genetic testing in pediatric neurology. Genet. Med. 19, 1055–1063 (2017). This is an excellent study of the impact of NGS in clinical practice.
Shashi, V. et al. The utility of the traditional medical genetics diagnostic evaluation in the context of next-generation sequencing for undiagnosed genetic disorders. Genet. Med. 16, 176–182 (2014).
Weiss, M. M. et al. Best practice guidelines for the use of next-generation sequencing applications in genome diagnostics: a national collaborative study of Dutch genome diagnostic laboratories. Hum. Mutat. 34, 1313–1321 (2013).
Sun, Y. et al. Next-generation diagnostics: gene panel, exome, or whole genome? Hum. Mutat. 36, 648–655 (2015).
Ece Solmaz, A. et al. Targeted multi-gene panel testing for the diagnosis of Bardet Biedl syndrome: Identification of nine novel mutations across BBS1, BBS2, BBS4, BBS7, BBS9, BBS10 genes. Eur. J. Med. Genet. 58, 689–694 (2015).
Schrijver, I. Hereditary non-syndromic sensorineural hearing loss. J. Mol. Diagn. 6, 275–284 (2004).
Myers, C. T. & Mefford, H. C. Advancing epilepsy genetics in the genomic era. Genome Med. 7, 91 (2015).
Mastrangelo, M. Novel genes of early-onset epileptic encephalopathies: from genotype to phenotypes. Pediatr. Neurol. 53, 119–129 (2015).
Cheng, A. Y., Teo, Y.-Y. & Ong, R. T.-H. Assessing single nucleotide variant detection and genotype calling on whole-genome sequenced individuals. Bioinformatics 30, 1707–1713 (2014).
Beck, T. F. & Mullikin, J. C., NISC Comparative Sequencing Program & Biesecker, L. G. Systematic evaluation of Sanger validation of next-generation sequencing variants. Clin. Chem. 62, 647–654 (2016).
Telenti, A. et al. Deep sequencing of 10,000 human genomes. Proc. Natl Acad. Sci. USA 113, 11901–11906 (2016).
Li, W. et al. Identifying human genome-wide CNV, LOH and UPD by targeted sequencing of selected regions. PLoS ONE 10, e0123081 (2014).
de Ligt, J. et al. Detection of clinically relevant copy number variants with whole-exome sequencing. Hum. Mutat. 34, 1439–1448 (2013).
Noll, A. C. et al. Clinical detection of deletion structural variants in whole-genome sequences. npj Genomic Med. 1, 16026 (2016).
Suzuki, T. et al. Precise detection of chromosomal translocation or inversion breakpoints by whole-genome sequencing. J. Hum. Genet. 59, 649–654 (2014).
Ellingford, J. M. et al. Validation of copy number variation analysis for next-generation sequencing diagnostics. Eur. J. Hum. Genet. 25, 719–724 (2017).
Budworth, H. & McMurray, C. T. A brief history of triplet repeat diseases. Methods Mol. Biol. 1010, 3–17 (2013).
Nowak, K. J. & Davies, K. E. Duchenne muscular dystrophy and dystrophin: pathogenesis and opportunities for treatment. EMBO Rep. 5, 872–876 (2004).
Singh, N. N., Seo, J., Rahn, S. J. & Singh, R. N. A multi-exon-skipping detection assay reveals surprising diversity of splice isoforms of spinal muscular atrophy genes. PLoS ONE 7, e49595 (2012).
Halvorsen, M. et al. Mosaic mutations in early-onset genetic diseases. Genet. Med. 18, 746–749 (2016).
Rios, J. J. & Delgado, M. R. Using whole-exome sequencing to identify variants inherited from mosaic parents. Eur. J. Hum. Genet. 23, 547–550 (2015).
Saudi Mendeliome Group. Comprehensive gene panels provide advantages over clinical exome sequencing for Mendelian diseases. Genome Biol. 16, 134 (2015).
van El, C. G. et al. Whole-genome sequencing in health care: recommendations of the European Society of Human Genetics. Eur. J. Hum. Genet. 21, 580–584 (2013).
Green, R. C. et al. ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genet. Med. 15, 565–574 (2013). This is a controversial paper advocating routine opportunistic screening of genomic sequence data in adults and children.
Matthijs, G. et al. Guidelines for diagnostic next-generation sequencing. Eur. J. Hum. Genet. 24, 2–5 (2016).
Boycott, K. et al. The clinical application of genome-wide sequencing for monogenic diseases in Canada: position statement of the Canadian College of Medical Geneticists. J. Med. Genet. 52, 431–437 (2015).
Ormondroyd, E. et al. “Not pathogenic until proven otherwise”: perspectives of UK clinical genomics professionals toward secondary findings in context of a Genomic Medicine Multidisciplinary Team and the 100,000 Genomes Project. Genet. Med. https://doi.org/10.1038/gim.2017.157 (2017).
Goldstein, D. B. et al. Sequencing studies in human genetics: design and interpretation. Nat. Rev. Genet. 14, 460–470 (2013).
Wright, C. F. et al. Making new genetic diagnoses with old data: iterative reanalysis and reporting from genome-wide data in 1133 families withdevelopmental disorders. Genet. Med. https://doi.org/10.1038/gim.2017.246 (2018).
Moorthie, S., Hall, A. & Wright, C. F. Informatics and clinical genome sequencing: opening the black box. Genet. Med. 15, 165–171 (2013).
Yen, J. L. et al. A variant by any name: quantifying annotation discordance across tools and clinical databases. Genome Med. 9, 7 (2017).
Danecek, P. et al. The variant call format and VCFtools. Bioinformatics 27, 2156–2158 (2011).
Endrullat, C., Glökler, J., Franke, P. & Frohme, M. Standardization and quality management in next-generation sequencing. Appl. Transl Genom. 10, 2–9 (2016).
Salgado, D., Bellgard, M. I., Desvignes, J.-P. & Béroud, C. How to identify pathogenic mutations among all those variations: variant annotation and filtration in the genome sequencing era. Hum. Mutat. 37, 1272–1282 (2016).
McLaren, W. et al. The ensembl variant effect predictor. Genome Biol. 17, 122 (2016).
Cingolani, P. et al. A program for annotating and predicting the effects of single nucleotide polymorphisms, SnpEff: SNPs in the genome of Drosophila melanogaster strain w1118; iso-2; iso-3. Fly 6, 80–92 (2012).
Desmet, F.-O. et al. Human Splicing Finder: an online bioinformatics tool to predict splicing signals. Nucleic Acids Res. 37, e67 (2009).
Soemedi, R. et al. Pathogenic variants that alter protein code often disrupt splicing. Nat. Genet. 49, 848–855 (2017).
Lek, M. et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature 536, 285–291 (2016). This is a landmark paper describing the ExAC database.
Popejoy, A. B. & Fullerton, S. M. Genomics is failing on diversity. Nature 538, 161–164 (2016).
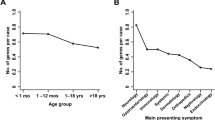
Retterer, K. et al. Clinical application of whole-exome sequencing across clinical indications. Genet. Med. 18, 696–704 (2016). This is a useful paper comparing the diagnostic yield of WES across different clinical indications.
Ansari, M. et al. Genetic heterogeneity in Cornelia de Lange syndrome (CdLS) and CdLS-like phenotypes with observed and predicted levels of mosaicism. J. Med. Genet. 51, 659–668 (2014).
Chambers, C., Jansen, L. A. & Dhamija, R. Review of commercially available epilepsy genetic panels. J. Genet. Couns. 25, 213–217 (2016).
Strande, N. T. et al. Evaluating the clinical validity of gene-disease associations: an evidence-based framework developed by the Clinical Genome Resource. Am. J. Hum. Genet. 100, 895–906 (2017).
Biesecker, L. G. Opportunities and challenges for the integration of massively parallel genomic sequencing into clinical practice: lessons from the ClinSeq project. Genet. Med. 14, 393–398 (2012).
Ghouse, J. et al. Numerous Brugada syndrome-associated genetic variants have no effect on J-point elevation, syncope susceptibility, malignant cardiac arrhythmia, and all-cause mortality. Genet. Med. 19, 521–528 (2017).
Landrum, M. J. et al. ClinVar: public archive of interpretations of clinically relevant variants. Nucleic Acids Res. 44, D862–868 (2016).
Deciphering Developmental Disorders Study. Large-scale discovery of novel genetic causes of developmental disorders. Nature 519, 223–228 (2015).
Köhler, S. et al. The Human Phenotype Ontology project: linking molecular biology and disease through phenotype data. Nucleic Acids Res. 42, D966–D974 (2014).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405–424 (2015).
Nykamp, K. et al. Sherloc: a comprehensive refinement of the ACMG-AMP variant classification criteria. Genet. Med. 19, 1105–1117 (2017).
Bragin, E. et al. DECIPHER: database for the interpretation of phenotype-linked plausibly pathogenic sequence and copy-number variation. Nucleic Acids Res. 42, D993–D1000 (2014).
Chatzimichali, E. A. et al. Facilitating collaboration in rare genetic disorders through effective matchmaking in DECIPHER. Hum. Mutat. 36, 941–949 (2015).
Kaye, J. The tension between data sharing and the protection of privacy in genomics research. Annu. Rev. Genom. Hum. Genet. 13, 415–431 (2012).
Gymrek, M., McGuire, A. L., Golan, D., Halperin, E. & Erlich, Y. Identifying personal genomes by surname inference. Science 339, 321–324 (2013).
Buske, O. J. et al. PhenomeCentral: a portal for phenotypic and genotypic matchmaking of patients with rare genetic diseases. Hum. Mutat. 36, 931–940 (2015).
Philippakis, A. A. et al. The Matchmaker Exchange: a platform for rare disease gene discovery. Hum. Mutat. 36, 915–921 (2015).
Sobreira, N., Schiettecatte, F., Valle, D. & Hamosh, A. GeneMatcher: a matching tool for connecting investigators with an interest in the same gene. Hum. Mutat. 36, 928–930 (2015).
ACMG Board Of Directors. Laboratory and clinical genomic data sharing is crucial to improving genetic health care: a position statement of the American College of Medical Genetics and Genomics. Genet. Med. 19, 721–722 (2017).
Ramoni, R. B. et al. The Undiagnosed Diseases Network: accelerating discovery about health and disease. Am. J. Hum. Genet. 100, 185–192 (2017).
Bowdin, S. et al. Recommendations for the integration of genomics into clinical practice. Genet. Med. 18, 1075–1084 (2016).
Thevenon, J. et al. Diagnostic odyssey in severe neurodevelopmental disorders: toward clinical whole-exome sequencing as a first-line diagnostic test. Clin. Genet. 89, 700–707 (2016).
Petrikin, J. E., Willig, L. K., Smith, L. D. & Kingsmore, S. F. Rapid whole genome sequencing and precision neonatology. Semin. Perinatol 39, 623–631 (2015).
Saunders, C. J. et al. Rapid whole-genome sequencing for genetic disease diagnosis in neonatal intensive care units. Sci. Transl Med. 4, 154ra135 (2012).
Miller, D. T. et al. Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am. J. Hum. Genet. 86, 749–764 (2010).
Meng, L. et al. Use of exome sequencing for infants in intensive care units: ascertainment of severe single-gene disorders and effect on medical management. JAMA Pediatr. 171, e173438 (2017).
Hartley, T. et al. Whole-exome sequencing is a valuable diagnostic tool for inherited peripheral neuropathies: outcomes from a cohort of 50 families. Clin. Genet. https://doi.org/10.1111/cge.13101 (2017).
Warr, A. et al. Exome sequencing: current and future perspectives. G3 5, 1543–1550 (2015).
Belkadi, A. et al. Whole-genome sequencing is more powerful than whole-exome sequencing for detecting exome variants. Proc. Natl Acad. Sci. USA 112, 5473–5478 (2015).
Boycott, K. M. & Innes, A. M. When one diagnosis is not enough. N. Engl. J. Med. 376, 83–85 (2017).
Robinson, E. B. et al. Genetic risk for autism spectrum disorders and neuropsychiatric variation in the general population. Nat. Genet. 48, 552–555 (2016).
Patel, K. A. et al. Type 1 diabetes genetic risk score: a novel tool to discriminate monogenic and type 1 diabetes. Diabetes 65, 2094–2099 (2016). This study provides a demonstration of the application of a genetic risk score derived from genome-wide association studies to discriminate between common complex and rare monogenic disease.
Oram, R. A. et al. A type 1 diabetes genetic risk score can aid discrimination between type 1 and type 2 diabetes in young adults. Diabetes Care 39, 337–344 (2016).
Adam, M. P. et al. GeneReviews® (University of Washington, Seattle, 2017).
Vissers, L. E. L. M., Gilissen, C. & Veltman, J. A. Genetic studies in intellectual disability and related disorders. Nat. Rev. Genet. 17, 9–18 (2016).
Tan, T. Y. et al. Diagnostic impact and cost-effectiveness of whole-exome sequencing for ambulant children with suspected monogenic conditions. JAMA Pediatr. 171, 855–862 (2017). This study presents evidence that cost-effectiveness is maximized by early application of WES in the diagnostic pathway of children with suspected monogenic conditions.
Stark, Z. et al. Prospective comparison of the cost-effectiveness of clinical whole-exome sequencing with that of usual care overwhelmingly supports early use and reimbursement. Genet. Med. 19, 867–874 (2017).
Stark, Z. et al. A prospective evaluation of whole-exome sequencing as a first-tier molecular test in infants with suspected monogenic disorders. Genet. Med. 18, 1090–1096 (2016).
Soden, S. E. et al. Effectiveness of exome and genome sequencing guided by acuity of illness for diagnosis of neurodevelopmental disorders. Sci. Transl Med. 6, 265ra168 (2014).
Willig, L. K. et al. Whole-genome sequencing for identification of Mendelian disorders in critically ill infants: a retrospective analysis of diagnostic and clinical findings. Lancet Respir. Med. 3, 377–387 (2015).
Konstan, M. W. et al. Assessment of safety and efficacy of long-term treatment with combination lumacaftor and ivacaftor therapy in patients with cystic fibrosis homozygous for the F508del-CFTR mutation (PROGRESS): a phase 3, extension study. Lancet Respir. Med. 5, 107–118 (2017).
Worthey, E. A. et al. Making a definitive diagnosis: successful clinical application of whole exome sequencing in a child with intractable inflammatory bowel disease. Genet. Med. 13, 255–262 (2011). This study provides the first published example where WES was successfully used in the clinic to diagnose and treat a child suffering from a severe rare disease.
Tarailo-Graovac, M. et al. Exome sequencing and the management of neurometabolic disorders. N. Engl. J. Med. 374, 2246–2255 (2016).
Stalke, A. et al. Diagnosis of monogenic liver diseases in childhood by next-generation sequencing. Clin. Genet. https://doi.org/10.1111/cge.13120 (2017).
Ormondroyd, E. et al. Insights from early experience of a Rare Disease Genomic Medicine Multidisciplinary Team: a qualitative study. Eur. J. Hum. Genet. 25, 680–686 (2017).
Moynihan, R., Doust, J. & Henry, D. Preventing overdiagnosis: how to stop harming the healthy. BMJ 344, e3502 (2012).
Newman-Toker, D. E. A unified conceptual model for diagnostic errors: underdiagnosis, overdiagnosis, and misdiagnosis. Diagnosis 1, 43–48 (2014).
Cummings, B. B. et al. Improving genetic diagnosis in Mendelian disease with transcriptome sequencing. Sci. Transl Med. 9, eaal5209 (2017). This is an excellent paper demonstrating the improved diagnostic power of combining transcriptome analysis with NGS for the diagnosis of rare neuromuscular disease.
Riordan, J. R. et al. Identification of the cystic fibrosis gene: cloning and characterization of complementary DNA. Science 245, 1066–1073 (1989).
Castellani, C. & CFTR2 Team. CFTR2: How will it help care? Paediatr. Respir. Rev. 14 (Suppl. 1), 2–5 (2013).
Claustres, M. et al. CFTR-France, a national relational patient database for sharing genetic and phenotypic data associated with rare CFTR variants. Hum. Mutat. 38, 1297–1315 (2017).
Bainbridge, M. N. et al. Whole-genome sequencing for optimized patient management. Sci. Transl Med. 3, 87re3 (2011).
Finkel, R. S. et al. Treatment of infantile-onset spinal muscular atrophy with nusinersen: a phase 2, open-label, dose-escalation study. Lancet 388, 3017–3026 (2016).
Finkel, R. S. et al. Nusinersen versus sham control in infantile-onset spinal muscular atrophy. N. Engl. J. Med. 377, 1723–1732 (2017).
Dever, D. P. et al. CRISPR/Cas9 β-globin gene targeting in human haematopoietic stem cells. Nature 539, 384–389 (2016).
Gaudelli, N. M. et al. Programmable base editing of A·T to G·C in genomic DNA without DNA cleavage. Nature 551, 464–471 (2017).
Cox, D. B. T. et al. RNA editing with CRISPR-Cas13. Science 358, 1019–1027 (2017).
Lionel, A. C. et al. Improved diagnostic yield compared with targeted gene sequencing panels suggests a role for whole-genome sequencing as a first-tier genetic test. Genet. Med. https://doi.org/10.1038/gim.2017.119 (2017).
Taylor-Cousar, J. L. et al. Tezacaftor-ivacaftor in patients with cystic fibrosis homozygous for Phe508del. N. Engl. J. Med. 377, 2013–2023 (2017).
Friedman, J. M. et al. Genomic newborn screening: public health policy considerations and recommendations. BMC Med. Genom. 10, 9 (2017).
Berg, J. S. et al. Newborn sequencing in genomic medicine and public health. Pediatrics 139, e20162252 (2017).
Dale, A. P. & Read, R. C. Genetic susceptibility to meningococcal infection. Expert Rev. Anti Infect. Ther. 11, 187–199 (2013).
Bønnelykke, K. & Ober, C. Leveraging gene-environment interactions and endotypes for asthma gene discovery. J. Allergy Clin. Immunol. 137, 667–679 (2016).
Michels, A. et al. Prediction and prevention of type 1 diabetes: update on success of prediction and struggles at prevention. Pediatr. Diabetes 16, 465–484 (2015).
Burke, W. et al. The translational potential of research on the ethical, legal, and social implications of genomics. Genet. Med. 17, 12–20 (2015).
Hercher, L. & Jamal, L. An old problem in a new age: revisiting the clinical dilemma of misattributed paternity. Appl. Transl Genom. 8, 36–39 (2016).
Jackson, L., Goldsmith, L., O'Connor, A. & Skirton, H. Incidental findings in genetic research and clinical diagnostic tests: a systematic review. Am. J. Med. Genet. A 158A, 3159–3167 (2012).
Botkin, J. R. et al. Points to consider: ethical, legal, and psychosocial implications of genetic testing in children and adolescents. Am. J. Hum. Genet. 97, 6–21 (2015).
Clarke, A. J. Managing the ethical challenges of next-generation sequencing in genomic medicine. Br. Med. Bull. 111, 17–30 (2014).
Wright, C. F., Middleton, A. & Parker, M. in Genomic Medicine Principles and Practice (eds Kumar, D. & Eng, C.) 250–258 (Oxford Univ. Press, 2014).
Anderson, J. A. et al. Parents perspectives on whole genome sequencing for their children: qualified enthusiasm? J. Med. Eth. 43, 535–539 (2016).
Horn, R. & Parker, M. Opening Pandora's box?: ethical issues in prenatal whole genome and exome sequencing. Prenat. Diagn. 23, 34–39 (2017).
Newson, A. J. Whole genome sequencing in children: ethics, choice and deliberation. J. Med. Eth. 43, 540–542 (2017).
Committee on Bioethics et al. Ethical and policy issues in genetic testing and screening of children. Pediatrics 131, 620–622 (2013).
Burstein, M. D., Robinson, J. O., Hilsenbeck, S. G., McGuire, A. L. & Lau, C. C. Pediatric data sharing in genomic research: attitudes and preferences of parents. Pediatrics 133, 690–697 (2014).
Wright, C. F., Hurles, M. E. & Firth, H. V. Principle of proportionality in genomic data sharing. Nat. Rev. Genet. 17, 1–2 (2016).
Muddyman, D., Smee, C., Griffin, H. & Kaye, J. Implementing a successful data-management framework: the UK10K managed access model. Genome Med. 5, 100 (2013).
Wilfond, B. S. & Carpenter, K. J. Incidental findings in pediatric research. J. Law Med. Eth. 36, 332–340 (2008).
Eldomery, M. K. et al. Lessons learned from additional research analyses of unsolved clinical exome cases. Genome Med. 9, 26 (2017).
Carrieri, D. et al. Recontacting in clinical genetics and genomic medicine? We need to talk about it. Eur. J. Hum. Genet. 25, 520–521 (2017).
Gliwa, C. & Berkman, B. E. Do researchers have an obligation to actively look for genetic incidental findings? Am. J. Bioeth 13, 32–42 (2013).
Crawford, G., Foulds, N., Fenwick, A., Hallowell, N. & Lucassen, A. Genetic medicine and incidental findings: it is more complicated than deciding whether to disclose or not. Genet. Med. 15, 896–899 (2013).
Clayton, E. W. Incidental findings in genetics research using archived DNA. J. Law Med. Eth. 36, 286–291 (2008).
Wolf, S. M. et al. Managing incidental findings and research results in genomic research involving biobanks and archived data sets. Genet. Med. 14, 361–384 (2012).
Kalia, S. S. et al. Recommendations for reporting of secondary findings in clinical exome and genome sequencing, 2016 update (ACMG SF v2.0): a policy statement of the American College of Medical Genetics and Genomics. Genet. Med. 19, 249–255 (2017).
Mand, C., Gillam, L., Delatycki, M. B. & Duncan, R. E. Predictive genetic testing in minors for late-onset conditions: a chronological and analytical review of the ethical arguments. J. Med. Eth. 38, 519–524 (2012).
Shkedi-Rafid, S., Fenwick, A., Dheensa, S. & Lucassen, A. M. Genetic testing of children for adult-onset conditions: opinions of the British adult population and implications for clinical practice. Eur. J. Hum. Genet. 23, 1281–1285 (2015).
Caga-anan, E. C. F., Smith, L., Sharp, R. R. & Lantos, J. D. Testing children for adult-onset genetic diseases. Pediatrics 129, 163–167 (2012).
Claustres, M. et al. Recommendations for reporting results of diagnostic genetic testing (biochemical, cytogenetic and molecular genetic). Eur. J. Hum. Genet. 22, 160–170 (2014).
Wright, C. F. et al. Policy challenges of clinical genome sequencing. BMJ 347, f6845 (2013).
FitzPatrick, D. R. Resequencing at scale in neurodevelopmental disorders. Nat. Genet. 49, 488–489 (2017).
Acknowledgements
The authors are all members of the management team of the Deciphering Developmental Disorders (DDD) Study, which undertakes independent research commissioned by the Health Innovation Challenge Fund [grant number HICF-1009-003], a parallel funding partnership between the Wellcome Trust and the Department of Health, and the Wellcome Trust Sanger Institute [grant number WT098051]. The views expressed in this publication are those of the authors and not necessarily those of the Wellcome Trust or the Department of Health. The study has UK Research Ethics Committee approval (10/H0305/83, granted by the Cambridge South REC, and GEN/284/12 granted by the Republic of Ireland REC). The research team acknowledges the support of the National Institute for Health Research, through the Comprehensive Clinical Research Network. This study makes use of DECIPHER, which is funded by the Wellcome Trust. H.V.F. is supported by The Wellcome Trust award 200990/Z/16/Z 'Designing, developing and delivering integrated foundations for genomic medicine'.
Author information
Authors and Affiliations
Contributions
C.F.W. and H.V.F. drafted and revised the manuscript. D.R.F. provided editorial input, designed some of the figures and contributed to the ideas and discussions on which the article is based.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
Glossary
- Developmental disorders
-
Diseases with their genesis in embryonic life or early fetal brain development.
- Structural variants
-
Blocks of DNA >1 kb that differ relative to the reference genome or general population, including inversions, balanced translocations and copy number variants (for example, deletions and duplications).
- Mosaicism
-
The presence of two or more populations of cells with different genotypes in an individual who has developed from a single fertilized egg.
- Penetrance
-
The proportion of individuals with a particular genotype who show features of the condition (however mildly). If some individuals with the genotype never show any features, the condition is said to have incomplete (or reduced) penetrance. If features develop with age, the condition is said to have age-dependent penetrance.
- Expressivity
-
The phenotypic variability and severity that a given genotype shows in individuals penetrant for the condition.
- Locus heterogeneity
-
When variants in a number of different genes independently cause the same phenotype.
- Allelic heterogeneity
-
When different mutations at the same locus cause the same phenotype.
- Monoallelic
-
Describes a mutation that affects only one copy of a gene. Autosomal dominant, de novo dominant or X-linked disorders are caused by a monoallelic pathogenic variant.
- Biallelic variants
-
Mutations that affect both copies of a gene. Autosomal recessive disorders are caused by pathogenic biallelic variants.
- Whole-exome sequencing
-
(WES). Next-generation sequencing of the entire protein-coding portion of the genome. In humans, the total length of coding and splicing regions is estimated to be ~35 Mb and comprises ~20,000 genes (1–2% of the genome).
- Whole-genome sequencing
-
(WGS). Next-generation sequencing of the entire genome, which, in humans, is typically ~3,000 Mb.
- Single-gene tests
-
Approaches that enable detailed analysis of a single gene. In addition to sequence analysis, they usually also include an assessment of dosage in order to detect exon-level deletions and duplications, which are often difficult to detect with current approaches to whole-exome sequencing and whole-genome sequencing.
- Cytogenetic tests
-
Genome-wide tests that analyse the number and structure of chromosomes, including copy number variants, but do not provide information about the DNA sequence.
- Karyotype
-
The chromosomal complement of a cell. Large-scale chromosomal imbalances can be detected using karyotyping approaches, such as imaging Giemsa-banded chromosomes with light microscopy.
- Copy number variants
-
(CNVs). Structural variants that involve either a deletion or a duplication of a section of DNA relative to the reference genome.
- Single nucleotide variants
-
(SNVs). Differences within a population, or between an individual and a reference genome, that affect a single base pair of DNA.
- Gene panels
-
Subsets of genes (usually linked to a particular phenotype) that are incorporated into a laboratory-based gene capture kit or that form the basis of computer-based virtual gene panels, which are applied to a subset of variant data from a clinical exome or a whole-exome sequencing and/or whole-genome sequencing assay.
- Minor allele frequencies
-
(MAFs). Measurements of how often the less common allele occurs at a given polymorphic locus.
- Human Phenotype Ontology
-
(HPO). A standardized vocabulary of phenotypic abnormalities encountered in human disease. Each term in the HPO describes a phenotypic abnormality, such as atrial septal defect. The HPO currently contains ~11,000 terms.
- Causative genotypes
-
Genotypes in which a single locus is perturbed and that have a high positive predictive value for a restricted pattern of morphological, biochemical or physiological features of clinical significance.
- Blended phenotype
-
A mixed phenotype that results from causal variants in two or more genes. The phenotypes may either be distinct, with discrete (composite) manifestations, or overlapping, with similar phenotypic manifestations that are impossible to disentangle.
- Genetic risk scores
-
Quantitative measures of genetic predisposition to a trait that are calculated from data for multiple (usually low-risk) genetic variants, which are usually obtained from genome-wide association studies.
- Pleiotropy
-
The phenomenon whereby variants in a single gene may cause multiple phenotypic expressions or disorders.
- Transcriptomics
-
A global approach for looking at gene expression patterns. This can involve measurements of thousands of genes simultaneously with microarrays or measurements of small numbers of genes that are facilitated by global sequence information from expressed sequence tag or genome-sequencing projects.
- Epigenomics
-
A global approach for looking at the complete collection of epigenetic marks, such as DNA methylation and histone modifications, and other molecules that can transmit epigenetic information, such as non-coding RNAs, that exist in a cell at any given point in time.
- Metabolomics
-
A global approach using quantitative analytical methods to look at the entire metabolic content of a cell or organism at a given time.
- Proteomics
-
A global approach for looking at the complete collection of proteins in a cell or tissue at a given time.
Rights and permissions
About this article
Cite this article
Wright, C., FitzPatrick, D. & Firth, H. Paediatric genomics: diagnosing rare disease in children. Nat Rev Genet 19, 253–268 (2018). https://doi.org/10.1038/nrg.2017.116
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrg.2017.116
This article is cited by
-
Trends in orphan medicinal products approvals in the European Union between 2010–2022
Orphanet Journal of Rare Diseases (2024)
-
GPAD: a natural language processing-based application to extract the gene-disease association discovery information from OMIM
BMC Bioinformatics (2024)
-
Long-read sequencing and optical mapping generates near T2T assemblies that resolves a centromeric translocation
Scientific Reports (2024)
-
Integrating non-mammalian model organisms in the diagnosis of rare genetic diseases in humans
Nature Reviews Genetics (2024)
-
The expanding diagnostic toolbox for rare genetic diseases
Nature Reviews Genetics (2024)