Abstract
Background:
Spontaneous movement abnormalities, occurring independent of medication status, are thought to reflect basal ganglia pathology in patients at ultrahigh risk (UHR) for psychosis. To date, the research literature has primarily focused on movements associated with elevated striatal dopamine (i.e., hyperkinesia) while little is known about motor symptoms associated with low levels of subcortical dopamine (i.e., spontaneous parkinsonisms; SPs). As SPs (e.g., bradykinesia) may be governed by distinct neural mechanisms, this line of research can provide a clearer picture of the etiological processes in the prodrome.
Aims:
To examine SPs and striatal structural correlates in youth at risk for psychosis.
Methods:
A total of 81 (35 UHR, 46 healthy controls) adolescents were administered a structured clinical interview, structural MRI scan, and handwriting kinematic analysis capable of assessing SPs that are not detectable by traditional observer-based inventories.
Results:
The UHR group exhibited significant decreased velocity scaling (indicative of SPs), t(79)=−2.65, P⩽0.01, as well as decreased ipsilateral t(68)=−3.16, P⩽0.001 and contralateral t(68)=−3.32, P⩽0.001 putamen volume compared with the healthy control group. Further, decreased velocity scaling was significantly associated with smaller ipsilateral putamen r(68)=0.23, P⩽0.05, 95% confidence interval (CI) (−0.005, 0.44), left r(68)=0.23, P⩽0.05, 95% CI (−0.005, 0.44) and right r(68)=0.21, P⩽0.05, 95% CI (−0.03, 0.42) caudate volume, as well as increased positive r(79)=−0.20, P=0.05, 95% CI (−0.40, −0.02) and negative r(79)=−0.27, P⩽0.05, 95% CI (−0.46, −0.06) symptoms across the sample.
Conclusions:
These findings represent the first evidence for hypokinetic movement abnormalities in the UHR period, indicating that pathophysiological processes in UHR patients may also involve hypodopaminergia. The results implicate a dopamine-induced imbalance contributing to frontal–subcortical circuit dysfunction in the psychosis prodrome.
Similar content being viewed by others
Introduction
Current etiological theories suggest that early vulnerabilities interact with later neurodevelopmental abnormalities and environmental stressors (e.g., drug use, interpersonal stress) during adolescence, eventually leading to the development of psychosis.1 One such early marker of neurodevelopmental abnormalities, motor impairment, precedes the onset of psychosis,2,3 and may yield novel biomarkers and also significantly inform etiological conceptions of psychosis.
The period preceding the onset of psychosis is marked by attenuated psychotic symptoms in both positive and negative domains and a decline in functioning.4 During this period, individuals at ultrahigh risk (UHR) for psychosis show gray matter abnormalities related to striatal motor regions.5 Investigating neural structures and related motor behavior poses an opportunity to understand the biological mechanisms and a potentially clearer view of core features of the disorder because many of the third variable confounds in studies of patients with psychosis (i.e., long term medication use, drug and alcohol abuse, chronic illness) are not as prevalent. Indeed, studying neuroleptic free individuals at risk for the disorder can be an important point of intervention because as many as 35% of individuals assessed as at risk will go on to develop psychosis within 2 years.6
Spontaneous movement abnormalities (SMAs) have been observed in patients with psychosis in terms of dyskinesia (withering, jerking movements in the face and upper extremities), as well as those associated with Parkinson’s disease such as bradykinesia (slowing of the velocity of movements).7 Prospective and cross-sectional studies suggest that dyskinesia are related to UHR symptoms, biological markers of risk for psychosis, and are predictive of future conversion to a psychotic disorder.3,5,8–10 Archival and prospective studies have focused entirely on dyskinesia in UHR individuals because this motor symptom is thought to be related to the abnormally elevated dopamine (DA) processes that underlie the development of positive symptoms. However, a recent systematic review describes dyskinesia and spontaneous parkinsonisms (SPs) occurring at the onset of the illness, independent from medication, and may constitute a constellation of core movement abnormalities in psychosis.7 Importantly, to our knowledge there have been no published investigations examining SPs during the UHR period. In patients with chronic schizophrenia, SPs are linked to a poorer prognosis for the illness, more severe SMAs due to medication, and increased time to remission.11–15 Innovative etiological theories suggest that the DA theory of psychosis is more complex than previously conceived16—a DA imbalance involving both elevated as well as deficit DA states is likely involved7,17,18—and exploring SPs is a potentially valuable point of understanding the motor signs associated with hypodopaminergia.
There are drawbacks to using traditional observer-based methods of measuring SMAs (i.e, long training times to establish reliability) and investigators have suggested that these methods may provide underestimates of the prevalence of SMAs in patients with psychosis.7,11 Innovative developments in instrumental measures of movement using force transducers and portable computerized tablets to capture handwriting samples have improved upon these drawbacks.13 Previous studies using instrumental procedures to quantify SPs have used a measure called velocity scaling (VS), which is defined as the ability to increase movement velocity with increases in target distances.14,19 In healthy individuals, peak velocities nearly double for similar increases in distance, whereas in patients with drug-induced parkinsonism, peak velocities stay generally the same for increased distances. Lower values of VS are a proximal measure of bradykinesia and reflect a decreased ability to coordinate agonist and antagonist muscles during movement, resulting in slower movements.13 This line of research is promising because the sensitivity of handwriting analysis may allow for the detection of subtle movement abnormalities that have not yet reached the severity seen in formal psychosis.
The striatum (i.e., caudate and putamen) is important in etiological conceptions of psychotic symptoms, as the structure represents the entry point for frontal–subcortical communication. More specifically, as cortico–striatal–pallido–thalamic–cortico circuits are thought to be responsible for mediating motor, affective, emotional, motivational, and cognitive behavior,20,21 understanding dysfunction in these circuits may help to improve understanding of why psychotic disorders involve such a heterogeneous series of symptomatology. As SMAs provide an in-depth and readily observable marker of aberrant neural transmission within these frontal–subcortical circuits,16,22,23 understanding the related motor behaviors holds significant promise for elucidating etiological processes and enhancing early identification. This is particularly relevant for UHR patients, who exhibit altered DA metabolic processes in the striatum,22 dyskinetic movements,10 and a wide range of positive and negative symptomatology, but have no known biomarker for hypodopaminergic states.
In this study, 81 (35 UHR, 46 controls) adolescent participants completed clinical interviews, a computerized handwriting task to determine if SPs are present, and structural magnetic resonance imaging (MRI) to assess any related symptom and striatal structure correlates. A proximal measure for bradykinesia, VS, was calculated by extracting kinematic measures of handwriting. We predicted that the UHR group would show a decreased ability to scale pen velocity, resulting in a lower value of VS than healthy controls. Second, we hypothesized that impaired VS would be related to elevated symptoms of risk for psychosis. Finally, on the basis of the literature suggesting that the putamen is a primary motor nucleus,23 we predicted that the impaired VS would be associates with decreased volume in the putamen but not the caudate.
Materials and methods
Participants
Adolescent UHR and healthy control participants (mean age=18.57, s.d.=2.36) were recruited at the University of Colorado Boulder’s Adolescent Development and Preventive Treatment research program. Importantly, all of the participants were not currently taking antipsychotic medication during the handwriting task and MRI scan. The University of Colorado Boulder Institutional Review Board approved the protocol and informed consent procedures. See Supplementary Material 1 for recruitment and exclusion criteria of the participants.
Clinical interviews
The Structured Interview for Prodromal Syndromes was used to diagnose a prodromal syndrome and the Structured Clinical Interview for Axis-I DSM-IV Disorders24 was administered to rule out a psychotic disorder diagnosis. See Supplementary Material 2 for additional clinical interview information.
Handwriting
Handwriting samples were obtained to compute a measure of VS. Lower values of VS, reflecting the slowing or inability to increase pen movement velocity across shorter and longer target distances, have been found in Parkinson’s patients and schizophrenia patients treated with neuroleptic medication.12 Handwriting samples for each participant were acquired using Neuroscript MoveAlyzer software (http://www.neuroscript.net) installed on a Fujitsu Lifebook T901 tablet computer with a non-inking pen. Participants were instructed to write eight loops continuously for three trials within a 2–4 cm vertical boundary with their dominant hand (see Figure 1). Handedness was determined using the Neurologic Evaluation Scale.25 Each trial consisted of 16 vertical strokes, which were segmented and processed for target variables: peak vertical velocity and absolute size of stroke. Valid trials included at least 10 segments. Target variables were extracted from MoveAlyzer and imported into SPSS (Armonk, NY, USA); a measure of VS was calculated for each participant using the regression method developed by Caligiuri et al.12 A regression with peak vertical velocity as the predicted variable was entered along with absolute size of the stroke (to account for variance of individual stroke sizes) and condition (2 and 4 cm) as covariates. A slope coefficient for condition was saved and used as the measure of VS in subsequent analyses.
Structural image processing
Structural MRI scans were acquired on a Siemens 3-Tesla Magnetom TIM Trio MRI scanner (Siemens AG, Munich, Germany) with a 12-channel head coil. See Supplementary Material 3 for the parameters used in the structural image processing. Striatal target structures, consisting of the left and right putamen and caudate, were segmented from the MPRAGE using the FreeSurfer suite of automated tools (see Figure 2).26 FreeSurfer calculates values for each participant’s total intracranial volume (whole-brain gray matter+white matter+cerebrospinal fluid), and each structure’s volume was divided by the total intracranial volume to control for whole-brain volume. Because the sample included left and right-handed participants, the left and right putamen volumes were assigned to the ipsilateral or contralateral side of the participant’s dominant hand. See Supplementary Material 4 for additional information about the structural data processing stream.
Additional statistical analysis
Independent t-tests and chi-square tests were employed to examine the differences between groups in continuous and categorical demographic variables, respectively. On the basis of previous work showing that decreased VS occurs in patients with Parkinson’s disease and schizophrenia patients following the treatment with neuroleptics,12,13,15 as well as work showing that movement abnormalities are linked to decreased striatal volume in UHR individuals,5 we used one-tailed independent t-tests to assess for group differences in VS and striatal regions of interest. Furthermore, one-tailed bivariate correlations were used to examine predicted relationships between lower VS and increased Structured Interview for Prodromal Syndromes symptom domains and striatal morphology. Correlations were first run with the entire sample and then in the UHR group alone.
Results
Participants
There were no significant differences between groups on demographic characteristics including age t(78.94)=1.43, education t(79)=0.83, gender χ2(1, N=81)=1.33, parental education t(78)=1.00, and handedness χ2(1, N=81)=0.17. As expected, UHR participants were rated significantly higher than controls on both Structured Interview for Prodromal Syndromes symptom domains positive t(40.01)=14.47, P⩽0.001 and negative t(34.78)=8.16, P⩽0.001 (see Table 1 for information about the participants).
Velocity scaling and relationship to symptoms
The UHR group showed a significantly lower VS than healthy controls, t(79)=−2.65, P⩽0.01 (see Table 1). Across the entire sample, lower VS was related to elevated positive symptoms r(79)=−0.20, P=0.05, 95% confidence interval (CI) (−0.40, −0.02) and with more severe negative symptoms r(79)=−0.27, P⩽0.05, 95% CI (−0.46, −0.06). Within the UHR group alone, there was not a relationship for VS with elevated positive symptoms r(33)=0.12, P=0.24, 95% CI (−0.22, 0.44); whereas in the predicted direction, the relationship of lower VS and more severe negative symptoms was not significant r(33)=−0.12, P=0.24, 95% CI (−0.44, 0.22).
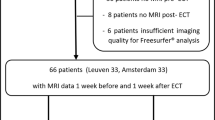
Striatal volumes and relationship to velocity scaling
The total sample size available for the measurement of striatal volumes includes 70 participants (n=33 UHR, 37 controls). The UHR group showed smaller ipsilateral (t(68)=−3.16, P⩽0.001) and contralateral (t(68)=−3.32, P⩽0.001) putamen volumes compared with the healthy controls. There were no group differences for either the left or right caudate (both P values ⩾0.3; see Table 2). Bivariate correlations showed that across the entire sample, lower VS was significantly associated with smaller ipsilateral putamen volume r(68)=0.23, P⩽0.05, 95% CI (−0.005, 0.44) and smaller contralateral putamen volume at trend level r(68)=0.15, P=0.1, 95% CI (−0.09, 0.37). Within the UHR group, there was no significant relationship with VS and ipsilateral or contralateral putamen (all P values ⩾0.2). Across the entire sample, smaller left r(68)=0.23, P⩽0.05, 95% CI (−0.005, 0.44) and right r(68)=0.21, P⩽0.05, 95% CI (−0.03, 0.42) caudate volumes were significantly related to lower VS. Within the UHR group, there was a trend level relationship with the left caudate volume and impaired VS r(31)=0.28, P=0.06, 95% CI (−0.07, 0.57) and a significant relationship between smaller right caudate volume and impaired VS r(31)=0.30, P⩽0.05, 95% CI (−0.05, 0.58).
Discussion
Main findings
The presenting findings, showing elevated SPs in UHR individuals, represent the first empirical evidence to suggest that hypodopaminergic function is also present in the psychosis prodrome. Given the related previous literature that has primarily focused on elevated striatal DA in this group,3,22 the present results add an important new perspective indicating that a DA imbalance model13,14,17 may also be relevant for understanding pathogenic processes driving the UHR period. Significant associations between elevated SPs and both decreased striatal morphology and increased positive and negative symptomatology support the notion that hypokinetic movements are closely tied to the pathophysiology of psychosis.7,13,27
Interpretation of findings in relationship to previously published work
It is well known that individuals who later develop schizophrenia show subtle movement abnormalities before the onset of illness.3,28–30 Research using observer ratings show that movement abnormalities, closely linked to basal ganglia function, could successfully classify UHR individuals likely to convert to psychosis.3 The findings that UHR individuals also show impaired VS is consistent with a review by Pappa and Dazzan7 that found a sizeable prevalence of bradykinesia in neuroleptic naive first-episode psychosis patients. Importantly, this is the second study to utilize MoveAlyzer in a UHR sample, suggesting that the software is capable of detecting more subtle or subthreshold movement abnormalities, including dyskinesia and SPs, in neuroleptic free UHR individuals.31 Previous research has suggested that handwriting analysis can detect a higher proportion of movement abnormalities than standard observer-based ratings,11 but medication side effects may confound analysis of movement abnormalities.13,14 Because the UHR individuals may not be experiencing abnormal neural processes or medication side effects to the extent of an individual with Parkinson’s disease or chronic schizophrenia, instrumental measures are excellent for detecting more subtle SMAs.
The present study found overlap with lower VS and both positive and negative symptom domains. Previous work in schizophrenia patients has found differing relationships to psychopathology. Investigators have noted a possible link between SPs and negative symptoms;32,33 however, other researchers have not found a relationship between SPs and positive or negative symptoms in patients with psychosis.27 The findings suggest that VS is related to both symptoms of risk for psychosis; however, the lack of a within-UHR-group relationship speaks to the complexity of looking at subtle movement abnormalities and symptom domains. These results may point towards the heterogeneity of movement abnormalities and symptom presentation in psychosis. The prevalence of SPs in neuroleptic naive first-episode psychosis patients ranges from 2.3 to 27%,7 suggesting that patient populations and method of examination of movement abnormalities are important considerations. These results may also suggest an issue with power, and it will be important to see replication in a study with a considerably larger sample. In addition, recent work suggests that movement abnormalities may cluster with several nonspecific negative and motor symptoms.34 Although outside the scope of the current study, future work should explore how SMAs cluster within symptoms domains to give a fuller picture of this complex issue.
Movement abnormalities associated with schizophrenia and Parkinson’s disease have predominantly been associated with basal ganglia dysfunction.7,35–37 Previous work has noted that UHR individuals show putamen brain volume reduction before the onset of psychosis.5,38 Consistent with previous work, the UHR individuals only showed reduced volume in the putamen, suggesting that there may be specific structural differences within the motor striatum related to risk for psychosis. The finding that caudate volumes did not differ between UHR and healthy controls is consistent with other investigations.39 The results of the striatal morphology analysis suggest that smaller volume in both putamen and caudate are related to lower VS performance. It is interesting that the caudate, usually considered to be more involved with cognitive processes related to reward and memory,23 is involved in impaired VS. This may reflect an impairment of spatial memory processes in the UHR group. In addition, the caudate contributes to executive function through a fronto–striatal circuit with specific connectivity to the dorsolateral prefrontal cortex.21 It is well known that UHR individuals show cognitive impairments, and future research should examine whether impairment in specific cognitive domains mediates performance on the handwriting task.
Strengths and limitation of this study
The current study holds several noteworthy strengths as well as some limitations. First, while previous studies exploring SMAs and structural MRI have included UHR samples of similar sizes,5 limited statistical power may have hampered our ability to detect potential relationships between VS and associated brain regions within the UHR group. However, the approach to examine motor behavior, brain volumes, and symptoms across the sample is a valid strategy as the variables of interest are continuous in nature; this approach has been utilized in related high-impact investigations.8 Second, although the inclusion of antipsychotic-free participants was an important component of the present study (given the well-documented relationship between neuroleptics and subcortical motor function40), the present study only examined a proximal marker of SPs—bradykinesia. Although bradykinesia is a cardinal SP symptom, other related phenomena involving tremor, posture, and rigidity were not assessed, and may also have a role in the UHR period. Future investigations including a broader array of motor assessments for UHR participants are highly warranted. Finally, given the relationships between SPs and the caudate, it is possible that the present motor assessment strategy may also be drawing upon other cognitive processes.23
Implications for Future Research, policy, and practice
The current study implicates striatal abnormalities in SPs, which are thought to reflect abnormal dopaminergic processes. Innovative theories of psychosis that challenge the traditional view of the disorder being solely related to increased striatal DA suggest that there may be abnormalities in the modulation of homeostatic regulation of DA, which might help explain why movement abnormalities associated with both hyperdopaminergic (dyskinesia) and hypodopaminergic (SPs) are seen in UHR participants.7,9,18,22,41 Future research examining these dynamic dopaminergic processes and SMAs by more direct imaging methods (e.g., resting state functional connectivity, PET) is sorely needed to understand the biological mechanisms underlying the etiology of psychosis.
Conclusions
The current study found that UHR individuals show a decreased ability to scale movement velocity during an innovative handwriting task and this movement abnormality was related to decreased striatal volume. These findings expand the current understanding of SMAs as vulnerability markers of aberrant neurodevelopment related to psychosis, and specifically highlight that SPs occur before the onset of the illness. It remains to be determined whether SPs are a part of the progression of the UHR syndrome. Future longitudinal research exploring the relationship of SPs to worsening symptoms or conversion status could bolster the notion that this subset of movement abnormalities is related to the pathophysiology of psychosis.
References
Walker E, Mittal V, Tessner K . Stress and the hypothalamic pituitary adrenal axis in the developmental course of schizophrenia. Annu Rev Clin Psychol 2008; 4: 189–216.
Mittal VA, Walker EF . Movement abnormalities predict conversion to Axis I psychosis among prodromal adolescents. J Abnorm Psychol 2007; 116: 796–803.
Mittal VA, Walker EF, Bearden CE, Walder DJ, Trottman HD, Daley M et al. Markers of basal ganglia dysfunction and conversion to psychosis: neurocognitive deficits and dyskinesias in the prodromal period. Biol Psychiatry 2010; 68: 93–99.
Yung AR, Phillips LJ, Yuen HP, McGorry PD . Risk factors for psychosis in an ultra high-risk group: psychopathology and clinical features. Schizophr Res 2004; 67: 131–142.
Mittal VA, Daley M, Shiode MF, Bearden CE, O'Neill J, Cannon TD . Striatal volumes and dyskinetic movements in youth at high-risk for psychosis. Schizophr Res 2010; 123: 68–70.
Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry 2012; 69: 220–229.
Pappa S, Dazzan P . Spontaneous movement disorders in antipsychotic-naive patients with first-episode psychoses: a systematic review. Psychol Med 2009; 39: 1065–1076.
Mittal VA, Neumann C, Saczawa M, Walker EF . Longitudinal progression of movement abnormalities in relation to psychotic symptoms in adolescents at high risk of schizophrenia. Arch Gen Psychiatry 2008; 65: 165–171.
Mittal VA, Tessner KD, Trottman HD, Esterberg M, Dhrub SH, Simeonova DI et al. Movement abnormalities and the progression of prodromal symptomatology in adolescents at risk for psychotic disorders. J Abnorm Psychol 2007; 116: 260–267.
Mittal VA, Dean DJ, Pelletier A, Caligiuri M . Associations between spontaneous movement abnormalities and psychotic-like experiences in the general population. Schizophr Res 2011; 132: 194–196.
Cortese L, Caligiuri MP, Malla AK, Manchanda R, Takhar J, Haricharan R . Relationship of neuromotor disturbances to psychosis symptoms in first-episode neuroleptic-naive schizophrenia patients. Schizophr Res 2005; 75: 65–75.
Caligiuri MP, Teulings HL, Filoteo JV, Song D, Lohr JB . Quantitative measurement of handwriting in the assessment of drug-induced parkinsonism. Hum Mov Sci 2006; 25: 510–522.
Caligiuri MP, Teulings HL, Dean CE, Niculescu AB, Lohr JB . Handwriting movement kinematics for quantifying extrapyramidal side effects in patients treated with atypical antipsychotics. Psychiatry Res 2010; 177: 77–83.
Caligiuri MP, Teulings HL, Dean CE, Niculescu AB, Lohr J . Handwriting movement analyses for monitoring drug-induced motor side effects in schizophrenia patients treated with risperidone. Hum Mov Sci 2009; 28: 633–642.
Caligiuri MP, Lohr JB, Ruck RK . Scaling of movement velocity: a measure of neuromotor retardation in individuals with psychopathology. Psychophysiology 1998; 35: 431–437.
Howes OD, Kapur S . The dopamine hypothesis of schizophrenia: version III—the final common pathway. Schizophr Bull 2009; 35: 549–562.
Mehler-Wex C, Riederer P, Gerlach M . Dopaminergic dysbalance in distinct basal ganglia neurocircuits: implications for the pathophysiology of Parkinson's disease, schizophrenia and attention deficit hyperactivity disorder. Neurotox Res 2006; 10: 167–179.
Grace AA . Phasic versus tonic dopamine release and the modulation of dopamine system responsivity: a hypothesis for the etiology of schizophrenia. Neuroscience 1991; 41: 1–24.
Koning JP, Kahn RS, Tenback DE, van Schelven LJ, van Harten PN . Movement disorders in nonpsychotic siblings of patients with nonaffective psychosis. Psychiatry Res 2011; 188: 133–137.
Bradshaw JL, Sheppard DM . The neurodevelopmental frontostriatal disorders: evolutionary adaptiveness and anomalous lateralization. Brain Lang 2000; 73: 297–320.
Lichter DG, Cummings JL . Frontal-Subcortical Circuits in Psychiatric and Neurological Disorders. Guilford Press, 2001.
Howes OD, Montgomery AJ, Asselin MC, Murray RM, Valli I, Tabraham P et al. Elevated striatal dopamine function linked to prodromal signs of schizophrenia. Arch Gen Psychiatry 2009; 66: 13–20.
Grahn JA, Parkinson JA, Owen AM . The cognitive functions of the caudate nucleus. Prog Neurobiol 2008; 86: 141–155.
First MB, Spitzer RL, Gibbon M, Williams JBW . Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute, 2002.
Buchanan RW, Heinrichs DW . The Neurological Evaluation Scale (NES): a structured instrument for the assessment of neurological signs in schizophrenia. Psychiatry Res 1989; 27: 335–350.
Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 2002; 33: 341–355.
McCreadie RG, Srinivasan TN, Padmavati R, Thara R . Extrapyramidal symptoms in unmedicated schizophrenia. J Psychiatr Res 2005; 39: 261–266.
Mittal VA, Jalbrzikowski M, Daley M, Roman C, Bearden CE, Cannon TD . Abnormal movements are associated with poor psychosocial functioning in adolescents at high risk for psychosis. Schizophr Res 2011; 130: 164–169.
Walker EF, Diforio D . Schizophrenia: a neural diathesis-stress model. Psychol Rev 1997; 104: 667–685.
Walker EF, Savoie T, Davis D . Neuromotor precursors of schizophrenia. Schizophr Bull 1994; 20: 441–451.
Dean DJ, Teulings HL, Caligiuri M, Mittal VA . Handwriting analysis indicates spontaneous dyskinesias in neuroleptic naive adolescents at high risk for psychosis. J Vis Exp 2013, e50852.
Chatterjee A, Chakos M, Koreen A, Geisler S, Sheitman B, Woerner M et al. Prevalence and clinical correlates of extrapyramidal signs and spontaneous dyskinesia in never-medicated schizophrenic patients. Am J Psychiatry 1995; 152: 1724–1729.
Morrens M, Hulstijn W, Sabbe B . Psychomotor slowing in schizophrenia. Schizophr Bull 2007; 33: 1038–1053.
Morrens M, Hulstijn W, Lewi P, Sabbe B . Bleuler revisited: psychomotor slowing in schizophrenia as part of a catatonic symptom cluster. Psychiatry Res 2008; 161: 121–125.
Swerdlow NR, Koob GF . Dopamine, schizophrenia, mania, and depression: toward a unified hypothesis of cortico-striatopallido-thalamic function. Behav Brain Sci 1987; 10: 197–208.
Thompson JL, Pogue-Geile MF, Grace AA . Developmental pathology, dopamine, and stress: a model for the age of onset of schizophrenia symptoms. Schizophr Bull 2004; 30: 875–900.
Obeso JA, Rodriguez-Oroz MC, Rodriguez M, Lanciego JL, Artieda J, Gonzalo N et al. Pathophysiology of the basal ganglia in Parkinson’s disease. Trends Neurosci 2000; 23: S8–S19.
Koutsouleris N, Patschurek-Kliche K, Scheuerecker J, Decker P, Bottlender R, Schmitt G et al. Neuroanatomical correlates of executive dysfunction in the at-risk mental state for psychosis. Schizophr Res 2010; 123: 160–174.
Hannan KL, Wood SJ, Yung AR, Velakoulis D, Phillips LJ, Soulsby B et al. Caudate nucleus volume in individuals at ultra-high risk of psychosis: a cross-sectional magnetic resonance imaging study. Psychiatry Res 2010; 182: 223–230.
Chakos MH, Lieberman JA, Bilder RM, Borenstein M, Lerner G, Bogerts B et al. Increase in caudate nuclei volumes of first-episode schizophrenic patients taking antipsychotic drugs. Am J Psychiatry 1994; 151: 1430–1436.
Lodge DJ, Grace AA . Developmental pathology, dopamine, stress and schizophrenia. Int J Dev Neurosci 2011; 29: 207–213.
Acknowledgements
Funding
This work was supported by National Institutes of Health Grants R01MH094650 and R21/R33MH103231 to VAM.
Author information
Authors and Affiliations
Contributions
Authors DJD and VAM developed the study concept. VAM obtained funding for the study. Both authors contributed to the study design. Testing, data collection, interpretation, and analysis was performed by DJD under the supervision of VAM. DJD drafted the paper and VAM provided the critical revisions. Both the authors approved the final version of the paper for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Dean, D., Mittal, V. Spontaneous parkinsonisms and striatal impairment in neuroleptic free youth at ultrahigh risk for psychosis. npj Schizophr 1, 14006 (2015). https://doi.org/10.1038/npjschz.2014.6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/npjschz.2014.6
This article is cited by
-
Speech characteristics yield important clues about motor function: Speech variability in individuals at clinical high-risk for psychosis
Schizophrenia (2023)
-
Motor precision deficits in clinical high risk for psychosis
European Archives of Psychiatry and Clinical Neuroscience (2023)
-
Facial and upper-limb movement abnormalities in individuals with psychotic-like experiences: a motion analysis study
European Archives of Psychiatry and Clinical Neuroscience (2023)
-
Clinical, cognitive and neuroanatomical associations of serum NMDAR autoantibodies in people at clinical high risk for psychosis
Molecular Psychiatry (2021)
-
Detecting motor slowing in clinical high risk for psychosis in a computerized finger tapping model
European Archives of Psychiatry and Clinical Neuroscience (2020)