Abstract
Cognitive deficits observed in schizophrenia are also frequently found in individuals with other schizophrenia spectrum disorders, such as schizotypal personality disorder (SPD). Dopamine appears to be a particularly important modulator of cognitive processes such as those impaired in schizophrenia spectrum disorders. In a double-blind, placebo-controlled clinical trial, we administered pergolide, a dopamine agonist targeting D1 and D2 receptors, to 25 participants with SPD and assessed the effect of pergolide treatment, as compared with placebo, on neuropsychological performance. We found that the pergolide group showed improvements in visual-spatial working memory, executive functioning, and verbal learning and memory. These results suggest that dopamine agonists may provide benefit for the cognitive abnormalities of schizophrenia spectrum disorders.
Similar content being viewed by others
INTRODUCTION
Impaired cognition is a core feature of schizophrenia (Green, 2006). Cognitive deficits, which are found in at least 75–85% of patients (Reichenberg et al, 2006), typically precede the onset of other symptoms (Sørensen et al, 2006) and persist after other symptoms have been effectively treated (Heinrichs, 2005). Cognitive deficits are the single best predictor of functional outcome in schizophrenia (Bozikas et al, 2006; Hofer et al, 2005; Milev et al, 2005). They predict poorer medication (Burton, 2005) and treatment (Prouteau et al, 2004) adherence, reduced adaptive and social skills (Bowie and Harvey, 2005), dysfunctional personality traits (Gurrera et al, 2005), and increased risk of relapse in first-episode patients (Chen et al, 2005). The cognitive dysfunction of schizophrenia appears to involve almost all the known neurotransmitter systems (Tamminga, 2006) and is also be found in probands’ non-schizophrenic relatives (Keefe et al, 1994; Sitskoorn et al, 2004).
Substantial research has implicated the dopaminergic system as a modulator of cognitive processes, particularly those subserved by the pre-frontal cortex (PFC), striatum, and associative structures (Cropley et al, 2006). A positive correlation between PFC D1 receptor alteration and cognitive impairments was initially reported in animal studies. Primate research has also consistently found that the natural aging process is associated with deterioration in the parameters of dopamine receptor signaling (Goldman-Rakic and Brown, 1981; Hemby et al, 2003; Naoi and Maruyama, 1999) and the emergence of impairments in working memory and executive functions (Volkow et al, 1998). Enhancement of working memory in aged monkeys is observed after D1 receptor signaling boost with D1 agonist treatment (Castner and Goldman-Rakic, 2004), and performance deficits in spatial working memory tasks can be pharmacologically reversed in DA-deficient monkeys and rats after dopamine D1 agonist administration (Arnsten et al, 1994; Castner et al, 2000; Castner and Goldman-Rakic, 2004). Furthermore, pharmacological modulation of working memory impairment through use of a D1 agonist in antipsychotic-treated monkeys shows lasting benefit 1 year later (Sawaguchi and Goldman-Rakic, 1991; Brozoski et al, 1979).
In humans, dopamine has been implicated in the cognitive dysfunction observed in a variety of neuropsychiatric disorders including Parkinson's disease (White, 1996; Owen and Robbins, 1998; Lange et al, 1992; Lewis et al, 2005), Huntington's disease, traumatic brain injury and stroke (McDowell, 1996), attention-deficit/hyperactivity disorder (Dinn et al, 2001; Shallice et al, 2002), and schizophrenia (Davis et al, 1991; Goldman-Rakic, 1999) and spectrum disorders (Trestman et al, 1995; Roitman et al, 2001). Therefore, pharmacological interventions targeting the dopamine system, and in particular D1 receptors, are a logical choice for treating the widespread cognitive dysfunction found in schizophrenia patients. However, there are several important challenges in examining the effect of dopamine modulation in this population, such as potential interactions with antipsychotic medication (Harvey and McClure, 2006).
Multiple cognitive abilities are impaired in people with schizotypal personality disorder (SPD), in a profile similar to that found in individuals with schizophrenia. Individuals with SPD show impairment as great as individuals with schizophrenia on tests using working memory (Heinrichs and Zakzanis, 1998; Mitropoulou et al, 2002, 2005). Impairments in episodic learning and memory are among the most widely replicated and pronounced cognitive deficits in schizophrenia (Saykin et al, 1991) and are also impaired in SPD in both verbal (Dickey et al, 2005) and visual-spatial modalities (McClure et al, 2007b). Thus, SPD patients show cognitive deficits that are similar to what is found in many individuals with schizophrenia, but these impairments are slightly reduced in severity and SPD patients are largely free from the potential confounds found in samples of schizophrenia patients.
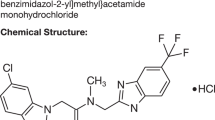
In this study, we sought to examine the effectiveness of pergolide, an agonist at both D1 and D2 receptors, for the treatment of cognitive abnormalities of individuals with SPD. Although pergolide is more potent at the D2 receptor, pergolide has a strong D1 receptor affinity and one of the most potent physiological effects at D1 receptor of the clinically available dopamine agonists (Gibbs and D’Esposito, 2006; Kimberg and D’Esposito, 2003; Müller et al, 1998). During the course of this study, concerns regarding the possibility of increased valvular heart disease in patients treated with ergot-derived dopamine agonists such as pergolide arose (Schade et al, 2007; Zanettini et al, 2007). Although none of the participants in this cohort had experienced any adverse effects from pergolide, because of these concerns we decided to suspend recruitment after enrolling 25 participants.
Pergolide has been shown to improve working memory in humans (Kimberg and D’Esposito, 2003), although it has not been previously administered to individuals in the schizophrenia spectrum. However, as we have previously found that the cognitive abnormalities of individuals with SPD were improved with pharmacological intervention (McClure et al, 2007a), we hypothesized pergolide would be an effective treatment for cognitive deficits observed within the schizophrenia spectrum. Specifically, we predicted that individuals with SPD who were treated with pergolide, compared with those treated with placebo, would show improved performance on neuropsychological tasks related to dopamine functioning, which includes a variety of measures of attention and working memory.
MATERIALS AND METHODS
Participants
We recruited male or female participants between the ages of 18 and 60 years from the outpatient clinics at the Mount Sinai Medical Center (New York, NY) and the James J Peters Veterans Affairs Medical Center (Bronx, NY). Participants were required to meet DSM-IV criteria for SPD while those who met current or lifetime DSM-IV criteria for schizophrenia or any schizophrenia-related psychotic disorder or for bipolar disorder were excluded. All participants were without abuse of illicit substances or alcohol within the past 6 months or a past history of substance dependence. All participants had been free of psychotropic medication for at least 2 weeks. All patients received a urine toxicology screen. See our previous publications for the full diagnostic assessment process. The study was approved by the institutional review boards of the Mount Sinai School of Medicine and the James J Peters Veterans Affairs Medical Center, and all participants signed a written informed consent statement after the study was explained to them.
Treatment Design
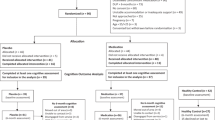
The placebo-controlled double-blind trial lasted for 4 weeks. Participants were randomized to receive either placebo or active drug and the dosage of pergolide was titrated upward in a stepwise design. The active drug group received 0.025 mg/day for the first 3 days, 0.05 mg/day for days 4 through 7, 0.1 mg/day for week 2, 0.2 mg/day for week 3, and 0.3 mg/day for week 4. The maximum dose was based on previous research (Müller et al, 1998) and pilot data indicating that a dose of 0.3 mg per day provided greater benefit than lower doses but was not enough to cause side effects in most participants. Participants were assessed at baseline and after 4 weeks of treatment.
Cognitive Assessments
DOT test
The DOT test is an assessment of visuospatial working memory in wide research use (Keefe et al, 1995, 1997). Subjects are presented a dot at a specific position on a standard size paper and then asked to reproduce it at the same location on a separate sheet after different periods of delay (no delay, 10, 20, or 30-s delay). The distance error at the 30-s delay minus the distance error at the immediate condition was the dependent variable of interest in this study.
Paced auditory serial addition test (PASAT)
The PASAT is a test of auditory verbal working memory that has been well described and validated in this population (Gronwall, 1977; Stuss et al, 1988). Briefly, subjects listen to a tape-recorded voice presenting a series of numbers (50 numbers at a rate of one digit per 2 s) and are asked to add each adjacent pair of numbers and respond by verbalizing the sum. The total number of correct responses is the dependent variable.
Wechsler memory scale visual reproduction test (WMS-VR)
The WMS-VR is a measure of memory for nonverbal stimuli (Wechsler, 1987). Four line drawings are presented one at a time for a 10-s exposure period. After the drawing is removed, the subject is asked to immediately draw the figure from memory. Participants are then asked to draw the four items from memory after a 30-min delay, with no prompts or cues provided. The raw score of the visual reproduction of the four figures after this delay is the dependent variable.
Word list learning (WLL)
The WLL test used in this study is an assessment of verbal learning and memory developed for use in clinical trials. Participants are presented with one of five matched lists of 25 words over five learning trials and are then presented with a distractor list. Participants are asked to recall the initial list immediately and after a 20-min delay. The total number of words recalled over the five learning trails and the number of words recalled at the 20-min delay interval were the dependent variables.
N-back working memory task (N-back)
The N-back is a commonly used measure of working memory (Braver et al, 1997; Casey et al, 1995) that has been frequently shown to elicit performance deficits among individuals with schizophrenia and their unaffected relatives (Barch et al, 2002; Braver et al, 1997). Participants observed letters presented on a computer screen one at a time over three conditions: (1) 0-back, (2) 1-back, and (3) 2-back. In the 0-back condition, participants responded to a single pre-specified target letter (eg, X). In the 1-back condition, the target was any letter identical to the one immediately preceding it (ie, one trial back). In the 2-back condition, the target was any letter identical to the one presented two trials back. For this study, the dependent variable was the number of correct responses for the 2-back condition.
Letter-number span (LNS)
This test requires subjects to listen to a list of intermingled letters and numbers. At the end of the presentation of the stimuli, subjects are asked to reproduce the information with the numbers in ascending order and the letters in alphabetical order, with numbers coming first. The number of correct trials served as the dependent variable.
Trail-making test (TMT)
TMT has two conditions that combine to assess verbal/spatial perception and psychomotor speed (Reitan and Wolfson, 1993). In Part A, the subject must connect numbers presented on a standard sheet of paper in ascending order (1–2–3). In Part B, the subject must alternate connecting numbers and letters (eg, 1-A, 2-B, 3-C, and so on). The amount of time to complete Part A and Part B were the two dependent variables.
AX-CPT task
Participants performed three conditions of the AX-CPT: standard, degraded, and interference. Sequences of letters were visually presented one at a time in a continuous manner on a computer display. Participants were instructed to make an affirmative response on target trials and a negative response otherwise (for a full description, please see Barch et al, 2004). The delay between cue and probe was manipulated, so that half of the trials had a short delay and half had a long delay. On short-delay trials, the cue-probe interval was 1 s, and the inter-trial interval was 4900 ms. On long-delay trials, the cue-probe interval was 5 s and the inter-trial interval was 1 s. Thus, the total trial duration was equivalent across conditions, providing a means of controlling for general factors that might affect performance (eg, pace of the task, response frequency, and total time on task). The task was presented in four blocks of 50 trials, all of which were either short- (two blocks) or long- (two blocks) delay trials, with the order of short- and long-delay blocks counterbalanced across subjects. Participants were asked to respond as quickly as possible to each stimulus while maintaining accuracy. For this study, we used the interference version of the AX-CPT, during which an interference stimulus is presented between the cue and the probe, thereby increasing the difficulty of the task. The critical dependent variables used in this study were BX errors after a short-delay interval and AY errors after a long-delay interval.
Data Analysis
We calculated difference scores (post-treatment minus baseline scores) for each of our neuropsychological measures and computed a multivariate analysis of variance with these difference scores serving as the dependent variables (WLL results were excluded from this analysis because of a large amount of missing data for this test). We then computed a series of one-way ANOVAs comparing the pergolide and placebo groups, with each of these difference scores serving as the dependent variables for the two-group comparison. To control for baseline levels of impairment, we entered the participants’ baseline scores into each model as a covariate. In addition, a Sidak correction for multiple comparisons was carried out for all ANOVAs.
RESULTS
In total, we enrolled 25 participants. One participant discontinued participation in the study after week 2, leaving 12 participants randomized to pergolide and 12 randomized to placebo. The groups were comparable on age, t(22)=0.334, p=0.74, and education, t(22)=0.694, p=0.50, and all participants were right-handed (See Table 1 for demographic characteristics). There was a significant difference in the gender composition of the groups, χ2 (1)=5.04, p<0.05, as there were fewer females in the placebo group; however, when groups were collapsed and the baseline performance of male participants was compared with that of female participants, there were no significant differences on any of our assessments. In addition, all but two participants, one from each group, were naïve to antipsychotic medication; one of these participants had taken stelazine for a few years beginning in 1972 and the other had taken imipramine and thorazine during a brief hospitalization several years before enrollment in the study.
Raw scores on our measures are presented in Table 2. Overall, the results of our MANOVA were statistically significant, F(1, 9)=14.63, p=0.006, suggesting that there was a difference between the groups after treatment with either pergolide or placebo. Furthermore, we found that individuals with SPD treated with pergolide showed statistically significant improvement, compared with those in the placebo group, on several tasks that are hypothesized to be related to the activity of dopamine (See Table 2). Specifically, verbal learning and memory improved with pergolide compared with placebo for both the immediate and delayed recall intervals of the WLL test. Furthermore, when compared with the placebo group, the pergolide group showed improvement on the verbal working memory as measured by LNS performance. The pergolide group also showed improvement on the TMT Part B, a measure of executive functioning, when compared with the placebo group. In addition, individuals treated with pergolide, compared with those given placebo, showed significant improvement in long-term visual-spatial memory, as measured by the WMS-VR delayed recall score. Individuals treated with pergolide also showed a significant improvement in visual-spatial working memory, as measured by the DOT test, although this was largely driven by a worsening in performance of individuals in the placebo group not observed in individuals in the pergolide group.
Results for our modified version of the AX-CPT were somewhat mixed. Contrary to our hypotheses, we did not observe a statistically significant difference between the pergolide group and the placebo group for AY errors after a long delay. Although there was a statistically significant difference between groups for BX errors after a short delay, these results should be interpreted with caution. Our pergolide group showed the expected decrease in BX errors after treatment; however, the placebo group, which had an unusually high number of BX errors at baseline, also showed a decrease in these types of errors. Thus, we cannot determine whether the effect of pergolide on the BX error frequency also reflected some tendencies of regression to the mean such as was observed in the placebo group.
To evaluate whether the results were influenced by the number of statistical tests performed, we re-ran the ANOVAs using a Sidak correction for multiple comparisons; using this correction, only LNS, WLL Delay, and Trails B remain significant. Thus, although there were a number of influences of pergolide on cognition, the corrected results indicate that three cognitive domains were beneficially affected.
DISCUSSION
This study was an examination of the effectiveness of pergolide for the treatment of cognitive deficits of individuals with SPD, a schizophrenia spectrum illness. A significant body of evidence suggests that the neurotransmitter dopamine has an important role in many cognitive functions. D1 receptors in particular appear to be related to both healthy cognitive functioning and cognitive abnormalities observed in many psychiatric illnesses such as schizophrenia. At this time, there are no selective D1 agonists available for use in humans. However, although pergolide primarily targets D2 receptors, it has a very high D1 receptor affinity.
As we predicted, SPD participants treated with pergolide showed an improved performance on a number of neuropsychological assessments, even after correction for multiple comparisons. In particular, processing speed, executive function/working memory, and verbal learning and memory improved after 4 weeks of pergolide treatment. In addition, participants treated with pergolide performed significantly better on one of our measures of verbal working memory and one of our measures of visual-spatial working memory. It should be noted, however, that although there was a significant difference between groups for our measure of visual-spatial long-term memory, there was a very small effect size for this difference. Although analyses of two other measures of working memory were not statistically significant, in both cases examination of mean scores suggests that there was an improvement for the pergolide group. There was evidence of some practice effects in the placebo group, but the parallel nature of this design means that greater improvements in patients randomized to pergolide could not be attributed solely to practice. Pergolide did not improve performance on a measure of processing speed, meaning that the other findings are not likely because of a stimulant-like effect of pergolide. The small sample size is a limitation of the design, but robust improvements in cognitive functioning in several domains were detected despite the small size of the study.
We also failed to observe an improvement in the context processing of individuals treated with pergolide, compared with those treated with placebo. In the past, we have found that AX-CPT performance of individuals with SPD was amenable to pharmacological intervention with guanfacine (McClure et al, 2007a). This is a small-scale study and the results must be viewed accordingly, which may mean that the baseline scores were unstable because of the small sample size. The effect of other dopamine agonists on context processing is an area that has been studied previously (Barch and Carter, 2005), and other dopaminergic agents merit investigation in this area as well.
Although this study was in progress, concerns were raised regarding the possibility of increased valvular heart disease in patients treated with ergot-derived dopamine agonists such as pergolide (Zanettini et al, 2007; Schade et al, 2007), which caused us to suspend recruitment after only 25 participants had been enrolled. Although pergolide has subsequently been removed from the market, the results of our study are promising and suggest that dopamine agonists that specifically target D1 receptors are in fact effective in ameliorating cognitive deficits such as those observed in SPD and schizophrenia. As cognitive abnormalities are closely linked to the functional outcomes of this population, the results are important for furthering the recovery of individuals with schizophrenia spectrum illnesses. Identifying a safe D1 agonist for use in human samples, therefore, is an avenue of future research that is vital for promoting recovery.
References
Arnsten AFT, Cai JX, Murphy BL, Goldman-Rakic PS (1994). Dopamine D1 receptor mechanisms in the cognitive performance of young adult and aged monkeys. Psychopharmacology 116: 143–151.
Barch DM, Carter CS (2005). Amphetamine improves cognitive function in medicated individuals with schizophrenia and in healthy volunteers. Schizophr Res 77: 43–58.
Barch DM, Csermansky J, Conturo T, Snyder AZ (2002). Working and long-term memory deficits in schizophrenia. Is there a common underlying prefrontal mechanism? J Abnorm Psychol 111: 478–494.
Barch DM, Mitropoulou V, Harvey PD, New AS, Silverman JM, Siever LJ (2004). Context processing deficits in schizotypal personality disorder. J Abnorm Psychol 113: 556–568.
Bowie CR, Harvey PD (2005). Cognition in schizophrenia: impairments, determinants, and functional importance. Psychiatr Clin North Am 28: 613–633.
Bozikas VP, Kosmidis MH, Kafantari A, Gamvrula K, Vasiliadou E, Petrikis P et al (2006). Community dysfunction in schizophrenia: rate-limiting factors. Prog Neuropsychopharmacol Biol Psychiatry 30: 463–470.
Braver TS, Cohen JD, Nystrom LE, Jonides J, Smith EE, Noll DC (1997). A parametric study of prefrontal cortex involvement in human working memory. Neuroimage 5: 49–62.
Brozoski TJ, Brown RM, Rosvold HE, Goldman PS (1979). Cognitive deficit caused by regional depletion of dopamine in prefrontal cortex of rhesus monkey. Science 205: 929–932.
Burton SC (2005). Strategies for improving adherence to second-generation antipsychotics in patients with schizophrenia by increasing ease of use. J Psychiatr Prac 11: 369–378.
Casey BJ, Cohen JD, Jezzard P, Turner R, Noll DC, Trainor RJ et al (1995). Activation of prefrontal cortex in children during a non-spatial working memory task with functional MRI. Neuroimage 2: 221–229.
Castner SA, Goldman-Rakic PS (2004). Enhancement of working memory in aged monkeys by a sensitizing regimen of dopamine D1 receptor stimulation. J Neurosci 24: 1446–1450.
Castner SA, Graham V, Goldman-Rakic PS (2000). Reversal of anitpsychotic-induced working memory deficits by short-term dopamine D1 receptor stimulation. Science 287: 2020–2022.
Chen EY, Hui CL, Dunn EL, Miao MY, Yeung WS, Wong CK et al (2005). A prospective 3-year longitudinal study of cognitive predictors of relapse in first-episode schizophrenia patients. Schizophr Res 77: 99–104.
Cropley VL, Fujita M, Innis RB, Nathan PJ (2006). Molecular imaging of the dopaminergic system and its association with human cognitive function. Biol Psychiatry 15: 898–907.
Davis KL, Kahn RS, Ko G, Davidson M (1991). Dopamine and schizophrenia: a reconceptualization. Am J Psychiatry 148: 1474–1486.
Dickey CC, McCarley RW, Niznikiewicz MA, Voglmaier MM, Seidman LJ, Kim S et al (2005). Clinical, cognitive, and social characteristics of a sample of neuroleptic-naive persons with schizotypal personality disorder. Schizophr Res 78: 297–308.
Dinn WM, Robbins NC, Harris CL (2001). Adult attention-deficit/hyperactivity disorder: neuropsychological correlates and clinical presentation. Brain Cogn 46: 114–121.
Gibbs SE, D’Esposito M (2006). A functional magnetic resonance imaging study of the effects of pergolide, a dopamine receptor agonist, on component processes of working memory. Neuroscience 139: 359–371.
Goldman-Rakic PS, Brown RM (1981). Regional changes of monoamines in cerebral cortex and subcortical structures of aging rhesus monkeys. Neuroscience 6: 177–187.
Goldman-Rakic PS (1999). The physiological approach: function architecture of working memory and disordered cognition in schizophrenia. Biol Psychiatry 46: 650–661.
Green MF (2006). Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatr 67: 3–8.
Gronwall DMA (1977). Paced auditory serial-addition task: a measure of recovery from concussion. Percept Motor Skills 44: 367–373.
Gurrera RJ, Nestor PG, O’Donnell BF, Rosenberg V, McCarley RW (2005). Personality differences in schizophrenia are related to performance on neuropsychological tasks. J Nerv Ment Dis 193: 714–721.
Harvey PD, McClure MM (2006). Pharmacological approaches to the management of cognitive dysfunction in schizophrenia. Drugs 66: 1465–1473.
Heinrichs RW, Zakzanis KK (1998). Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology 12: 426–445.
Heinrichs RW (2005). The primacy of cognition in schizophrenia. Am Psychol 60: 229–242.
Hemby SE, Trojanowski JQ, Ginsberg SD (2003). Neuron-specific age-related decreases in dopamine receptor subtype mRNAs. J Comp Neurol 456: 176–183.
Hofer A, Baumgartner S, Bodner T, Edlinger M, Hummer M, Kemmler G et al (2005). Patient outcomes in schizophrenia II: the impact of cognition. Eur Psychiatry 20: 395–402.
Keefe RS, Lees-Roitman SE, Dupre RL (1997). Performance of patients with schizophrenia on a pen and paper visuospatial working memory task with short delay. Schizophr Res 26: 9–14.
Keefe RS, Roitman SE, Harvey PD, Blum C, DuPre R, Davidson M et al (1995). A pen and paper human analogue of a monkey prefrontal cortex activation task: spatial working memory in patients with schizophrenia. Schizophr Res 17: 25–33.
Keefe RS, Silverman JM, Roitman SE, Harvey PD, Duncan MA, Alroy D et al (1994). Performance of nonpsychotic relatives of schizophrenic patients on cognitive tests. Psychiatry Res 53: 1–12.
Kimberg DY, D’Esposito M (2003). Cognitive effects of the dopamine receptor agonist pergolide. Neuropsychologia 41: 1020–1027.
Lange KW, Robbins TW, Marsden CD, James M, Owen AM, Paul GM (1992). L-dopa withdrawal in Parkinson's disease selectively impairs cognitive performance in tests sensitive to frontal lobe dysfunction. Psychophamocology 107: 394–404.
Lewis SJ, Slabosz A, Robbins TW, Barker RA, Owen AM (2005). Dopaminergic basis for deficits in working memory but not attentional set-shifting in Parkinson's disease. Neuropsychologia 43: 823–832.
McClure MM, Barch DM, Romero MJ, Minzenberg MJ, Triebwasser J, Harvey PD et al (2007a). The effects of guanfacine on context processing abnormalities in schizotypal personality disorder. Biol Psychiatry 15: 1157–1160.
McClure MM, Romero MJ, Bowie CR, Reichenberg A, Harvey PD, Siever LJ (2007b). Visual-spatial learning and memory in schizotypal personality disorder: continued evidence for the importance of working memory in the schizophrenia spectrum. Arch Clin Neuropsychol 22: 109–116.
McDowell SK (1996). A role for dopamine in executive function deficits. J Head Trauma Rehabil 11: 89–92.
Milev P, Ho BC, Arndt S, Andreasen NC (2005). Predictive values of neurocognition and negative symptoms on functional outcome in schizophrenia: a longitudinal first-episode study with 7-year follow-up. Am J Psychiatry 162: 495–506.
Mitropoulou V, Harvey PD, Maldari LA, Moriarty PJ, New AS, Silverman JM et al (2002). Neuropsychological performance in schizotypal personality disorder: evidence regarding diagnostic specificity. Biol Psychiatry 52: 1175–1182.
Mitropoulou V, Harvey PD, Zegarelli G, New AS, Silverman JM, Siever LJ (2005). Neuropsychological performance in schizotypal personality disorder: importance of working memory. Am J Psychiatry 162: 1896–1903.
Müller U, von Cramon DY, Pollmann S (1998). D1- versus D2-receptor modulation of visuospatial working memory in humans. J Neurosci 18: 2720–2728.
Naoi M, Maruyama W (1999). Cell death of dopamine neurons in aging and Parkinson's disease. Mech Ageing Dev 111: 175–188.
Owen AM, Robbins TW (1998). Attention and working memory in movements disorders. In: Jahanashi M, Brown R (eds). Neuropsychology of Movement Disorders. Amsterdam, North-Holland.
Prouteau A, Verdoux H, Briand C, Lesage A, Lalonde P, Nicole L et al (2004). Cognitive predictors of psychosocial functioning outcome in schizophrenia: a follow-up study of subjects participations in a rehabilitation program. Schizophr Res 77: 343–353.
Reichenberg A, Weiser M, Caspi A, Knobler HY, Lubin G, Harvey PD et al (2006). Premorbid intellectual functioning and risk of schizophrenia and spectrum disorders. J Clin Exp Neuropsychol 28: 193–207.
Reitan RM, Wolfson D (1993). The Halstead-Reitan Neuropsychological Test Battery: Theory and Clinical Interpretation, 2nd edn. Neuropsychological Press: Tucson, AZ.
Roitman SE, Mitropoulou V, Keefe RS, Silverman JM, Serby M, Harvey PD et al (2001). Visuospatial working memory in schizotypal personality disorder patients. Schizophr Res 41: 447–455.
Sawaguchi T, Goldman-Rakic PS (1991). D1 dopamine receptors in prefrontal cortex involvement in working memory. Science 251: 947–950.
Saykin AJ, Gur RC, Gur RE, Mozley PD, Mozley LH, Resnick SM et al (1991). Neuropsychological function in schizophrenia: specific deficit in learning and memory. Arch Gen Psychiatry 48: 618–623.
Schade R, Andersohn F, Suissa S, Haverkamp W, Garbe E (2007). Dopamine agonists and the risk of cardiac-valve regurgitation. N Engl J Med 356: 29–38.
Shallice T, Marzocchi GM, Coser S, Del Savio M, Meuter RF, Rumiati RI (2002). Executive function profile of children with attention deficit hyperactivity disorder. Dev Neuropsychol 21: 43–71.
Sitskoorn MM, Aleman A, Ebisch SJ, Appels MC, Kahn RS (2004). Cognitive deficits in relatives of patients with schizophrenia: a meta-analysis. Schizophr Res 71: 285–295.
Sørensen HJ, Mortensen EL, Parnas J, Mednick SA (2006). Premorbid neurocognitive functioning in schizophrenia spectrum disorder. Schizophr Bull 32: 578–583.
Stuss DT, Stethem LL, Pelchat G (1988). Three tests of attention and rapid information processing: an extension. Clin Neuropsychol 2: 246–250.
Tamminga CA (2006). The neurobiology of cognition in schizophrenia. J Clin Psychiatry 67 (Suppl 9): 9–13; discussion 36–42.
Trestman RL, Keefe RSE, Mitropoulou V, Harvey PD, deVegvar ML, Lees-Roitment S et al (1995). Cognitive function and biological correlates of cognitive performance in schizotypal personality disorder. Psychiatry Res 59: 127–136.
Volkow ND, Gur RC, Wang GJ, Fowler JS, Moberg PJ, Ding YS et al (1998). Association between decline in brain dopamine activity with age and cognitive and motor impairment in healthy individuals. Am J Psychiatry 155: 344–349.
Wechsler D (1987). The Wechsler Memory Scale—Revised. The Psychological Corporation: San Antonio, TX.
White F (1996). Synaptic regulation of mesocorticolimbic dopamine neurons. Annu Rev Neurosci 19: 405–436.
Zanettini R, Antonini A, Gatto G, Gentile R, Tesei S, Pezzoli G (2007). Valvular heart disease and the use of dopamine agonists for Parkinson's disease. N Engl J Med 356: 39–46.
Acknowledgements
This work was supported by a Veterans Affairs Merit Review Grant (7609-028) to Dr Larry J Siever and by the Veterans Affairs VISN3 Mental Illness Research, Education, and Clinical Center. This work was also supported in part by Grant Number MO1-RR-00071 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCRR or NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
In the last 3 years Dr Harvey has served as a consultant for: Eli Lilly and Company, Johnson and Johnson, Pfizer, Solvay-Wyeth, The Sanofi-Aventis Group, Neurogen, and Daimippon Sumitomo America. Dr Harvey has grant support from Astra-Zeneca Pharmaceuticals. Dr Koenigsberg had grant support from Janssen Pharmaceuticals. The remaining authors declare that, except for income received from their primary employers, no financial support or compensation has been received from any individual or corporate entity over the past 3 years for research or professional service and there are no personal financial holdings that could be perceived as constituting a potential conflict of interest.
Rights and permissions
About this article
Cite this article
McClure, M., Harvey, P., Goodman, M. et al. Pergolide Treatment of Cognitive Deficits Associated with Schizotypal Personality Disorder: Continued Evidence of the Importance of the Dopamine System in the Schizophrenia Spectrum. Neuropsychopharmacol 35, 1356–1362 (2010). https://doi.org/10.1038/npp.2010.5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2010.5
Keywords
This article is cited by
-
Diagnosis and treatment of schizotypal personality disorder: evidence from a systematic review
npj Schizophrenia (2018)
-
Effects of the D1 Dopamine Receptor Agonist Dihydrexidine (DAR-0100A) on Working Memory in Schizotypal Personality Disorder
Neuropsychopharmacology (2015)
-
Schizotypal Personality Disorder: A Current Review
Current Psychiatry Reports (2014)
-
Prefrontal dopamine D1 receptors and working memory in schizotypal personality disorder: a PET study with [11C]NNC112
Psychopharmacology (2014)
-
Inhibition of phosphodiesterase 10A has differential effects on dopamine D1 and D2 receptor modulation of sensorimotor gating
Psychopharmacology (2014)