Abstract
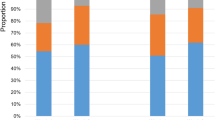
Sloughing esophagitis is characterized by superficial necrotic squamous epithelium and endoscopic plaques or membranes. According to abstract reports SE affects older, debilitated patients on multiple medications. This study seeks to evaluate the clinical findings in patients with SE. Thirty-one patients with necrotic superficial squamous epithelium, with endoscopic white plaques or membranes, but without fungi, were compared with 34 patients having esophageal biopsies done for any purpose other than Barrett's surveillance. Sloughing esophagits patients were older than controls (56 vs 43.5 years) and were more likely to be taking five or more medications (77 vs 32%), especially central nervous system depressants (65 vs 32%) and medications associated with esophageal injury (55 vs 18%). In 69% the plaques were in the distal and/or mid-esophagus; 23% involved the entire esophagus; 8% were limited to the proximal esophagus. There was no correlation between medication history and site. Sloughing esophagitis patients were likely to be debilitated based on evidence such as being on home oxygen, in nursing homes, bedridden, hospitalized, or malnourished, having metastatic cancer, organ transplantation, and/or being immunosuppressed. Sloughing esophagitis patients were more likely to have died since the biopsy (23 vs 3%), have peptic ulcer disease (55 vs 24%), or renal insufficiency (16% vs none), but no more likely to have dysmotility disorders, irritable bowel disease, or atherosclerosis. SE patients were less likely to have gastroesophageal reflux disease (45 vs 74%). No specific cause for sloughing esophagitis was identified, but the association with multiple drugs and conditions that may lead to esophageal stasis and/or injury, suggest that this is a local, perhaps contact injury, rather than an ischemic injury.
Similar content being viewed by others
Main
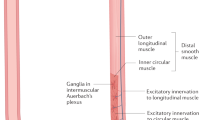
Superficial epithelial necrosis in the esophagus may have a variety of causes, including Candidiasis, pills that are direct irritants such as doxycycline and quinidine, and corrosive agents such as acids or alkalis.1, 2, 3, 4, 5, 6, 7, 8, 9 Some of these injuries produce endoscopic white plaques or membranes. There is one form of superficial esophageal necrosis that produces extensive, sometimes spectacular endoscopic membranes for which a specific cause has not been established, called ‘sloughing esophagitis.’ To our knowledge, sloughing esophagitis, defined in the manner described below, has been reported in detail only by a single group of investigators in two different abstracts describing first 4 and then 32 patients.10, 11 In these studies, patients with sloughing esophagitis most commonly had endoscopic white exudates or plaques in the mid and distal esophagus, while others had erosions, webs, and endoscopic esophagitis. Histologically, there was superficial eosinophilic, necrotic squamous epithelium, partially or completely detached from the underlying epithelium. A band of neutrophils with or without vacuoles in the interface between the necrotic and viable squamous cell layers was often present. In the larger study of 32 patients, the most common indications for endoscopy were upper gastrointestinal bleeding, dysphagia, and nausea and vomiting. Most patients were male and middle-aged, and about half were immunosuppressed. In addition, a recent paper describing a group of patients with esophagitis dissecans superficialis equates that diagnosis to sloughing esophagitis, although the inclusion criteria for that study are different from others’ criteria.12 We have recognized the sloughing esophagitis pattern of injury since reading the first report of four cases. We have now accumulated enough cases for analysis of the patient demographics and exposures that might help to define the cause or causes or, at the least, the predispositions.
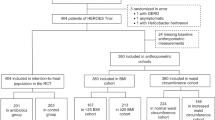
Materials and methods
Biopsies were studied that fulfilled two major criteria. First, the biopsy must have superficial epithelial necrosis or desquamation. Second, there had to have been endoscopic white plaques or membranes. Thirty-one cases meeting these criteria were identified by searching the University of Michigan surgical pathology archives, and these constitute the study set. An additional requirement for inclusion into the study was the absence of invasive Candidiasis. We scrutinized hematoxylin and eosin stained slides for fungal organisms, and all biopsies were negative. In addition, 11 of the cases with inflammation were stained with PAS/diastase, and all were again negative for fungi. The medical records of all patients were reviewed. We established the following criteria for a clinically debilitated state: inability to work/on disability, on home oxygen, residing in assisted living facility or nursing home, bedridden, hospitalized >1 month, currently hospitalized (at the time of biopsy), malnourished, metastatic cancer with or without current chemotherapy, and transplant in the preceding 6 months and/or on immunosuppressive therapy. The control group consisted of 34 consecutive patients having esophageal biopsies for any purpose other than Barrett's surveillance. Although the control patients were encountered over a short time interval compared with the sloughing esophagitis patients, most of the latter were recent biopsies, so it is likely that the background diseases in our patient population are a valid comparison with the study patients. Barrett's esophagus patients were excluded because the biopsies are performed on a schedule for surveillance, rather than as a response to symptoms, and little endoscopic information is recorded about the squamous mucosa. Data were analyzed using Fisher's exact test and unpaired t-test.
Results
Clinical Presentation
Among the sloughing esophagitis patients, there were 17 women and 14 men with a mean age of 58 years (range 32–85) (Table 1). The controls had a similar sex distribution, but a significantly younger mean age of 43 years (range 10–70) (P=0.0004). Fourteen sloughing esophagitis patients (45%) and 20 controls (59%) presented with esophageal symptoms, including dysphagia/globus sensation, odynophagia, non-cardiac chest pain, heartburn, regurgitation, or cough. The most common presenting esophageal symptom was dysphagia/globus sensation for both sloughing esophagitis patients (10/14 patients) and controls (11/20 patients). The next most common presenting symptom was nausea (10/31, 32%, and 8/34, 24%). There were not statistically significant differences between sloughing esophagitis patients and controls for any of these presenting symptoms.
Endoscopic Findings
By definition, all patients in this study had endoscopic white plaques or membranes (Figures 1 and 2). The locations of the white plaques or membranes were specifically stated in the endoscopy reports of 26 of the 31 sloughing esophagitis patients (Table 2). Distal esophageal location for the endoscopic abnormalities was significantly more common than other sites (P<0.002). When the middle or proximal esophagus was involved, it was generally part of diffuse endoscopic abnormalities, rather than as localized disease. Additional endoscopic findings were infrequent and nonspecific, and included erythema beneath the white membranes in two patients, rings in two patients, distal narrowing in one patient, nodular mucosa in one patient, hiatal hernias in four patients, an irregular Z-line in one patient, and distal salmon-colored mucosa that was not biopsied in one patient. One additional patient had a large esophageal diverticulum containing pill fragments.
Twelve controls (52%) had no esophageal endoscopic abnormality described. Five of these patients (42%) had an entirely normal upper endoscopy. Six of these controls (50%) had a normal esophagus endoscopically but had abnormalities in the stomach or duodenum. The endoscopic appearance of the esophagus of the remaining patient was not mentioned in the report but was presumed to be normal. Another 12 of the controls (35%) had some degree of endoscopic esophagitis. Two of these patients actually had membranes or plaques in the esophagus, but the sites were not specified in the endoscopy reports; one of these patients had a normal biopsy and the other had an ulcer. The endoscopic findings in the other 10 controls included suspected Barrett's esophagus, an irregular Z-line, furrows, rings, a tapered appearance or stricture, ectopic gastric mucosa, and an esophagogastric anastomosis.
Histologic Appearance
The abnormal esophageal squamous epithelium in all sloughing esophagitis biopsies had a two-toned appearance, with a superficial eosinophilic zone of necrosis (Figures 3 and 4). The nuclei in this upper layer varied from pyknotic (resembling parakeratosis of the skin) to faded (ghost nuclei). The underlying deeper squamous mucosa was either normal or appeared more basophilic due to basal cell hyperplasia. In some cases, the superficial eosinophilic and necrotic epithelium was completely separated from the underlying deep epithelium, present as separate strips on the glass slides (Figure 5). In 23 patients, these two layers in some cases were separated by a layer of neutrophils. When present, the neutrophilic infiltrate between the necrotic layers and the deeper layers of squamous epithelium varied from mild (a few intraepithelial neutrophils) to marked (multifocal microabscesses or more prominent neutrophil infiltration of squamous epithelium) (Figure 6). Of these 23 cases with sloughing and inflammation, 4/31 (13%) had mild, 11/31 (35%) had moderate, and 8/31 (26%) had severe inflammation. In eight cases, there was no inflammation. No fungi were present, as this was an exclusion criterion.
Twenty-five controls (74%) had a normal esophageal biopsy. Biopsy findings in the remaining nine controls included eosinophilic esophagitis, Barrett's esophagus, reflux changes, ulcer or acute inflammation, and a fibroepithelial polyp. None of the control patients had superficial epithelial necrosis. Controls and SE patients had a variety of endoscopic and biopsy findings in the stomach and duodenum that did not differ significantly between the two groups.
Medical History: Gastrointestinal Diseases
There were no significant differences between sloughing esophagitis patients and controls regarding history of most types of gastrointestinal diseases, including motility disorders, inflammatory bowel disease, upper gastrointestinal stricture, hiatal hernia, and history of esophagogastric, small bowel, or large bowel surgery (Table 3). Sloughing esophagitis patients were more likely than controls to have past or current peptic ulcer disease; whereas, controls were more likely to have gastroesophageal reflux disease or related symptoms.
Only five sloughing esophagitis patients (16%) had anatomic conditions of the type that predispose to pill-induced esophageal injury, such as left atrial enlargement due to valvular disease, aneurysm of the aortic arch, enlarged lymph nodes or carcinoma, an enlarged thyroid gland, entrapment by adhesions following thoracic surgery, an aberrant right subclavian artery, and osteophytes on the anterior aspect of the cervical vertebrae.
Medical History, Non-Gastrointestinal Diseases
None of the sloughing esophagitis patients had a history of bullous skin disease (Table 4). SE patients were more likely than all controls to have coronary artery disease (35 vs 12%), including angina or a history of myocardial infarct, or other cardiovascular disease (39 vs 9%), including congestive heart failure, valvular disease, or arrhythmias. SE patients were also more likely to have history of hypertension (61 vs 29%). Two patients had hypotensive episodes 3 days and 1 week before the biopsy, respectively. A third patient was admitted with hypotension and an infected lower extremity and had a guillotine amputation 5 days before biopsy. Sloughing esophagitis patients were also more likely than controls to have chronic renal disease or renal insufficiency (16% vs none). However, when sloughing esophagitis patients are compared with control patients aged 40 years and older, the prevalence of cardiovascular diseases becomes essentially equivalent, except that sloughing esophagitis patients are still more likely to have congestive heart failure and/or valvular heart disease, and much more likely to have chronic renal insufficiency, disorders that may make these patients more likely to take some of the medications known to injure the esophageal epithelium, discussed below. There is no difference in any of these groups in the prevalence of autoimmune, neurodegenerative, or malignant neoplastic diseases, and no differences in the proportions of patients taking antineopastic chemotherapy, immunosuppressive therapy, or having nutritional deficiencies.
Medication History
Twenty-four SE patients (77%, median age 67 years) were on five or more prescription medications at the time of esophageal biopsy, compared with 11 controls (32%, median age 46 years), a highly significant difference (Table 5). Two other SE patients were on three medications. Of the remaining five patients, four were on 1–2 prescription medications and for one patient, the medication history was unknown.
SE patients were significantly more likely than controls to be taking some type of central nervous system depressant capable of decreasing voluntary muscle control and affecting swallowing (65 vs 32%), such as a narcotic (52 vs 24%) or benzodiazepine (35 vs 9%). Nearly three times the number of SE patients (17/31, 55%) were on a medication known to cause esophageal injury (including iron, ASA, and KCl) compared with controls (6/34, 18%). In addition, SE patients were more likely than controls to be taking medications that cause dry mouth or interfere with swallowing (84 vs 47%). The most common prescription drugs were opioids (16 patients), selective serotonin reuptake inhibitors (13 patients), benzodiazepines (11 patients), and antiepileptics (9 patients). No SE patient or control had a history of caustic ingestion. When sloughing esophagitis patients were compared with control patients 40 years of age or older, only medications known to cause esophageal injury remains significantly different, as well as the proportion of patients taking five or more prescription medications.
Location of Endoscopic Plaques, Number of Medications, and Injury-Causing Medications
Nearly all of the sloughing esophagitis patients had their endoscopic disease involving the mid and/or distal esophagus (Table 6). Most of these patients were taking multiple medications, but that is not surprising, since most of all the study patients were taking multiple medications. Nearly all (10/13) of those in whom the mid-esophagus was involved, with or without other areas, were taking medications known to injure the esophageal mucosa, compared with less than half (5/11) of those with only distal esophageal disease. However, this difference was not statistically significant.
Clinical Features: Debilitation Status and Outcomes
Sloughing esophagitis patients were significantly more likely than control patients to live in an assisted living facility or nursing home, be bedridden, be currently hospitalized, or be immunosuppressed for transplantation or another reason (Table 7). Overall, sloughing esophagitis patients were significantly more likely than controls to have one or more features of debilitation (68 vs 21%), and 11 patients (35%) had two or more features (controls: 9%). When sloughing esophagitis patients are compared with controls older than age 40 years, current hospitalization and having any or multiple debilitation factors remain significantly more common in the study population.
There are too little data in the medical records of sloughing esophagitis patients to make meaningful observations about the natural history of the disease. Most often, no specific therapy followed the diagnosis of sloughing esophagitis, as it was and is a largely unknown entity. The patients’ clinical courses were dominated by the treatment and outcomes of their significant underlying diseases, for the most part. Five sloughing esophagitis patients had a least one follow-up esophageal biopsy, none of which had sloughing esophagitis. Three of these five patients had normal biopsies, including both patients who had repeated follow-up biopsies. One patient had lymphocytic esophagitis, and the other patient had mild reflux-type changes.
Sloughing esophagitis patients were more likely than controls to have died since the time of esophageal biopsy (23%, with a mean time to death of 116 days; controls: 3% with a time to death of 40 days). The causes of death were as varied as their complex medical histories.
Discussion
Using the definition outlined above, sloughing esophagitis has been previously described only by one other group in two abstracts, first in four patients and then in a total of 32 patients.10, 11 Similar to the present study, these abstracts reported endoscopic white exudates or plaques, mostly in the middle and distal esophagus, and sloughing epithelium or erosions. The histologic features described were also similar, consisting of squamous mucosa with a superficial eosinophilic, necrotic zone that partially or completely detached from the lower layers, imparting a ‘two-toned’ appearance to the tissue. Neutrophils were described at the junction of the necrotic and underlying epithelium. In some cases, polarizable material was associated with the sloughed mucosa. Almost certainly, these abstracts are describing the same lesion as the current study. The only differences between their cases and ours was a higher proportion of male patients (56 vs 32%) and immunosuppressed patients (56 vs 32%), differences that are not statistically significant (P=0.4536 and 0.0769).
A number of other conditions, both common and rare, come into the differential diagnosis of sloughing esophagitis. The most common of these is Candida esophagitis, a common condition that endoscopically appears as white plaques. Pseudohyphae and sometimes yeast forms are present within the superficial squamous epithelium. Corrosive injury to the esophagus from alkaline (lye) or acid ingestion also have endoscopic white membranes, edema, and hemorrhage. Histologically, necrosis and intense inflammation involve squamous epithelium but may extend deeper, even through the muscularis propria leading to perforation. Scar and strictures develop commonly following this severe injury.1, 2, 3
There is a rare entity known as acute esophageal necrosis, first described in 1990 in the endoscopic literature, that initially has patchy or diffuse pigmentation of the esophageal mucosa (‘black esophagus’). As early as 7 days later, however, this appearance is replaced by a thick white exudate and necrotic debris over an ulcer. The necrosis and extensive acute inflammation frequently extend into the submucosa and even deeper into the muscularis propria, and may be associated with fibrin thrombi within dilated capillaries in the lamina propria.4, 5, 6 Acute esophageal necrosis occurs in elderly patients with multiple underlying medical problems, and is thought to be caused by ischemia, as patients may also have ischemic colitis, recent surgical intervention, or hemodynamic instability. Its pathogenesis also involve gastric outlet obstruction resulting in reflux into the esophagus.4, 5, 6 Therefore, acute mucosal necrosis shares several features with sloughing, including older patient age, comorbidities, and location in the mid and lower esophagus, but it is a much deeper and more necrotizing disease than sloughing esophagitis. Acute esophageal necrosis patients and sloughing esophagitis patients are generally older and thus both groups are more likely to have advanced atherosclerotic disease, recent preceding surgical intervention or a period of hemodynamic instability leading to ischemia. However, only 3 of our 31 study patients had hypotensive events or surgery in the days before biopsy.
A recent report equates sloughing esophagitis with esophagitis dissecans superficialis, a rare entity that has been described sporadically over the past 70 years in a series of case reports.12 The 21 patients in the recent report included only 12 who fulfilled our criteria for SE, having both characteristic endoscopic and histologic features. The study also included as many as nine patients with ‘bacterial and fungal colonies.’ With no control group, a predominance of male patients from a Veterans Administration Health Center, and no clinical information for most patients, comparisons between that study and this one are not reasonably possible. It is likely that this description of esophagitis dissecans superficialis includes some patients with sloughing esophagitis. Esophagitis dissecans superficialis was described in the late 1800s, and is characterized endoscopically by a sloughed esophageal ‘cast’ or pearly white mucosa, which may have longitudinal and/or circumferential cracks and rings or ridges, resembling the features of sloughing esophagitis. The histologic features of esophagitis dissecans superficialis include detached fragments of normal squamous epithelium, and there may be a cleavage plane in the suprabasal squamous layers or occasionally between the basal cell layer and the lamina propria. Spongiosis is rare.13, 14 Most reports note paucity or even complete lack of inflammation, which is mostly mononuclear inflammation when it occurs. However, microabscesses around basal esophageal papillae have been reported.15, 16 In both sloughing esophagitis and esophagitis dissecans superficialis, there are desquamated squamous epithelium, with or without inflammation, but in esophagitis dissecans superficialis, there is generally no squamous epithelial necrosis or ulcers.14, 17 While focal parakeratosis has been described, no two-toned appearance, such as occurs in sloughing esophagitis, is mentioned.14 In contrast, in sloughing esophagitis patients, necrosis and/or two-toned epithelium was always present.
Esophagitis dissecans superficialis is thought to be secondary to injury to the esophageal mucosa (thermal, chemical, or physical), specifically from medications, hot beverages, caustic agents, alcohol, spicy foods, swallowing large amounts of food quickly, repeated forceful vomiting, Mallory–Weiss syndrome, esophageal sclerotherapy and nasogastric intubation, and medications such as bisphosphonates.18, 19, 20 Interestingly, one of the two patients reported in the literature with esophagitis dissecans superficialis due to bisphosphonates was a 90-year-old woman who was bedridden and had been taking alendronate while in bed.20 Esophagitis dissecans superficialis has also been observed in patients with strictures, severe infectious esophagitis, renal failure, and in association with various autoimmune bullous dermatoses, including pemphigus vulgaris and bullous pemphigoid, both of which have cleavage planes that are occasionally seen histologically in esophagitis dissecans superficialis. Alternatively, esophagitis dissecans superficialis may be idiopathic with no associated trauma or disease.13, 17 A wide age range with equal sex distribution is reported in the literature, and cases have been reported in healthy young adults, who often present with dysphagia or odynophagia or who rarely may vomit a membranous cast.13, 14, 15, 16, 17, 18, 19, 20, 21 Therefore, esophagitis dissecans superficialis shares with sloughing esophagitis the facts that both of them are intraepithelial abnormalities, both may be drug-related, and both may have endoscopic membranes. However, esophagitis dissecans superficialis seems, in some cases, to have associations that are not observed in sloughing esophagitis, and often has different histologic patterns and different clinical presentations. Perhaps, the cases that have been grouped together under the label esophagitis dissecans superficialis include esophageal injuries from diverse cases, including some cases of sloughing esophagitis along with other esophageal injuries.
It is well established that medications may injure the esophageal mucosa, and may cause endoscopic white membranes. Pill esophagitis, most common in the middle or distal esophagus, can be caused by doxycycline, quinidine, or other drugs, and histologically may have necrotic squamous epithelium, but there is also spongiosis and sometimes a prominent eosinophilic infiltrate. Desquamating mucosa in the lower two-thirds of the esophagus was described in a case of esophagitis due to the nonsteroidal anti-inflammatory drug celecoxib, a COX-2 inhibitor.8 Potassium chloride and alendronate (a bisphosphonate) may cause esophageal ulcers and strictures. Oral iron supplements may cause an erosive esophagitis with sloughed epithelium containing brown–black material, usually in older patients. Kayexalate (the sorbitol component mixed with it) may cause erosions or ulcers with rhomboid or triangular basophilic crystals that do not polarize, attached to surface epithelium or within exudates. In addition, Vitamin C supplements, methylxanthines such as theophylline, aspirin, acid-containing products (clindamycin, erythromycin, and tetracycline), zidovudine (AZT) and gluconate have been implicated in esophageal injury.
In the current study, sloughing esophagitis patients were significantly more likely than controls to be on multiple medications (77 vs 32%), including central nervous system depressants that may decrease voluntary muscle control and affect swallowing, and medications known to injure esophageal epithelium. The middle esophagus has traditionally been cited as the most common location. The increased medication use in the study population persists even when they are compared only to the older control patients, making drug-induced injury a likely candidate for the cause of at least some cases of sloughing esophagitis.
SE patients were significantly more likely than controls to have clinical features of chronic debilitation (68 vs 21%), and were more likely to have died in the interval between having the biopsy and this study. Debilitation may enhance the likelihood of a drug-induced esophageal injury by increasing the chance that patients will be taking multiple medications, and also by increasing the chance that patients may take their medications while recumbent.
Sloughing esophagitis appears to be acute, and possibly self-limited, because none of the five patients having subsequent esophageal biopsies still had sloughing.
Conclusion
Sloughing esophagitis is a unique condition, which has not been well characterized. Compared with controls, SE patients are more likely to be on multiple medications, including CNS depressants and those that directly injure the esophageal epithelium. They are also more likely to be chronically debilitated, and to have died between the time of the biopsy and the completion of this study. Coronary artery disease and other cardiovascular diseases are also more common in SE patients than controls, although this may be due to the fact that this is an older population, since the differences diminish when an older control population is used. However, we cannot exclude cardiovascular disease and ischemia as contributing factors. No specific cause for sloughing esophagitis was definitively identified, but it is likely that chronic debilitation, as well as certain medications such as CNS depressants, contribute to esophageal stasis, exacerbating the effect of other medications, including those known to injure esophageal mucosa. Although some ischemic component cannot be entirely excluded, the evidence is stronger for sloughing esophagitis being a local, perhaps direct contact injury, rather than an ischemic injury.
References
Alinejad A . Caustic injury to the upper gastrointestinal tract. SEMJ 2003;4, No. 1.
de Jong AL, Macdonald R, Ein S, et al. Corrosive esophagitis in children: a 30-year review. Int J Pediatr Otorhinolaryngol 2001;57:203–211.
Poley JW, Steyerberg EW, Kuipers EJ, et al. Ingestion of acid and alkaline agents: outcome and prognostic value of early upper endoscopy. Gastrointest Endosc 2004;60:372–377.
Augusto F, Fernandes V, Cremers MI, et al. Acute necrotizing esophagitis: a large retrospective case series. Endoscopy 2004;36:411–415.
Yamauchi J, Mitsufuji S, Taniguchi J, et al. Acute esophageal necrosis followed by upper endoscopy and esophageal manometry/pH test. Dig Dis Sci 2005;50:1718–1721.
Gurvits GE, Shapsis A, Lau N, et al. Acute esophageal necrosis: a rare syndrome. J Gastroenterol 2007;42:29–38.
Yasuda H, Yamada M, Endo Y, et al. Acute necrotizing esophagitis: role of nonsteroidal anti-inflammatory drugs. J Gastroenterol 2006;41:193–197.
Mantry P, Shah A, Sundaram U . Celecoxib associated esophagitis: review of gastrointestinal side effects from Cox-2 inhibitors. J Clin Gastroenterol 2003;37:61–63.
Parfitt JR, Driman DK . Pathological effects of drugs on the gastrointestinal tract: a review. Hum Pathol 2007;38:527–536.
Moore RJ, Lazenby AJ, Wilcox CM . Sloughing esophagitis: a distinct histologic and endoscopic entity. Mod Pathol 1999;12:81A.
Pugh JL, Moore RJ, Wilcox CM, et al. Sloughing esophagitis: a newly recognized clinicopathologic entity. Gastroenterol 2005;128 (Suppl 2):A636–A637.
Carmack SW, Vemulapalli R, Spechler SJ, et al. Esophagitis dissecans superficialis (‘Sloughing Esophagitis’). A clinicopathologic study of 12 cases. Am J Surg Pathol 2009;33:1789–1794.
Coppola D, Lu L, Boyce Jr HW . Chronic esophagitis dissecans presenting with esophageal strictures: a case report. Hum Pathol 2000;31:1313–1317.
Ponsot P, Molas G, Scoazec JY, et al. Chronic esophagitis dissecans: an unrecognized clinicopathologic entity? Gastrointest Endosc 1997;45:38–45.
Hage-Nassar G, Rotterdam H, Frank D, et al. Esophagitis dissecans superficialis associated with celiac disease. Gastrointest Endosc 2003;57:140–141.
Pérez-Carreras M, Castellano G, Colina F, et al. Esophagitis dissecans superficialis (esophageal cast) complicating esophageal sclerotherapy. Am J Gastroenterol 1998;93:655–656.
Schissel DJ, David-Bajar K . Esophagitis dissecans superficialis associated with pemphigus vulgaris. Cutis 1999;63:157–160.
Hokama A, Ihama Y, Nakamoto M, et al. Esophagitis dissecans superficialis associated with bisphosphonates. Endoscopy 2007;39 (Suppl 1):E91.
Beck RN . Oesophagitis dissecans superficialis. Br Med J 1954;1:501–502.
Cameron RB . Esophagitis dissecans superficialis and alendronate: case report. Gastrointest Endosc 1997;46:562–563.
Ramaswami G, Jain PK, Talati VR . Oesophagitis dissecans superficialis complicating repeated rigid oesophagoscopy and dilatation. J Laryngol Otol 2007;121:92–93.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Purdy, J., Appelman, H. & McKenna, B. Sloughing esophagitis is associated with chronic debilitation and medications that injure the esophageal mucosa. Mod Pathol 25, 767–775 (2012). https://doi.org/10.1038/modpathol.2011.204
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2011.204
Keywords
This article is cited by
-
Esophagitis unrelated to reflux disease: current status and emerging diagnostic challenges
Virchows Archiv (2018)
-
Esophagitis Dissecans Superficialis: Clinical, Endoscopic, and Histologic Features
Digestive Diseases and Sciences (2015)
-
Esophagitis dissecans superficialis
Indian Journal of Gastroenterology (2015)
-
Esophageal leukoplakia or epidermoid metaplasia: a clinicopathological study of 18 patients
Modern Pathology (2014)