Abstract
There is currently a need for vaccines that stimulate cell-mediated immunity—particularly that mediated by CD8+ cytotoxic T lymphocytes (CTLs)—against viral and tumor antigens. The optimal induction of cell-mediated immunity requires the presentation of antigens by specialized cells of the immune system called dendritic cells1 (DCs). DCs are unique in their ability to process exogenous antigens via the major histocompatibility complex (MHC) class I pathway2 as well as in their ability to activate naive, antigen-specific CD8+ and CD4+ T cells1,3. Vaccine strategies that target or activate DCs in order to elicit potent CTL-mediated immunity are the subject of intense research. We report here that whole recombinant Saccharomyces cerevisiae yeast expressing tumor or HIV-1 antigens potently induced antigen-specific, CTL responses, including those mediating tumor protection, in vaccinated animals. Interactions between yeast and DCs led to DC maturation, IL-12 production and the efficient priming of MHC class I- and class II-restricted, antigen-specific T-cell responses. Yeast exerted a strong adjuvant effect, augmenting DC presentation of exogenous whole-protein antigen to MHC class I- and class II-restricted T cells. Recombinant yeast represent a novel vaccine strategy for the induction of broad-based cellular immune responses.
Similar content being viewed by others
Main
Dendritic cells (DCs) possess the unique ability to process particulate antigens efficiently into the major histocompatibility complex (MHC) class I pathway, in a process known as cross-priming2,4. In this regard, immunostimulatory complexes composed of liposome-like material incorporating antigenic proteins or peptides with added adjuvants have shown promise at stimulating cytotoxic T lymphocytes5,6 (CTLs). Yeast exhibit many of the particulate features of immunostimulatory complexes. In addition, they naturally possess adjuvant-like properties7,8 and can be easily engineered to express multiple antigens. On this basis, we investigated whether recombinant Saccharomyces cerevisiae yeast engineered to express a heterologous antigen would be capable of eliciting CTL-mediated responses and protective immunity in mice.
To determine whether recombinant yeast could trigger a protective CTL response, we used the E.G7-OVA tumor model that employs mouse EL-4 lymphoma cells expressing chicken ovalbumin5,9,10,11 (OVA). We vaccinated C57Bl/6 mice (H-2b) subcutaneously with either PBS or 2 × 107 whole recombinant S. cerevisiae expressing ovalbumin (OVAX). Seven days after the second weekly vaccination, mice were challenged with either EL-4 or E.G7-OVA cells. As expected, EL-4 lymphomas formed progressive tumors in mock- and OVAX-vaccinated mice (Fig. 1a), whereas mice vaccinated with OVAX, but not PBS, were protected from E.G7-OVA tumor formation (Fig. 1b). We evaluated the role of CD8+ T cells in mediating OVAX-induced tumor protection by vaccinating CD8-deficient C57Bl/6-Cd8atm1Mak knockout mice. E.G7-OVA tumors progressed similarly in OVAX- or mock-immunized CD8-deficient mice (Fig. 1c), indicating that the protective immunity elicited by the recombinant yeast vaccine in this model required CD8+ T cells.
a–c, Immunization with OVAX elicits CD8+ T-cell–dependent immunity to the OVA-transfected lymphoma E.G7-OVA; EL-4 (a) and E.G7-OVA (b and c) tumor growth in wild-type C57Bl/6 (a and b), and CD8-deficient (c) mice immunized with PBS (○) or OVAX (●). Tumor growth was measured on the indicated day after challenge. Results are presented as the mean tumor volume in mm3 observed in individual mice (6 per experimental group) ± s.e.m. d, HIVAX elicits gp160-specific, H-2d-restricted CTLs in BALB/c (H-2d) mice compared with PBS and YVEC. Targets are [51Cr]-labeled P815 (H-2d) cells infected with recombinant vaccinia virus encoding either HIV-1SF2-gp160 (rVV-SF2) at effector:target (E:T) ratios of 10:1 (▪), 20:1 (□) and 40:1 (░) or β-galactosidase (rVV-lac) at an E:T ratio of 40:1 (▨). Results are presented as the average percent specific lysis obtained using cells from individual mice (mean of triplicate samples at the indicated ratio) ± s.e.m. No killing was observed with MHC-mismatched rVV-SF2-infected B16 (H-2b) targets at an E:T ratio of 40:1 (▒), or with uninfected P815, uninfected B16 and rVV-lac-infected-B16 target cells (data not shown). e, HIVAX elicits gp120-specific T-cell proliferative responses in BALB/c (H-2d) mice compared with PBS and YVEC. T cells were assessed for proliferative response to medium alone (▪) or gp120-LAV from E. coli (□), gp120-SF2 from yeast (░), gp120-SF2 from CHO cells (▨) and gp130-FeLV from yeast (▒). T-cell proliferation results are presented as the average counts per minutes (c.p.m.) obtained using cells from individual mice (mean of triplicate samples) ± s.e.m. Numbers over bars represent stimulation indices.
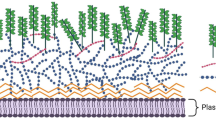
The ability of the yeast-based vaccine to stimulate protective CD8+ T cells in vivo prompted an investigation of the interaction between yeast and DCs in vitro. To determine whether yeast were phagocytosed by DCs, bone-marrow–derived DCs were incubated with control yeast (YVEC) labeled with the fluorescent dye MitoTracker Red. Yeast were internalized by DCs by 4 hours (Fig. 2a and c) and appeared largely fragmented by 24 hours (Fig. 2d). We observed a concomitant decrease in red fluorescence intensity as yeast were degraded, and detected no internalized yeast by 72 hours.
a–d, Immature DCs from day 5 bone-marrow cultures were co-incubated without (b) or with yeast stained with MitoTracker Red at 10 yeast cells per DC for 4 (a and c) or 24 (d) hours. DCs were then stained with FITC-conjugated antibodies specific for CD11c (a and b) or MHC class II (c and d). e and f, T-cell responses restricted by MHC class I (e) and class II (f) were determined using syngeneic antigen-pulsed DCs in combination with OT-1 OVA-specific Tg T cells or DO11.10 OVA-specific Tg T cells, respectively. Stimulator DCs were incubated overnight with graded amounts of OVAX yeast (yeast:DC ratio), or cognate MHC class I- or MHC class II-restricted OVA-derived peptide epitope, as indicated. Stimulation indices are shown over each bar.
To determine if DCs that had internalized yeast could present yeast-associated antigens via class I MHCs and prime antigen-specific T cells, we incubated DCs derived from C57Bl/6 mice with OVAX yeast for 24 hours and used these DCs to stimulate naive OVA-specific CD8+ T cells derived from OT-1 T-cell receptor transgenic (Tg) mice12. DCs pulsed with OVAX, but not YVEC yeast, induced potent, dose-dependent proliferation of OT-1 Tg T cells (Fig. 2e). Presentation of yeast-derived, MHC class I-restricted OVA epitopes was highly efficient; quantitative western-blot analysis revealed that OVAX contained approximately 0.01 nM OVA (OVAX:DC = 20:1; stimulation index = 359). This was similar to the proliferation observed with DCs pulsed with an apparently saturating amount of the cognate OVA257-264 peptide SIINFEKL (1 μM). To ascertain whether yeast-associated proteins were also presented via MHC class II, we used DCs derived from BALB/c mice and naive CD4+ OVA-specific T cells derived from DO-11.10 T-cell receptor Tg mice13. OVAX-pulsed DCs were highly effective at stimulating DO-11.10 Tg T cells to proliferate in an antigen-specific fashion (Fig. 2f). The responses from OVAX-pulsed DCs using as few as five yeast per DC (∼0.0025 nM OVA) were similar to the maximum response obtained with a saturating concentration of OVA323-339 peptide (5 μM).
To efficiently present antigens to naive T cells, immature DCs must be activated to mature, as defined by the upregulation of MHC and costimulatory molecules1 and production of cytokines, such as IL-12, which are critical for the induction of cellular immune responses14,15. Uptake of yeast by DCs increased surface expression of CD40, CD80, CD86, MHC class II and CD 54 (also known as ICAM- 1) to levels comparable to that induced by exposure to bacterial lipopolysaccharide (LPS), a potent DC maturation factor16,17 (Fig. 3a). As further evidence of yeast-induced activation, DCs pulsed with yeast produced significant amounts of IL-12 (Fig. 3b).
a, Immature DCs exposed for 48 h to medium alone (□) or yeast (░) mature into efficient APCs, showing increasing cell-surface expression (presented as fold increase in mean fluorescent channel; MFC) of MHC class II, CD40, CD54, CD80 and CD86, to an extent comparable with that achieved by bacterial LPS (▪). b, C57Bl/6-derived DCs incubated with graded amounts of YVEC yeast (yeast:DC ratio) or bacterial LPS were assessed for production of IL-12 by ELISA. IL-12 production is expressed as pg/ml of IL-12 produced after 48 h of stimulation. c and d, Syngeneic DCs pulsed overnight with OVAX yeast or varying amounts of soluble OVA protein in the presence or absence of YVEC yeast were used to stimulate proliferation of MHC class I-restricted, OT-1 OVA-specific Tg T cells (c) or MHC class II-restricted, DO11.10 OVA-specific Tg T cells (d). Stimulation indices are shown over each bar.
The effect of yeast on DC maturation prompted an investigation into the impact of yeast on the efficiency with which DCs present exogenous OVA to naive MHC class I- and class II-restricted, OVA-specific T cells. We co-incubated C57Bl/6- or BALB/c-derived DCs overnight with either OVAX (10 OVAX per DC), graded amounts of whole OVA protein or combinations of OVA together with YVEC (10 YVEC per DC). We then irradiated the DCs and combined them with naive OT-1 or DO11.10 Tg T cells in a lymphocyte proliferation assay. Very little MHC class I-restricted T-cell stimulation was obtained from DCs pulsed with exogenous soluble OVA antigen alone (Fig. 3c). Remarkably, combining YVEC with exogenous OVA resulted in a 50-fold increase in MHC class I-restricted, antigen-specific T-cell stimulation as compared with exogenous OVA alone. Despite the increase in OVA-specific T-cell stimulation associated with the addition of YVEC, the responses obtained with OVAX-pulsed DCs were greater still. On a per molar antigen basis, DCs pulsed with OVAX (containing ∼0.005 nM OVA at 10 OVAX per DC) yielded twice the stimulation obtained with YVEC plus 0.2 μM OVA. We also observed an adjuvant effect of yeast on DC presentation of OVA to MHC class II-restricted, OVA-specific T cells (Fig 3d). In this representative experiment, proliferation induced by DCs pulsed with YVEC plus 12 μM OVA was comparable with that obtained using 10 OVAX per DC, calculated to contain 0.005 nM OVA.
We next investigated whether yeast engineered to express a clinically relevant antigen, in this case the HIV-1SF2-gp160 envelope protein18 (HIVAX), could also elicit CTL activity. We vaccinated BALB/c mice (H-2d) once a week for three weeks with HIVAX, YVEC or PBS. CTL generated from mice vaccinated with HIVAX, but not PBS or YVEC, were able to kill target cells expressing gp160-SF2 (Fig. 1d). This killing was antigen-specific and MHC-restricted; whereas H-2d-bearing P815 cells infected with rVV-gp160-SF2 were killed by the BALB/c (H-2d)-derived CTL, rVV-lac–infected P815 and rVV-gp160-SF2–infected B16 melanoma cells (H-2b) were not (Fig. 1d). This vaccination regime also induced helper T lymphocytes specific for HIV-1-gp120. T cells isolated from spleen and mesenteric lymph nodes of HIVAX-vaccinated, but not mock- or YVEC-vaccinated, mice specifically responded to highly purified, recombinant-derived HIV-1SF2-gp120 envelope protein (gp160 devoid of the gp41 fusogen; Fig. 1e). Specificity of the response for HIV-1-gp120 was further supported by the observation that the T cells did not respond to yeast-derived feline leukemia virus gp130.
Here we provide the first demonstration that whole recombinant yeast can deliver heterologous antigens into both MHC class I and class II pathways and induce potent cell-mediated immunity when administered as a vaccine. Only one previous study examined the potential use of whole recombinant S. cerevisiae as a vaccine, and that study, while showing weak antibody responses, did not examine priming of cytotoxic or helper T cells19. We also show a potential role for DCs in mediating the potent cellular immune responses to yeast-derived antigens. The data indicate that yeast provide a powerful activation stimulus to DCs, resulting in upregulation of costimulatory and MHC molecules and IL-12 production. These data also indicate that the process of internalizing yeast or, alternatively, exposure to a yeast-derived factor matures DCs in a manner similar to that observed when DCs are exposed to microbial activation stimuli such as bacteria or bacterial products20, including LPS (refs. 16,17).
Yeast cell-wall components, especially β-1,3-d-glucan and mannan, possess adjuvant potential7,8,21,22. Our data likewise demonstrate that whole yeast act as a potent adjuvant and augment the ability of DCs pulsed with exogenous whole-protein antigen to stimulate both MHC class I- and class II-restricted primary T-cell responses in vitro. In fact, OVA-protein–pulsed DCs were unable to prime MHC class I-restricted T cells at all in the absence of yeast. Yeast acted as an adjuvant in this system despite the fact that the addition of yeast did not measurably increase OVA uptake by DCs; the amount of exogenous [14C]-labeled OVA protein internalized by DCs under these experimental conditions was not significantly altered by the addition of yeast (data not shown). This finding indicates that the observed increase in antigen-specific stimulation by DCs exposed to yeast results from either a qualitative change in the ability of DCs to process incorporated antigen via the MHC class I pathway or an increase in the efficiency of antigen presentation. Although yeast are shown to possess adjuvant potential, these properties cannot wholly account for the efficiency with which recombinant yeast-expressed antigens are processed and presented by DCs. Recombinant yeast appear to provide antigen to DCs in discrete, concentrated packages that are avidly internalized, thereby effectively increasing the amount of antigen available for processing. These results support the work of others, such as Inaba et al.23, who have shown the process of phagocytosis to be an extremely efficient means of antigen loading.
In summary, the recombinant-yeast–based vaccine approach integrates efficient antigen delivery with DC activation in a powerful vaccine formulation that does not require accessory adjuvant components. The ability of recombinant yeast to mature DCs into potent APCs while efficiently delivering antigens into both MHC class I and class II processing pathways indicates that recombinant yeast-based vaccine vectors might provide a powerful strategy for the induction of cell-mediated immunity directed against a variety of infectious diseases and cancer targets.
Methods
Mice.
We used 8–18-wk-old BALB/c, C57Bl/6, CD8-deficient C57Bl/6-Cd8atm1Mak mice (Jackson Labs, Bar Harbor, Maine), OT-1 transgenic mice (from T. Potter) and DO11.10 transgenic mice (from J. DeGregori). OT-1 and DO-11.10 mice express T cell receptor transgenes that recognize OVA257-264 peptide in the context of H-2Kb and OVA323-339 peptide in the context of I-Ad respectively.
Medium.
All assays were performed in RPMI-1640 (Life Technologies, Rockville, Maryland) plus 10% FBS (Hy-Clone, Logan, Utah), 50 μM 2ME (Sigma) and 10 μg/ml gentamicin-sulphate (Life Technologies). E.G7-OVA were cultured with 500 μg/ml G4.18 (Life Technologies). Supernatants from rat spleen cells stimulated for 24 h with 2.5 μg/ml concanavalin A were used as a source of T-cell growth factors (rat CAS).
Antigens and T-cell mitogens.
Purified HIV-1LAV-gp120 expressed in E. coli, HIV-1SF2-gp120 and FeLV-gp130 expressed in yeast, and HIV-1SF2-gp120 expressed in CHO cells were from Chiron Corporation (Emeryville, California) through the AIDS Reagent Program (NIH-NIAID, Bethesda, Maryland). Ovalbumin and concanavalin A were from Sigma. HPLC-purified SIINFEKL and IDQAVHAAHAEINEANTIGENR peptides were synthesized at National Jewish Medical and Research Center.
Yeast.
HIVAX yeast (AFY435) was described18. OVAX yeast expressed chicken ovalbumin cDNA (from M. Bevan) under control of CUP1 promoter in the Yex-Bx vector (Amrad Biotech, Baronia, Victoria, Australia) with a 10 h copper induction period. Ovalbumin expression in OVAX, compared to ovalbumin standards, was quantified by STORM PhosphorImager (Molecular Dynamics, Sunnyvale, California) analysis of immunoblots using monoclonal antibody against ovalbumin (Accurate, Westbury, New York) and goat anti-mouse alkaline phosphatase antibody (Sigma). In 3 analyses, ovalbumin levels in OVAX yeast were calculated to be ∼5 nmol/OD600 (1 OD600 = 1.0 × 107 viable yeast). Live yeast were used for vaccination, and heat-killed yeast were used in all other experiments.
DC cultures.
DCs were cultured from bone marrow as described24. Bone-marrow cells were cultured in complete RPMI-1640 plus 1000 U/ml mGM-CSF and 1000 U/ml IL-4 (R&D, Minneapolis, Minnesota). Surface phenotype analysis by flow cytometry on days 5–7 consistently revealed typical immature DC surface phenotype (MAC3−, CD80+, CD86+, CD40Low, CD54+, H-2Kb+, I-Ab+ and capable of FITC-dextran uptake) in ∼70% cells and microscopically revealed a dendritic, veiled morphology.
DC maturation.
Day 5 bone-marrow–derived DCs were incubated with maturation factors for 48 h, then analyzed by flow cytometry for known DC-surface maturation markers (CD80, CD86, CD54, CD40, MHC class I and MHC class II).
Fluorescent microscopy.
Yeast were stained 30 min in medium containing 0.1% MitoTracker-Red-CMX-Ros (Molecular Probes, Eugene, Oregon), then heat killed. DCs were co-incubated with yeast, then fixed and labeled with FITC-conjugated antibodies against murine CD11c or I-Ab for digital deconvolution microscopy.
Flow cytometry.
All antibodies were obtained directly conjugated to fluorochrome from PharMingen (San Diego, California) unless otherwise stated. Cells were incubated with antibodies for 30 min. Analysis was performed on a Beckton-Dickinson FACStar flow cytometer.
Quantification of OVA uptake by DCs.
DCs were suspended at 1 × 106/ml in 1.5 ml DC media. [14C]ovalbumin (Sigma) was added at 10 μg/ml alone or with YVEC at 10 yeast/DC. After overnight incubation, DCs were washed in ice-cold HBSS or 150 mM glycine (pH 4) to strip cell-surface–associated antigen, prior to liquid scintillation counting. DCs incorporated ∼10 ng OVA per 1 × 106 cells.
IL-12 ELISA.
DCs were incubated alone, with LPS (Sigma) or with yeast for 48 h and supernatant frozen at −80 °C. IL-12 in supernatant was quantified using Immulon-II plates (Dynex Technologies, Chantilly, Virginia) and murine p70 IL-12 ELISA kits (PharMingen). Plates were analyzed with Molecular Devices microplate reader.
Naive T-cell purification.
Nylon wool purified T lymphocytes were obtained from spleens and lymph nodes from OT-1 and DO11.10 mice. Specificity of OT-1 T cells was determined with PE-conjugated MHC class I tetramers comprising H-2Kb plus SIINFEKL. Specificity of DO11.10-purified T-cells was determined with FITC-conjugated monoclonal antibodies (KJ.1).
T-cell proliferation assays.
For OVAX presentation by DCs, day 7 murine bone-marrow–derived DCs were co-incubated overnight with antigens as indicated. DCs were irradiated (3000 R), washed and combined in triplicate at varying dilutions with enriched transgenic T cells at 1 × 105/ml. The plates were then pulsed with [3H]thymidine after 72 h. For HIVAX experiments, spleen and mesenteric lymph nodes were collected and single-cell suspensions were prepared. Enriched T-cell populations were obtained following removal of B cells and adherent cells by 'panning' with goat antibody against mouse immunoglobulin. Unfractionated, irradiated (3000 R) spleen and lymph node cells from the same mice were used as antigen-presenting cells (APCs). Enriched T cells and irradiated APCs were mixed 1:1 (final concentration of each cell type was 2 × 106/ml) and added to triplicate wells containing antigens (1 μg/ml) or mitogens. Plates were pulsed with [3H]thymidine on days 3 and 6. In each case, plates were pulsed with 1 μCi [3H]TdR/well in media, and [3H]thymidine incorporation measured after 16 h incubation on a Wallace-LKB Betaplate 1205 liquid scintillation counter. Stimulation index (SI) was calculated as CPM of T cells plus APC with antigen/CPM of T cells plus APC in media.
CTL generation.
40 × 106 unfractionated spleen and lymph node cells were placed in flasks containing 2 × 107 HIVAX yeast in 10 ml medium. On day 5, 5% rat CAS was added to all flasks. CTLs were collected by ficoll/hypaque density gradient centrifugation and resuspended in medium.
CTL assay.
Mouse P815 leukemia (H-2d) or B16 melanoma (H-2b) target cells were infected with 1 × 106 p.f.u. vaccinia virus expressing β-galactosidase or HIV-1SF2 gp160 overnight, then labeled with 100 μCi Na2[51Cr]O4 prior to plating in the CTL assay. Effector CTLs were diluted and mixed with [51Cr]-labeled target cells at varying effector:target (E:T) ratios. Cytolysis was determined by [51Cr]-release assay from target cells after 4 h at 37 °C. Data was calculated as mean percent specific cytolysis ± s.d., subtracting spontaneous chromium release.
Tumorigenicity studies.
Mice were injected s.c. and i.p. twice, with PBS or with 2 × 107 whole, live OVAX yeast 14 and 7 d before subcutaneous challenge with 1 × 106 EL-4 or E.G7-OVA lymphoma cells in 100 μl PBS. Tumor was injected subcutaneously near the vaccination site and on the contralateral flank. Tumor volume was determined using calipers. Mice were killed when tumor volumes exceeded 2 cm3.
References
Banchereau, J. & Steinman, R.M. Dendritic cells and the control of immunity. Nature 392, 245–52 (1998).
Rodriguez, A., Regnault, A., Kleijmeer, M., Ricciardi-Castagnoli, P. & Amigorena, S. Selective transport of internalized antigens to the cytosol for MHC class I presentation in dendritic cells. Nature Cell Biol. 1, 362–368 (1999).
Ridge, J.P., Di Rosa, F. & Matzinger, P. A conditioned dendritic cell can be a temporal bridge between a CD4+ T-helper and a T-killer cell. Nature 393, 474–8 (1998).
Yewdell, J.W., Norbury, C.C. & Bennink, J.R. Mechanisms of exogenous antigen presentation by MHC class I molecules in vitro and in vivo: implications for generating CD8+ T cell responses to infectious agents, tumors, transplants, and vaccines. Adv. Immunol. 73, 1–77 (1999).
Falo, L.D., Jr., Kovacsovics-Bankowski, M., Thompson, K. & Rock, K.L. Targeting antigen into the phagocytic pathway in vivo induces protective tumour immunity. Nature Med. 1, 649–53 (1995).
O'Hagan, D.T. Recent advances in vaccine adjuvants for systemic and mucosal administration. J. Pharm. Pharmacol. 50, 1–10 (1998).
Williams, D.L. et al. Development of a water-soluble, sulfated (1,3)—-D-glucan biological response modifier derived from Saccharomyces cerevisiae. Carbohydr. Res. 235, 247–57 (1992).
Rios-Hernandez, M., Dos-Santos, N.J., Silvia, C., Bello-Garciga, J.L. & Pedroso, M. Immunopharmacological studies of β-1,3-glucan. Arch. Med. Res. 25, 179–80 (1994).
McCabe, B.J. et al. Minimal determinant expressed by a recombinant vaccinia virus elicits therapeutic antitumor cytolytic T lymphocyte responses. Cancer Res. 55, 1741–7 (1995).
Brossart, P., Goldrath, A.W., Butz, E.A., Martin, S. & Bevan, M.J. Virus–mediated delivery of antigenic epitopes into dendritic cells as a means to induce CTL. J. Immunol. 158, 3270–6 (1997).
Cho, H.J. et al. Immunostimulatory DNA-based vaccines induce cytotoxic lymphocyte activity by a T-helper cell-independent mechanism. Nature Biotechnol. 18, 509–14 (2000).
Hogquist, K.A. et al. T cell receptor antagonist peptides induce positive selection. Cell 76, 17–27 (1994).
Murphy, K.M., Heimberger, A.B. & Loh, D.Y. Induction by antigen of intrathymic apoptosis of CD4+CD8+TCRlo thymocytes in vivo. Science 250, 1720–3 (1990).
Cella, M. et al. Ligation of CD40 on dendritic cells triggers production of high levels of interleukin-12 and enhances T cell stimulatory capacity: T-T help via APC activation. J. Exp. Med. 184, 747–52 (1996).
Koch, F. et al. High level IL-12 production by murine dendritic cells: upregulation via MHC class II and CD40 molecules and downregulation by IL-4 and IL-10. J. Exp. Med. 184, 741–6 (1996).
De Smedt, T. et al. Regulation of dendritic cell numbers and maturation by lipopolysaccharide in vivo. J. Exp. Med. 184, 1413–24 (1996).
Roake, J.A. et al. Dendritic cell loss from nonlymphoid tissues after systemic administration of lipopolysaccharide, tumor necrosis factor, and interleukin 1. J. Exp. Med. 181, 2237–47 (1995).
Franzusoff, A., Volpe, A.M., Josse, D., Pichuantes, S. & Wolf, J.R. Biochemical and genetic definition of the cellular protease required for HIV-1 gp160 processing. J. Biol. Chem. 270, 3154–9 (1995).
Schreuder, M.P., Deen, C., Boersma, W.J., Pouwels, P.H. & Klis, F.M. Yeast expressing hepatitis B virus surface antigen determinants on its surface: implications for a possible oral vaccine. Vaccine 14, 383–8 (1996).
Sallusto, F., Cella, M., Danieli, C. & Lanzavecchia, A. Dendritic cells use macropinocytosis and the mannose receptor to concentrate macromolecules in the major histocompatibility complex class II compartment: downregulation by cytokines and bacterial products. J. Exp. Med. 182, 389–400 (1995).
Toda, S. et al. HIV-1-specific cell-mediated immune responses induced by DNA vaccination were enhanced by mannan-coated liposomes and inhibited by anti-interferon-gamma antibody. Immunology 92, 111–7 (1997).
Shibata, Y., Metzger, W.J. & Myrvik, Q.N. Chitin particle-induced cell-mediated immunity is inhibited by soluble mannan: mannose receptor-mediated phagocytosis initiates IL-12 production. J. Immunol. 159, 2462–7 (1997).
Inaba, K. et al. Efficient presentation of phagocytosed cellular fragments on the major histocompatibility complex class II products of dendritic cells. J. Exp. Med. 188, 2163–73 (1998).
Mayordomo, J.I. et al. Therapy of murine tumors with p53 wild-type and mutant sequence peptide-based vaccines. J. Exp. Med. 183, 1357–65 (1996).
Acknowledgements
We thank M. Schleicher, K. Hance, J. Moore and L. Sylvan for technical assistance; G. Devendra for construction of the rVV-SF2-gp160 virus; T. Potter for OT-1 TCR transgenic mice; J. DeGregory for DO11.10 TCR transgenic mouse; P. Marrack, R. Kedl, B. Kotzin and S. Rozzo for discussion and useful suggestions. B. Moss for the vaccinia virus vSC8 (rVV-lac). This work has been supported by grants from the Cancer League of Colorado (A.C.S., A.F. and R.C.D.), the Colorado Advanced Technology Institute (D.B.), and by USPHS-NIH grants AI-01459 and AI-42704 (C.W.), AI-42688 (R.C.D.), AI-43143 (R.C.D and A.F.), AI-34747 (A.F.), AI-33299 (D.K.). This study made use of the Immunology and Tissue Culture Core Facilities of the University of Colorado Cancer Center supported by USPHS-NIH grant CA-46934.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Stubbs, A., Martin, K., Coeshott, C. et al. Whole recombinant yeast vaccine activates dendritic cells and elicits protective cell-mediated immunity. Nat Med 7, 625–629 (2001). https://doi.org/10.1038/87974
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/87974
This article is cited by
-
Development of therapeutic vaccines for the treatment of diseases
Molecular Biomedicine (2022)
-
Yeast-derived nanoparticles remodel the immunosuppressive microenvironment in tumor and tumor-draining lymph nodes to suppress tumor growth
Nature Communications (2022)
-
Lyophilized yeast powder for adjuvant free thermostable vaccine delivery
Applied Microbiology and Biotechnology (2021)
-
Yeast display platform technology to prepare oral vaccine against lethal H7N9 virus challenge in mice
Microbial Cell Factories (2020)
-
Formaldehyde effects on kanamycin resistance gene of inactivated recombinant Escherichia coli vaccines
Biotechnology Letters (2020)