Abstract
Nicotine is considered an important component of tobacco responsible for the smoking habit in humans. Nicotine increases glutamate-mediated transmission throughout brain reward circuitries. This action of nicotine could potentially contribute to its intrinsic rewarding and reward-enhancing properties, which motivate consumption of the drug. Here we show that the competitive N-methyl-D-aspartate (NMDA) receptor antagonist LY235959 (0.5–2.5 mg per kg) abolished nicotine-enhanced brain reward function, reflected in blockade of the lowering of intracranial self-stimulation (ICSS) thresholds usually observed after experimenter-administered (0.25 mg per kg) or intravenously self-administered (0.03 mg per kg per infusion) nicotine injections. The highest LY235959 dose (5 mg per kg) tested reversed the hedonic valence of nicotine from positive to negative, reflected in nicotine-induced elevations of ICSS thresholds. LY235959 doses that reversed nicotine-induced lowering of ICSS thresholds also markedly decreased nicotine self-administration without altering responding for food reinforcement, whereas the α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid receptor antagonist NBQX had no effects on nicotine intake. In addition, nicotine self-administration upregulated NMDA receptor subunit expression in the central nucleus of the amygdala (CeA) and ventral tegmental area (VTA), suggesting important interactions between nicotine and the NMDA receptor. Furthermore, nicotine (1 μM) increased NMDA receptor-mediated excitatory postsynaptic currents in rat CeA slices, similar to its previously described effects in the VTA. Finally, infusion of LY235959 (0.1–10 ng per side) into the CeA or VTA decreased nicotine self-administration. Taken together, these data suggest that NMDA receptors, including those in the CeA and VTA, gate the magnitude and valence of the effects of nicotine on brain reward systems, thereby regulating motivation to consume the drug.
Similar content being viewed by others
INTRODUCTION
Nicotine amplifies reward signals in the brain, an effect common with other drugs of abuse (Rice and Cragg, 2004). This action of nicotine may partly account for its intrinsic rewarding properties, and also may explain how nicotine increases sensitivity to nondrug-related rewarding environmental stimuli (Kenny, 2007). Consistent with an excitatory action of nicotine on reward circuitries, intravenously self-administered and experimenter-administered bolus nicotine injections lower intracranial self-stimulation (ICSS) thresholds in rats (Huston-Lyons and Kornetsky, 1992; Bauco and Wise, 1994; Harrison et al, 2002; Kenny and Markou, 2006), reflecting nicotine-induced increases in brain-stimulation reward. Importantly, rats may regulate their pattern of intravenous nicotine self-administration at a level that achieves maximal nicotine-induced increased sensitivity of brain reward pathways, potentially reflected in lowered ICSS thresholds (Kenny and Markou, 2006). Thus, obtaining the rewarding and reward-enhancing effects of nicotine (actions that likely share common neurobiological mechanisms) may represent crucial sources of reinforcement that motivate nicotine consumption and contributes to the addictive properties of this drug (Donny et al, 2003; Kenny, 2007). Therefore, an improved understanding of the mechanisms by which nicotine amplifies brain reward function, reflected in lowered ICSS thresholds, may provide important insights into the persistence of the tobacco-smoking habit in human smokers.
To date, many investigations into neurocircuitries that regulate the motivation to consume nicotine have focused on the mesoaccumbens dopamine system, which comprises dopamine-containing neurons arising in the ventral tegmental area (VTA) and projecting to the nucleus accumbens (NAcc). Lesions of dopamine neurons in the VTA (Corrigall et al, 1992), or infusion of nicotinic acetylcholine receptor (nAChR) antagonists into the VTA (Corrigall et al, 1994), decreased nicotine self-administration in rats. Mice and rats self-administer nicotine directly into the VTA in a manner sensitive to nAChR and dopamine receptor blockade (David et al, 2006; Ikemoto et al, 2006). Furthermore, lentiviral-mediated reexpression of β2 nAChR subunits in the VTA of β2 nAChR subunit knockout mice reestablished nicotine self-administration and nicotine-evoked accumbal dopamine release that was otherwise absent in these mutant mice (Maskos et al, 2005). Thus, mesoaccumbens dopamine transmission is important in nicotine reinforcement. Nicotine enhances midbrain dopamine transmission, at least in part, by increasing excitatory glutamate-mediated input to the VTA (Fu et al, 2000; Grillner and Svensson, 2000; Mansvelder and McGehee, 2000), which in turn activates N-methyl-D-aspartate (NMDA) and α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA) receptors located on VTA dopamine neurons. Consistent with this action of nicotine, blockade of NMDA receptors, particularly those in the VTA, decreases nicotine-enhanced dopamine release in the NAcc (Schilstrom et al, 1998; Fu et al, 2000). In addition, NMDA receptor blockade attenuated the conditioned rewarding effects of VTA-administered nicotine injections, as measured in a place-conditioning procedure in rats (Laviolette and van der Kooy, 2003). These data support a role for NMDA receptors in nicotine reward. Nevertheless, relatively little is known concerning the role of NMDA receptors in regulating nicotine-induced amplification of brain reward function, and nicotine self-administration.
In addition to its effects in the VTA, nicotine increases glutamate-mediated transmission throughout cortical and limbic brain regions such as the hypothalamus (Hatton and Yang, 2002) and prefrontal cortex (PFC; Lambe et al, 2003), regions that serve as important anatomical substrates for the reinforcing actions of other drugs of abuse. Moreover, c-fos and extracellular signal-regulated kinase expression patterns (both molecular indicators of neuronal activation) suggest that nicotine increases the activity of reward-related brain regions in rats, including the NAcc, PFC, and central nucleus of the amygdala (CeA; Pagliusi et al, 1996; Pich et al, 1997; Brunzell et al, 2003; Valjent et al, 2004). Thus, NMDA receptors located in extra-mesoaccumbens brain regions also may regulate nicotine reinforcement processes.
Here, we investigated the role of NMDA receptors in regulating nicotine-enhanced brain reward function, and in regulating nicotine consumption. Specifically, we examined the effects of the competitive NMDA receptor antagonist LY235959 (see Schoepp et al, 1991; Ornstein et al, 1993; Fischer and Dykstra, 2006) on the ability of nicotine to lower ICSS thresholds, and on intravenous nicotine self-administration behavior. Next, we sought to identify the brain regions within which NMDA receptors regulate nicotine reinforcement. First, we assessed the effects of nicotine self-administration on NMDA receptor subunit expression levels in brain regions implicated in drug-dependence processes, based on the prediction that nicotine intake may elicit experience-dependent alterations in the function of NMDA receptors involved in its actions. Second, we employed in-vitro intracellular recordings to assess the excitatory effects of nicotine on NMDA receptor-mediated transmission in brain regions with altered NMDA receptor subunit expression. Finally, we examined the effects of infusing the NMDA receptor antagonist LY235959 into the identified brain regions on nicotine self-administration.
MATERIALS AND METHODS
Animals
Male Wistar rats (n=100; Charles River Laboratories, Raleigh, NC) weighing 300–320 (behavioral experiments) or 200–300 g (electrophysiological experiments) were housed in groups of 2–3 per cage in an environmentally controlled vivarium on a 12-h reverse light/dark cycle, with ad-libitum access to food and water until behavioral training commenced. All procedures were conducted in adherence with the National Institutes of Health Guide for the Care and Use of Laboratory Animals and were approved by the Institutional Animal Care and Use Committee of The Scripps Research Institute.
Drugs
For systemic administration, (−)-nicotine hydrogen tartrate salt (Sigma Chemical Co., St Louis, MO), LY235959 and NBQX (Tocris, Ballwin, MO) were dissolved in sterile saline solution (0.9% w/v), and delivered in a volume of 1 ml/kg body weight by subcutaneous (s.c.; nicotine) or intraperitoneal (i.p.; LY235959 and NBQX) injection. For intra-CeA or intra-VTA administration, LY235959 was dissolved in sterile saline, and administered bilaterally in a volume of 0.5 μl per side delivered over 66 s using stainless-steel injectors. Injectors were kept in place for an additional 60 s to allow for drug diffusion. Self-administration sessions were initiated 10–15 min later. For intravenous self-administration, nicotine was dissolved in sterile saline (pH adjusted to ∼7). Each infusion consisted of 0.03 mg per kg per infusion nicotine freebase, delivered over 1 s. All drug doses refer to the salt form, with the exception of nicotine doses that refer to the freebase form.
Surgery
Rats prepared with intracerebral cannulae or stimulating electrodes were first anesthetized by inhalation of 1–3% isoflurane in oxygen and positioned in a stereotaxic frame (Kopf Instruments, Tujunga, CA). Bilateral stainless steel guide cannulae (23 gauge, 14 mm in length) were implanted 2.5 mm above the VTA (AP, −4.8 mm from bregma; ML, ±1.0 mm; DV, 5.0 mm from skull surface) or 2.5 mm above the CeA (AP, −2.3 mm from bregma; ML, ±4.2 mm; DV, 4.5 mm from dura) (Paxinos and Watson, 1986). Cannulae were kept patent using 14 mm long stainless steel stylets (30 gauge). Bipolar ICSS electrodes (11 mm in length) were implanted into the posterior lateral hypothalamus (AP, −0.5 mm from bregma; ML, ±1.7 mm; DV, 8.3 mm from dura; incisor bar was adjusted to 5 mm above the interaural line) (Pellegrino et al, 1979). Four stainless steel skull screws and dental acrylic held the cannula or electrode in place. For self-administration, rats were anesthetized by inhalation of 1–3% isoflurane in oxygen and surgically prepared with silastic catheters in the jugular vein (Caine et al, 1993). The catheter was passed s.c. to a polyethylene assembly mounted on the animal's back. In the case of animals tested in both the self-administration and ICSS procedures, animals were first prepared with ICSS electrodes and trained in the ICSS threshold procedure (see below) prior to undergoing catheter surgery and self-administration training.
Western Blotting
Brains were rapidly removed from nonanesthetized subjects, frozen in isopentane, and kept on dry ice. To extract tissue from brain regions of interest, brains were sectioned at −20°C on a cryostat (HM 505 E, Microm, Walldorf, Germany) until the anterior end of each region of interest was exposed (distance from bregma: PFC, 2.20 mm; caudate-putamen (CPu), 1.60 mm; NAcc, 2.0 mm; CeA and basolateral amygdala (BLA), −2.30 mm; and VTA, −5.20 mm) (Paxinos and Watson, 1986). Bilateral 1 mm2 punches were then taken from each region as they came into plane, and were kept frozen on dry ice. Tissues were sonicated in 100 μl 1% SDS and the protein content of each sample adjusted to 2 mg per ml protein. NuPAGE LDS sample buffer (Invitrogen, Carlsbad, CA) and 50 mM dithiothreitol were added to each sample prior to heating at 70°C for 10 min. Each sample (20 μg) was loaded onto NuPAGE Novex 3–8% Tris-acetate gels (Invitrogen) for separation by gel electrophoresis. HiMark high molecular weight prestained standards (Invitrogen) were also run for molecular weight estimation. Proteins were subsequently transferred to polyvinylidene fluoride membrane (PerkinElmer Life Sciences, Boston, MA). Nonspecific binding was blocked for 2 h at room temperature (RT) in blocking buffer (5% nonfat dry milk in phosphate-buffered saline (PBS) and 0.1% Tween 20 (PBS-T)). Blots were incubated in primary antibody (1 : 3000 rabbit anti-NR2A; 1 : 3000 rabbit anti-NR2B (Chemicon International, Temecula, CA); 1 : 3000 rabbit anti-NR1; 1 : 2000 rabbit anti-GluR1; 1 : 3000 rabbit anti-GluR2 (this antibody detects GluR2 almost exclusively, although it is directed against a portion of GluRs that shares homology with GluR3 (Prince et al, 1995)) (Upstate, Lake Placid, NY)) in PBS-T overnight at 4°C. Blots were washed in PBS-T, then incubated in secondary antibody (1 : 5000 goat anti-rabbit horseradish peroxidase-linked IgG (Vector Laboratories, Burlingame, CA)) for 2 h at RT. Blots were washed, followed by immunological detection using Chemiluminescence Reagent Plus (PerkinElmer Life Sciences) and a Kodak Image Station 440. Antibodies were stripped from the blots by incubation with stripping buffer (62.5 mM Tris, 2% SDS, 100 mM β-mercaptoethanol, pH 6.8) for 15 min at 50°C, and subsequently re-blocked and probed with 1 : 20 000 rabbit anti-β-actin (Sigma). Optical density of protein bands was analyzed using an image analysis program (Kodak Digital Science 1D). Approximate band sizes: NR2A and NR2B, 180 kDa; GluR2, 110 kDa; GluR1, 106 kDa; NR1, 100 kDa; and β-actin, 42 kDa.
Electrophysiology
Amygdala slices (400 μm) were prepared as described previously (Roberto et al, 2006), superfused continuously (flow rate of 2–4 ml/min) with warm (31°C), gassed artificial cerebrospinal fluid (aCSF) of the following composition (in mM): NaCl, 130; KCl, 3.5; NaH2PO4, 1.25; MgSO4 7H2O, 1.5; CaCl2, 2.0; NaHCO3, 24; glucose, 10; and gassed with 95% O2 and 5% CO2. CeA neurons were recorded with sharp micropipettes (3 M KCl) using discontinuous voltage- or current-clamp mode. In voltage-clamp mode, a switching frequency of 3–5 kHz was used, and electrode settling time and capacitance neutralization at the headstage were monitored on a separate oscilloscope. Data were acquired with an Axoclamp-2A preamplifier (Axon Instruments, Foster City, CA) and stored for later analysis using pClamp software (Axon Instruments). Pharmacologically isolated NMDA receptor-mediated excitatory postsynaptic currents (NMDA-EPSCs) were evoked by stimulating locally within the CeA using a bipolar stimulating electrode in low Mg++ (0.75 mM instead of 1.5 mM) aCSF containing 30 μM bicuculline, 1 μM CGP-55845A, and 10 μM 6-cyano-7-nitroquinoxaline-2,3-dione (CNQX) to block γ-aminobutyric acid-A (GABAA) receptors, GABAB receptors and non-NMDA ionotropic glutamate receptors, respectively. Cells were held near resting membrane potential (RMP; mean: −76 mV), and hyperpolarizing/depolarizing current steps were applied (200 pA increments, 750 ms duration) to generate voltage–current (V/I) curves. Paired-pulse facilitation (PPF) of NMDA-EPSCs was examined in each neuron using 100 ms interstimulus intervals (Roberto et al, 2004). The stimulus strength was adjusted such that the amplitude of the first NMDA-EPSC was 50% of maximal determined in an input/output (I/O) relationship. The PPF ratio was calculated as the second NMDA-EPSC amplitude over that of the first. All measurements were made prior to and during (5–10 min) nicotine superfusion, and following nicotine washout (20–30 min).
ICSS Thresholds
Animals were trained to respond according to a modification of the discrete trial current threshold procedure (Kornetsky and Esposito, 1979; Markou and Koob, 1992). This is a rate-independent threshold measure, designed based on the psychophysical method of limits specifically to permit detection of the reward threshold with minimal sensitivity to performance-disrupting effects of pharmacological treatments (Markou and Koob, 1992). Briefly, ICSS current levels were varied in alternating descending and ascending series in 5 μA steps. In each testing session, four alternating descending/ascending series were presented. The threshold for each series was defined as the midpoint between two consecutive current intensities for which animals responded in at least two of the three trials, and two consecutive current intensities for which animals did not respond in two or more of the three trials. The overall threshold of the session was defined as the mean of the thresholds for the four individual series. Each testing session was 30 min in duration. Stable ICSS thresholds were defined as⩽10% variation in thresholds over 5 consecutive days, usually established after 10–14 days of training.
Intravenous Nicotine Self-Administration
Rats were food-restricted such that they maintained a body weight of 85% that of free-feeding rats, and were trained to press an active lever for 45 mg food pellets on a fixed ratio 5 time-out 20 s (FR5TO20) schedule of reinforcement. Rats were also presented with an inactive lever during training and testing sessions, responses on which were recorded but were without scheduled consequence (data not presented). Rats responded for food until stable intake was achieved, defined as>90 pellets per 1 h session. Rats then responded for nicotine on an FR5TO20 s schedule during 1-h daily sessions, when five active lever responses resulted in the delivery of one nicotine infusion (0.03 mg per kg per infusion freebase, 1 s infusion), which initiated the time-out period signaled by a light cue located above the lever, during which responding on the lever was without consequence.
Statistical Analyses
For ICSS experiments, percentage change from baseline reward thresholds was calculated by expressing the drug-influenced threshold scores as a percentage of the previous day's threshold (for experimenter-administered nicotine injections) or the mean thresholds obtained on the 3 days prior to the first nicotine self-administration session. Data were analyzed by two- or three-way repeated-measures analyses of variance (ANOVA) as appropriate. Post hoc comparisons among means were conducted with Fisher's protected t-tests. For nicotine self-administration and food-responding experiments, percentage change from baseline nicotine or food reinforcers was calculated by expressing the number of drug-influenced reinforcers earned as a percentage of the baseline number of reinforcers minus 100. Baseline intake was the mean number of reinforcers earned on the 3 days prior to each injection day. Data were subjected to two-factor repeated-measures ANOVA. IC50 values for the effects of LY235959 on nicotine or food intake were calculated using GraphPad Prism software (GraphPad, San Diego, CA). For Western blots, the optical density of the protein of interest was normalized to that of β-actin for each sample. Fold-induction data were analyzed by three-way repeated-measures ANOVA (Brain region × Treatment × Protein; with repeated-measures on Protein) followed by Fisher's protected t-tests for each brain region. For electrophysiological experiments, all values were analyzed by between- or within-subjects repeated-measures ANOVA as appropriate, followed by Newman–Keuls post hoc tests. In all cases, post hoc comparisons were performed only after significant main or interaction effects in an ANOVA. In this manner the null hypothesis could be rejected and Type I errors during post hoc test were less likely.
RESULTS
Experiment 1: NMDA Receptors Gate the Magnitude and Valence of the Effects of Nicotine on Brain Reward Systems
Rats (n=9) were prepared with ICSS electrodes and trained in the ICSS threshold procedure until stable thresholds were established (see above). Rats were then pretreated with saline or LY235959 (1 mg per kg) 30 min prior to testing, and received a nicotine injection (0, 0.125, 0.25, or 0.5 mg per kg; within-subjects Latin-square design) 10 min prior to being tested in the ICSS procedure. Next, the same rats were injected with saline or LY235959 (2.5 or 5 mg/kg, i.p.) 30 min prior to testing, and also a saline or nicotine (0.25 mg per kg, s.c.) injection 10 min prior to reward threshold assessment (Latin-square design). This dose of nicotine (0.25 mg per kg) was chosen because it induced maximal lowering of reward thresholds when tested alone or in combination with the lower dose (1 mg per kg) of LY235959 (Figure 1). There were at least 48 h between each drug injection.
N-methyl-D-aspartate (NMDA) receptor antagonism switched the effects of experimenter-administered nicotine on brain reward systems from stimulatory to inhibitory. (a) Rats (n=9) were pretreated with saline or LY235959 (1 mg per kg), and subsequently received saline or nicotine (0.125–0.5 mg per kg) injection. Data are expressed as mean (±SEM) percentage change from baseline thresholds. *p<0.05, effects of nicotine in saline and LY235959 pretreated rats compared with saline effects in saline and LY235959 pretreated rats, follow-up tests of the significant main effect of Nicotine in analysis of variance (ANOVA). (b) Rats were then pretreated with saline or LY235959 (2.5–5 mg per kg), and subsequently received saline or nicotine (0.25 mg per kg) injection. **p<0.01, saline–nicotine treatment compared with saline–saline treatment; ##p<0.01, LY235959–nicotine treatment compared with saline–nicotine treatment, post hoc tests after significant interaction effect in two-way ANOVA.
Mean (±SEM) baseline ICSS threshold prior to drug treatment was 128.8±13.9 μA. Two-way repeated-measures ANOVA on the data involving the 1 mg per kg LY235959 dose demonstrated a significant main effect of Nicotine (F(3,24)=6.3, p<0.01), no effect of LY235959 (1 mg per kg) (F(1,8)=0.18), and no significant LY235959 × Nicotine interaction (F(3,24)=1.1). Further analysis of the main effect of Nicotine demonstrated that thresholds were significantly lowered in rats pretreated with saline or LY235959 at nicotine doses 0.125–0.25 mg per kg (p<0.05; Figure 1a).
Two-way repeated-measures ANOVA on the data involving the two higher doses of LY235959 (2.5–5 mg per kg) and the threshold-lowering effects of a single dose of nicotine (0.25 m per kg) demonstrated a main effect of LY235959 (F(1,8)=6.4, p<0.01), a significant Nicotine × LY235959 interaction (F(1,8)=6.3, p<0.01), and no statistically significant main effect of nicotine (F(1,8)=0.02, p=0.9). Further analysis of the main effect of LY235959 demonstrated that reward thresholds were significantly elevated in rats pretreated with the highest does of LY235959 (5 mg per kg) (p<0.01; Figure 1b).
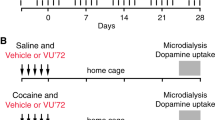
Experiment 2: Reward-Enhancing and Reinforcing Effects of Self-Administered Nicotine Require NMDA Receptors
Rats (n=16) were prepared with ICSS electrodes and trained in the ICSS threshold procedure until stable reward thresholds were achieved. All rats were then prepared with intravenous catheters. One group of rats (nicotine rats; n=9) was trained in the nicotine self-administration procedure, and reward thresholds were assessed 1-h before (prethresholds) and 15 min after (postthresholds) each self-administration session. The remaining rats (control rats; n=7) were tested in the ICSS procedure at the same time each day as the self-administering rats, but were returned to their home cages during the self-administration sessions, and thus remained nicotine naive throughout the experiment.
Mean (±SEM) baseline ICSS thresholds prior to the start of nicotine self-administration were 92.1±15.2 and 75.3±5.2 μA in the nicotine and control rats, respectively. Mean (±SEM) baseline number of nicotine infusions earned by nicotine rats was 10.5±1.0. As expected, prethresholds and postthresholds remained stable and unaltered in the control rats (Figure 2a). However, in replication of our recently published data (Kenny and Markou, 2006; Paterson et al, 2008), daily postthresholds were lowered after each self-administration session in the nicotine rats compared to prethresholds during the initial 7-day access to nicotine, prior to any LY235959 treatment (Figure 2b). In addition, a downward drift was observed in pre- and postthresholds in nicotine rats (Figure 2b) similar to that previously reported (Kenny and Markou, 2006), reflecting a long-lasting nicotine-induced increase in the baseline sensitivity of brain reward systems. Accordingly, two-way repeated-measures ANOVA over this 7-day period on threshold data from control and nicotine rats demonstrated a significant main effect of Drug (nicotine or control group) (F(1,13)=5.7, p<0.05), a main effect of Session (prethresholds or postthresholds) (F(1,13)=6.3, p<0.05), and a significant Drug × Session interaction (F(1,13)=7.9, p<0.05). Two-way ANOVA of the threshold data obtained only from the nicotine rats over this time period revealed significant main effects of Days (F(6,48)=2.3, p<0.05) and Session (F(1,8)=12.1, p<0.01).
N-methyl-D-aspartate (NMDA) receptor antagonism switched the effects of self-administered nicotine on brain reward systems from stimulatory to inhibitory and thereby decreased nicotine self-administration in rats. (a) Pre- and postthresholds for control rats (n=7), expressed as mean (±SEM) percentage change from baseline thresholds on the 7 days prior to LY235959 treatment. (b) Pre- and postthresholds for nicotine self-administering rats (n=9) on the 7 days prior to LY235959 treatment. **p<0.01, main effect of nicotine on reward thresholds, two-way analysis of variance (ANOVA). (c) Effects of LY235959 on pre- and postthresholds in control rats. (d) Effects of LY235959 on reward thresholds in nicotine rats. Three-way ANOVA demonstrated no effect of Session (pre- or postthresholds) in nicotine rats, so pre- and postthresholds were collapsed and analyzed by one-way ANOVA. Post hoc analyses demonstrated that LY235959 significantly elevated thresholds at the 1 (*p<0.05) and 2.5 mg per kg (***p<0.001) doses. (e) Effects of LY235959 on nicotine self-administration. Data are expressed as mean (±SEM) percentage change from baseline nicotine infusions. *p<0.05, ***p<0.001 compared with vehicle treatment; post hoc test after significant one-way ANOVA. (f) Effects of LY235959, administered after nicotine self-administration but prior to postthresholds assessment, on postthresholds in control and nicotine rats. LY235959 was administered in this manner to examine its effects on nicotine-induced lowering of reward thresholds without the confounding inhibitory influence of LY235959 on nicotine self-administration. *p<0.05, **p<0.01, and ***p<0.001, compared with postthresholds in nicotine rats after saline injection; post hoc test after significant one-way ANOVA. (g) The effects of LY235959 on nicotine self-administration compared with food intake. Data are expressed as mean (±SEM) percentage change from baseline nicotine infusions (n=7), or change from baseline food reinforcers under an FR5TO20 s reinforcement schedule (n=8), or under an FR5TO210 s schedule (n=7) that equated rates of responding for nicotine and food. **p<0.01 compared with nicotine infusions earned after vehicle injection; pair-wise test after significant ANOVA. #p<0.05 compared with corresponding food reinforcers under an FR5TO210 s schedule; ^^p<0.01 compared with corresponding food reinforcers earned an FR5TO20 s schedule; pair-wise test after significant ANOVA. (h) Effects of NBQX on nicotine self-administration and food responding under an FR5TO20 s schedule. Data are expressed as mean (±SEM) percentage change from baseline nicotine infusions or food reward earned.
After 7 consecutive days of nicotine self-administration, the effects of LY235959 on reward thresholds were examined in nicotine and control rats. First, the effects of LY235959 on prethresholds, nicotine self-administration, and postthresholds were assessed. That is, both groups of rats were pretreated with LY235959 (0, 0.5, 1, or 2.5 mg per kg; Latin-square design; minimum of 7 days between injections), and 15 min later prethresholds were assessed. Rats were then permitted to self-administer nicotine or were returned to their home cages (control rats), and postthresholds were subsequently assessed. Administration of LY235959 before prethreshold assessment did not alter prethresholds or postthresholds in control rats (Figure 2c). However, LY235959 blocked the lowering of post-nicotine reward thresholds typically observed in nicotine rats (Figure 2d). Three-way repeated-measures ANOVA on the reward threshold data confirmed a significant main effect of LY235959 (F(3,42)=4.5, p<0.01), a significant Drug (nicotine or control group) × LY235959 interaction (F(3,42)=3.8, p<0.05). Two-way ANOVA on the reward threshold data from the nicotine rats demonstrated a main effect of LY235959 (F(3,24)=6.5, p<0.01).
Because no effect of Session was observed in the above analysis, data from the two Sessions (prethresholds and postthresholds) were combined for each dose and then compared with the 0 mg per kg treatment condition for the nicotine rats. This analysis indicated that there was a main effect of LY235959 (F(3,24)=10.3, p<0.001), and that thresholds tended to be elevated at the 0.5 mg per kg dose (p=0.06), and were significantly elevated at the 1 (p<0.05) and 2.5 mg per kg (p<0.001) LY235959 doses compared with thresholds observed after saline treatment (Figure 2d).
In addition to reversing the lowering effects of self-administered nicotine on ICSS thresholds, LY235959 also decreased nicotine intake. Mean (±SEM) baseline number of nicotine reinforcers earned by the nicotine rats prior to LY235959 treatment was 12.0±1.5. LY235959 dose dependently decreased nicotine intake in the nicotine rats (Figure 2e), reflected in a significant effect of LY235959 (F(3,24)=41.0, p<0.001). Post hoc analysis demonstrated that nicotine intake was significantly decreased by 0.5 (p<0.05) and 1–2.5 mg per kg (p<0.01) LY235959 doses (Figure 2e).
Next, we examined the effects of LY235959 (0–2.5 mg per kg; Latin-square design) administered immediately after the self-administration session on postthresholds assessed 15 min later. In this manner, we could directly assess the influence of LY235959 on threshold lowering induced by self-administered nicotine while avoiding the confounding inhibitory effects of LY235959 on nicotine self-administration. LY235959 administered in this manner reversed the lowering of postthresholds observed in the nicotine rats, but did not alter thresholds in control rats (Figure 2f). Two-way repeated-measures ANOVA demonstrated a significant main effect of LY235959 (F(3,42)=6.5, p<0.01), a significant Drug (nicotine or control group) × LY235959 interaction (F(3,42)=8.3, p<0.001), and no main effect of Drug (F(1,14)=1.7, p=0.2). One-way repeated-measures ANOVA of threshold data from nicotine rats demonstrated a significant effect of LY235959 (F(3,24)=13.5, p<0.001). Post hoc analysis on the reward thresholds in nicotine rats demonstrated that thresholds were significantly elevated after the 0.5 (p<0.05), 1 (p<0.01), and 2.5 mg/kg (p<0.001) LY235959 doses compared to thresholds after saline administration (Figure 2f).
To determine if the inhibitory effects of LY235959 on nicotine self-administration observed in the nicotine rats above (Figure 2e) were secondary to a disruptive effect on operant performance, we again assessed the effects of LY235959 (0.1–5 mg per kg) on nicotine self-administration in a new cohort of rats, and compared these effects with the actions of LY235959 on responding for food reinforcement. Nicotine self-administering rats (n=7) were injected with LY235959 (0, 0.1, 0.5, 1, 2.5, or 5 mg/kg; Latin-square design), and nicotine intake was evaluated 30 min later. The effects of LY235959 were also assessed in rats (n=8) trained to respond for food reinforcement (45 mg pellet) under an FR5TO20 s schedule, and in rats (n=7) trained under a FR5TO210 s schedule. This adjusted schedule incorporated a longer time-out period (210 vs 20 s) that better equated rates of responding for nicotine and food.
Mean (±SEM) baseline number of nicotine infusions earned by this second cohort of rats prior to treatment with LY235959 was 10.8±0.7. The mean (±SEM) baseline number of food rewards earned by rats under the FR5TO20 s and the FR5TO210 s schedules of reinforcement prior to LY235959 treatment was 109.5±9.6 and 16.3±0.3, respectively. Two-way repeated-measures ANOVA demonstrated a significant effect of Reinforcer (F(2,19)=17.2, p<0.001), a significant effect of LY235959 (F(5,10)=19.4, p<0.001), and no Reinforcer × LY235959 interaction (F(10,95)=1.4). Preplanned comparisons demonstrated that LY235959 decreased nicotine intake at doses⩾0.5 mg per kg (Figure 2g; confirming the results reported above in a separate cohort of rats shown in Figure 2e), but decreased food intake under FR5TO20 or FR5TO210 s reinforcement schedules only at the highest doses tested (2.5–5 mg per kg; Figure 2g). Further analyses of the above data demonstrated that LY235959 decreased nicotine intake with an IC50 of 0.53 mg per kg, and decreased food responding under FR5TO20 and FR5TO210 s schedules with IC50 values of 1.88 and 2.2 mg per kg, respectively.
Next, to determine whether glutamate transmission in general, or if NMDA receptor-mediated glutamate transmission selectively impacts nicotine reward, the effects of the AMPA receptor antagonist NBQX (0, 0.1, 0.5, 1, and 5 mg per kg; Latin-square design) on nicotine self-administration (n=8) and on food responding (n=5) were assessed under FR5TO20 s reinforcement schedules. Mean (±SEM) baseline number of nicotine infusions and food reinforcers earned prior to NBQX treatment was 17.1±1.8 and 141.1±8.3, respectively. Two-way repeated-measures ANOVA demonstrated that NBQX did not alter responding for nicotine or food reinforcement at any dose tested (Reinforcer: F(1,11)=0.5; NBQX, F(4,4)=0.08; Reinforcer × NBQX, F(4,44)=1.5) (Figure 2h).
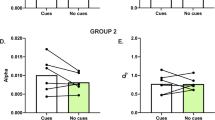
Experiment 3: Nicotine Self-Administration Alters Glutamate Receptor Subunit Expression Levels in Reward Circuits
In Experiments 1 and 2, we found that NMDA receptors regulate nicotine-induced lowering of ICSS thresholds and nicotine self-administration in rats. Next, we hypothesized that populations of NMDA receptors that regulate the nicotine reinforcement may undergo adaptations, such as altered expression profiles, upon repeated exposure to self-administered nicotine. Hence, we examined the expression levels of NMDA receptor subunits NR1, NR2A, and NR2B in the brains of nicotine self-administering rats (n=9; 21 consecutive 1-h daily sessions) and control saline self-administering rats (n=8) that were also prepared with intravenous catheters and had as many exposures to the operant testing chambers as the nicotine self-administering rats. Rats were decapitated without anesthesia 24 h after their last self-administration session (at the time when the next self-administration session would have occurred) and their brains were rapidly frozen. This treatment regimen was chosen because it corresponds closely with the total number of days of access to nicotine that rats had in Experiment 2 above. In addition, we examined the expression levels of AMPA receptor subunits GluR1 and GluR2. Tissue samples were processed for Western blotting as described in the ‘Materials and Methods’ section.
Mean (±SEM) baseline number of nicotine and saline infusions earned prior to tissue harvesting was 10.6±0.9 and 3.3±0.9, respectively. Three-way repeated-measures ANOVA revealed a statistically significant Brain Region × Treatment × Protein interaction (F(20,192)=2.4344, p=0.001). Post hoc comparisons among expression levels in discrete brain regions revealed the following: in the VTA, there was a significant increase of NR2A subunit expression in nicotine rats compared with controls (p<0.05; Figure 3a); in the CeA there were statistically significant increases in the expression of NR2A, NR2B, NR1, GluR1, and GluR2 subunits in nicotine rats compared with controls (p<0.05 in each case; Figure 3b); in the NAcc there was a significant increase in GluR1 expression in nicotine rats compared with controls (p<0.05; Figure 3d). Conversely, in the PFC, there were statistically significant decreases in the expression of NR2A, NR2B, and GluR2 receptor subunits in nicotine rats compared with controls (p<0.05 in each case; Figure 3c). There were no differences in expression levels between nicotine rats and controls in CPu or BLA (data not shown).
Nicotine self-administration alters the expression of glutamate receptor subunits in reward-related cortical and limbic brain regions. Rats were permitted to self-administer nicotine for 21 days, or remained nicotine naive over the same time period and euthanized 24 h after the last nicotine self-administration session for the nicotine rats. (a) Upper panel, exposure to nicotine self-administration increased the expression of the N-methyl-D-aspartate (NMDA) receptors subunit NR2A in the ventral tegmental area (VTA). Lower panel, representative blots from control (saline-treated; Con) and nicotine self-administering (Nic) rats for the subunit that demonstrated altered expression levels and for β-actin. (b) Upper panel, nicotine self-administration increased expression of NR2A, NR2B, and NR1 subunits, and increased expression of the AMPA receptor subunits GluR1 and GluR2 compared with control rats in the central nucleus of the amygdala (CeA). Lower panel, representative blots for the subunits that demonstrated altered expression levels and for β-actin. (c) Upper panel, nicotine self-administration decreased expression of NR2A, NR2B, and GluR2 subunits compared with control rats in the prefrontal cortex (PFC). Lower panel, representative blots for the subunits that demonstrated altered expression levels and for β-actin. (d) Upper panel, nicotine self-administration increased expression of GluR1 subunits compared with control rats in the nucleus accumbens (NAcc). Lower panel, representative blots for the subunit that demonstrated altered expression levels and for β-actin. *p<0.05, **p<0.01 compared with nicotine-naive controls; post hoc test after significant three-way analysis of variance (ANOVA).
Experiment 4: Nicotine Increases NMDA Receptor-Mediated Transmission in Rat CeA Slices
In Experiment 3, we found that chronic nicotine self-administration increased NMDA receptor subunit expression in the CeA and VTA (see Figure 3). Based on these data we hypothesized that nicotine may act in the CeA to increase NMDA receptor-mediated transmission similar to its effects in the VTA (see Introduction), an action that could potentially contribute to its reinforcing and reward-enhancing properties. To test this hypothesis, we examined the effects of nicotine on NMDA receptor-mediated transmission in rat CeA neurons.
Recordings were made from seven CeA neurons (from n=7 rats) that had a mean RMP of −76±2 mV and a mean input resistance of 108±6 MΩ. After obtaining a stable baseline of evoked, pharmacologically isolated NMDA-EPSCs (10–15 min), nicotine (1 μM) was superfused for 7–10 min. Nicotine applied for 7–10 min increased (∼25%; assessed at ∼2–3 min of nicotine application; F(4,14)=7.05; p<0.05) NMDA-EPSCs in rat CeA slices (Figure 4a, upper and lower panels). Nicotine had no effects on basic membrane properties such as membrane potential, input resistance, or spike amplitude (data not shown). To investigate whether the stimulatory effects of nicotine on NMDA-EPSCs were regulated by a presynaptic action on excitatory glutamate inputs, the PPF of NMDA-EPSC in CeA neurons was examined before, during, and after nicotine application. Nicotine (1 μM) decreased (F(5,5)=10.2; p<0.05) the PPF ratio of NMDA-EPSCs (Figure 4b; upper and lower panels). Similarly, nicotine also decreased (p<0.05) the PPF of compound glutamate (NMDA and non-NMDA) EPSCs (isolated by bicuculline and CGP-55845A to block GABAA and GABAB receptors, respectively; n=6) and also non-NMDA EPCSs (isolated by aminophosphonovaleric acid (NMDA receptor blocker), bicuculline, and CGP-55845A; n=5), by approximately 15% in CeA (data not shown). Thus, nicotine likely increased NMDA receptor-mediated transmission in the CeA by activating presynaptic nicotinic receptors to facilitate the release of glutamate, which subsequently activated postsynaptic NMDA receptors.
Nicotine increases N-methyl-D-aspartate (NMDA) receptor-mediated transmission in rat central nucleus of the amygdala (CeA) slices. (a) Nicotine (1 μM) increased the amplitude of evoked, pharmacologically isolated NMDA receptor excitatory postsynaptic currents (EPSCs) in CeA neurons. Upper panel, current records of evoked NMDA-EPSCs in a CeA neuron before, during and after nicotine superfusion. Lower panel, in CeA neurons, nicotine (2–3 min of application) induced a transient increase in the mean amplitudes of five evoked NMDA-EPSCs by approximately 25% compared with pretreatment levels. *p<0.05, post hoc test after significant analysis of variance (ANOVA). (b) Application of nicotine (1 μM) increased glutamate release in CeA neurons. Upper panel, current records of NMDA-EPSCs in response to two stimuli (paired pulses) spaced 100 ms apart in a CeA neuron. Lower panel, pooled data of paired-pulse facilitation (PPF) ratios expressed as the second NMDA-EPSC amplitude over the first. Nicotine decreased the mean PPF ratio of NMDA-EPSCs, suggesting a presynaptic stimulatory effect of nicotine on glutamate release in CeA tissues. *p<0.05, post hoc test after significant ANOVA.
Experiment 5: NMDA Receptors in the VTA and CeA Regulate Nicotine Self-Administration
On the basis of the protein expression and electrophysiological data obtained in Experiments 3 and 4, we hypothesized that NMDA receptors in the CeA and VTA may regulate nicotine reinforcement. To test this hypothesis, we next examined the effects of intra-VTA and intra-CeA infusions of LY235959 on nicotine self-administration. Rats with bilateral cannulae directed toward the CeA or VTA were trained in the nicotine self-administration procedure until stable nicotine intake was achieved. LY235959 then was injected directly into the CeA or VTA (0, 0.1, 0.5, 1, or 10 ng per 0.5 μl per side; n=10 VTA, n=6 CeA; Latin-square design; minimum of 7 days between injections), and nicotine self-administration was evaluated 10–15 min later. Next, rats received a control injection of LY235959 (1 ng per 0.5 μl per side) 2 mm above the CeA or VTA. At the conclusion of the experiments, all animals were anesthetized and perfused with 10% formalin solution, and their brains were removed. The brains were cut in 50 μm sections, stained by cresyl violet staining, and placements of the injectors and the cannulae were examined. Only those rats with injection tips located within the CeA or VTA were included in statistical analyses.
Mean (±SEM) baseline numbers of nicotine reinforcers earned prior to intra-VTA or intra-CeA LY235959 infusions were 11.5±1.3 and 11.22±2.1, respectively. Injection of LY235959 (0.1–10 ng per 0.5 μl per side) into the VTA dose dependently decreased nicotine self-administration (F(4,28)=7.3, p<0.001; Figure 5b; see Figure 5a for a graphical representation of the injection sites after histological examination). Post hoc analysis revealed that nicotine intake was significantly decreased by doses of LY235959⩾1 ng per 0.5 μl per side (Figure 5b). Further analyses of the above data demonstrated that LY235959 decreased nicotine intake with an IC50 of 0.87 ng per 0.5 μl (per side), and by approximately 40% at the IC50 value. A dose of LY235959 (1 ng per 0.5 μl per side) that significantly decreased nicotine self-administration after intra-VTA administration did not alter nicotine intake when infused 2 mm above the VTA (Figure 5b). Similarly, injection of LY235959 (0.1–10 ng per 0.5 μl per side) into the CeA dose dependently decreased nicotine self-administration (F(5,15)=7.5, p<0.01; Figure 5d; see Figure 5c for a graphical representation of the injection sites). Post hoc analysis revealed that nicotine intake was significantly decreased by doses of LY235959⩾1 ng per 0.5 μl per side (Figure 5d). LY235959 (1 ng per 0.5 μl per side) infused 2 mm above the CeA did not alter nicotine intake (Figure 5d). LY235959 administered into the CeA decreased nicotine self-administration with an IC50 value of 0.97 ng per 0.5 μl (per side), and reduced intake by approximately 20% at the IC50 value.
N-methyl-D-aspartate (NMDA) receptors in the ventral tegmental area (VTA) and central nucleus of the amygdala (CeA) regulate nicotine self-administration. (a) Diagrammatic representation of coronal sections from the rat brain showing histological reconstruction of the injection sites in the VTA. Black lines indicate locations of cannulae and injector tips (n=7) in the VTA that were included in the statistical analysis. (b) LY235959 (0.1–10 ng per 0.5 μl per side) administered into the VTA, but not 2 mm above (1 ng per 0.5 μl per side), decreased nicotine self-administration. *p<0.05, **p<0.01, difference from nicotine infusions earned after vehicle injection, post hoc test after significant one-way analysis of variance (ANOVA). (c) Histological reconstruction of the injection sites in the CeA. Black lines indicate locations of cannulae and injector tips (n=6) in the CeA that were included in statistical analysis. (d) LY235959 (0.1–10 ng per 0.5 μl per side) administered into the CeA, but not 2 mm above (1 ng per 0.5 μl per side), decreased nicotine self-administration. *p<0.05, **p<0.01, difference from nicotine infusions earned after vehicle injection, post hoc test after significant one-way ANOVA.
DISCUSSION
LY235959 is the active isomer of LY274614 (Ornstein et al, 1993) and acts as a highly potent and selective competitive antagonist at NMDA receptors in vivo and in vitro (Schoepp et al, 1991; Fischer and Dykstra, 2006). We found that LY235959 attenuated the amplification of brain reward function induced by experimenter-administered or intravenously self-administered nicotine injections, as reflected in blockade of nicotine-induced lowering of ICSS thresholds. Indeed, antagonism of NMDA receptors switched the effects of volitional and nonvolitional nicotine administration on brain reward systems from stimulatory to inhibitory, detected by nicotine-induced elevations of ICSS thresholds. Furthermore, LY235959 decreased nicotine self-administration at doses that did not alter responding for food reinforcement, whereas the AMPA receptor antagonist NBQX did not alter nicotine self-administration behavior. These observations suggest that NMDA receptors, but not AMPA receptors, regulate the magnitude and valence of nicotine's effects on brain reward systems, and may thereby regulate nicotine self-administration behavior. We also found that NMDA receptor subunit expression was upregulated in the CeA and VTA of nicotine self-administering rats, that nicotine transiently increased EPSCs in the CeA via potentiation of glutamate release similar to its previously reported effects in the VTA, and that LY235959 infused into the CeA or VTA decreased nicotine self-administration. Taken together, these findings suggest that nicotine enhances glutamate-mediated transmission at NMDA receptors in the CeA and VTA, and that this action of nicotine is central to its stimulatory effects on brain reward function and the motivation to consume the drug. Further, it is likely that NMDA receptors that regulate the reinforcing actions of nicotine undergo profound adaptations after chronic exposure to volitionally consumed nicotine.
Reward-Enhancing and Reinforcing Effects of Nicotine Require NMDA Receptors
Experimenter-administered nicotine infusions lowered ICSS thresholds, suggesting that nicotine increased the rewarding effects of ICSS; that is, nicotine enhanced the reward value of the ICSS stimulation. We found that lower doses of LY235959 blocked, whereas a higher dose reversed the effects of experimenter-administered nicotine from reward enhancing into reward inhibitory. Importantly, doses of LY235959 (2.5–5 mg per kg) that blocked or reversed the effects of nicotine on brain reward systems had no effects on baseline reward thresholds in saline pretreated animals. Similarly, these doses of LY235959 did not alter response latencies, considered an accurate measure of performance in the ICSS procedure (Kornetsky and Esposito, 1979; Markou and Koob, 1992), in saline- or nicotine-treated rats (data not shown). These observations support the notion that LY235959 selectively modulates the reward-related effects of nicotine, and that the actions of LY235959 are not secondary to inhibitory effects on motor performance in the ICSS procedure.
Considerable evidence suggests that brain reward systems may respond differentially to volitional vs nonvolitional drug consumption. Indeed, neurobiological correlates of reward (eg neurotransmitter release in the basal ganglia) are increased after response-contingent drug infusions by a far greater magnitude than by response non-contingent drug infusions (Wilson et al, 1994; Mark et al, 1999; Kimmel et al, 2005; Lecca et al, 2007). In addition, different gene expression, neurochemical, stress system, and behavioral adaptations occur in response to volitional vs nonvolitional drug consumption (Stefanski et al, 1999; Jacobs et al, 2005). Therefore, in addition to effects on experimenter-administered nicotine injections, we also assessed the effects of LY235959 on the threshold lowering induced by intravenously self-administered nicotine infusions. We found that at lower doses LY235959 blocked nicotine-induced lowering of reward thresholds in self-administering rats, and at higher doses LY235959 reversed the effects of nicotine on brain reward systems from stimulatory to inhibitory. LY235959 also reversed the long-lasting stimulatory actions of volitionally consumed nicotine on brain reward systems, reflected in persistently lowered reward thresholds assessed before each daily self-administration session (prethresholds; Figure 2d). Importantly, doses of LY235959 that reversed the effects of nicotine on reward thresholds in nicotine self-administering animals did not alter thresholds in control animals. Hence, together with the fact that reward thresholds detected in the rate-free procedure utilized in these studies are not affected by motoric effects of manipulations, these effects of LY235959 are unlikely to be secondary to nonspecific inhibitory actions on operant performance. Taken together, the above data are consistent with a permissive role for NMDA receptors in regulating the stimulatory effects of nicotine on brain reward systems. Blockade of α7 nAChRs in the VTA could similarly reverse the hedonic valence of VTA-infused nicotine injections from rewarding to aversive, measured in a place-conditioning procedure (Laviolette and van der Kooy, 2003). Nicotine increases glutamate release in the VTA by a stimulatory action at α7 nAChRs, and thereby facilitates NMDA receptor-mediated transmission in this brain region (Mansvelder and McGehee, 2000; Schilstrom et al, 2000). Thus, blockade of nicotine's stimulatory effects on NMDA receptor-mediated transmission, either directly or indirectly, likely switches the hedonic valence of nicotine from positive to negative.
In addition to reversing the reward-enhancing effects of nicotine, LY235959 also dose dependently decreased nicotine self-administration. Furthermore, a broad range of LY235959 doses (0.1–1 mg per kg) that decreased nicotine self-administration failed to alter responding for food under a similar schedule of reinforcement (FR5TO20 s), or under an adjusted schedule (FR5TO210 s) that better equated overall rates of responding for food and nicotine. Thus, antagonism of NMDA receptors unlikely decreased nicotine intake by inducing nonspecific deficits in operant performance. Instead, these data are consistent with the hypothesis that nicotine-induced amplification of brain reward activity provides an important source of motivation that supports the initiation and maintenance of nicotine self-administration in rats (Kenny and Markou, 2006), and perhaps the tobacco-smoking habit in humans (Donny et al, 2003; Kenny, 2007). On the basis of our observation that NMDA receptor blockade reversed the valence of nicotine's actions on reward circuitries, we may speculate that NMDA receptor antagonism decreased nicotine intake by rendering rats less sensitive to the appetitive effects of nicotine and more sensitive to its aversive effects (see Laviolette et al, 2002; Laviolette and van der Kooy, 2003). Such an interpretation would account for the fact that rats did not display compensatory increases in their nicotine intake after LY235959 treatment similar to those observed in cocaine or amphetamine self-administering rats treated with doses of dopamine receptor antagonists that attenuate the rewarding effects of these drugs (Yokel and Wise, 1975; Koob et al, 1987).
In rats that intravenously self-administered nicotine, we observed a gradual lowering of baseline reward thresholds across days, an effect not observed in nicotine-naive control rats. This observation confirms recent data from our laboratory (Kenny and Markou, 2006) and suggests that the excitatory effects of self-administered nicotine on reward systems are long lasting and at least partly cumulative (Kenny and Markou, 2006). Intriguingly, recent data from human patients have shown that even a single exposure to nicotine can induce persistent increases (>7 days) in sensitivity to nondrug-rewarding environmental stimuli (Barr et al, 2007). Considering that nicotine-induced amplification of brain reward signals is considered an important factor in motivating nicotine consummatory behaviors (Kenny and Markou, 2006; Kenny, 2007), the enduring stimulatory effects of nicotine on reward systems could potentially contribute to the reinforcing effects of the drug and facilitate the development of nicotine dependence. The mechanisms by which self-administered nicotine elicits persistent increases in reward sensitivity are unclear but may involve hypersensitivity of nAChRs located in brain reward systems (Dani and Heinemann, 1996; Buisson and Bertrand, 2002). Indeed, the nAChR antagonist dihydro-β-erythroidine blocked both the acute lowering of reward thresholds and also the persistently lowered baseline reward thresholds induced by self-administered nicotine in rats (Kenny and Markou, 2006). Similarly, in the present study LY235959 also reversed acutely lowered and persistently lowered baseline reward thresholds in nicotine self-administering rats. Thus, it is possible that persistently activated NMDA receptors in brain reward circuitries, either directly through altered number and/or function of these receptors (see below) or perhaps indirectly through nicotine-induced hyperactivity of nAChRs, may contribute to the enduringly increased reward sensitivity in nicotine self-administering rats.
Noncompetitive antagonists of the NMDA receptor such as phencyclidine, ketamine, and dizocilpine, have reward-facilitating actions and can lower ICSS thresholds in rats (Herberg and Rose, 1989; Carlezon and Wise, 1993). This stimulatory action of NMDA receptor channel blockers on brain reward systems likely contributes to the abuse liability of these ligands. In the present study, we found that LY235959 had no intrinsic reward-facilitating (ie ICSS threshold-lowering) effects at any dose tested. Thus, it is likely that LY235959 and mechanistically related NMDA receptor antagonists are likely hedonically inert. The reason for the differential sensitivity of brain reward systems to noncompetitive vs competitive NMDA receptor antagonists is presently unclear. However, one possible explanation is the fact that NMDA receptor channel blockers are ‘use-dependent’ antagonists that voltage dependently occlude NMDA receptors, whereas competitive antagonists act at the glutamate-binding site to competitively antagonize NMDA receptors. Thus, it is possible that NMDA receptor channel blockers but not competitive antagonists may selectively target populations of NMDA receptors, perhaps in a voltage-dependent manner, which have a tonic inhibitory influence on brain reward systems. Whatever the explanation may be, the present data suggest that the competitive NMDA receptor antagonists are hedonically inert and therefore devoid of intrinsic abuse liability, an observation that supports their potential clinical utility for the treatment of substance abuse disorders.
Plasticity of Glutamate Receptors in Brain Reward Circuits Induced by Self-Administered Nicotine
Far lower doses of LY235959 (0.5–1 mg per kg) were required to block the ICSS threshold-lowering effects of self-administered nicotine compared with those doses (⩾2.5 mg per kg) required to block the effects of bolus experimenter-administered nicotine injections (Figures 1 and 2). The magnitude by which reward thresholds were lowered was equivalent following experimenter-administered or self-administration nicotine injections. Furthermore, rats obtained similar amounts of acute nicotine under these two treatment conditions. Thus, the increased sensitivity to LY235959 in nicotine self-administering rats was unlikely secondary to differences in the magnitude by which thresholds were lowered, or to different amounts of nicotine acting on reward systems. Instead, these observations suggest that populations of NMDA receptors that regulate the actions of nicotine may undergo functional adaptation after nicotine self-administration, thereby increasing their sensitivity to antagonist blockade. On the basis of this behavioral observation, we next assessed NMDA receptor subunit expression levels in the brains of nicotine self-administering rats compared with controls. The underlying hypothesis was that populations of NMDA receptors that regulate the reinforcing effects of nicotine would undergo compensatory adaptations, including altered expression of the protein subunits that compose the receptor, upon repeated activation by self-administered nicotine infusions.
In general, NMDA receptors are heteromeric complexes composed of multiple NR1 subunits in combination with at least one of the four types of NR2 subunits (Cull-Candy et al, 2001). Both NR1 and NR2 subunits confer distinct properties to the NMDA receptor, and changes in expression levels of the subunits would be expected to alter NMDA receptor subunit stoichiometry and function. We found that the expression of NMDA receptor subunits (NR2A, NR2B, and/or NR1) was increased in the VTA and CeA, decreased in the PFC, and unaltered in the NAcc, BLA, or CPu, of nicotine self-administering rats compared with controls. Importantly, similar increases in NMDA receptor subunit expression in the VTA and CeA and decreases in the PFC have been observed in rats self-administering cocaine, opiates, or alcohol and in post-mortem brain tissues from human cocaine users (Ortiz et al, 1995; Ghasemzadeh et al, 1999; Lu et al, 2003, 2005; Tang et al, 2003; Turchan et al, 2003; Roberto et al, 2006; Ben-Shahar et al, 2007). The effects of self-administered nicotine on NMDA receptor subunit expression were far more pronounced in the CeA compared with the VTA. Indeed, marked increases were observed in the expression of all NMDA receptor subunits assessed in the CeA, whereas only the NR2A subunit was increased in the VTA. The underlying mechanism or functional significance of this differential pattern of NMDA receptor subunit upregulation is unclear but may indicate that the CeA is particularly sensitive to the effects of nicotine and readily undergoes functional adaptations upon consumption of the drug. A caveat to these expression data is that NMDA receptor subunit levels were detected in tissue homogenates, and not from purified membrane homogenates in which mature NMDA receptors are located. Thus, the altered NMDA receptor subunit expression levels that were observed may reflect, in part, altered levels of intracellular subunits not yet incorporated into mature receptors in the membrane. In contrast to the present data, a recent study reported that nicotine intake did not alter NMDA receptor subunit expression in the VTA, and increased expression in the PFC (Wang et al, 2007). The effects of nicotine self-administration on NMDA receptor subunit expression in the amygdala were not assessed in this previous study (Wang et al, 2007). There are a number of methodological differences that may account for these apparent discrepancies. First, in the present investigations Wistar rats were used, whereas Wang et al used Sprague–Dawley. Further, in our studies rats were permitted 1-h daily access to nicotine self-administration, whereas the previous study employed a 23-h daily access schedule. Finally, in our study brain tissues were harvested approximately 23-h after the final nicotine self-administration session, whereas Wang et al collected brains approximately 30 min after the last nicotine infusion (Wang et al, 2007). Thus, it is possible that expression levels of NMDA receptor subunits may be temporally regulated in a highly dynamic manner, such that the time since last nicotine exposure may be important in determining the direction in which NMDA receptor subunit levels are altered. Our data suggest that NMDA receptors in the VTA, CeA, and PFC undergo profound plasticity upon repeated exposure to rewarding doses of self-administered nicotine. Recent data have shown that other glutamate receptors, including group II metabotropic glutamate (mGlu2/3) receptors, similarly undergo profound adaptations upon repeated exposure to self-administered nicotine and when assessed 24 h after the last nicotine self-administration sessions (Liechti et al, 2007) similar to the present study. In future studies, it will be interesting to determine if similar adaptations in NMDA receptors are observed in ‘yoked’ animals that receive intravenous nicotine infusions nonvolitionally in a manner time-locked to a partner rat that responds for nicotine volitionally. Inasmuch as altered NMDA receptor subunit expression levels can be correlated with complex behavioral states, we speculate that these data may explain the differential sensitivity to NMDA receptor blockade that we observed in these rats relative to non-self-administering rats. Importantly, NMDA receptor plasticity is considered a fundamental process in the regulation of synaptic efficacy and remodeling in the brain (Lau and Zukin, 2007). Thus, the nicotine-induced plasticity in NMDA receptors located in brain regions heavily implicated in drug-dependence processes may be important in the persistence of nicotine self-administration behavior in rats, and perhaps the tobacco habit in human smokers (Kenny and Markou, 2004; Jones and Bonci, 2005; Kalivas and Volkow, 2005; see also Kenny et al, 2003).
Role of NMDA Receptors in the VTA and CeA in Nicotine Self-Administration
The VTA is considered a key anatomical region that regulates nicotine-dependence processes (Corrigall et al, 1994; Kenny et al, 2003; Maskos et al, 2005; David et al, 2006; Ikemoto et al, 2006). On the basis of our observation that NMDA receptor subunit expression was upregulated in the VTA and CeA, we hypothesized that nicotine may act in these two areas to increase NMDA receptor-mediated transmission, and thereby elicit its reinforcing effects. Nicotine increases NMDA receptor-mediated transmission in the VTA of rats (Fu et al, 2000; Grillner and Svensson, 2000; Mansvelder and McGehee, 2000; Schilstrom et al, 2000). Considerably less is known regarding the effects of nicotine in the CeA, although a recent study suggested that nicotine may enhance glutamate-mediated transmission in the mouse amygdala (Barazangi and Role, 2001). Therefore, we examined the effects of nicotine on NMDA receptor-mediated transmission in rat CeA slices. As predicted, nicotine transiently increased NMDA receptor-mediated transmission in the CeA, likely by stimulating nAChRs located on presynaptic glutamate terminals to facilitate glutamate release, subsequently activating postsynaptic NMDA receptors. A drawback to the present studies is that the effects of nicotine on NMDA receptor-mediated currents were assessed only in drug-naive rats, and not in rats with prior experience of nicotine self-administration. Such an assessment may have revealed alterations in the stimulatory actions of nicotine on excitatory glutamate release, or modifications in the response of NMDA receptors to nicotine-enhanced glutamate transmission, which represent important adaptations to nicotine self-administration that contribute to the persistence of this behavior in rats. Nevertheless, consistent with an important role for NMDA receptors in the VTA and CeA in nicotine reinforcement, we found that infusion of LY235959 directly into these brain regions, but not 2 mm above these sites (demonstrating anatomical specificity), dose dependently decreased nicotine self-administration behavior. Importantly, the effects of only a single NMDA receptor antagonist (LY235959), administered systemically or directly into discrete brain regions, were assessed on nicotine-induced lowering of ICSS thresholds and nicotine self-administration. Future studies utilizing different classes of competitive NMDA receptor antagonists will be necessary to confidently attribute the actions of LY235959 reported here solely to an action at NMDA receptors. Further, a caveat to the central administration studies described above is that the effects of infusing LY235959 into the VTA or CeA on responding for a nondrug reinforcer were not assessed. These additional control groups would have increased confidence that NMDA receptors in the VTA or CeA regulate nicotine reinforcement. Finally, it is also important to highlight the possibility, not tested here, that in addition to blocking the rewarding and reward-enhancing effects of nicotine, systemically or centrally administered LY235959 may also diminish the effects of secondary reinforcers such as the cue light paired with each nicotine infusion in the self-administration procedure and thereby decrease nicotine-seeking behaviors (Mead and Stephens, 2003). Taken together, the above observations suggest that cessation of nicotine intake is associated with decreased glutamate-mediated transmission in the CeA and VTA, resulting in compensatory increases in the expression of postsynaptic NMDA receptor subunits, and decreased expression of inhibitory presynaptic mGluII receptors (Liechti et al, 2007). The present data may be interpreted within the framework of nicotine-stimulating nAChRs located on glutamate terminals in the VTA and CeA to increase NMDA receptor-mediated transmission, actions of nicotine that contribute to its constitutive rewarding and reward-enhancing properties that drive nicotine consumption.
As noted above, we observed marked decreases in NMDA receptor subunit expression in the PFC of nicotine self-administering rats, effects opposite in direction to those observed in the CeA and VTA. This observation is consistent with previous reports demonstrating that molecular and neurochemical adaptations in response to nicotine are often opposite in direction in the PFC compared with limbic or basal ganglia sites (Carboni et al, 2000; Konu et al, 2001; Hwang and Li, 2006; Sun et al, 2007). Although not assessed here, it is an interesting possibility that the PFC may regulate nicotine reinforcement similar to the CeA and VTA, as has been shown for other drugs of abuse (Goeders and Smith, 1984; McBride et al, 1999). Consistent with this possibility, another cortical brain region, the insula, has been shown to be important in motivating tobacco consumption and damage to this area can result in cessation of the tobacco-smoking habit in human patients (Naqvi et al, 2007).
Role of AMPA Receptors in Nicotine Reinforcement
AMPA receptors are a subgroup of ionotropic glutamate receptors found at most excitatory synapses, and are considered the primary postsynaptic mediators of glutamate-mediated transmission in the NAcc and other reward-relevant brain regions (Dingledine et al, 1999). We found that the AMPA receptor antagonist NBQX did not alter nicotine self-administration behavior. These data suggest that AMPA receptors are not involved in nicotine reward, an observation consistent with the previous observations that systemic, intra-VTA, or intra-NAcc administration of the closely related AMPA receptor antagonist CNQX did not alter nicotine-induced increases in mesoaccumbens dopamine transmission (Schilstrom et al, 1998; Fu et al, 2000; Sziraki et al, 2002). However, a recent study demonstrated that ZK200775, an AMPA antagonist structurally related to NBQX and CNQX, attenuated nicotine-induced increases in NAcc dopamine release (Kosowski et al, 2004), suggesting a potential role for AMPA receptors in regulating nicotine reinforcement. One explanation for this apparent discrepancy is that ZK200775 may block populations of AMPA receptors distinct from those antagonized by NBQX (Kosowski et al, 2004). Alternatively, ZK200775 is less selective than NBQX for AMPA receptors compared with NMDA receptors (Randle et al, 1992; Kosowski et al, 2004), raising the possibility that the inhibitory actions of ZK200775 on nicotine-evoked NAcc dopamine release may reflect an indirect action at NMDA receptors. It is important to note that the doses of NBQX tested on nicotine self-administration behavior do not induce nonspecific decreases in operant performance (Jackson et al, 1996), but have been shown to precipitate withdrawal in nicotine-dependent rats (Kenny et al, 2003) and decrease responding for ethanol reinforcement (Stephens and Brown, 1999). Thus, these doses of NBQX were likely sufficient to antagonize AMPA receptors in reward circuitries.
Although administration of an AMPA receptor antagonist had no effects on nicotine self-administration, we found that AMPA receptor subunit expression was increased in the CeA and NAcc, and decreased in the PFC of nicotine self-administering rats compared with controls. Similar effects on AMPA subunit expression have been observed in post-mortem brain tissues of human cocaine users (Hemby et al, 2005). Interestingly, Carlezon and colleagues have postulated that AMPA receptor subunit expression in the NAcc may regulate reward sensitivity. Specifically, it was found that virally mediated overexpression of GluR1 subunits in the NAcc elevated ICSS thresholds in rats (Todtenkopf et al, 2006), and that expression of this receptor subunit may be increased during periods of drug withdrawal (Chartoff et al, 2006). Thus, although AMPA receptors are likely not involved in regulating nicotine self-administration based on the present data, it is an interesting possibility that increased NAcc GluR1 expression may represent a compensatory (homeostatic) response in brain reward circuits to repeated exposure to the reward-enhancing effects of nicotine. In addition, considering the important roles of the PFC and CeA in relapse processes (Kalivas and Volkow, 2005; Lu et al, 2007), nicotine-induced adaptations in AMPA receptor subunit expression in these brain regions may also contribute to the persistence of the smoking habit in humans. Future studies in which molecular techniques are utilized to induce regionally specific alterations in NMDA or AMPA receptor subunit expression may enable a more detailed analysis of how each change affects sensitivity to nicotine.
Conclusions
The data presented here suggest that nicotine enhances NMDA receptor-mediated neurotransmission in the VTA and CeA, and that this action of nicotine plays an essential ‘permissive’ role in the reward-enhancing effects of nicotine that may motivate its consumption. Furthermore, analysis of protein expression levels demonstrate that a history of nicotine self-administration induces dramatic plasticity in glutamate-mediated transmission throughout reward-relevant brain regions such as the VTA and CeA, an action that may contribute to the persistence of the drug-taking habit. In addition to highlighting the important role for NMDA receptors located in the VTA in nicotine reinforcement, these data reveal a previously unrecognized role for the CeA in this process. In conclusion, NMDA receptors are central to nicotine reinforcement processes and may therefore prove to be useful therapeutic targets for the treatment of tobacco addiction.
References
Barazangi N, Role LW (2001). Nicotine-induced enhancement of glutamatergic and gabaergic synaptic transmission in the mouse amygdala. J Neurophysiol 86: 463–474.
Barr RS, Pizzagalli DA, Culhane MA, Goff DC, Evins AE (2007). A single dose of nicotine enhances reward responsiveness in nonsmokers: implications for development of dependence. Biol Psychiatry in press.
Bauco P, Wise RA (1994). Potentiation of lateral hypothalamic and midline mesencephalic brain stimulation reinforcement by nicotine: examination of repeated treatment. J Pharmacol Exp Ther 271: 294–301.
Ben-Shahar O, Keeley P, Cook M, Brake W, Joyce M, Nyffeler M et al (2007). Changes in levels of D1, D2, or NMDA receptors during withdrawal from brief or extended daily access to iv cocaine. Brain Res 1131: 220–228.
Brunzell DH, Russell DS, Picciotto MR (2003). In vivo nicotine treatment regulates mesocorticolimbic CREB and ERK signaling in C57BL/6J mice. J Neurochem 84: 1431–1441.
Buisson B, Bertrand D (2002). Nicotine addiction: the possible role of functional upregulation. Trends Pharmacol Sci 23: 130–136.
Carboni E, Bortone L, Giua C, Di Chiara G (2000). Dissociation of physical abstinence signs from changes in extracellular dopamine in the nucleus accumbens and in the prefrontal cortex of nicotine dependent rats. Drug Alcohol Depend 58: 93–102.
Carlezon Jr WA, Wise RA (1993). Phencyclidine-induced potentiation of brain stimulation reward: acute effects are not altered by repeated administration. Psychopharmacology (Berl) 111: 402–408.
Caine SB, Lintz R, Koob GF (1993). Intravenous drug self-administration techniques in animals. In: Sahgal A (ed). Behavioural Neuroscience: A Practical Approach, vol 2. IRL Press: Oxford. pp 117–143.
Chartoff EH, Mague SD, Barhight MF, Smith AM, Carlezon Jr WA (2006). Behavioral and molecular effects of dopamine D1 receptor stimulation during naloxone-precipitated morphine withdrawal. J Neurosci 26: 6450–6457.
Corrigall WA, Coen KM, Adamson KL (1994). Self-administered nicotine activates the mesolimbic dopamine system through the ventral tegmental area. Brain Res 653: 278–284.
Corrigall WA, Franklin KB, Coen KM, Clarke PB (1992). The mesolimbic dopaminergic system is implicated in the reinforcing effects of nicotine. Psychopharmacology (Berl) 107: 285–289.
Cull-Candy S, Brickley S, Farrant M (2001). NMDA receptor subunits: diversity, development and disease. Curr Opin Neurobiol 11: 327–335.
Dani JA, Heinemann S (1996). Molecular and cellular aspects of nicotine abuse. Neuron 16: 905–908.
David V, Besson M, Changeux JP, Granon S, Cazala P (2006). Reinforcing effects of nicotine microinjections into the ventral tegmental area of mice: dependence on cholinergic nicotinic and dopaminergic D1 receptors. Neuropharmacology 50: 1030–1040.
Dingledine R, Borges K, Bowie D, Traynelis SF (1999). The glutamate receptor ion channels. Pharmacol Rev 51: 7–61.
Donny EC, Chaudhri N, Caggiula AR, Evans-Martin FF, Booth S, Gharib MA et al (2003). Operant responding for a visual reinforcer in rats is enhanced by noncontingent nicotine: implications for nicotine self-administration and reinforcement. Psychopharmacology (Berl) 169: 68–76.
Fischer BD, Dykstra LA (2006). Interactions between an N-methyl-D-aspartate antagonist and low-efficacy opioid receptor agonists in assays of schedule-controlled responding and thermal nociception. J Pharmacol Exp Ther 318: 1300–1306.
Fu Y, Matta SG, Gao W, Brower VG, Sharp BM (2000). Systemic nicotine stimulates dopamine release in nucleus accumbens: re-evaluation of the role of N-methyl-D-aspartate receptors in the ventral tegmental area. J Pharmacol Exp Ther 294: 458–465.
Ghasemzadeh MB, Nelson LC, Lu XY, Kalivas PW (1999). Neuroadaptations in ionotropic and metabotropic glutamate receptor MRNA produced by cocaine treatment. J Neurochem 72: 157–165.
Goeders NE, Smith JE (1984). Parameters of intracranial self-administration of cocaine into the medial prefrontal cortex. NIDA Res Monogr 55: 132–137.
Grillner P, Svensson TH (2000). Nicotine-induced excitation of midbrain dopamine neurons in vitro involves ionotropic glutamate receptor activation. Synapse 38: 1–9.
Harrison AA, Gasparini F, Markou A (2002). Nicotine potentiation of brain stimulation reward reversed by DhβE and SCH 23390, but not by eticlopride, LY314582 or MPEP in rats. Psychopharmacology (Berl) 160: 56–66.
Hatton GI, Yang QZ (2002). Synaptic potentials mediated by alpha 7 nicotinic acetylcholine receptors in supraoptic nucleus. J Neurosci 22: 29–37.
Hemby SE, Tang W, Muly EC, Kuhar MJ, Howell L, Mash DC (2005). Cocaine-induced alterations in nucleus accumbens ionotropic glutamate receptor subunits in human and non-human primates. J Neurochem 95: 1785–1793.
Herberg LJ, Rose IC (1989). The effect of MK-801 and other antagonists of NMDA-type glutamate receptors on brain-stimulation reward. Psychopharmacology (Berl) 99: 87–90.
Huston-Lyons D, Kornetsky C (1992). Effects of nicotine on the threshold for rewarding brain stimulation in rats. Pharmacol Biochem Behav 41: 755–759.
Hwang YY, Li MD (2006). Proteins differentially expressed in response to nicotine in five rat brain regions: identification using a 2-DE/MS-based proteomics approach. Proteomics 6: 3138–3153.
Ikemoto S, Qin M, Liu ZH (2006). Primary reinforcing effects of nicotine are triggered from multiple regions both inside and outside the ventral tegmental area. J Neurosci 26: 723–730.
Jackson A, Brown G, Stephens DN (1996). N-methyl-D-aspartate (NMDA) and alpha-amino-3-hydroxy-5-methyl-4-isoxazoleproprionate (AMPA) glutamate-receptor antagonists have different interactions with the discriminative stimuli of abused drugs. Psychopharmacology (Berl) 128: 320–327.
Jacobs EH, Smit AB, de Vries TJ, Schoffelmeer AN (2005). Long-term gene expression in the nucleus accumbens following heroin administration is subregion-specific and depends on the nature of drug administration. Addict Biol 10: 91–100.
Jones S, Bonci A (2005). Synaptic plasticity and drug addiction. Curr Opin Pharmacol 5: 20–25.
Kalivas PW, Volkow ND (2005). The neural basis of addiction: a pathology of motivation and choice. Am J Psychiatry 162: 1403–1413.
Kenny PJ (2007). Brain reward systems and compulsive drug use. Trends Pharmacol Sci 28: 135–141.
Kenny PJ, Gasparini F, Markou A (2003). Group II metabotropic and alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionate (AMPA)/kainate glutamate receptors regulate the deficit in brain reward function associated with nicotine withdrawal in rats. J Pharmacol Exp Ther 306: 1068–1076.
Kenny PJ, Markou A (2004). The ups and downs of addiction: role of metabotropic glutamate receptors. Trends Pharmacol Sci 25: 265–272.
Kenny PJ, Markou A (2006). Nicotine self-administration acutely activates brain reward systems and induces a long-lasting increase in reward sensitivity. Neuropsychopharmacology 31: 1203–1211.
Kimmel HL, Ginsburg BC, Howell LL (2005). Changes in extracellular dopamine during cocaine self-administration in squirrel monkeys. Synapse 56: 129–134.
Konu O, Kane JK, Barrett T, Vawter MP, Chang R, Ma JZ et al (2001). Region-specific transcriptional response to chronic nicotine in rat brain. Brain Res 909: 194–203.
Koob GF, Le HT, Creese I (1987). The D1 dopamine receptor antagonist SCH 23390 increases cocaine self-administration in the rat. Neurosci Lett 79: 315–320.
Kornetsky C, Esposito RU (1979). Euphorigenic drugs: effects on the reward pathways of the brain. Fed Proc 38: 2473–2476.
Kosowski AR, Cebers G, Cebere A, Swanhagen AC, Liljequist S (2004). Nicotine-induced dopamine release in the nucleus accumbens is inhibited by the novel AMPA antagonist ZK200775 and the NMDA antagonist CGP39551. Psychopharmacology (Berl) 175: 114–123.
Lambe EK, Picciotto MR, Aghajanian GK (2003). Nicotine induces glutamate release from thalamocortical terminals in prefrontal cortex. Neuropsychopharmacology 28: 216–225.
Lau CG, Zukin RS (2007). NMDA receptor trafficking in synaptic plasticity and neuropsychiatric disorders. Nat Rev Neurosci 8: 413–426.
Laviolette SR, Alexson TO, van der Kooy D (2002). Lesions of the tegmental pedunculopontine nucleus block the rewarding effects and reveal the aversive effects of nicotine in the ventral tegmental area. J Neurosci 22: 8653–8660.
Laviolette SR, van der Kooy D (2003). The motivational valence of nicotine in the rat ventral tegmental area is switched from rewarding to aversive following blockade of the alpha7-subunit-containing nicotinic acetylcholine receptor. Psychopharmacology (Berl) 166: 306–313.
Lecca D, Cacciapaglia F, Valentini V, Acquas E, Di Chiara G (2007). Differential neurochemical and behavioral adaptation to cocaine after response contingent and noncontingent exposure in the rat. Psychopharmacology (Berl) 191: 653–667.
Liechti ME, Lhuillier L, Kaupmann K, Markou A (2007). Metabotropic glutamate 2/3 receptors in the ventral tegmental area and the nucleus accumbens shell are involved in behaviors relating to nicotine dependence. J Neurosci 27: 9077–9085.
Lu L, Dempsey J, Shaham Y, Hope BT (2005). Differential long-term neuroadaptations of glutamate receptors in the basolateral and central amygdala after withdrawal from cocaine self-administration in rats. J Neurochem 94: 161–168.
Lu L, Grimm JW, Shaham Y, Hope BT (2003). Molecular neuroadaptations in the accumbens and ventral tegmental area during the first 90 days of forced abstinence from cocaine self-administration in rats. J Neurochem 85: 1604–1613.
Lu L, Uejima JL, Gray SM, Bossert JM, Shaham Y (2007). Systemic and central amygdala injections of the mGluR(2/3) agonist LY379268 attenuate the expression of incubation of cocaine craving. Biol Psychiatry 61: 591–598.
Mansvelder HD, McGehee DS (2000). Long-term potentiation of excitatory inputs to brain reward areas by nicotine. Neuron 27: 349–357.
Mark GP, Hajnal A, Kinney AE, Keys AS (1999). Self-administration of cocaine increases the release of acetylcholine to a greater extent than response-independent cocaine in the nucleus accumbens of rats. Psychopharmacology (Berl) 143: 47–53.
Markou A, Koob GF (1992). Construct validity of a self-stimulation threshold paradigm: effects of reward and performance manipulations. Physiol Behav 51: 111–119.
Maskos U, Molles BE, Pons S, Besson M, Guiard BP, Guilloux JP et al (2005). Nicotine reinforcement and cognition restored by targeted expression of nicotinic receptors. Nature 436: 103–107.
McBride WJ, Murphy JM, Ikemoto S (1999). Localization of brain reinforcement mechanisms: intracranial self-administration and intracranial place-conditioning studies. Behav Brain Res 101: 129–152.
Mead AN, Stephens DN (2003). Selective disruption of stimulus-reward learning in glutamate receptor gria1 knock-out mice. J Neurosci 23: 1041–1048.
Naqvi NH, Rudrauf D, Damasio H, Bechara A (2007). Damage to the insula disrupts addiction to cigarette smoking. Science 315: 531–534.
Ornstein PL, Arnold MB, Augenstein NK, Deeter JB, Leander JD, Lodge D et al (1993). Unusual stereochemical preferences of decahydroisoquinoline-3-carboxylic acid competitive NMDA antagonists. Bioorg Med Chem Lett 3: 2067–2072.
Ortiz J, Fitzgerald LW, Charlton M, Lane S, Trevisan L, Guitart X et al (1995). Biochemical actions of chronic ethanol exposure in the mesolimbic dopamine system. Synapse 21: 289–298.
Pagliusi SR, Tessari M, DeVevey S, Chiamulera C, Pich EM (1996). The reinforcing properties of nicotine are associated with a specific patterning of c-fos expression in the rat brain. Eur J Neurosci 8: 2247–2256.
Paterson NE, Balfour DJ, Markou A (2008). Chronic bupropion partially attenuated the reinforcement-enhancing, but not the reinforcing, effects of self-administered nicotine and enhanced the motivational properties of a nicotine-associated conditioned stimulus in rats. Nicotine Tob Res in press.
Paxinos G, Watson CH (eds) (1986). The Rat Brain Atlas in Stereotaxic Coordinates. Academic Press: London.
Pellegrino LJ, Pellegrino AS, Cushman AJ (eds) (1979). A Stereotaxic Atlas of the Rat Brain. Plenum Press: New York.
Pich EM, Pagliusi SR, Tessari M, Talabot-Ayer D, Hooft van Huijsduijnen R, Chiamulera C (1997). Common neural substrates for the addictive properties of nicotine and cocaine. Science 275: 83–86.
Prince HK, Conn PJ, Blackstone CD, Huganir RL, Levey AI (1995). Down-regulation of AMPA receptor subunit GluR2 in amygdaloid kindling. J Neurochem 64: 462–465.
Randle JC, Guet T, Cordi A, Lepagnol JM (1992). Competitive inhibition by NBQX of kainate/AMPA receptor currents and excitatory synaptic potentials: importance of 6-nitro substitution. Eur J Pharmacol 215: 237–244.
Rice ME, Cragg SJ (2004). Nicotine amplifies reward-related dopamine signals in striatum. Nat Neurosci 7: 583–584.
Roberto M, Bajo M, Crawford E, Madamba SG, Siggins GR (2006). Chronic ethanol exposure and protracted abstinence alter NMDA receptors in central amygdala. Neuropsychopharmacology 31: 988–996.
Roberto M, Madamba SG, Stouffer DG, Parsons LH, Siggins GR (2004). Increased GABA release in the central amygdala of ethanol-dependent rats. J Neurosci 24: 10159–10166.
Schilstrom B, Fagerquist MV, Zhang X, Hertel P, Panagis G, Nomikos GG et al (2000). Putative role of presynaptic alpha7* nicotinic receptors in nicotine stimulated increases of extracellular levels of glutamate and aspartate in the ventral tegmental area. Synapse 38: 375–383.
Schilstrom B, Nomikos GG, Nisell M, Hertel P, Svensson TH (1998). N-methyl-D-aspartate receptor antagonism in the ventral tegmental area diminishes the systemic nicotine-induced dopamine release in the nucleus accumbens. Neuroscience 82: 781–789.
Schoepp DD, Ornstein PL, Salhoff CR, Leander JD (1991). Neuroprotectant effects of LY274614, a structurally novel systemically active competitive NMDA receptor antagonist. J Neural Transm Gen Sect 85: 131–143.
Stefanski R, Ladenheim B, Lee SH, Cadet JL, Goldberg SR (1999). Neuroadaptations in the dopaminergic system after active self-administration but not after passive administration of methamphetamine. Eur J Pharmacol 371: 123–135.
Stephens DN, Brown G (1999). Disruption of operant oral self-administration of ethanol, sucrose, and saccharin by the AMPA/kainate antagonist, NBQX, but not the AMPA antagonist, GYKI 52466. Alcohol Clin Exp Res 23: 1914–1920.
Sun D, Huang W, Hwang YY, Zhang Y, Zhang Q, Li MD (2007). Regulation by nicotine of Gpr51 and Ntrk2 expression in various rat brain regions. Neuropsychopharmacology 32: 110–116.
Sziraki I, Sershen H, Hashim A, Lajtha A (2002). Receptors in the ventral tegmental area mediating nicotine-induced dopamine release in the nucleus accumbens. Neurochem Res 27: 253–261.
Tang WX, Fasulo WH, Mash DC, Hemby SE (2003). Molecular profiling of midbrain dopamine regions in cocaine overdose victims. J Neurochem 85: 911–924.
Todtenkopf MS, Parsegian A, Naydenov A, Neve RL, Konradi C, Carlezon Jr WA (2006). Brain reward regulated by AMPA receptor subunits in nucleus accumbens shell. J Neurosci 26: 11665–11669.
Turchan J, Maj M, Przewlocka B (2003). The effect of drugs of abuse on NMDAR1 receptor expression in the rat limbic system. Drug Alcohol Depend 72: 193–196.
Valjent E, Pages C, Herve D, Girault JA, Caboche J (2004). Addictive and non-addictive drugs induce distinct and specific patterns of ERK activation in mouse brain. Eur J Neurosci 19: 1826–1836.
Wang F, Chen H, Steketee JD, Sharp BM (2007). Upregulation of ionotropic glutamate receptor subunits within specific mesocorticolimbic regions during chronic nicotine self-administration. Neuropsychopharmacology 32: 103–109.
Wilson JM, Nobrega JN, Corrigall WA, Coen KM, Shannak K, Kish SJ (1994). Amygdala dopamine levels are markedly elevated after self- but not passive-administration of cocaine. Brain Res 668: 39–45.
Yokel RA, Wise RA (1975). Increased lever pressing for amphetamine after pimozide in rats: implications for a dopamine theory of reward. Science 187: 547–549.
Acknowledgements
This study was supported by the National Institute on Drug Abuse (DA20686 to PJK; DA12736 to WC; and DA11946 to AM), and the James and Esther King Biomedical Research Program, Florida Department of Health (07KN-06 to PJK). We thank Mrs Gina Stouffer and Ms Nurith Amitai for technical assistance and Mr Mike Arends for editorial assistance. This is publication 16208 from The Scripps Research Institute.
Author information
Authors and Affiliations
Corresponding authors
Additional information
DISCLOSURE
Over the past 3 years, William Carlezon has received compensation from HUYA Biosciences, Infinity Pharmaceuticals, Myneurolab.com, and Psychogenics. He holds several patents and patent applications that are not related to the work described in this report. Athina Markou received an honorarium from Abbott during the past 3 years, and research contract support from Lundbeck and Intracellular Therapeutics. Athina Markou and Paul Kenny hold a patent on the role of metabotropic glutamate receptors in drug dependence. There are no personal financial holdings that may be perceived as constituting a potential conflict of interest.
Rights and permissions
About this article
Cite this article
Kenny, P., Chartoff, E., Roberto, M. et al. NMDA Receptors Regulate Nicotine-Enhanced Brain Reward Function and Intravenous Nicotine Self-Administration: Role of the Ventral Tegmental Area and Central Nucleus of the Amygdala. Neuropsychopharmacol 34, 266–281 (2009). https://doi.org/10.1038/npp.2008.58
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2008.58
Keywords
This article is cited by
-
Multimodal 7T imaging reveals enhanced functional coupling between salience and frontoparietal networks in young adult tobacco cigarette smokers
Brain Imaging and Behavior (2024)
-
Altered neuronal activity in the ventromedial prefrontal cortex drives nicotine intake escalation
Neuropsychopharmacology (2023)
-
Investigating the effects of chronic perinatal alcohol and combined nicotine and alcohol exposure on dopaminergic and non-dopaminergic neurons in the VTA
Scientific Reports (2021)
-
Do Hallucinogens Have a Role in the Treatment of Addictions? A Review of the Current Literature
SN Comprehensive Clinical Medicine (2021)
-
Investigating the influence of perinatal nicotine exposure on genetic profiles of neurons in the sub-regions of the VTA
Scientific Reports (2020)