Abstract
The phosphatidylinositol-3-kinase pathway is one of the most commonly altered molecular pathways in invasive breast carcinoma, with phosphatidylinositol-3-kinase catalytic subunit (PIK3CA) mutations in 25% of invasive carcinomas. Ductal carcinoma in situ (DCIS), benign papillomas, and small numbers of columnar cell lesions harbor an analogous spectrum of PIK3CA and AKT1 mutations, yet there is little data on usual ductal hyperplasia and atypical ductal and lobular neoplasias. We screened 192 formalin-fixed paraffin-embedded breast lesions from 75 patients for point mutations using a multiplexed panel encompassing 643 point mutations across 53 genes, including 58 PIK3CA substitutions. PIK3CA point mutations were identified in 31/62 (50%) proliferative lesions (usual ductal hyperplasia and columnar cell change), 10/14 (71%) atypical hyperplasias (atypical ductal hyperplasia and flat epithelial atypia), 7/16 (44%) lobular neoplasias (atypical lobular hyperplasia and lobular carcinoma in situ), 10/21 (48%) DCIS, and 13/37 (35%) invasive carcinomas. In genotyping multiple lesions of different stage from the same patient/specimen, we found considerable heterogeneity; most notably, in 12 specimens the proliferative lesion was PIK3CA mutant but the concurrent carcinoma was wild type. In 11 additional specimens, proliferative epithelium and cancer contained different point mutations. The frequently discordant genotypes of usual ductal hyperplasia/columnar cell change and concurrent carcinoma support a role for PIK3CA-activating point mutations in breast epithelial proliferation, perhaps more so than transformation. Further, these data suggest that proliferative breast lesions are heterogeneous and may represent non-obligate precursors of invasive carcinoma.
Similar content being viewed by others
Main
The phosphatidylinositol-3-kinase pathway is one of the most commonly mutated pathways in invasive breast carcinoma. Activating mutations in the phosphatidylinositol-3-kinase catalytic subunit (PIK3CA) are present in ∼25% of invasive carcinomas and are present in an even higher percentage (on the order of 40%) of low-grade estrogen receptor-positive carcinomas (luminal A intrinsic subtype).1, 2, 3, 4, 5, 6, 7, 8, 9, 10 PIK3CA mutations cluster in ‘hotspots’ in exon 9 (helical domain, E542K and E545K) and exon 20 (kinase domain, H1047R/L).1, 2, 3, 4, 5, 6, 7, 8, 9, 10 In addition, this pathway is activated by mutations in the plekstrin-homology domain of AKT1 in ∼5% of breast carcinomas, by the loss of the phosphatase PTEN (phosphatase and tensin homolog on chromosome 10), or rarely by amplification or alterations in other regulatory subunits, and is a target of active drug development.8, 9, 10, 11 In recent large studies of estrogen receptor-positive tumors, the presence of activating PIK3CA hotspot point mutations has been paradoxically associated with more favorable outcome as compared with breast carcinomas with wild-type PIK3CA.3, 12, 13
We and other groups have previously shown that the PIK3CA genotype is concordant between ductal carcinoma in situ (DCIS) and concurrent invasive carcinoma in 66–100% of tested samples.14, 15, 16, 17 However, several small studies suggest that pre-neoplastic or benign breast lesions, such as papillomas, radial scars, or columnar cell lesions, may also very frequently harbor PIK3CA mutations.18, 19, 20, 21, 22, 23 The goal of this study was to systematically screen a large number of hyperplastic and putative precursor breast lesions, along with accompanying carcinomas for known activating mutations in PIK3CA and other key signaling molecules.
Materials and methods
After Institutional Review Board approval, computerized pathology files of Oregon Health and Science University (2005–2010) were surveyed for breast specimens containing usual ductal hyperplasia, columnar cell change, atypical hyperplasia, and lobular neoplasia. Usual and atypical ductal hyperplasias were classified using the criteria of Page, Schnitt and others,24, 25 and the columnar cell lesion spectrum classified using the criteria of Schnitt et al.24, 26 Slides were reviewed to confirm histologic diagnosis and select lesions for genotyping. Where available, a spectrum of lesions was isolated from the same specimen, including proliferative lesions, atypical lesions, in situ, invasive, and/or metastatic carcinoma. Data on invasive tumor size, grade, nodal status, and hormone receptor status were abstracted from pathology reports. There was no known prior chemotherapy or radiation therapy for breast carcinoma, with the exception of two recurrent cases as noted (excluded from totals by histologic lesion Table 1, but included in Figure 2 and Supplementary Table 1). Some patients had recent prior breast excisional biopsy/lumpectomy at other hospitals and presented to our institution for definitive surgery, such that carcinoma was not available for genotyping.
Lesional tissue was isolated by punching the formalin-fixed paraffin-embedded tissue block(s), using 1 or 2 mm coring devices, with a hematoxylin and eosin (H&E) stained slide as the template. Multiple cores of each lesion were collected; cores were re-embedded in paraffin and an H&E slide was prepared from the recipient block in order to confirm and/or re-classify lesional tissue. Unsatisfactory cores were excluded from further testing. This method yielded samples composed of lesional epithelium, surrounding myoepithelium, and stroma, with variable percentage of lesional cells. Diagnoses of usual ductal hyperplasia and columnar cell change were reviewed by two pathologists (DA, MLT). Usual ductal hyperplasia and columnar cell change were frequently intimately associated and were combined for most analyses. A separate subgroup analysis was conducted on ‘pure’ lesions consisting of >80% usual ductal hyperplasia or >80% columnar cell change. Likewise, the analysis of atypical lesions included only specimens composed of >80% atypical lesional epithelium; there was frequently a small percentage of accompanying columnar cell lesion. Other mixed lesions were excluded from analysis; however, they are illustrated in Figure 2 and annotated as such in Supplementary Table 1A.
Paraffin shavings from the recipient blocks were prepared and DNA was extracted from paraffin using standard protocols (Qiagen Qiamp Mini kit, Valencia, CA). DNA yield was quantitated on a Nanodrop (Thermo Scientific, Wilmington DE) or Qubit fluoromenter (Life Technologies, Grand Island, NY). DNA extracts (0.75 μg) were screened for a large panel of activating point mutations using a multiplexed PCR–mass spectroscopy-based technique encompassing 643 point mutations in 53 genes (Sequenom MassArray, Sequenom, San Diego, CA), as previously described.19, 27 In brief, the mutation panel covers point mutations in AKT1/2/3, ALK, BRAF, CDK4, CSF1R, CTNNB1, EGFR, ERBB2, ERCC6, FBX4, FBXW7, FES, FGFR1/2/3/4, FOXL2, GNA11, GNAQ, GNAS, HRAS, IDH1/2, IGF1R, KDR, KIT, KRAS, MAP2K1/2/7, MET, MYC, NEK9, NRAS, NTRK1/2/3, PDGFRA, PIK3CA, PIK3R1/4/5, PKHD1, PRKCB1, RAF1, RET, SMO, SOS1, STAT1, TEC, and TP53. The panel includes 58 substitutions in 34 codons of the PIK3CA gene. Results were excluded if >5% of assays failed, unless a point mutation was confirmed. Point mutations identified by mass spectroscopy screening were confirmed by direct sequencing on an ABI3130 sequencer (Applied Biosystems, Carlsbad, CA) using the BigDye terminator method, with or without the use of a locked nucleic acid probe to partially suppress amplification of the wild-type allele, as previously described in detail.28 The assay sensitivity is ∼5–10% mutant allele for mass spectroscopy screening and 0.6–2.5% mutant allele for locked nucleic acid sequencing.27, 28
Ki-67 immunohistochemical staining was performed on a subset of pure columnar cell lesions using antibody clone 30-9 (pre-dilute, cell conditioning 1, and mild antigen retrieval) on Ventana XT instruments with Ultraview detection (all from Ventana, Tucson, AZ), using standard protocols. Statistical analysis with χ2 and Fisher’s exact test were computed using Excel software.
Results
Patients and Genotyping
We reviewed H&E-stained archival slides of formalin-fixed paraffin-embedded breast excisional specimens (breast reduction, surgical biopsy, lumpectomy, and mastectomy) to select lesions for genotyping, to include benign/proliferative epithelial lesions, atypical lesions, lobular neoplasia, DCIS, invasive carcinoma, and lymph nodes metastasis, where available.24, 25, 26 We focused on specimens with benign proliferative lesions, including usual ductal hyperplasia and columnar cell change, especially those with accompanying carcinomas available for comparative study. Lesions were screened for known hotspot point mutations using a multiplexed mass spectroscopy-based approach with a panel covering 643 common activating point mutations in 53 known cancer genes, including 58 hotspot substitutions in the PIK3CA gene, along with coverage of other breast cancer genes such as AKT1, ERBB2, PIK3R1, and TP53; identified mutations were sequence confirmed.19, 20, 21, 27, 28 The final study group included 192 breast lesions successfully genotyped from 75 patients, as follows (Supplementary Table 1A and B): 62 usual ductal hyperplasia/columnar cell lesion, 14 atypical ductal hyperplasia/flat epithelial atypia, 16 lobular neoplasias, 21 DCIS, 37 invasive carcinomas, 6 lymph node metastases, and 36 other lesions (papillomas, mixed histology, and from patients with recurrent cancer).
Mutational Profile of Usual Ductal Hyperplasia and Columnar Cell Lesions without Atypia
Usual ductal hyperplasia was often intimately admixed with, or adjacent to, epithelium showing columnar cell change; thus, a combined group of usual ductal hyperplasia and columnar cell lesion was analyzed. We found PIK3CA-activating point mutations in half of the proliferative lesions in this category (31/62, 50%; Table 1, Figures 1 and 2, Supplementary Table 1B). No point mutations in other genes of the large screening panel were detected in usual ductal hyperplasia/columnar cell lesions. We separately analyzed smaller subgroups of ‘pure’ lesions (>80% usual ductal hyperplasia and >80% columnar cell lesion, respectively). Again, nearly half of the lesions in each of these subgroups harbored PIK3CA mutations: usual ductal hyperplasia 6/12 (50%) and columnar cell lesion 11/26 (42%; Table 1, Supplementary Table 1B). In many cases, multiple non-atypical epithelial lesions from the same specimen/patient were screened and often had discordant genotypes, as discussed in detail below and illustrated in Figures 1 and 2. In this group of proliferative lesions, PIK3CA exon 20 kinase domain mutations were most common (22 exon 20 mutations and 9 exon 9 mutations), unlike in invasive and in situ carcinomas (see below and Table 1).
Morphologic and genotypic characterization of breast lesions, patient 11. (a) Usual ductal hyperplasia (UDH, left). PCR–mass spectroscopy analysis (right) demonstrates a phosphatidylinositol-3-kinase catalytic subunit (PIK3CA) H1047R mutant (*) peak (upper), along with a larger wild-type peak (WT). The H1047R mutation was confirmed by direct sequencing (data not shown). The lower tracing demonstrates wild-type PIK3CA E542K assay. (b) Columnar cell lesion (CCL, left). PCR–mass spectroscopy indicates a PIK3CA E542K mutant peak (*), along with a larger WT peak. The E542K mutation was confirmed by direct sequencing (data not shown). (c) Lobular carcinoma in situ (LCIS, left). PCR–mass spectroscopy analysis (right) shows a PIK3CA H1047R mutant (*) peak, along with a larger WT peak. The H1047R mutation was confirmed by direct sequencing (data not shown). All other screened codons were WT. (d) Invasive lobular carcinoma (ILC, left). PCR–mass spectroscopy analysis (right) demonstrates a PIK3CA H1047R mutant (*) peak, along with a larger WT peak. The H1047R mutation was confirmed by direct sequencing (data not shown). All other screened codons were WT. (e) Lobular carcinoma metastatic to lymph node (left). PCR–mass spectroscopy analysis (right) demonstrates a PIK3CA H1047R mutant (*) peak, along with a larger WT peak in the upper panel. In addition, a FGFR2 N550K mutant peak (*) was seen, shown together with its WT sequence in the lower tracing. Both mutations were confirmed by direct sequencing (data not shown). All other screened codons were WT. The small peaks in the middle of the PIK3CA H1047R PCR–mass spectroscopy tracings represent WT peaks from an unrelated, multiplexed assay. Original magnifications for hematoxylin and eosin stained sections: × 200.
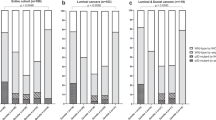
Mutational status by patient. Each row indicates samples from a single patient; mutations are color-coded. Blank boxes indicated no lesion/not tested. ‘&’ Two separate lesions tested. ‘/’ Two mutations identified within the same lesional sample. ‘^’Mixed with other histologies. These lesions were excluded from Table 1. See Supplementary Table for further detail. ADH, atypical ductal hyperplasia; ALH, atypical lobular hyperplasia; CCL, columnar cell lesion; DCIS, ductal carcinoma in situ; FEA, flat epithelial atypia; LCIS, lobular carcinoma in situ; IDC, invasive ductal carcinoma; ILC, invasive lobular carcinoma; UDH, usual ductal hyperplasia; WT, wild type for all point mutations screened.
Retrospective review revealed no qualitative difference in morphology of usual ductal hyperplasia/columnar cell lesion with PIK3CA mutant or wild-type genotype. The ‘pure’ columnar cell lesion group was further stratified as columnar cell change (no hyperplasia, 3 of 8 with mutations), columnar cell hyperplasia (3 of 6 with mutations), or both (5 of 12 with mutations). We also used Ki-67 immunohistochemical stating to assess proliferative fraction of the ‘pure’ columnar cell lesion group. The mean Ki-67 staining in the columnar cell lesions with PIK3CA mutations was 2% (1.4% s.d., n=8 with tissue available for analysis), whereas the mean Ki-67 in the wild-type columnar cell lesions was 3.7% (2.4% s.d., n=15).
Mutational Profile of Atypical Ductal and Lobular Lesions
Atypical ductal hyperplasia and flat epithelial atypia comprise the group of atypical ductal lesions.24, 26 Seventy-one percent of atypical ductal lesions contained PIK3CA-activating point mutations (10/14, 71%; Table 1, Supplementary Table 1B). However, this includes three samples of atypical ductal epithelium from the same patient/specimen (all with PIK3CA exon 4 N345K substitution) and two atypical lesions from another patient (both wild type). Combining lesions by patient nevertheless yields 8/11 (72%) of atypical specimens with activating point mutations. One atypical hyperplasia had a PIK3CA N345K mutation, co-occurring with a KRAS G12D mutation.
Sixteen lesions of atypical lobular hyperplasia and/or lobular carcinoma in situ were screened, yielding 7/16 (44%) of lesions with mutations, all in the PIK3CA gene (Table 1, Supplementary Table 1B).
Mutational Profile of In Situ, Invasive, and Metastatic Carcinoma
We conducted mutational screening on 21 samples of DCIS, resulting in 10/21 (48%) lesions with activating point mutations in the PI3K-AKT pathway (Table 1, Supplementary Table 1B). The invasive carcinoma subgroup included 24 cases of invasive ductal carcinoma, 11 invasive lobular carcinoma, 1 invasive papillary carcinoma, and 1 metaplastic carcinoma. Overall, 13 of 37 (35%) of invasive carcinomas harbored mutations, again with the vast majority in the PIK3CA gene. For the in situ and invasive carcinomas combined, there were 10 PIK3CA exon 9 mutations and only 6 exon 20 mutations; the frequency of exon 20 mutations was different in UDH/CCL as compared with carcinoma (exon 20 mutations UDH/CCL=22/62; carcinoma=6/57, P=0.001), whereas exon 9 mutations were not significantly different in these groups (exon 9 mutations UDH/CCL=9/62; carcinoma=10/57, P=0.2). We encountered TP53 mutations (R175H and R273H) in two invasive ductal carcinomas and an FBXW7 mutation was seen along with a PIK3CA exon 9 mutation in an invasive lobular carcinoma. The invasive ductal subgroup included 7/24 (29%) of carcinomas with mutations, whereas the invasive lobular subgroup had 6/11 (54%) point mutations (Table 1, Supplementary Table 1B).
In correlating genotype with other biomarkers, the overwhelming majority of invasive carcinomas in the study were estrogen receptor-positive, precluding meaningful analysis of hormone receptor profile. The five estrogen receptor-negative tumors were wild type for PIK3CA; both TP53-mutated tumors were estrogen receptor- and Her-2/neu-negative. There were no differences in genotype by carcinoma grade (data not shown).
We analyzed axillary lymph node metastases from a small number of patients, yielding 5/6 (82%) of metastasis with point mutations. Four cases had PIK3CA mutations; two of these had coincident mutations in other genes: PIK3CA E545K and FBXW7*, as was also seen in the primary breast carcinoma; and the other had PIK3CA H1047R and FGFR2 N550K, with only the PIK3CA mutation in the primary breast sample (Table 1, Supplementary Table 1B).
Comparison of the Mutation Spectrum of Proliferative, Atypical, and Malignant Breast Lesions in Individual Patients
Multiple concurrent epithelial lesions with different histologic features were available for mutation screening in 58 patients/specimens, including 51 with invasive or in situ carcinoma. Figure 2 illustrates the mutation profile over the spectrum of breast lesions by specimen/patient (also see Supplementary Table 1 for further details). In six specimens, point mutations were identified in usual ductal hyperplasia/columnar cell lesions, and the same mutations were found in concurrent carcinomas (concordant with point mutations), as depicted at the top of Figure 2 (patients 1–6). Likewise, in a subset of 13 patients the proliferative lesions and concurrent carcinomas each screened as wild type for the tested panel (concordant wild type, Figure 2, patients 49–60). However, the majority of specimens contained breast proliferative lesions and carcinoma with discordant genotypes. Eight patients had proliferative lesions screened as wild type, with an apparent ‘gain’ of activating point mutations in carcinoma (‘discordant: carcinoma mutant,’ Figure 2 patients 40–47). Interestingly, there were 12 breast specimens harboring usual ductal hyperplasia/columnar cell lesion with activating point mutations, accompanied by wild-type invasive or in situ carcinoma (‘discordant: carcinoma wild-type,’ Figure 2, patients 19–30). The vast majority of these proliferative lesions had PIK3CA exon 20 H1047R mutations10. Further, 11 other patients had a spectrum of lesions with multiple different PIK3CA point mutations (‘discordant multiple,’ Figure 2, patients 7–16,18).
Of the proliferative lesions from patients with no known prior, concurrent, or subsequent ipsilateral invasive or in situ carcinoma, 8/10 were wild type, whereas only 2 had PIK3CA mutations (H1047R, C420R; see Figure 2 and Supplementary Table 1, patients 8R, 21L, 34, 46R, 63R&L, 66, 68, 69, 73; 3 had contralateral cancer).
Although the study was focused on proliferative lesions, we also analyzed carcinoma in situ as compared with concurrent carcinoma where possible, yielding good concordance despite small numbers (Supplementary Table 1C). For DCIS and paired invasive ductal carcinoma, five out of seven specimens had concordant genotypes (concordant mutant or concordant wild type). One specimen had wild-type DCIS but PIK3CA H1047R mutation in a recurrent invasive ductal carcinoma (discordant: carcinoma mutant, Figure 2, Supplementary Table 1C, patient 43), whereas another had mutant DCIS with wild-type invasive metaplastic carcinoma (discordant: carcinoma wild type, Figure 2, Supplementary Table 1C, patient 12). Interestingly, concordance was also good for lobular neoplasia (atypical lobular hyperplasia/lobular carcinoma in situ) and concurrent invasive lobular carcinoma. Six specimens containing both lesions had concordant PIK3CA genotypes (four concordant wild-type and two concordant mutant). Two patients had a PIK3CA exon 9 E542K mutation in lobular neoplasia, but the invasive carcinomas each harbored a PIK3CA codon 1047 mutation; one of these was a recurrent carcinoma with an additional HRAS mutation in one of two tested invasive carcinomas (discordant multiple, Figure 2, Supplementary Table 1C, patient 15).
Discussion
Activating PIK3CA point mutations are among the most common genetic aberrations in invasive breast cancer,1, 2, 3, 4, 5, 6, 7, 8, 9, 10 and several studies have shown that these mutations exist at nearly the same frequency in DCIS.14, 15, 16, 17 Accumulating evidence suggests that PIK3CA point mutations may also be common in other proliferative breast lesions such as benign papillomas and columnar cell lesions.18, 19, 20, 21, 22, 23 Prior studies have failed to identify PIK3CA mutations in histologically normal breast tissue, even with the same sensitive methods employed here.1, 8, 16, 19 In this study, we demonstrated a 50% frequency of PIK3CA point mutations in usual ductal hyperplasia and columnar cell lesions across 62 lesions, representing the largest series to date. We also found similarly a high frequency of PIK3CA mutations in smaller cohorts of atypical ductal lesions (71%) and lobular neoplasia (44%), and a near-lack of other ‘hotspot’ activating mutations in genes such as AKT1. Table 2 represents a summary of our laboratory’s experience with activating point mutations in proliferative and malignant breast lesions in this and prior studies. Our data on PIK3CA mutations in DCIS (48% in this study and 45% combined) and invasive mammary carcinoma (35% in this study and 34% combined) matches the literature.1, 2, 3, 4, 5, 6, 7, 8 We identified point mutations in other genes in invasive carcinomas, but not in ‘earlier’ lesions, including TP53, FBXW7, FGFR2, and HRAS.
In analyzing multiple breast lesions from the same specimen/patient, spanning the morphologic spectrum of non-atypical epithelial lesions (usual ductal hyperplasia and columnar cell change), atypical ductal lesions, lobular neoplasia, in situ, invasive, and metastatic carcinoma, we found a wide diversity of genotypes. These observations provide some insight as to the role of activating PIK3CA mutations in breast carcinogenesis, as well as the precursor status of these early breast lesions. If PIK3CA mutations are an early or late ‘driver’ of breast carcinogenesis, these mutations would be expected to appear in committed precursor lesions, and persist through the development of carcinoma as further genetic changes evolve, perhaps as reflected in the ‘concordant mutant’ and ‘discordant: carcinoma mutant’ groups of specimens in our study, respectively (Figure 2). However, we identified a relatively large group of specimens/patients in which activating PIK3CA mutations were present in usual ductal hyperplasia and/or columnar cell change, but the accompanying carcinomas were wild type for these mutations (Figure 2, see ‘discordant: carcinoma wild type’). This result is not likely to be biased by assay sensitivity, as the mass spectrometry screening method was previously demonstrated to have a sensitivity of 5–10% mutant allele,27 and the carcinomas isolated generally had greater lesional cellularity as compared with the non-atypical epithelial lesions. Further, these findings have implications for clinical and research genotyping of breast carcinomas, emphasizing the need for prudent isolation of lesional tissue in order to avoid ‘false positives,’ as could occur if a wild-type invasive carcinoma is accompanied by proliferative epithelium harboring PIK3CA mutation.
Many studies over the past 20 years have applied genomic assays in an attempt to map breast cancer progression and to identify early breast precursor lesions (Supplementary Table 2).24, 29, 30, 31, 32, 33, 34 Nevertheless, defining the role of usual ductal hyperplasia and columnar cell lesions as precursors, non-obligate precursors, or unrelated bystanders in the sequence of breast carcinogenesis remains a challenge. It has recently been proposed that columnar cell lesion may represent the first histologically distinct, but non-obligate precursor of breast carcinoma based on genetic and immunohistochemical data as recently summarized.24, 19, 35, 36 Genomic findings in usual ductal hyperplasia have varied widely based on tissue substrate (fresh/frozen/formalin fixed), method of lesion dissection, method of genomic analysis, including karyotypic analysis, loss of heterozygosity/allelic imbalance, and, most recently, comparative genomic hybridization (Supplementary Table 2).24, 29, 30, 31, 32, 33, 34 These prior studies and our data support a general theme of fewer yet more heterogeneous genomic alterations in hyperplasia as compared with carcinoma (Supplementary Table 2).24, 29, 30, 31, 32, 33, 34
The few studies of point mutations in breast hyperplasias have yielded a paucity of mutations in specific genes such as TP53 and PTEN (Table 3).37, 38, 39, 40, 41 However, Fuqua et al42 reported the K303R mutation in ESR1 (encoding estrogen receptor-α) in 20/59 (34%) of breast hyperplasias, a mutation that confers estrogen hypersensitivity and has been shown to activate the PI3K pathway in vitro.(43) Li et al16 studied PIK3CA mutations in usual ductal hyperplasia and found no mutations in 16 lesions, in contrast to our results; the differences may be due to sample size and methodologic sensitivity, as they used less-sensitive direct Sanger sequencing.16
The activating PIK3CA hotspot mutations seen frequently in breast cancers and proliferative lesions, most notably H1047R, E542K and, E545K, have transforming potential when overexpressed in a variety of cell culture models,8, 9, 10 which arise before the most common ancestor in the genomic history of several breast carcinomas23, 44 and have thus been logically viewed as drivers of carcinogenesis. Interestingly, expression of the PIK3CA H1047R mutation at physiologic or inducible supraphysiologic levels in the mouse mammary gland leads to increased branching, duct dilation, and luminal epithelial hyperplasia.45, 46, 47 Expressing the PIK3CA H1047R mutant at physiologic levels throughout mammary development leads to mouse mammary tumors after very long latency (median tumor free survival of 484 days or 492 days nulliparous, as reported by two independent groups).46, 47 The resulting tumors are heterogeneous in morphology (fibroadenoma, adenocarcinoma, adenosquamous carcinoma, and spindle cell carcinoma) and hormone expression.46, 47 Activation of downstream elements of the PIK3CA signaling cascade such as pAKT and pS6 was demonstrated in tumors, but not at time points with early mammary hyperplastic lesions, suggesting crosstalk or additional hits in tumors.46, 47 Further, genetic profiling of mammary tumors in these mouse model systems revealed that they contained the engineered PIK3CA mutation, but had also gained other genomic changes such as p53, MET, c-Myc, and other oncogenes, even becoming independent of the PIK3CA mutation, as was seen in two-thirds of the tumors in the inducible model.45, 47 These animal models, together with our findings in usual ductal hyperplasia and columnar cell lesions from patient specimens, support the hypothesis that activated PIK3CA may have a role in breast epithelial proliferation, more so than as a driver of breast oncogenesis, and alone is insufficient for carcinogenesis.45, 46, 47
The discordance in PIK3CA mutation status between breast proliferative lesions and concurrent carcinoma bears some similarities to that of FGFR3 mutation and overexpression in early bladder cancers. FGFR3 mutations are seen in ∼60% of in situ bladder lesions, but in <20% of T2-stage invasive carcinomas.48, 49 Further, genotyping of multiple regions from the same bladder cancer specimen revealed FGFR3 mutations in the non-invasive component with paired wild-type invasive carcinoma from eight discordant specimens, and different point mutations in one sample (of 43 specimens with multiple areas tested).48, 49 With regard to these findings, the authors suggest that FGFR3 contributes early in the process of tumor development, and either the FGFR3 mutant allele was lost in the high stage lesion or it is a small subpopulation of FGFR3 wild-type cells in the non-invasive lesion that progresses to invasive carcinoma.48, 49
In conclusion, we have screened a spectrum of 192 breast lesions with emphasis on proliferative lesions, and found that PIK3CA mutations were very frequent and were heterogeneous between multiple lesions in the same specimen. Importantly, point mutations in proliferative lesions were often paired with wild-type carcinomas. These findings support the concept of usual ductal hyperplasia and/or columnar cell lesion as heterogenous non-obligate precursors of breast cancer, and to the notion that PIK3CA ‘hotspot’ mutations are important early in breast epithelial proliferation/neoplasia, but may not contribute a selective advantage at later stages of tumor progression. Further studies of functional pathway activation, as well as more detailed genomic and epigenomic studies will be necessary to more fully characterize the putative precursor role of usual ductal hyperplasia and columnar cell lesions, and the molecular evolution of breast carcinogenesis.
References
Barbareschi M, Buttitta F, Felicioni L et al. Different prognostic roles of mutations in the helical and kinase domains of the PIK3CA gene in breast carcinomas. Clin Cancer Res 2007;13:6064–6069.
Stemke-Hale K, Gonzalez-Angulo AM, Lluch A et al. An integrative genomic and proteomic analysis of PIK3CA, PTEN, and AKT mutations in breast cancer. Cancer Res 2008;68:6084–6091.
Kalinsky K, Jacks LM, Heguy A et al. PIK3CA mutation associates with improved outcome in breast cancer. Clin Cancer Res 2009;15:5049–5059.
Ellis MJ, Ding L, Shen D et al. Whole-genome analysis informs breast cancer response to aromatase inhibition. Nature 2012;486:353–360.
Banerji S, Cibulskis K, Rangel-Escareno C et al. Sequence analysis of mutations and translocations across breast cancer subtypes. Nature 2012;486:405–409.
Stephens PJ, Tarpey PS, Davies H et al. The landscape of cancer genes and mutational processes in breast cancer. Nature 2012;486:400–404.
Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature 2012;490:61–70.
Troxell ML . PIK3CA/AKT1 mutations in breast carcinoma: A comprehensive review of experimental and clinical studies. J Clin Exper Pathol 2012;S1:002 doi:10.4172/2161-0681.S1-002 (e-pub ahead of print).
McAuliffe PF, Meric-Bernstam F, Mills GB et al. Deciphering the role of PI3K/Akt/mTOR pathway in breast cancer biology and pathogenesis. Clin Breast Cancer 2010;10 (Suppl 3):S59–S65.
Gonzalez-Angulo AM, Blumenschein GR Jr . Defining biomarkers to predict sensitivity to PI3K/Akt/mTOR pathway inhibitors in breast cancer. Cancer Treat Rev 2013;39:313–320.
Carpten JD, Faber AL, Horn C et al. A transforming mutation in the pleckstrin homology domain of AKT1 in cancer. Nature 2007;448:439–444.
Loi S, Haibe-Kains B, Majjaj S et al. PIK3CA mutations associated with gene signature of low mTORC1 signaling and better outcomes in estrogen receptor-positive breast cancer. Proc Natl Acad Sci USA 2010;107:10208–10213.
Cizkova M, Cizeron-Clairac G, Vacher S et al. Gene expression profiling reveals new aspects of PIK3CA mutation in Eralpha-positive breast cancer: major implication of the Wnt signaling pathway. PloS One 2010;5:e15647.
Dunlap J, Le C, Shukla A et al. Phosphatidylinositol-3-kinase and AKT1 mutations occur early in breast carcinoma. Breast Cancer Res Treat 2010;120:409–418.
Miron A, Varadi M, Carrasco D et al. PIK3CA mutations in in situ and invasive breast carcinomas. Cancer Res 2010;70:5674–5678.
Li H, Zhu R, Wang L et al. PIK3CA mutations mostly begin to develop in ductal carcinoma of the breast. Exp Mol Pathol 2010;88:150–155.
Kalinsky K, Heguy A, Bhanot UK et al. PIK3CA mutations rarely demonstrate genotypic intratumoral heterogeneity and are selected for in breast cancer progression. Breast Cancer Res Treat 2011;129:635–643.
Troxell ML, Levine J, Beadling C et al. High prevalence of PIK3CA/AKT pathway mutations in papillary neoplasms of the breast. Mod Pathol 2010;23:27–37.
Troxell ML, Brunner AL, Neff T et al. Phosphatidylinositol-3-kinase pathway mutations are common in breast columnar cell lesions. Mod Pathol 2012;25:930–937.
Kehr EL, Jorns JM, Ang D et al. Mucinous breast carcinomas lack PIK3CA and AKT1 mutations. Hum Pathol 2012;43:2207–2212.
Flatley E, Ang D, Warrick A et al. Troxell ML. PIK3CA-AKT pathway mutations in micropapillary breast carcinoma. Hum Pathol 2013;44:1320–1327.
Wolters KL, Ang D, Warrick A et al. Frequent PIK3CA mutations in radial scars. Diagn Mol Pathol (in press).
Newburger DE, Kashef-Haghighi D, Weng Z et al. Genome evolution during progression to breast cancer. Genome Res. 2013;23:1097–1108.
Schnitt SJ, Ellis IO, van de Vijver MJ et al. Intraductal proliferative lesions In: Lakhani SR, Ellis IO, Schnitt SJ, et al. (eds). WHO Classification of Tumours of the Breast. IARC Press: Lyon, France, 2012, pp 84–94.
Schnitt SJ, Connolly JL, Tavassoli FA et al. Interobserver reproducibility in the diagnosis of ductal proliferative breast lesions using standardized criteria. Am J Surg Pathol 1992;16:1133–1143.
Schnitt SJ, Vincent-Salomon A . Columnar cell lesions of the breast. Adv Anat Pathol 2003;10:113–124.
Beadling C, Heinrich MC, Warrick A et al. Multiplex mutation screening by mass spectrometry: evaluation of 820 cases from a personalized cancer medicine registry. J Mol Diagn 2011;13:504–513.
Ang D, O’Gara R, Schilling A et al. Novel method for PIK3CA mutation analysis: locked nucleic acid-PCR sequencing. J Mol Diagn 2013;15:312–318.
Lakhani SR, Slack DN, Hamoudi RA et al. Detection of allelic imbalance indicates that a proportion of mammary hyperplasia of usual type are clonal, neoplastic proliferations. Lab Invest 1996;74:129–135.
O'Connell P, Pekkel V, Fuqua SA et al. Analysis of loss of heterozygosity in 399 premalignant breast lesions at 15 genetic loci. J Natl Cancer Inst 1998;90:697–703.
Lakhani SR . The transition from hyperplasia to invasive carcinoma of the breast. J Pathol 1999;187:272–278.
Gong G, DeVries S, Chew KL et al. Genetic changes in paired atypical and usual ductal hyperplasia of the breast by comparative genomic hybridization. Clin Cancer Res 2001;7:2410–2414.
Jones C, Merrett S, Thomas VA et al. Comparative genomic hybridization analysis of bilateral hyperplasia of usual type of the breast. J Pathol 2003;199:152–156.
Xu S, Wei B, Zhang H et al. Evidence of chromosomal alterations in pure usual ductal hyperplasia as a breast carcinoma precursor. Oncol Rep 2008;19:1469–1475.
Reis-Filho JS, Lakhani SR . The diagnosis and management of pre-invasive breast disease: genetic alterations in pre-invasive lesions. Breast Cancer Res 2003;5:313–319.
Simpson PT, Gale T, Reis-Filho JS et al. Columnar cell lesions of the breast: the missing link in breast cancer progression? A morphological and molecular analysis. Am J Surg Pathol 2005;29:734–746.
Millikan R, Hulka B, Thor A et al. p53 mutations in benign breast tissue. J Clin Oncol 1995;13:2293–2300.
Done SJ, Arneson NCR, Ozcelik H et al. p53 mutations in mammary ductal carcinoma in situ but not in epithelial hyperplasias. Cancer Res 1998;58:785–789.
Kandel R, Li SQ, Ozcelik H et al. p53 protein accumulation and mutations in normal and benign breast tissue. Int J Cancer 2000;87:73–78.
Mao X, Fan C, Wei J et al. Genetic mutations and expression of p53 in non-invasive breast lesions. Mol Med Rep 2010;3:929–934.
Yang J, Ren Y, Wang L et al. PTEN mutation spectrum in breast cancers and breast hyperplasia. J Cancer Res Clin Oncol 2010;136:1303–1311.
Fuqua SA, Wiltschke C, Zhang QX et al. A hypersensitive estrogen receptor-alpha mutation in premalignant breast lesions. Cancer Res 2000;60:4026–4029.
Barone I, Cui Y, Herynk MH et al. Expression of the K303R estrogen receptor-alpha breast cancer mutation induces resistance to an aromatase inhibitor via addiction to the PI3K/Akt kinase pathway. Cancer Res 2009;69:4724–4732.
Nik-Zainal S, Van Loo P, Wedge DC et al. The life history of 21 breast cancers. Cell 2012;149:994–1007.
Liu P, Cheng H, Santiago S et al. Oncogenic PIK3CA-driven mammary tumors frequently recur via PI3K pathway-dependent and PI3K pathway-independent mechanisms. Nat Med 2011;17:1116–1120.
Tikoo A, Roh V, Montgomery KG et al. Physiological levels of Pik3ca(H1047R) mutation in the mouse mammary gland results in ductal hyperplasia and formation of ERalpha-positive tumors. PLoS One 2012;7:e36924.
Yuan W, Stawiski E, Janakiraman V et al. Conditional activation of Pik3ca(H1047R) in a knock-in mouse model promotes mammary tumorigenesis and emergence of mutations. Oncogene 2013;32:318–326.
Tomlinson DC, Baldo O, Harnden P et al. FGFR3 protein expression and its relationship to mutation status and prognostic variables in bladder cancer. J Pathol 2007;213:91–98.
Knowles MA . Role of FGFR3 in urothelial cell carcinoma: biomarker and potential therapeutic target. World J Urol 2007;25:581–593.
Zhang Z, Yamashita H, Toyama T et al. Estrogen receptor alpha mutation (A-to-G transition at nucleotide 908) is not found in different types of breast lesions from Japanese women. Breast Cancer 2003;10:70–73.
Tebbit CL, Bentley RC, Olson JA Jr et al. Estrogen receptor alpha (ESR1) mutant A908G is not a common feature in benign and malignant proliferations of the breast. Genes Chromosomes Cancer 2004;40:51–54.
Acknowledgements
A subset of this data was presented in abstract form at the San Antonio Breast Conference 6 December 2012 (cases with lobular neoplasia and lobular carcinoma). Mass spectroscopy and sequence data from 60 lesions comprise the validation cohort for a novel locked nucleic acid sequencing method, but were not further analyzed by any histologic or clinical parameter.28 The PIK3CA mutation frequency in 23 invasive carcinomas was cited as a comparator group in prior studies of special types of invasive breast carcinoma.20, 21 We acknowledge the expert technical skills of Jennifer Podolak, Dylan Nelson, and Linh Matsumura, as well as the computer graphical expertise of Alex Bolinder. Dr Robert West critically read the manuscript and provided helpful suggestions. This work was supported by a Susan G Komen Career Catalyst Grant (KG100112) to MLT.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Modern Pathology website
Supplementary information
Rights and permissions
About this article
Cite this article
C Ang, D., Warrick, A., Shilling, A. et al. Frequent phosphatidylinositol-3-kinase mutations in proliferative breast lesions. Mod Pathol 27, 740–750 (2014). https://doi.org/10.1038/modpathol.2013.197
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2013.197
Keywords
This article is cited by
-
Tall cell carcinoma of the breast with reversed polarity (TCCRP) with mutations in the IDH2 and PIK3CA genes: a case report
Molecular Biology Reports (2020)
-
PIK3CA mutations are common in lobular carcinoma in situ, but are not a biomarker of progression
Breast Cancer Research (2017)
-
Multiplexed imaging reveals heterogeneity of PI3K/MAPK network signaling in breast lesions of known PIK3CA genotype
Breast Cancer Research and Treatment (2016)