Abstract
Infections with human papillomavirus (HPV) are common and transmitted by direct contact. Although the great majority of infections resolve within 2 years, 13 phylogenetically related, sexually transmitted HPV genotypes, notably HPV16, cause — if not controlled immunologically or by screening — virtually all cervical cancers worldwide, a large fraction of other anogenital cancers and an increasing proportion of oropharyngeal cancers. The carcinogenicity of these HPV types results primarily from the activity of the oncoproteins E6 and E7, which impair growth regulatory pathways. Persistent high-risk HPVs can transition from a productive (virion-producing) to an abortive or transforming infection, after which cancer can result after typically slow accumulation of host genetic mutations. However, which precancerous lesions progress and which do not is unclear; the majority of screening-detected precancers are treated, leading to overtreatment. The discovery of HPV as a carcinogen led to the development of effective preventive vaccines and sensitive HPV DNA and RNA tests. Together, vaccination programmes (the ultimate long-term preventive strategy) and screening using HPV tests could dramatically alter the landscape of HPV-related cancers. HPV testing will probably replace cytology-based cervical screening owing to greater reassurance when the test is negative. However, the effective implementation of HPV vaccination and screening globally remains a challenge.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Bravo, I. G. & Félez-Sánchez, M. Papillomaviruses: viral evolution, cancer and evolutionary medicine. Evol. Med. Public Health 2015, 32–51 (2015).
Van Doorslaer, K. Evolution of the Papillomaviridae. Virology 445, 11–20 (2013).
Rodríguez, A. C. et al. Rapid clearance of human papillomavirus and implications for clinical focus on persistent infections. J. Natl Cancer Inst. 100, 513–517 (2008).
Bosch, F. X. et al. Comprehensive control of human papillomavirus infections and related diseases. Vaccine 31 (Suppl. 7), H1–H31 (2013). Summarizes the most current issues in HPV epidemiology and in preventing the diseases caused by HPV, which serves as a portal to the published literature and regional issues.
Guan, P. et al. Human papillomavirus types in 115,789 HPV-positive women: a meta-analysis from cervical infection to cancer. Int. J. Cancer 131, 2349–2359 (2012).
Plummer, M. et al. Global burden of cancers attributable to infections in 2012: a synthetic analysis. Lancet Glob. Health 4, e609–e616 (2016). Provides the most recent and definitive estimation of the role of HPV in cancer burden worldwide.
World Health Organization & International Agency for Research on Cancer. IARC Monographs on the evaluation of carcinogenic risks to humans. Volume 90. Human papillomaviruses. IARChttp://monographs.iarc.fr/ENG/Monographs/vol90/mono90.pdf (2007).
World Health Organization & International Agency for Research on Cancer. IARC Monographs on the evaluation of carcinogenic risks to humans. biological agents. Volume 100B: a review of human carcinogens. IARChttp://monographs.iarc.fr/ENG/Monographs/vol100B/mono100B.pdf (2012). The section on HPV is the authoritative consideration of which HPV types are carcinogenic and the reasoning underlying this classification.
Crosbie, E. J., Einstein, M. H., Franceschi, S. & Kitchener, H. C. Human papillomavirus and cervical cancer. Lancet 382, 889–899 (2013).
Vaccarella, S. et al. 50 years of screening in the Nordic countries: quantifying the effects on cervical cancer incidence. Br. J. Cancer 111, 965–969 (2014).
Alemany, L. et al. Human papillomavirus DNA prevalence and type distribution in anal carcinomas worldwide. Int. J. Cancer 136, 98–107 (2015).
De Vuyst, H., Clifford, G. M., Nascimento, M. C., Madeleine, M. M. & Franceschi, S. Prevalence and type distribution of human papillomavirus in carcinoma and intraepithelial neoplasia of the vulva, vagina and anus: a meta-analysis. Int. J. Cancer 124, 1626–1636 (2009).
Alemany, L. et al. Role of human papillomavirus in penile carcinomas worldwide. Eur. Urol. 69, 953–961 (2016).
de Martel, C. et al. Cancers attributable to infections among adults with HIV in the United States. AIDS 29, 2173–2181 (2015).
Castellsagué, X. et al. HPV involvement in head and neck cancers: comprehensive assessment of biomarkers in 3680 patients. J. Natl Cancer Inst. 108, djv403 (2016).
Combes, J.-D. & Franceschi, S. Role of human papillomavirus in non-oropharyngeal head and neck cancers. Oral Oncol. 50, 370–379 (2014).
Chaturvedi, A. K. et al. Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J. Clin. Oncol. 31, 4550–4559 (2013).
Kreimer, A. R. et al. Evaluation of human papillomavirus antibodies and risk of subsequent head and neck cancer. J. Clin. Oncol. 31, 2708–2715 (2013).
Liu, Z., Rashid, T. & Nyitray, A. G. Penises not required: a systematic review of the potential for human papillomavirus horizontal transmission that is non-sexual or does not include penile penetration. Sex. Health 13, 10–21 (2016).
Sundström, K. et al. Interactions between high- and low-risk HPV types reduce the risk of squamous cervical cancer. J. Natl Cancer Inst. 107, djv185 (2015).
Vaccarella, S. et al. Clustering of multiple human papillomavirus infections in women from a population-based study in Guanacaste, Costa Rica. J. Infect. Dis. 204, 385–390 (2011).
Wentzensen, N. et al. No evidence for synergy between human papillomavirus genotypes for the risk of high-grade squamous intraepithelial lesions in a large population-based study. J. Infect. Dis. 209, 855–864 (2014).
de Araujo-Souza, P. S. et al. Determinants of baseline seroreactivity to human papillomavirus type 16 in the Ludwig–McGill cohort study. BMC Infect. Dis. 14, 578 (2014).
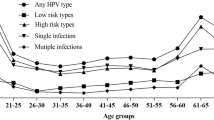
Bruni, L. et al. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J. Infect. Dis. 202, 1789–1799 (2010).
Plummer, M. et al. A 2-year prospective study of human papillomavirus persistence among women with a cytological diagnosis of atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesion. J. Infect. Dis. 195, 1582–1589 (2007).
Schiffman, M., Castle, P. E., Jeronimo, J., Rodriguez, A. C. & Wacholder, S. Human papillomavirus and cervical cancer. Lancet 370, 890–907 (2007).
Ronco, G. et al. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet 383, 524–532 (2014). Provides definitive evidence for why HPV testing is the preferred method of primary cervical cancer screening.
Giuliano, A. R. et al. The human papillomavirus infection in men study: human papillomavirus prevalence and type distribution among men residing in Brazil, Mexico, and the United States. Cancer Epidemiol. Biomarkers Prev. 17, 2036–2043 (2008).
Markowitz, L. E., Sternberg, M., Dunne, E. F., McQuillan, G. & Unger, E. R. Seroprevalence of human papillomavirus types 6, 11, 16, and 18 in the United States: National Health and Nutrition Examination Survey 2003–2004. J. Infect. Dis. 200, 1059–1067 (2009).
Lu, B. et al. Seroprevalence of human papillomavirus (HPV) type 6 and 16 vary by anatomic site of HPV infection in men. Cancer Epidemiol. Biomarkers Prev. 21, 1542–1546 (2012).
Garnock-Jones, K. P. & Giuliano, A. R. Quadrivalent human papillomavirus (HPV) types 6, 11, 16, 18 vaccine: for the prevention of genital warts in males. Drugs 71, 591–602 (2011).
Lehtinen, M. & Dillner, J. Clinical trials of human papillomavirus vaccines and beyond. Nat. Rev. Clin. Oncol. 10, 400–410 (2013).
Chung, C. H., Bagheri, A. & D'Souza, G. Epidemiology of oral human papillomavirus infection. Oral Oncol. 50, 364–369 (2014).
Palmer, E. et al. Human papillomavirus infection is rare in nonmalignant tonsil tissue in the UK: implications for tonsil cancer precursor lesions. Int. J. Cancer 135, 2437–2443 (2014).
Gillison, M. L. et al. Prevalence of oral HPV infection in the United States, 2009–2010. JAMA 307, 693–703 (2012).
International Collaboration of Epidemiological Studies of Cervical Cancer et al. Carcinoma of the cervix and tobacco smoking: collaborative reanalysis of individual data on 13,541 women with carcinoma of the cervix and 23,017 women without carcinoma of the cervix from 23 epidemiological studies. Int. J. Cancer 118, 1481–1495 (2006).
International Collaboration of Epidemiological Studies of Cervical Cancer. Cervical carcinoma and reproductive factors: collaborative reanalysis of individual data on 16,563 women with cervical carcinoma and 33,542 women without cervical carcinoma from 25 epidemiological studies. Int. J. Cancer 119, 1108–1124 (2006).
International Collaboration of Epidemiological Studies of Cervical Cancer et al. Cervical cancer and hormonal contraceptives: collaborative reanalysis of individual data for 16,573 women with cervical cancer and 35,509 women without cervical cancer from 24 epidemiological studies. Lancet 370, 1609–1621 (2007).
Safaeian, M. et al. Chlamydia trachomatis and risk of prevalent and incident cervical premalignancy in a population-based cohort. J. Natl Cancer Inst. 102, 1794–1804 (2010).
Smith, J. S. et al. Chlamydia trachomatis and invasive cervical cancer: a pooled analysis of the IARC multicentric case–control study. Int. J. Cancer 111, 431–439 (2004).
Gargano, J. W. et al. Age-group differences in human papillomavirus types and cofactors for cervical intraepithelial neoplasia 3 among women referred to colposcopy. Cancer Epidemiol. Biomarkers Prev. 21, 111–121 (2012).
Vaccarella, S., Lortet-Tieulent, J., Plummer, M., Franceschi, S. & Bray, F. Worldwide trends in cervical cancer incidence: impact of screening against changes in disease risk factors. Eur. J. Cancer 49, 3262–3273 (2013).
Peto, J., Gilham, C., Fletcher, O. & Matthews, F. E. The cervical cancer epidemic that screening has prevented in the UK. Lancet 364, 249–256 (2004).
Schiffman, M. & Rodríguez, A. C. Heterogeneity in CIN3 diagnosis. Lancet Oncol. 9, 404–406 (2008).
Plummer, M., Peto, J., Franceschi, S. & International Collaboration of Epidemiological Studies of Cervical Cancer. Time since first sexual intercourse and the risk of cervical cancer. Int. J. Cancer 130, 2638–2644 (2012).
Chung, S.-H., Franceschi, S. & Lambert, P. F. Estrogen and ERα: culprits in cervical cancer? Trends Endocrinol. Metab. 21, 504–511 (2010).
den Boon, J. A. et al. Molecular transitions from papillomavirus infection to cervical precancer and cancer: role of stromal estrogen receptor signaling. Proc. Natl Acad. Sci. USA 112, E3255–E3264 (2015).
Brake, T. & Lambert, P. F. Estrogen contributes to the onset, persistence, and malignant progression of cervical cancer in a human papillomavirus-transgenic mouse model. Proc. Natl Acad. Sci. USA 102, 2490–2495 (2005).
Spurgeon, M. E., Chung, S.-H. & Lambert, P. F. Recurrence of cervical cancer in mice after selective estrogen receptor modulator therapy. Am. J. Pathol. 184, 530–540 (2014).
Pai, S. I. & Westra, W. H. Molecular pathology of head and neck cancer: implications for diagnosis, prognosis, and treatment. Annu. Rev. Pathol. 4, 49–70 (2009).
Rietbergen, M. M. et al. No evidence for active human papillomavirus (HPV) in fields surrounding HPV-positive oropharyngeal tumors. J. Oral Pathol. Med. 43, 137–142 (2014).
Doorbar, J. et al. The biology and life-cycle of human papillomaviruses. Vaccine 30 (Suppl. 5), F55–F70 (2012). Expands on the basic aspects of HPV pathophysiology introduced in this Primer.
Buck, C. B. et al. Arrangement of L2 within the papillomavirus capsid. J. Virol. 82, 5190–5197 (2008).
Doorbar, J. Molecular biology of human papillomavirus infection and cervical cancer. Clin. Sci. (Lond.) 110, 525–541 (2006).
Bernard, H.-U. Regulatory elements in the viral genome. Virology 445, 197–204 (2013).
Schwartz, S. Papillomavirus transcripts and posttranscriptional regulation. Virology 445, 187–196 (2013).
Wise-Draper, T. M. & Wells, S. I. Papillomavirus E6 and E7 proteins and their cellular targets. Front. Biosci. 13, 1003–1017 (2008).
Doorbar, J. The papillomavirus life cycle. J. Clin. Virol. 32, S7–S15 (2005).
Cornall, A. M. et al. Anal and perianal squamous carcinomas and high-grade intraepithelial lesions exclusively associated with “low-risk” HPV genotypes 6 and 11. Int. J. Cancer 133, 2253–2258 (2013).
Pyeon, D., Pearce, S. M., Lank, S. M., Ahlquist, P. & Lambert, P. F. Establishment of human papillomavirus infection requires cell cycle progression. PLoS Pathog. 5, e1000318 (2009).
Doorbar, J. Latent papillomavirus infections and their regulation. Curr. Opin. Virol. 3, 416–421 (2013).
Egawa, N., Egawa, K., Griffin, H. & Doorbar, J. Human papillomaviruses; epithelial tropisms, and the development of neoplasia. Viruses 7, 3863–3890 (2015).
Cladel, N. M., Hu, J., Balogh, K., Mejia, A. & Christensen, N. D. Wounding prior to challenge substantially improves infectivity of cottontail rabbit papillomavirus and allows for standardization of infection. J. Virol. Methods 148, 34–39 (2008).
Valencia, C. et al. Human papillomavirus E6/E7 oncogenes promote mouse ear regeneration by increasing the rate of wound re-epithelization and epidermal growth. J. Invest. Dermatol. 128, 2894–2903 (2008).
Hoffmann, R., Hirt, B., Bechtold, V., Beard, P. & Raj, K. Different modes of human papillomavirus DNA replication during maintenance. J. Virol. 80, 4431–4439 (2006).
Egawa, N. et al. The E1 protein of human papillomavirus type 16 is dispensable for maintenance replication of the viral genome. J. Virol. 86, 3276–3283 (2012).
Zheng, Z.-M. & Baker, C. C. Papillomavirus genome structure, expression, and post-transcriptional regulation. Front. Biosci. 11, 2286–2302 (2006).
Bodily, J. M., Hennigan, C., Wrobel, G. A. & Rodriguez, C. M. Regulation of the human papillomavirus type 16 late promoter by E7 and the cell cycle. Virology 443, 11–19 (2013).
Isaacson Wechsler, E. et al. Reconstruction of human papillomavirus type 16-mediated early-stage neoplasia implicates E6/E7 deregulation and the loss of contact inhibition in neoplastic progression. J. Virol. 86, 6358–6364 (2012).
Vande Pol, S. B. & Klingelhutz, A. J. Papillomavirus E6 oncoproteins. Virology 445, 115–137 (2013).
Klingelhutz, A. J. & Roman, A. Cellular transformation by human papillomaviruses: lessons learned by comparing high- and low-risk viruses. Virology 424, 77–98 (2012).
Roman, A. & Munger, K. The papillomavirus E7 proteins. Virology 445, 138–168 (2013).
Ganti, K. et al. The human papillomavirus E6 PDZ binding motif: from life cycle to malignancy. Viruses 7, 3530–3551 (2015).
Duensing, A. et al. Centrosome overduplication, chromosomal instability, and human papillomavirus oncoproteins. Environ. Mol. Mutagen. 50, 741–747 (2009).
Wentzensen, N., Vinokurova, S. & von Knebel Doeberitz, M. Systematic review of genomic integration sites of human papillomavirus genomes in epithelial dysplasia and invasive cancer of the female lower genital tract. Cancer Res. 64, 3878–3884 (2004).
Vinokurova, S. et al. Type-dependent integration frequency of human papillomavirus genomes in cervical lesions. Cancer Res. 68, 307–313 (2008).
Warren, C. J. et al. APOBEC3A functions as a restriction factor of human papillomavirus. J. Virol. 89, 688–702 (2015).
Burgers, W. A. et al. Viral oncoproteins target the DNA methyltransferases. Oncogene 26, 1650–1655 (2007).
D'Costa, Z. J. et al. Transcriptional repression of E-cadherin by human papillomavirus type 16 E6. PLoS ONE 7, e48954 (2012).
Stanley, M. A. Epithelial cell responses to infection with human papillomavirus. Clin. Microbiol. Rev. 25, 215–222 (2012). Comprehensively describes the immune response to HPV infections.
Heaton, S. M., Borg, N. A. & Dixit, V. M. Ubiquitin in the activation and attenuation of innate antiviral immunity. J. Exp. Med. 213, 1–13 (2016).
Tummers, B. & Burg, S. H. High-risk human papillomavirus targets crossroads in immune signaling. Viruses 7, 2485–2506 (2015).
Habiger, C., Jäger, G., Walter, M., Iftner, T. & Stubenrauch, F. Interferon kappa inhibits human papillomavirus 31 transcription by inducing Sp100 proteins. J. Virol. 90, 694–704 (2016).
Fausch, S. C., Da Silva, D. M. & Kast, W. M. Heterologous papillomavirus virus-like particles and human papillomavirus virus-like particle immune complexes activate human Langerhans cells. Vaccine 23, 1720–1729 (2005).
Sperling, T. et al. Human papillomavirus type 8 interferes with a novel C/EBPβ-mediated mechanism of keratinocyte CCL20 chemokine expression and Langerhans cell migration. PLoS Pathog. 8, e1002833 (2012).
Matthews, K. et al. Depletion of Langerhans cells in human papillomavirus type 16-infected skin is associated with E6-mediated down regulation of E-cadherin. J. Virol. 77, 8378–8385 (2003).
Woo, Y. L. et al. Characterising the local immune responses in cervical intraepithelial neoplasia: a cross-sectional and longitudinal analysis. BJOG 115, 1616–1621; discussion 1621–1622 (2008).
van der Burg, S. H., de Jong, A., Welters, M. J. P., Offringa, R. & Melief, C. J. M. The status of HPV16-specific T-cell reactivity in health and disease as a guide to HPV vaccine development. Virus Res. 89, 275–284 (2002).
Visser, J. et al. Frequencies and role of regulatory T cells in patients with (pre)malignant cervical neoplasia. Clin. Exp. Immunol. 150, 199–209 (2007).
Trimble, C. L. et al. Human papillomavirus 16-associated cervical intraepithelial neoplasia in humans excludes CD8 T cells from dysplastic epithelium. J. Immunol. 185, 7107–7114 (2010).
Moore, R. A., Nicholls, P. K., Santos, E. B., Gough, G. W. & Stanley, M. A. Absence of canine oral papillomavirus DNA following prophylactic L1 particle-mediated immunotherapeutic delivery vaccination. J. Gen. Virol. 83, 2299–2301 (2002).
Maglennon, G. A., McIntosh, P. & Doorbar, J. Persistence of viral DNA in the epithelial basal layer suggests a model for papillomavirus latency following immune regression. Virology 414, 153–163 (2011).
Maglennon, G. A., McIntosh, P. B. & Doorbar, J. Immunosuppression facilitates the reactivation of latent papillomavirus infections. J. Virol. 88, 710–716 (2014).
Brotman, R. M. et al. Interplay between the temporal dynamics of the vaginal microbiota and human papillomavirus detection. J. Infect. Dis. 210, 1723–1733 (2014).
Hubert, P. et al. Altered α-defensin 5 expression in cervical squamocolumnar junction: implication in the formation of a viral/tumour-permissive microenvironment. J. Pathol. 234, 464–477 (2014).
Wiens, M. E. & Smith, J. G. Alpha-defensin HD5 inhibits furin cleavage of human papillomavirus 16 L2 to block infection. J. Virol. 89, 2866–2874 (2015).
Wira, C. R., Rodriguez-Garcia, M. & Patel, M. V. The role of sex hormones in immune protection of the female reproductive tract. Nat. Rev. Immunol. 15, 217–230 (2015).
Kovats, S. Estrogen receptors regulate innate immune cells and signaling pathways. Cell. Immunol. 294, 63–69 (2015).
Stanley, M., Pinto, L. A. & Trimble, C. Human papillomavirus vaccines — immune responses. Vaccine 30 (Suppl. 5), F83–F87 (2012).
Giannini, S. L. et al. Enhanced humoral and memory B cellular immunity using HPV16/18 L1 VLP vaccine formulated with the MPL/aluminium salt combination (AS04) compared to aluminium salt only. Vaccine 24, 5937–5949 (2006).
Einstein, M. H. et al. Comparison of the immunogenicity of the human papillomavirus (HPV)-16/18 vaccine and the HPV-6/11/16/18 vaccine for oncogenic non-vaccine types HPV-31 and HPV-45 in healthy women aged 18–45 years. Hum. Vaccin. 7, 1359–1373 (2011).
Giuliano, A. R. et al. Efficacy of quadrivalent HPV vaccine against HPV infection and disease in males. N. Engl. J. Med. 364, 401–411 (2011).
Joura, E. A. et al. A 9-valent HPV vaccine against infection and intraepithelial neoplasia in women. N. Engl. J. Med. 372, 711–723 (2015).
Castellsagué, X. et al. Immunogenicity and safety of the 9-valent HPV vaccine in men. Vaccine 33, 6892–6901 (2015).
[No authors listed.] Human papillomavirus vaccines: WHO position paper, October 2014. WHO Wkly Epidemiol. Rec. 89, 465–492 (2014).
Hanson, C. M., Eckert, L., Bloem, P. & Cernuschi, T. Gavi HPV programs: application to implementation. Vaccines 3, 408–419 (2015).
Palefsky, J. M. et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N. Engl. J. Med. 365, 1576–1585 (2011).
[No authors listed.] Meeting of the Strategic Advisory Group of Experts on immunization, April 2014 — conclusion and recommendations. WHO Wkly Epidemiol. Rec. 89, 221–236 (2014).
Dobson, S. R. et al. Immunogenicity of 2 doses of HPV vaccine in younger adolescents vs 3 doses in young women: a randomized clinical trial. JAMA 309, 1793–1802 (2013).
Romanowski, B. et al. Immunogenicity and safety of the HPV-16/18 AS04-adjuvanted vaccine administered as a 2-dose schedule compared with the licensed 3-dose schedule: results from a randomized study. Hum. Vaccin. 7, 1374–1386 (2011).
Castellsagué, X. et al. End-of-study safety, immunogenicity, and efficacy of quadrivalent HPV (types 6, 11, 16, 18) recombinant vaccine in adult women 24–45 years of age. Br. J. Cancer 105, 28–37 (2011).
Muñoz, N. et al. Impact of human papillomavirus (HPV)-6/11/16/18 vaccine on all HPV-associated genital diseases in young women. J. Natl Cancer Inst. 102, 325–339 (2010).
Lehtinen, M. et al. Overall efficacy of HPV-16/18 AS04-adjuvanted vaccine against grade 3 or greater cervical intraepithelial neoplasia: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 13, 89–99 (2012).
Schiller, J. T., Castellsagué, X. & Garland, S. M. A review of clinical trials of human papillomavirus prophylactic vaccines. Vaccine 30 (Suppl. 5), F123–F138 (2012).
Drolet, M. et al. Population-level impact and herd effects following human papillomavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect. Dis. 15, 565–580 (2015).
Garland, S. M. et al. Impact and effectiveness of the quadrivalent human papillomavirus vaccine: a systematic review of 10 years of real-world experience. Clin. Infect. Dis. 63, 519–527 (2016).
Giuliano, A. R. et al. Seroconversion following anal and genital HPV infection in men: the HIM study. Papillomavirus Res. 1, 109–115 (2015).
Scherpenisse, M. et al. Characteristics of HPV-specific antibody responses induced by infection and vaccination: cross-reactivity, neutralizing activity, avidity and IgG subclasses. PLoS ONE 8, e74797 (2013).
Wheeler, C. M. et al. Cross-protective efficacy of HPV-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by non-vaccine oncogenic HPV types: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 13, 100–110 (2012).
Elfström, K. M. et al. Long term duration of protective effect for HPV negative women: follow-up of primary HPV screening randomised controlled trial. BMJ 348, g130 (2014).
Kjaer, S. K. et al. A pooled analysis of continued prophylactic efficacy of quadrivalent human papillomavirus (types 6/11/16/18) vaccine against high-grade cervical and external genital lesions. Cancer Prev. Res. (Phila.) 2, 868–878 (2009).
International Agency for Research on Cancer. IARC handbooks of cancer prevention. Volume 10. Cervix cancer screening. IARChttp://www.iarc.fr/en/publications/pdfs-online/prev/handbook10/HANDBOOK10.pdf (2005).
Arbyn, M. et al. Evidence regarding human papillomavirus testing in secondary prevention of cervical cancer. Vaccine 30 (Suppl. 5), F88–F99 (2012).
Gage, J. C. et al. Reassurance against future risk of precancer and cancer conferred by a negative human papillomavirus test. J. Natl Cancer Inst. 106, dju153 (2014).
Huh, W. K. et al. Use of primary high-risk human papillomavirus testing for cervical cancer screening: interim clinical guidance. Gynecol. Oncol. 136, 178–182 (2015).
Health Council of the Netherlands. Population screening for cervical cancer. The Hague: Health Council of the Netherlands (No. 2011/07E). RIVMhttps://www.gezondheidsraad.nl/sites/default/files/201107E_PopulationSCC_0.pdf (2011).
Ronco, G. et al. Health technology assessment report: HPV DNA based primary screening for cervical cancer precursors. Epidemiol. Prev. 36, e1–e72 (in Italian) (2012).
Cuzick, J. et al. Comparing the performance of six human papillomavirus tests in a screening population. Br. J. Cancer 108, 908–913 (2013).
Wentzensen, N., Schiffman, M., Palmer, T. & Arbyn, M. Triage of HPV positive women in cervical cancer screening. J. Clin. Virol. 76, S49–S55 (2016).
Massad, L. S., Jeronimo, J., Schiffman, M. & National Institutes of Health/American Society for Colposcopy and Cervical Pathology (NIH/ASCCP) Research Group. Interobserver agreement in the assessment of components of colposcopic grading. Obstet. Gynecol. 111, 1279–1284 (2008).
Bergeron, C. et al. Informed cytology for triaging HPV-positive women: substudy nested in the NTCC randomized controlled trial. J. Natl Cancer Inst. 107, dju423 (2015).
Richardson, L. A. et al. HPV DNA testing with cytology triage in cervical cancer screening: influence of revealing HPV infection status. Cancer Cytopathol. 123, 745–754 (2015).
Wentzensen, N. et al. p16/Ki-67 dual stain cytology for detection of cervical precancer in HPV-positive women. J. Natl Cancer Inst. 107, djv257 (2015).
Schiffman, M. et al. Proof-of-principle study of a novel cervical screening and triage strategy: computer-analyzed cytology to decide which HPV-positive women are likely to have ≥CIN2. Int. J. Cancerhttp://dx.doi.org/10.1002/ijc.30456 (2016).
Ikenberg, H. et al. Screening for cervical cancer precursors with p16/Ki-67 dual-stained cytology: results of the PALMS study. J. Natl Cancer Inst. 105, 1550–1557 (2013).
Carozzi, F. et al. Risk of high-grade cervical intraepithelial neoplasia during follow-up in HPV-positive women according to baseline p16-INK4A results: a prospective analysis of a nested substudy of the NTCC randomised controlled trial. Lancet Oncol. 14, 168–176 (2013).
Cuzick, J. et al. Individual detection of 14 high risk human papilloma virus genotypes by the PapType test for the prediction of high grade cervical lesions. J. Clin. Virol. 60, 44–49 (2014).
Schiffman, M. et al. A study of genotyping for management of human papillomavirus-positive, cytology-negative cervical screening results. J. Clin. Microbiol. 53, 52–59 (2015).
De Strooper, L. M. A. et al. CADM1, MAL and miR124-2 methylation analysis in cervical scrapes to detect cervical and endometrial cancer. J. Clin. Pathol. 67, 1067–1071 (2014).
Vasiljevic´, N., Scibior-Bentkowska, D., Brentnall, A. R., Cuzick, J. & Lorincz, A. T. Credentialing of DNA methylation assays for human genes as diagnostic biomarkers of cervical intraepithelial neoplasia in high-risk HPV positive women. Gynecol. Oncol. 132, 709–714 (2014).
Mirabello, L. et al. Methylation of human papillomavirus type 16 genome and risk of cervical precancer in a Costa Rican population. J. Natl Cancer Inst. 104, 556–565 (2012).
Vasiljevic´, N., Scibior-Bentkowska, D., Brentnall, A. R., Cuzick, J. & Lorincz, A. A comparison of methylation levels in HPV18, HPV31 and HPV33 genomes reveals similar associations with cervical precancers. J. Clin. Virol. 59, 161–166 (2014).
Wentzensen, N. et al. Methylation of HPV18, HPV31, and HPV45 genomes and cervical intraepithelial neoplasia grade 3. J. Natl Cancer Inst. 104, 1738–1749 (2012).
Luhn, P. et al. Chromosomal gains measured in cytology samples from women with abnormal cervical cancer screening results. Gynecol. Oncol. 130, 595–600 (2013).
Zhao, F.-H. et al. An evaluation of novel, lower-cost molecular screening tests for human papillomavirus in rural China. Cancer Prev. Res. (Phila.) 6, 938–948 (2013).
van Baars, R. et al. Investigating diagnostic problems of CIN1 and CIN2 associated with high-risk HPV by combining the novel molecular biomarker panHPVE4 With P16INK4a. Am. J. Surg. Pathol. 39, 1518–1528 (2015).
Gage, J. C. et al. Number of cervical biopsies and sensitivity of colposcopy. Obstet. Gynecol. 108, 264–272 (2006).
Pretorius, R. G. et al. Colposcopically directed biopsy, random cervical biopsy, and endocervical curettage in the diagnosis of cervical intraepithelial neoplasia II or worse. Am. J. Obstet. Gynecol. 191, 430–434 (2004).
Wentzensen, N. et al. Multiple biopsies and detection of cervical cancer precursors at colposcopy. J. Clin. Oncol. 33, 83–89 (2015). Reports evidence for improved colposcopic biopsy practice.
Kelly, R. S., Walker, P., Kitchener, H. & Moss, S. M. Incidence of cervical intraepithelial neoplasia grade 2 or worse in colposcopy-negative/human papillomavirus-positive women with low-grade cytological abnormalities. BJOG 119, 20–25 (2012).
Massad, L. S., Jeronimo, J. & Katki, H. A., Schiffman, M. & National Institutes of Health/American Society for Colposcopy and Cervical Pathology Research Group. The accuracy of colposcopic grading for detection of high-grade cervical intraepithelial neoplasia. J. Low. Genit. Tract Dis. 13, 137–144 (2009).
Petry, K. U. et al. Evaluating HPV-negative CIN2+ in the ATHENA trial. Int. J. Cancer 138, 2932–2939 (2016).
Bornstein, J. et al. 2011 terminology of the vulva of the International Federation for Cervical Pathology and Colposcopy. J. Low. Genit. Tract Dis. 16, 290–295 (2012).
Dalla Pria, A. et al. High-resolution anoscopy screening of HIV-positive MSM: longitudinal results from a pilot study. AIDS 28, 861–867 (2014).
Nathan, M. et al. Performance of anal cytology in a clinical setting when measured against histology and high-resolution anoscopy findings. AIDS 24, 373–379 (2010).
Palefsky, J. M. Screening to prevent anal cancer: current thinking and future directions. Cancer Cytopathol. 123, 509–510 (2015).
Schiffman, M. & Wentzensen, N. A. Suggested approach to simplify and improve cervical screening in the United States. J. Low. Genit. Tract Dis. 20, 1–7 (2016). Defines an approach to unify the many different cervical screening options that are currently available.
McCredie, M. R. E. et al. Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: a retrospective cohort study. Lancet Oncol. 9, 425–434 (2008).
Castle, P. E., Schiffman, M., Wheeler, C. M. & Solomon, D. Evidence for frequent regression of cervical intraepithelial neoplasia-grade 2. Obstet. Gynecol. 113, 18–25 (2009).
Griffin, H. et al. Stratification of HPV-induced cervical pathology using the virally encoded molecular marker E4 in combination with p16 or MCM. Mod. Pathol. 28, 977–993 (2015).
Herfs, M. et al. A discrete population of squamocolumnar junction cells implicated in the pathogenesis of cervical cancer. Proc. Natl Acad. Sci. USA 109, 10516–10521 (2012).
Chow, E. P. F. et al. Quadrivalent vaccine-targeted human papillomavirus genotypes in heterosexual men after the Australian female human papillomavirus vaccination programme: a retrospective observational study. Lancet Infect. Dis. http://dx.doi.org/10.1016/S1473-3099(16)30116-5 (2016).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02328872 (2016).
Trimble, C. L. et al. Safety, efficacy, and immunogenicity of VGX-3100, a therapeutic synthetic DNA vaccine targeting human papillomavirus 16 and 18 E6 and E7 proteins for cervical intraepithelial neoplasia 2/3: a randomised, double-blind, placebo-controlled phase 2b trial. Lancet 386, 2078–2088 (2015).
Tewari, K. S. & Monk, B. J. New strategies in advanced cervical cancer: from angiogenesis blockade to immunotherapy. Clin. Cancer Res. 20, 5349–5358 (2014).
Tewari, K. S. et al. Improved survival with bevacizumab in advanced cervical cancer. N. Engl. J. Med. 370, 734–743 (2014).
Monk, B. J. & Tewari, K. S. Evidence-based therapy for recurrent cervical cancer. J. Clin. Oncol. 32, 2687–2690 (2014).
Burger, R. A. et al. Human papillomavirus type 18: association with poor prognosis in early stage cervical cancer. J. Natl Cancer Inst. 88, 1361–1368 (1996).
National Comprehensive Cancer Network. NCCN Guidelines®. NCCNhttps://www.nccn.org/professionals/physician_gls/f_guidelines.asp (accessed 1 Oct 2016) Provides the definitive current US guidelines for cervical, vulvar, anal, penile and oropharyngeal cancers.
Tsikouras, P. et al. Cervical cancer: screening, diagnosis and staging. J. BUON 21, 320–325 (2016).
Houlihan, O. A. & O'Neill, B. D. P. Chemoradiotherapy for anal squamous cell carcinoma. Surgeon 14, 202–212 (2016).
Monk, B. J., Tewari, K. S. & Koh, W.-J. Multimodality therapy for locally advanced cervical carcinoma: state of the art and future directions. J. Clin. Oncol. 25, 2952–2965 (2007).
Shridhar, R., Shibata, D., Chan, E. & Thomas, C. R. Anal cancer: current standards in care and recent changes in practice. CA Cancer J. Clin. 65, 139–162 (2015).
Pfister, D. G. et al. Head and neck cancers, version 2. 2014. Clinical practice guidelines in oncology. J. Natl Compr. Canc. Netw. 12, 1454–1487 (2014).
Fakhry, C. et al. Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J. Natl Cancer Inst. 100, 261–269 (2008).
Fakhry, C. et al. Human papillomavirus and overall survival after progression of oropharyngeal squamous cell carcinoma. J. Clin. Oncol. 32, 3365–3373 (2014).
Ang, K. K. et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N. Engl. J. Med. 363, 24–35 (2010).
Fakhry, C., Andersen, K. K., Eisele, D. W. & Gillison, M. L. Oropharyngeal cancer survivorship in Denmark, 1977–2012. Oral Oncol. 51, 982–984 (2015).
Patel, M. A. et al. Rising population of survivors of oral squamous cell cancer in the United States. Cancer 122, 1380–1387 (2016).
O'Rorke, M. A. et al. Human papillomavirus related head and neck cancer survival: a systematic review and meta-analysis. Oral Oncol. 48, 1191–1201 (2012).
Benson, E., Li, R., Eisele, D. & Fakhry, C. The clinical impact of HPV tumor status upon head and neck squamous cell carcinomas. Oral Oncol. 50, 565–574 (2014).
Kimple, R. J. et al. Enhanced radiation sensitivity in HPV-positive head and neck cancer. Cancer Res. 73, 4791–4800 (2013).
Agrawal, N. et al. Exome sequencing of head and neck squamous cell carcinoma reveals inactivating mutations in NOTCH1. Science 333, 1154–1157 (2011).
Ward, M. J. et al. Tumour-infiltrating lymphocytes predict for outcome in HPV-positive oropharyngeal cancer. Br. J. Cancer 110, 489–500 (2014).
Badoual, C. et al. PD-1-expressing tumor-infiltrating T cells are a favorable prognostic biomarker in HPV-associated head and neck cancer. Cancer Res. 73, 128–138 (2013).
Holsinger, F. C. & Ferris, R. L. Transoral endoscopic head and neck surgery and its role within the multidisciplinary treatment paradigm of oropharynx cancer: robotics, lasers, and clinical trials. J. Clin. Oncol. 33, 3285–3292 (2015).
Pfister, D. G. et al. Head and neck cancers, version 1. 2015. J. Natl Compr. Canc. Netw. 13, 847–855 (2015).
Giorgi Rossi, P. et al. Why follow-back studies should be interpreted cautiously: the case of an HPV-negative cervical lesion. Cancer Cytopathol. 124, 66–67 (2016).
Canfell, K. et al. Prevention of cervical cancer in rural China: evaluation of HPV vaccination and primary HPV screening strategies. Vaccine 29, 2487–2494 (2011).
Campos, N. G. et al. The comparative and cost-effectiveness of HPV-based cervical cancer screening algorithms in El Salvador. Int. J. Cancer 137, 893–902 (2015).
Burk, R. D., Chen, Z. & Van Doorslaer, K. Human papillomaviruses: genetic basis of carcinogenicity. Public Health Genomics 12, 281–290 (2009).
Bouvard, V. et al. A review of human carcinogens — part B: biological agents. Lancet Oncol. 10, 321–322 (2009).
Schiffman, M., Clifford, G. & Buonaguro, F. M. Classification of weakly carcinogenic human papillomavirus types: addressing the limits of epidemiology at the borderline. Infect. Agent. Cancer 4, 8 (2009).
Kovacic, M. B. et al. Relationships of human papillomavirus type, qualitative viral load, and age with cytologic abnormality. Cancer Res. 66, 10112–10119 (2006).
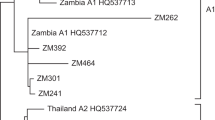
Mirabello, L. et al. HPV16 sublineage associations with histology-specific cancer risk using HPV whole-genome sequences in 3200 women. J. Natl Cancer Inst. 108, djw100 (2016). Reports on how whole-genome sequencing of the HPV genome will redefine our understanding of HPV epidemiology, natural history and carcinogenesis.
Darragh, T. M. et al. The Lower Anogenital Squamous Terminology Standardization project for HPV-associated lesions: background and consensus recommendations from the College of American Pathologists and the American Society for Colposcopy and Cervical Pathology. Int. J. Gynecol. Pathol. 32, 76–115 (2013).
Kreimer, A. R. et al. Efficacy of fewer than three doses of an HPV-16/18 AS04-adjuvanted vaccine: combined analysis of data from the Costa Rica vaccine and PATRICIA trials. Lancet Oncol. 16, 775–786 (2015).
Bosch, F. X. et al. HPV-FASTER: broadening the scope for prevention of HPV-related cancer. Nat. Rev. Clin. Oncol. 13, 119–132 (2016). Several prominent researchers advocate a vaccination and screening approach that could reduce HPV-related cancer incidence faster than current strategies.
Mustafa, R. A. et al. Systematic reviews and meta-analyses of the accuracy of HPV tests, visual inspection with acetic acid, cytology, and colposcopy. Int. J. Gynaecol. Obstet. 132, 259–265 (2016).
Fokom-Domgue, J. et al. Performance of alternative strategies for primary cervical cancer screening in sub-Saharan Africa: systematic review and meta-analysis of diagnostic test accuracy studies. BMJ 351, h3084 (2015).
Denny, L., Kuhn, L., Hu, C.-C., Tsai, W.-Y. & Wright, T. C. Human papillomavirus-based cervical cancer prevention: long-term results of a randomized screening trial. J. Natl Cancer Inst. 102, 1557–1567 (2010).
Valdez, M. et al. Effectiveness of novel, lower cost molecular human papillomavirus-based tests for cervical cancer screening in rural China. Int. J. Cancer 138, 1453–1461 (2016).
Cremer, M. et al. Adapting CryoPen, a non-gas based cryotherapy system for use in low- and middle-income countries. J. Glob. Oncol. 2, 11s−12s (2016).
Schiffman, M. & Wentzensen, N. Human papillomavirus infection and the multistage carcinogenesis of cervical cancer. Cancer Epidemiol. Biomarkers Prev. 22, 553–560 (2013).
Wellings, K. et al. Sexual behaviour in context: a global perspective. Lancet 368, 1706–1728 (2006).
Baussano, I., Lazzarato, F., Brisson, M. & Franceschi, S. Human papillomavirus vaccination at a time of changing sexual behavior. Emerg. Infect. Dis. 22, 18–23 (2016).
Gravitt, P. E. et al. Soil-transmitted helminth infections are associated with an increase in human papillomavirus prevalence and a T-helper type 2 cytokine signature in cervical fluids. J. Infect. Dis. 213, 723–730 (2016).
Clayton, E. et al. A single type of progenitor cell maintains normal epidermis. Nature 446, 185–189 (2007).
Martens, J. E., Arends, J., Van der Linden, P. J. Q., De Boer, B. A. G. & Helmerhorst, T. J. M. Cytokeratin 17 and p63 are markers of the HPV target cell, the cervical stem cell. Anticancer Res. 24, 771–775 (2004).
Reich, O., Pickel, H. & Regauer, S. Why do human papillomavirus infections induce sharply demarcated lesions of the cervix? J. Low. Genit. Tract Dis. 12, 8–10 (2008).
Herfs, M., Hubert, P., Moutschen, M. & Delvenne, P. Mucosal junctions: open doors to HPV and HIV infections? Trends Microbiol. 19, 114–120 (2011).
Santesso, N. et al. World Health Organization guidelines for treatment of cervical intraepithelial neoplasia 2–3 and screen-and-treat strategies to prevent cervical cancer. Int. J. Gynaecol. Obstet. 132, 252–258 (2016).
Acknowledgements
J.D. is supported by the UK Medical Research Council through programme grant MC_U117584278 (Molecular Biology of Human Papillomavirus Infection).
Author information
Authors and Affiliations
Contributions
Introduction (M.S.); Epidemiology (S.d.S., S.F., M.S. and N.W.); Mechanisms/pathophysiology (J.D. and M.A.S.); Diagnosis, screening and prevention (N.W., M.A.S., S.F. and M.S.); Management (B.J.M. and C.F.); Quality of life (M.S.); Outlook (all authors); Overview of the Primer (M.S.). All authors were involved in the editing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
M.A.S. has served as a consultant for Sanofi Pasteur MSD, GSK Biologicals and Merck Vaccines. S.d.S. has received institutional grants from Merck for research and educational projects and has conducted trials of vaccine products developed by Genticel and Merck. M.S. and N.W. have conducted US National Cancer Institute-led projects on HPV testing and cytology interpretations at reduced or no cost with BD Biosciences, Roche and Qiagen. J.D., C.F., B.J.M. and S.F. declare no competing interests.
Supplementary information
Rights and permissions
About this article
Cite this article
Schiffman, M., Doorbar, J., Wentzensen, N. et al. Carcinogenic human papillomavirus infection. Nat Rev Dis Primers 2, 16086 (2016). https://doi.org/10.1038/nrdp.2016.86
Published:
DOI: https://doi.org/10.1038/nrdp.2016.86
This article is cited by
-
Comparison of high-risk HPV detection by the AmpFire® HPV Screening 16/18/HR technique (Atila Biosystems) and the hybrid capture 2 test (Qiagen)
Molecular Biology Reports (2024)
-
Calcium-Activated Potassium Channel (KCNMA1) as Biomarker of Pre-Invasive and Invasive Cervical Cancer
Indian Journal of Gynecologic Oncology (2024)
-
Validation in Zambia of a cervical screening strategy including HPV genotyping and artificial intelligence (AI)-based automated visual evaluation
Infectious Agents and Cancer (2023)
-
Transcriptional activity of the long control region in human papillomavirus type 33 intratype variants
Virology Journal (2023)
-
Prevalence and genotype distribution of human papillomavirus infections in Beijing, China between 2016 and 2020
Virology Journal (2023)