Abstract
The adenovirus type 5 (Ad5)-based vaccine developed by Merck failed to either prevent HIV-1 infection or suppress viral load in subsequently infected subjects in the STEP human Phase 2b efficacy trial. Analogous vaccines had previously also failed in the simian immunodeficiency virus (SIV) challenge–rhesus macaque model. In contrast, vaccine protection studies that used challenge with a chimeric simian-human immunodeficiency virus (SHIV89.6P) in macaques did not predict the human trial results. Ad5 vector–based vaccines did not protect macaques from infection after SHIV89.6P challenge but did cause a substantial reduction in viral load and a preservation of CD4+ T cell counts after infection, findings that were not reproduced in the human trials. Although the SIV challenge model is incompletely validated, we propose that its expanded use can help facilitate the prioritization of candidate HIV-1 vaccines, ensuring that resources are focused on the most promising candidates. Vaccine designers must now develop T cell vaccine strategies that reduce viral load after heterologous challenge.
Similar content being viewed by others
Main
Passive transfer studies with broadly neutralizing antibodies in nonhuman primates provide a proof of principle that immunological protection against HIV-1 is possible1,2,3. Moreover, natural history studies in cohorts of HIV-1–infected humans and analogous studies with SIV in macaques show that cell-mediated immunity (CMI) can control primate immunodeficiency virus replication4. It is generally agreed that an effective HIV-1 vaccine will probably need to elicit broadly neutralizing antibodies as well as robust cellular immune responses to provide protection from infection, disease or both and to reduce transmission.
The failure of VaxGen's AIDSVAX HIV-1 vaccine was announced in 2003—this envelope-specific, gp120-based vaccine induced antibodies that did not neutralize primary HIV-1 isolates in vitro, did not prevent HIV-1 infection of humans, and had no effect on viral load in trial participants who became HIV-1 infected5. To date, no HIV-1 vaccine has induced broadly reactive neutralizing antibodies in clinical trials; this 'neutralizing antibody problem' remains the primary obstacle to a safe and effective vaccine and is being addressed by a number of groups and consortia, including IAVI's Neutralizing Antibody Consortium6.
The HIV-1 vaccine field has also been developing cytotoxic T lymphocyte (CTL)-based immunogens, encouraged by data from natural history studies and nonhuman primate models showing control of virus replication by CTLs (discussed below). To that end, an efficacy trial of a prime-boost regimen consisting of a canarypox vector prime and an AIDSVAX protein boost started in late 2003 amidst considerable controversy as to its likely outcome7,8; researchers in the field still await the results of this trial, now expected in 2009.
Unfortunately, the most promising approach for inducing CTL responses tested clinically to date, an Ad5-based vaccine regimen, has recently failed in human efficacy trials9. In the STEP human phase 2b efficacy trial, it neither prevented HIV-1 infection nor reduced viral load in subsequently infected subjects. This candidate vaccine, developed by Merck, was a replication-defective Ad5 vector, expressing the Gag, Pol and Nef proteins from HIV-1. The vaccine had elicited CMI responses against the HIV-1 Gag, Pol and Nef proteins in safety and immunogenicity trials10. However, on average, individual volunteers mounted relatively weak responses (10–20% of that seen in HIV-1–infected individuals controlling viral replication). Furthermore, T cells from vaccinees recognized a total of only three epitopes in the Gag, Pol and Nef immunogens, which may not be adequate for protection. It is possible that some or even all of these responses were rendered ineffective by HIV-1 sequence diversity, as the viruses to which human vaccinees were exposed differ in sequence by ∼10% even when the clade of the vaccine strain matched the one most prevalent within the trial site. Sequence mismatches are a particularly relevant concern because analyses of variability in regions of the virus outside the Envelope protein have shown that the majority of amino acid replacements are selected for by CTLs11,12. Hence, one can anticipate that many circulating viruses incorporate mutations that allow them to escape from normally immunodominant responses induced by vaccines that fail to stimulate CMI of sufficient breadth.
Advancement of candidate AIDS vaccines from phase 1 and 2a safety and immunogenicity trials to Phase 2b and 3 efficacy trials has been empirical. We discuss below the hopes for a T cell–based vaccine and the way in which the SIV-rhesus macaque challenge model predicted the failure of the Merck vaccine. We also propose mechanisms for the future prioritization of candidate HIV-1 vaccines.
Hopes for a T cell vaccine
There is evidence that CTLs can control AIDS virus replication in the absence of antibodies. The first indications that CTLs could suppress HIV-1 replication in vivo were observations that the reduction in viremia in acute infection was temporally associated with the appearance of HIV-1-specific CTLs13,14. A neutralizing antibody response usually occurs after this initial CTL response, after viremia has been controlled. The important role of CTLs was further suggested by work in the SIV-macaque model of HIV-1 infection. When monoclonal antibodies to CD8 were used to transiently deplete circulating CD8+ lymphocytes, the resulting loss of CD8+ cells significantly impaired immunological control of SIV replication in both the acute and chronic phases, leading to substantial increases in plasma viremia15,16,17,18.
The best long-term solution to the HIV-1 pandemic is a vaccine that prevents infection completely ('sterilizing immunity'). A less desirable, but still valuable, alternative is a vaccine that substantially reduces HIV-1–induced disease and the risk of transmitting infection to a new host. The latter was the most realistic goal of the Merck vaccine and of other CTL-inducing vectors that do not engender neutralizing antibodies. The risk of HIV-1 transmission is greatest when viremia is highest, that is, during acute infection and chronic infection with elevated viral load19,20,21. Any HIV-1 vaccine that cannot provide sterilizing immunity should, therefore, aim to limit peak viremia in acute infection and reduce chronic-phase viral loads from the median value of ∼30,000 copies/ml in untreated subjects to levels at which transmission is unlikely. In an observational study, infected individuals with viral loads of fewer than 1,500 copies/ml had a substantially reduced risk of infecting their seronegative partners (Fig. 1)22,23,24. This is a ∼1.5-log reduction. We therefore propose that a reduction of chronic phase viremia by ≥1.5 logs be established as a criterion of vaccine efficacy.
In practice, this is about a 1.5-log reduction, from a set point of 30,000 RNA copies/ml of plasma to <1,500 copies/ml. A similar numerical reduction in SIVmac239 viral load of rhesus macaques would be from about 1 × 106 RNA copies/ml to <30,000 copies/ml, although whether this would be sufficient to reduce any hypothetical transmission of SIV from macaque to macaque is unknown.
Limited success of CTL vaccines in the SIV model
Unfortunately, few CTL-based vaccine regimens have significantly lowered viral load or affected disease course in macaques challenged with the most stringent SIV strains, SIVmac239 and SIVmac25125,26,27,28. SIVmac251 is an uncloned biological isolate comprised of many related but distinct 'quasispecies', often described as a 'swarm', whereas SIVmac239 is a single clone derived from an SIVmac251-infected macaque29. Several vaccine regimens including modified vaccinia Ankara (MVA), canarypox virus (ALVAC) and New York vaccinia virus (NYVAC), all encoding SIV proteins, have exerted only modest levels of control over SIVmac251 replication30,31,32,33,34,35.
MVA, NYVAC, ALVAC and fowlpox vectors have also been used alone or after a DNA prime to vaccinate macaques that were subsequently challenged with SHIV89.6P. In 2001, Amara et al.36 used a DNA prime–MVA boost strategy to control SHIV89.6P replication, as manifested by viral load reduction and preservation of peripheral CD4+ T cells. Studies conducted by Merck and others had similar outcomes37,38,39. Although doubts have long been raised about the suitability of SHIV89.6P challenge for testing CTL-based vaccines40,41, some researchers considered control of SHIV89.6P replication in macaques to be sufficient to warrant further evaluation of analogous vaccines in humans. The failure of the Merck vaccine to control HIV-1 replication was, however, mimicked by macaque studies that used SIV challenges as we discuss below.
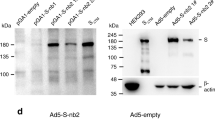
Adenovirus-based vaccines in macaques
Adenovirus-vectored vaccines consistently induce strong CMI responses and have therefore been considered strong candidates for further development. Previous studies have shown that macaques vaccinated with a DNA prime–Ad5 boost were more effective at controlling SIV replication than macaques immunized with a Ad5 prime–Ad5 boost (as was used in the recent Merck trial). However, even with the DNA prime–Ad5 boost, only macaques expressing a macaque MHC class I protein that had previously been associated with diminished viral replication (Mamu-A*01) showed any control of SIVmac239 replication (Fig. 2a). Vaccination with Ad5 prime–Ad5 boost was ineffective in both Mamu-A*01–positive and Mamu-A*01–negative macaques (Fig. 2b), and Mamu-A*01–negative macaques vaccinated with DNA prime–Ad5 boost did not control virus replication42,43.
(a) Mamu-A*01–positive macaques were vaccinated with Gag and then challenged with a high dose of SIVmac239 intrarectally. The macaques were either primed three times with DNA and then boosted with Ad5 (DNA-Ad5) or primed three times with Ad5 and boosted with Ad5 (Ad5). In macaques primed with DNA Gag, the peak of viremia was six times lower than in control macaques, and the early chronic set point was 15 times lower. There were no differences in either peak viremia or the early chronic set point in macaques primed with Ad5 Gag compared to control macaques. (b) Mamu-A*01–negative macaques were primed with three doses of DNA Gag, and then boosted with Ad5 Gag. The vaccinated macaques had a peak of viremia that was lower than in control macaques, but no difference was observed in viral loads at any subsequent time points, indicating that Mamu-A*01 has only a moderate protective effect in Gag-vaccinated macaques42.
A DNA prime–Ad5 boost regimen in which the Ad5 encodes SIVmac239 Env, Gag and Pol has been tested by the Vaccine Research Center in Indian rhesus macaques44,45. This vaccine resulted in transient control (until day 112) of the homologous SIVmac251 challenge virus, amelioration of memory CD4+ T cell loss during the acute phase and prolonged survival of vaccinees. However, given the inclusion of a matched Env construct in the vaccine regimen and the marginal reduction in replication of the homologous challenge virus, the prospects for the success of this type of vaccination in humans are not compelling.
Whether vaccine-induced cellular immunity in the absence of any Env-specific antibodies can control viral replication was studied by multiple low-dose challenges with the highly pathogenic SIVmac239 isolate46. In this experiment, eight Mamu-A*01–positive Indian rhesus macaques were vaccinated with SIV Gag, Tat, Rev and Nef using a DNA prime–adenovirus boost strategy. Peak viremia (P = 0.007) and the chronic phase, set point viral load (P = 0.0192) were significantly decreased in the vaccinated cohort up to 1 year after infection (Fig. 3). Of note, only one of the eight vaccinees had developed Env-specific neutralizing antibodies by one year after infection. Thus, vaccine-induced CMI responses can clearly exert considerable control over replication of a primate immunodeficiency virus in the complete absence of neutralizing antibodies. This finding supports the idea that a vaccine that induces only CMI responses might be able to control viral replication.
Mamu-A*01–positive rhesus macaques were primed with DNA encoding Gag, Tat, Rev and Nef three times and then boosted with an Ad5 vector encoding the same four proteins before a repeated low-dose intrarectal challenge. Both the peak and the set point viral loads were significantly lower in the vaccinees than in control macaques46.
Live attenuated SIV
The most successful non-human primate vaccine to date is live attenuated SIV. But even this vaccine is only partially effective against a heterologous SIV challenge. Unfortunately, these attenuated viruses often become pathogenic and thus will not be used in humans for safety reasons. Immunization with live attenuated SIV has consistently protected rhesus macaques against challenge with a homologous, pathogenic SIV47,48,49. However, only a few small studies have addressed whether this type of vaccine can control replication of a heterologous SIV with mixed results50,51,52.
Why did the Merck vaccine fail?
The vaccine's failure to control HIV-1 replication may have been due to the Ad5 vector, the choice of HIV-1 transgenes or a combination of these two factors. It is possible that a replication-defective Ad5 vector is simply unable to stimulate CMI responses of sufficient breadth to control HIV-1 infection. Furthermore, many people have been infected with Ad5 and therefore have immunity to this virus. Pre-existing Ad5-specific antibodies could restrict the number of Ad5 particles that can infect target cells and produce transgene-derived proteins. In individuals previously exposed to an adenovirus, anamnestic adenovirus-specific CD8+ T cells dominate the initial response to the Ad5 vaccine. Pre-existing Ad5-specific CD8+ T cell responses could also potentially reduce the potency and breadth of vaccine-induced HIV-1-specific CD8+ T cell responses. Many different factors might affect the preferential expansion of these Ad5-specific CD8+ T cells, thereby diminishing the expansion of the HIV-1–specific precursors53,54,55,56,57. Moreover, the selection of HIV-1 transgenes used (gag-pol-nef) may be insufficient for inducing control. In contrast to the limited number of HIV-1 gene products expressed by the Ad5 vector, the live attenuated SIV that protects against heterologous SIV challenges is a persistently replication-competent (albeit weakened) virus that expresses every SIV antigen with the exception of parts of Nef. Developing the next generation of improved vaccine candidates will require that we address the key issues detailed below.
Vaccines should broaden immune responses
Volunteers in the STEP Ad5 vaccine trial mounted only a limited, and possibly inadequate, number of epitope-specific CTL responses against the HIV-1 Gag, Pol and Nef transgene products. Although several factors can contribute to the antiviral efficacy of CD8+ T cells, including functional avidity58, killing efficiency59, polyfunctionality60, evolutionary constraints on the epitope sequences61,62, the kinetics of antigen presentation63,64 and proliferative ability, it is becoming increasingly apparent that not all CTLs are functionally equivalent. In natural infections, the CTL response is often focused on a few immunodominant epitopes. But these CTL populations may not necessarily be the best antiviral effectors. Hence, one possible approach to a vaccine is to induce as many CTL responses as possible. It may be necessary to alter the natural immunodominance patterns of HIV-1– or SIV-specific CD8+ T cell responses to reveal subdominant responses of potentially greater efficacy65,66.
How will we know which CTLs are the most effective?
It is imperative to identify which of the many different CTL responses that arise during HIV-1 infection actually contribute to reducing viral replication67. To do this, new and sensitive methods of assessing CTL function should be developed. Previous assays have relied on autologous Epstein-Barr virus–transformed B cell lines pulsed with high concentrations of peptides to assess CD8+ T cell function. Similarly, conventional enzyme-linked immunosorbent spot or intracellular cytokine staining assays assess the ability of CD8+ T cells to secrete interferon-γ in response to rather high peptide concentrations. None of these assays necessarily measures the ability of CTLs to suppress the replication of HIV-1 in autologous CD4+ T cells or in cell lines. However, new assays have very recently been developed that measure these parameters64,68,69,70,71,72 and should help to determine, for the first time, which of the many CTL responses can actually control HIV-1 replication in vitro.
HIV-1 sequence variability
The enormous variability of HIV-1 is among the major hurdles that must be overcome if an effective vaccine is to be successfully developed. Accumulated nucleotide changes within the highly mutable env gene are important in classifying HIV-1 into different groups (M, N and O) and then into subtypes or clades. Sequence analysis shows that env nucleotide sequences may vary by up to 35% between clades and by up to 20% even within a clade73. Hence, many CMI-based HIV-1 vaccine designs have abandoned Env as an immunogen to focus on more conserved proteins (for example, Pol and Gag). However, even relatively minor variations in these proteins may have grave implications for vaccine efficacy; single amino-acid differences can impair or even eliminate antigen recognition by vaccine-induced CD8+ T cells74,75.
Summary and conclusions
The results of the STEP trial, although disappointing, were consistent with and arguably predicted by studies of analogous SIV vaccines in rhesus macaques. Because no macaque study has predicted a positive result in humans (as there have been none), one must exercise caution in interpreting nonhuman primate challenge studies. Nonetheless, the concordance of outcomes from SIV vaccine experiments in nonhuman primates and human efficacy trials does suggest that SIV challenge of monkeys can be a valuable filter for choosing which vaccine candidates should advance to clinical trials. But how stringent should the conditions for product advancement be?
First, it should be noted that SIV antigens are different from HIV-1 antigens and that MHC types differ between humans and macaques. Thus, epitope-specific CTL responses against SIV epitopes may not be directly comparable to CTL responses against HIV-1 epitopes. There are also several other variables that might affect the outcomes of vaccine trials in nonhuman primates, including the species of macaque, the choice of the challenge virus, the distribution of MHC class I alleles in the study macaques and the route of challenge. The factors outlined below should therefore be considered when judging whether a vaccine should enter large-scale phase 3 efficacy and licensing trials.
1. Safety and immunogenicity trials in humans. The vaccine candidate should be shown to be safe and immunogenic in phase 1 and 2a trials. Immunogenicity should be based on validated assays that should show that a vast majority of volunteers immunized with the vaccine show positive responses. The quality and/or quantity of the immune responses to a CMI vaccine should be markedly improved over those elicited by the Merck Ad5 product.
2. Protection conferred by an analogous vaccine in the SIV–rhesus macaque challenge model. Whenever feasible, the analogous SIV vaccine should be designed and tested in rhesus macaques before advancing the candidate to a phase 2 screening test of concept (STOC) trial76 (see point 3 below). This may not always be possible, as some candidate vaccines—for example, epitope-based concepts, some bacterial-vectored delivery systems and some viral vectors that are species-specific for humans—cannot be appropriately modeled in SIV–nonhuman primate challenge studies. For those candidate vaccines that can be evaluated in the SIV–rhesus macaque model, the vaccine should suppress viral load by a minimum of 1.5 logs (peak and set point) compared to control macaques when tested for its efficacy against a heterologous repeated low-dose mucosal SIV challenge.
3. Protection of humans in a STOC trial76. STOC trials could rapidly screen a limited number of leading HIV-1 vaccine candidates, enabling the most promising to be prioritized to large-scale, phase 3 efficacy licensing trials. The primary endpoint of a STOC trial is plasma HIV-1 RNA viral load at set point (about 3–6 months after infection) in participants who become infected with HIV-1. In a STOC trial, ∼30 incident HIV-1 infections are enough to detect a minimum of a one-log suppression of viral load with sufficient statistical power. Any candidate vaccines that show a 1.5-log suppression of viral load for longer than 1 year should be considered for advancement to phase 3 licensing trials.
4. Feasibility for large-scale manufacture and distribution. Candidate vaccines that have fulfilled criteria 1 and 2 or 1 and 3 should be advanced to phase 3 licensing and efficacy trials, provided that they can be manufactured on a large enough scale to enable their widespread distribution if they turn out to be effective.
References
Baba, T.W. et al. Human neutralizing monoclonal antibodies of the IgG1 subtype protect against mucosal simian-human immunodeficiency virus infection. Nat. Med. 6, 200–206 (2000).
Mascola, J.R. et al. Protection of macaques against vaginal transmission of a pathogenic HIV-1/SIV chimeric virus by passive infusion of neutralizing antibodies. Nat. Med. 6, 207–210 (2000).
Parren, P.W. et al. Antibody protects macaques against vaginal challenge with a pathogenic R5 simian/human immunodeficiency virus at serum levels giving complete neutralization in vitro. J. Virol. 75, 8340–8347 (2001).
Deeks, S.G. & Walker, B.D. Human immunodeficiency virus controllers: mechanisms of durable virus control in the absence of antiretroviral therapy. Immunity 27, 406–416 (2007).
VaxGen. VaxGen announces results of its phase 3 HIV vaccine trial in Thailand: vaccine fails to meet endpoints. <http://investor.vaxgen.com/profiles/investor/ResLibraryView.asp?ResLibraryID=5836&GoTopage=16&BzID=923&Category=214> (2003).
Burton, D.R. et al. HIV vaccine design and the neutralizing antibody problem. Nat. Immunol. 5, 233–236 (2004).
Burton, D.R. et al. Public health. A sound rationale needed for phase 3 HIV-1 vaccine trials. Science 303, 316 (2004).
McNeil, J.G., Johnston, M.I., Birx, D.L. & Tramont, E.C. Policy rebuttal. HIV vaccine trial justified. Science 303, 961 (2004).
[Anonymous]. HIV vaccine failure prompts Merck to halt trial. Nature 449, 390 (2007).
Priddy, F. H. et al. Safety and immunogenicity of a replication-incompetent adenovirus type 5 HIV-1 clade B gag/pol/nef vaccine in healthy adults. Clin. Infect. Dis. 46, 1769–1781 (2008).
Allen, T.M. et al. Selective escape from CD8+ T cell responses represents a major driving force of human immunodeficiency virus type 1 (HIV-1) sequence diversity and reveals constraints on HIV-1 evolution. J. Virol. 79, 13239–13249 (2005).
O'Connor, D.H. et al. A dominant role for CD8+ T lymphocyte selection in simian immunodeficiency virus sequence variation. J. Virol. 78, 14012–14022 (2004).
Borrow, P., Lewicki, H., Hahn, B.H., Shaw, G.M. & Oldstone, M.B. Virus-specific CD8+ cytotoxic T lymphocyte activity associated with control of viremia in primary human immunodeficiency virus type 1 infection. J. Virol. 68, 6103–6110 (1994).
Koup, R.A. et al. Temporal association of cellular immune responses with the initial control of viremia in primary human immunodeficiency virus type 1 syndrome. J. Virol. 68, 4650–4655 (1994).
Matano, T. et al. Administration of an anti-CD8 monoclonal antibody interferes with the clearance of chimeric simian/human immunodeficiency virus during primary infections of rhesus macaques. J. Virol. 72, 164–169 (1998).
Schmitz, J.E. et al. Control of viremia in simian immunodeficiency virus infection by CD8+ lymphocytes. Science 283, 857–860 (1999).
Jin, X. et al. Dramatic rise in plasma viremia after CD8+ T cell depletion in simian immunodeficiency viru–infected macaques. J. Exp. Med. 189, 991–998 (1999).
Friedrich, T.C. et al. Subdominant CD8+ T cell responses are involved in durable control of AIDS virus replication. J. Virol. 81, 3465–3476 (2007).
Leynaert, B., Downs, A.M. & de Vincenzi, I. Heterosexual transmission of human immunodeficiency virus: variability of infectivity throughout the course of infection. European Study Group on Heterosexual Transmission of HIV. Am. J. Epidemiol. 148, 88–96 (1998).
Pilcher, C.D. et al. Brief but efficient: acute HIV infection and the sexual transmission of HIV. J. Infect. Dis. 189, 1785–1792 (2004).
Wawer, M.J. et al. Rates of HIV-1 transmission per coital act, by stage of HIV-1 infection, in Rakai, Uganda. J. Infect. Dis. 191, 1403–1409 (2005).
Quinn, T.C. et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. Rakai Project Study Group. N. Engl. J. Med. 342, 921–929 (2000).
Gray, R.H. et al. Probability of HIV-1 transmission per coital act in monogamous, heterosexual, HIV-1–discordant couples in Rakai, Uganda. Lancet 357, 1149–1153 (2001).
Gray, R.H. et al. Stochastic simulation of the impact of antiretroviral therapy and HIV vaccines on HIV transmission; Rakai, Uganda. AIDS 17, 1941–1951 (2003).
Vogel, T.U. et al. Multispecific vaccine-induced mucosal cytotoxic T lymphocytes reduce acute-phase viral replication but fail in long-term control of simian immunodeficiency virus SIVmac239. J. Virol. 77, 13348–13360 (2003).
Allen, T.M. et al. Tat-vaccinated macaques do not control simian immunodeficiency virus SIVmac239 replication. J. Virol. 76, 4108–4112 (2002).
Allen, T.M. et al. Effects of cytotoxic T lymphocytes (CTL) directed against a single simian immunodeficiency virus (SIV) Gag CTL epitope on the course of SIVmac239 infection. J. Virol. 76, 10507–10511 (2002).
Allen, T.M. et al. Induction of AIDS virus–specific CTL activity in fresh, unstimulated peripheral blood lymphocytes from rhesus macaques vaccinated with a DNA prime/modified vaccinia virus Ankara boost regimen. J. Immunol. 164, 4968–4978 (2000).
Thakallapally, R. & Kuiken, C. in HIV Molecular Immunology 2000 (eds. Korber, B. et al.) 73–81 (Los Alamos National Laboratory, Los Alamos, 2000).
Benson, J. et al. Recombinant vaccine–induced protection against the highly pathogenic simian immunodeficiency virus SIV(mac251): dependence on route of challenge exposure. J. Virol. 72, 4170–4182 (1998).
Horton, H. et al. Immunization of rhesus macaques with a DNA prime/modified vaccinia virus Ankara boost regimen induces broad simian immunodeficiency virus (SIV)-specific T cell responses and reduces initial viral replication but does not prevent disease progression following challenge with pathogenic SIVmac239. J. Virol. 76, 7187–7202 (2002).
Pal, R. et al. ALVAC–SIV-gag-pol-env–based vaccination and macaque major histocompatibility complex class I (A*01) delay simian immunodeficiency virus SIVmac-induced immunodeficiency. J. Virol. 76, 292–302 (2002).
Hel, Z. et al. Containment of simian immunodeficiency virus infection in vaccinated macaques: correlation with the magnitude of virus-specific pre- and postchallenge CD4+ and CD8+ T cell responses. J. Immunol. 169, 4778–4787 (2002).
Hel, Z. et al. Equivalent immunogenicity of the highly attenuated poxvirus-based ALVAC-SIV and NYVAC-SIV vaccine candidates in SIVmac251-infected macaques. Virology 304, 125–134 (2002).
Hel, Z. et al. Improved vaccine protection from simian AIDS by the addition of nonstructural simian immunodeficiency virus genes. J. Immunol. 176, 85–96 (2006).
Amara, R.R. et al. Control of a mucosal challenge and prevention of AIDS by a multiprotein DNA-MVA vaccine. Science 292, 69–74 (2001).
Barouch, D.H. et al. Control of viremia and prevention of clinical AIDS in rhesus monkeys by cytokine-augmented DNA vaccination. Science 290, 486–492 (2000).
Rose, N.F. et al. An effective AIDS vaccine based on live attenuated vesicular stomatitis virus recombinants. Cell 106, 539–549 (2001).
Shiver, J.W. et al. Replication-incompetent adenoviral vaccine vector elicits effective anti–immunodeficiency virus immunity. Nature 415, 331–335 (2002).
Feinberg, M.B. & Moore, J.P. AIDS vaccine models: challenging challenge viruses. Nat. Med. 8, 207–210 (2002).
Lifson, J.D. & Martin, M.A. One step forwards, one step back. Nature 415, 272–273 (2002).
Casimiro, D.R. et al. Attenuation of simian immunodeficiency virus SIVmac239 infection by prophylactic immunization with DNA and recombinant adenoviral vaccine vectors expressing Gag. J. Virol. 79, 15547–15555 (2005).
McDermott, A.B. et al. Cytotoxic T lymphocyte escape does not always explain the transient control of simian immunodeficiency virus SIVmac239 viremia in adenovirus-boosted and DNA-primed Mamu-A*01–positive rhesus macaques. J. Virol. 79, 15556–15566 (2005).
Mattapallil, J.J. et al. Vaccination preserves CD4 memory T cells during acute simian immunodeficiency virus challenge. J. Exp. Med. 203, 1533–1541 (2006).
Letvin, N.L. et al. Preserved CD4+ central memory T cells and survival in vaccinated SIV-challenged monkeys. Science 312, 1530–1533 (2006).
Wilson, N.A. et al. Vaccine-induced cellular immune responses reduce plasma viral concentrations after repeated low-dose challenge with pathogenic simian immunodeficiency virus SIVmac239. J. Virol. 80, 5875–5885 (2006).
Wyand, M.S., Manson, K.H., Garcia-Moll, M., Montefiori, D. & Desrosiers, R.C. Vaccine protection by a triple deletion mutant of simian immunodeficiency virus. J. Virol. 70, 3724–3733 (1996).
Daniel, M.D., Kirchhoff, F., Czajak, S.C., Sehgal, P.K. & Desrosiers, R.C. Protective effects of a live attenuated SIV vaccine with a deletion in the nef gene. Science 258, 1938–1941 (1992).
Johnson, R.P. et al. Highly attenuated vaccine strains of simian immunodeficiency virus protect against vaginal challenge: inverse relationship of degree of protection with level of attenuation. J. Virol. 73, 4952–4961 (1999).
Wyand, M.S. et al. Protection by live, attenuated simian immunodeficiency virus against heterologous challenge. J. Virol. 73, 8356–8363 (1999).
Nilsson, C. et al. Live attenuated simian immunodeficiency virus (SIV)mac in macaques can induce protection against mucosal infection with SIVsm. AIDS 12, 2261–2270 (1998).
Abdel-Motal, U.M. et al. Kinetics of expansion of SIV Gag–specific CD8+ T lymphocytes following challenge of vaccinated macaques. Virology 333, 226–238 (2005).
Yewdell, J.W. Confronting complexity: real-world immunodominance in antiviral CD8+ T cell responses. Immunity 25, 533–543 (2006).
Smith, C.L. et al. Immunodominance of poxviral-specific CTL in a human trial of recombinant-modified vaccinia Ankara. J. Immunol. 175, 8431–8437 (2005).
Kastenmuller, W. et al. Cross-competition of CD8+ T cells shapes the immunodominance hierarchy during boost vaccination. J. Exp. Med. 204, 2187–2198 (2007).
Willis, R.A., Kappler, J.W. & Marrack, P.C. CD8 T cell competition for dendritic cells in vivo is an early event in activation. Proc. Natl. Acad. Sci. USA 103, 12063–12068 (2006).
Chen, W., Anton, L.C., Bennink, J.R. & Yewdell, J.W. Dissecting the multifactorial causes of immunodominance in class I–restricted T cell responses to viruses. Immunity 12, 83–93 (2000).
Bennett, M.S., Ng, H.L., Dagarag, M., Ali, A. & Yang, O.O. Epitope-dependent avidity thresholds for cytotoxic T lymphocyte clearance of virus-infected cells. J. Virol. 81, 4973–4980 (2007).
Rollman, E. et al. Killing kinetics of simian immunodeficiency virus–specific CD8+ T cells: implications for HIV vaccine strategies. J. Immunol. 179, 4571–4579 (2007).
Betts, M.R. et al. HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood 107, 4781–4789 (2006).
Friedrich, T.C. et al. Reversion of CTL escape-variant immunodeficiency viruses in vivo. Nat. Med. 10, 275–281 (2004).
Leslie, A.J. et al. HIV evolution: CTL escape mutation and reversion after transmission. Nat. Med. 10, 282–289 (2004).
Sacha, J.B. et al. Gag-specific CD8+ T lymphocytes recognize infected cells before AIDS-virus integration and viral protein expression. J. Immunol. 178, 2746–2754 (2007).
Ali, A. et al. Impacts of epitope expression kinetics and class I downregulation on the antiviral activity of human immunodeficiency virus type 1–specific cytotoxic T lymphocytes. J. Virol. 78, 561–567 (2004).
Palmowski, M.J. et al. Competition between CTL narrows the immune response induced by prime-boost vaccination protocols. J. Immunol. 168, 4391–4398 (2002).
Rodriguez, F., Harkins, S., Slifka, M.K. & Whitton, J.L. Immunodominance in virus-induced CD8+ T cell responses is dramatically modified by DNA immunization and is regulated by γ interferon. J. Virol. 76, 4251–4259 (2002).
Yang, O.O. Will we be able to 'spot' an effective HIV-1 vaccine? Trends Immunol. 24, 67–72 (2003).
Chung, C. et al. Not all cytokine-producing CD8+ T cells suppress simian immunodeficiency virus replication. J. Virol. 81, 1517–1523 (2007).
Loffredo, J.T. et al. Tat28–35SL8-specific CD8+ T lymphocytes are more effective than Gag(=181–189CM9-specific CD8+ T lymphocytes at suppressing simian immunodeficiency virus replication in a functional in vitro assay. J. Virol. 79, 14986–14991 (2005).
Van Baalen, C.A. et al. Kinetics of antiviral activity by human immunodeficiency virus type 1–specific cytotoxic T lymphocytes (CTL) and rapid selection of CTL escape virus in vitro. J. Virol. 72, 6851–6857 (1998).
Yang, O.O. et al. Suppression of human immunodeficiency virus type 1 replication by CD8+ cells: evidence for HLA class I–restricted triggering of cytolytic and noncytolytic mechanisms. J. Virol. 71, 3120–3128 (1997).
Tomiyama, H., Fujiwara, M., Oka, S. & Takiguchi, M. Cutting Edge: Epitope-dependent effect of Nef-mediated HLA class I down-regulation on ability of HIV-1–specific CTLs to suppress HIV-1 replication. J. Immunol. 174, 36–40 (2005).
Gaschen, B. et al. Diversity considerations in HIV-1 vaccine selection. Science 296, 2354–2360 (2002).
Valentine, L.E. et al. Recognition of escape variants in ELISPOT does not always predict CD8+ T cell recognition of simian immunodeficiency virus–infected cells expressing the same variant sequences. J. Virol. 82, 575–581 (2008).
Bennett, M.S., Ng, H.L., Ali, A. & Yang, O.O. Cross-clade detection of HIV-1–specific cytotoxic T lymphocytes does not reflect cross-clade antiviral activity. J. Infect. Dis. 197, 390–397 (2008).
Excler J.L., Rida W., Priddy F., Fast P. & Koff, W. A strategy for accelerating the development of preventive AIDS vaccines. AIDS 21, 2259–2263 (2007).
Acknowledgements
We thank J. Loffredo, A. Espinosa, N. Wilson Schlei, T. Friedrich and L. Valentine for help in preparing this article. We are also grateful to the members of the Watkins Laboratory for advice on its contents and to S. Noble of IAVI for assistance with editing. The preparation of this article and of the research it describes was supported by US National Institutes of Health grants R01 AI049120, R01 AI052056, R24 RR015371 and R24 RR016038 to D.I.W., grants R37 AI36082 and R01 AI45463 to J.P.M., grant U01 AI69420 to E.G.K. and grants R37 AI33292 and R01 AI055332 to D.R.B. We also wish to acknowledge Merck and IAVI for their support of the Watkins Laboratory and Fundação de Amparo à Pesquisa do Estado de São Paulo for support of the Kallas Laboratories.
Author information
Authors and Affiliations
Ethics declarations
Competing interests
D.I.W. has enjoyed a long-standing collaboration with scientists at Merck. They have supplied his group with DNA and Ad5 constructs for vaccine studies. E.G.K. is a Federal University of SSãoo Paulo site principal investigator for the STEP trial and has been receiving funds from Merck to run clinical trials; he also provides consultant services for Merck and Bristol-Meyers Squibb.
Rights and permissions
About this article
Cite this article
Watkins, D., Burton, D., Kallas, E. et al. Nonhuman primate models and the failure of the Merck HIV-1 vaccine in humans. Nat Med 14, 617–621 (2008). https://doi.org/10.1038/nm.f.1759
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.f.1759
This article is cited by
-
HIV-1 subtype C Nef-mediated SERINC5 down-regulation significantly contributes to overall Nef activity
Retrovirology (2023)
-
Bioengineering translational models of lymphoid tissues
Nature Reviews Bioengineering (2023)
-
Targeted immune epitope prediction to HHLA2 and MAGEB5 protein variants as therapeutic approach to related viral diseases
BMC Immunology (2021)
-
“World in motion” – emulsion adjuvants rising to meet the pandemic challenges
npj Vaccines (2021)
-
Induction of neutralizing antibodies against tier 2 human immunodeficiency virus 1 in rhesus macaques infected with tier 1B simian/human immunodeficiency virus
Archives of Virology (2019)