Abstract
Increased numbers of T regulatory (Treg) cells are found in B-chronic lymphocytic leukemia, but the nature and function of these Tregs remains unclear. Detailed characterization of the Tregs in chronic lymphocytic leukemia has not been performed and the degree of heterogeneity of among these cells has not been studied to date. Using 15-color flow cytometry we show that Treg cells, defined using CD4, CD25, and forkhead box P3 (FOXP3), can be divided into multiple complex subsets based on markers used for naïve, memory, and effector delineation as well as markers of Treg activation. Furthermore FOXP3+ cells can be identified among CD4+CD25− as well as CD8+CD4− populations in increased proportions in patients with chronic lymphocytic leukemia compared with healthy donors. Significantly different frequencies of naïve and effector Tregs populations are found in healthy donor controls compared with donors with chronic lymphocytic leukemia. A population of CCR7+CD39+ Tregs was significantly associated with chronic lymphocytic leukemia. This population demonstrated slightly reduced suppressive activity compared with total Tregs or Tregs of healthy donors. These data suggest that FOXP3-expressing cells, particularly in patients with chronic lymphocytic leukemia are much more complex for Treg sub-populations and transitions than previously reported. These findings demonstrate the complexity of regulation of T-cell responses in chronic lymphocytic leukemia and illustrate the use of high-dimensional analysis of cellular phenotypes in facilitating understanding of the intricacies of cellular immune responses and their dysregulation in cancer.
Similar content being viewed by others
Main
Chronic lymphocytic leukemia is one of the most common leukemias in adults in the Western hemisphere and is characterized by a slow, progressive accumulation of monoclonal B lymphocytes. Among patients with chronic lymphocytic leukemia, the progress of disease and response to therapy varies greatly for largely unknown reasons. Although chronic lymphocytic leukemia is a disease of B lymphocytes, a number of abnormalities in the T-lymphocyte compartment of the immune system have previously been described in patients, suggesting that an altered immune response occurs in response to the leukemia, or is a causal factor in the escape of the leukemic cells from normal immune recognition (Table 1).1, 2, 3, 4, 5, 6, 7, 8 Among the observed T-cell alterations is the intriguing finding of elevated frequencies of T regulatory (Treg) cells in the peripheral circulation of patients with chronic lymphocytic leukemia.5, 7, 8, 9, 10
Natural Treg cells in humans are most often characterized as CD4+ T cells with high expression of CD25 and the transcription factor forkhead box P3 (FOXP3), a master regulator of Tregs. Tregs are also generally agreed upon to demonstrate a phenotype of CTLA-4+, CD62L+, CD127low, and GITR+.11, 12 In the peripheral circulation of healthy adults and elderly individuals, the majority of Tregs express CD45RO, and are termed as effector Tregs, which might reflect differentiation of either natural Tregs derived from the thymus or induced Tregs derived from memory cells in the peripheral circulation.13, 14, 15, 16 CD45RA+ Tregs predominate in cord blood, but persist into adulthood, where they represent a minority of Tregs in the peripheral circulation.17 The percentage of CD45RA expressing Tregs decreases with increasing age in adults.18 A number of other Treg subsets have been described by the expression of various markers. Some of these have been associated with increased Treg suppressive activity, including CD39, HLA-DR, and CD103.
Using CD4+CD25high expression to identify Tregs, Beyer et al5 found increased percentages of Treg in chronic lymphocytic leukemia compared with age-mismatched healthy donors, and noted a correlation between the frequency of Tregs and stage of disease using the Binet staging classification. Giannopoulos et al6, 10 similarly noted an increase in the percentage of Tregs in chronic lymphocytic leukemia using CD4+CD25highFOXP3 to identify Tregs. Although they also found a correlation between the frequency of Tregs and Binet stage, they found no significant correlation with ZAP-70 or CD38. Using CD4+CD25brightCD127low to identify Tregs, Jak et al7 found an increase in the absolute number of Tregs in chronic lymphocytic leukemia and reported that the percentage of Tregs increase with increasing stage of disease using the Rai classification. This group also reported a predominance of CD45RO+ Tregs in these patients, suggesting that these cells arise from the memory T-cell pool in a CD70-dependent manner and accumulate due to reduced apoptosis.7 Recently, Weiss et al,19 using CD3+CD4+CD25+CD127− to identify Tregs, found a significant elevation of percentage of Tregs in chronic lymphocytic leukemia compared with age-mismatched healthy control donors. This group further determined that Tregs are an independent predictor of time to initial treatments in these patients. In the study by Weiss et al,19 the percentage of Tregs correlated with unmutated IgVH, high CD38 expression, as well as specific cytogenetic findings.
It is thought that Tregs facilitate progression of disease in chronic lymphocytic leukemia, as well as in solid tumors, by suppressing T-cell anti-tumor responses.20 In chronic lymphocytic leukemia, therapy with fludarabine, thalidomide, or lenalidomide has been reported to reduce the frequency, and limit the function, of Tregs in these patients,5, 6 suggesting the efficacy of these therapies might be due at least in part to effects on Tregs. Chronic lymphocytic leukemia is also strongly associated with a progressive immunodeficiency in these patients and it has also been speculated that Tregs arising in this disease might be a cause of the autoimmune complications.21 Tregs found in chronic lymphocytic leukemia patients neither have been characterized in any great detail nor have definitive reasons for their increased frequency in chronic lymphocytic leukemia been delineated.
In the current study, high-resolution phenotyping of T-cell subsets and characterization of Treg sub-populations in the circulation of chronic lymphocytic leukemia was accomplished using the 15-color immunophenotyping that included markers to identify Tregs as well as those reported to be associated with naïve, memory, and suppressive activity in T cells. This permits more rigorous examination of Tregs to discern complex phenotypes that may differ from those of healthy donors or that may correlate with progressive disease or the mutational status of the malignant population in chronic lymphocytic leukemia. Using probability state modeling (PSM)22, 23, 24 these complex Treg phenotypes were then analyzed to better understand marker correlations defined by the high-dimensional data. A selected Treg subset identified in this manner was sorted and assayed for suppression of autologous T-cell responses.
Materials and methods
Patient Samples
Peripheral blood specimens from 21 patients with B-chronic lymphoid leukemia and 16 age-matched healthy donors were studied. Peripheral blood from healthy donors enrolled in the NHLBI study 09-H-0201 and 09-H-0229 was collected into vacutainer tubes containing sodium heparin. Written informed consent for all procedures and research collections was obtained. Peripheral blood mononuclear cells (PBMCs) were isolated by density gradient centrifugation over Lymphocyte Separation Medium (LSM, ICN Biomedicals, Aurora, OH). Cells were viably frozen and kept in fetal calf serum containing 10% dimethyl sulfoxide and stored in liquid nitrogen. Peripheral blood was collected from treatment naïve chronic lymphocytic leukemia patients with RAI scores of 2 or less enrolled in the NCI study 97-C-0178 (ClinicalTrials.gov Identifier: NCT00019370) (Table 2). Mononuclear cells were isolated and viably frozen in a similar manner to the healthy donor cells. For all chronic lymphocytic leukemia patients, data were collected on whether the tumor cells expressed a mutated (m-chronic lymphocytic leukemia) or an unmutated IgVH gene (u-chronic lymphocytic leukemia), as well as expression of CD38 and ZAP-70, to serve as markers of a more indolent disease and longer overall survival.25, 26
Flow Cytometry
Single-cell suspensions from viably cryopreserved samples were thawed and washed once in PBS. After washing, cells were incubated for 30 min in presence of LIVE/DEAD Aqua fixable viability dye (Invitrogen, Carlsbad, CA), followed by a wash in staining buffer (PBS supplemented with 2% normal mouse serum (Gemini Bioproducts, West Sacramento, CA)). To determine the proportion of Tregs, we stained the cells with a 13-color combination of the following monoclonal antibodies: anti-CD3APC−Cy7, anti-CD4V450, anti-CD38PerCP−Cy5.5, anti-CD25PE−Cy−7, anti-CD127APC (Becton Dickinson, San Jose, CA), anti-CD45Qdot800, anti-CD8Qdot605, anti-CD27Qdot655, anti-HLA-DRPE−Cy5.5, anti-CD39FITC, anti-CD103PE−Cy5 (Invitrogen, Eugene, OR), anti-CD45-RAPE−TR (Beckman Coulter, Miami, FL), anti-CCR7Alexafluor700 (R&D Systems, Minneapolis, MN). After cell surface staining, the cells were permeabilized with eBioperm buffer (eBioscience, San Diego, CA) and stained with anti-FOXP3 PE (eBioscience, clone PCH101). After staining, cells were washed, fixed in PBS containing 2% formaldehyde, and acquired on an LSRII flow cytometer equipped with 405, 488, 532, and 638 laser lines using DIVA 6.1.2 software (Becton Dickinson). Data were analyzed with the FlowJo software version 8.8.6 (Treestar, San Carlos, CA) and by the GemStone probability state modeling software (Verity Software House, Topsham, ME). Lymphocytes were identified according to their light-scattering properties (Figure 1a) and then analyzed gated on viable cells and CD45+ events. In CD4+ and CD8+ cells, four sub-populations could be defined, according to a consensus among several publications,27, 28, 29 as follows: naïve cells (CD45RA+), central memory (CM) cells (CD45RA−CD27+CCR7+), effector memory (EM) cells (CD45RA−CD27+CCR7−), and effector cells (EC) (CD45RA−CD27−CCR7−). Conventional Treg cells were defined as viable CD45+CD3+CD8−CD4+CD25+FOXP3+ mononuclear cells (Figure 1a). Among the Treg population, as previously performed for CD4 and CD8 cells, we identified naïve Treg (CD45RA+), CM Treg (CD45RA−CD27+CCR7+), EM Treg (CD45RA−CD27+CCR7−), and effector Treg (CD45RA−CD27−CCR7−).
Gating strategy to identify T regulatory (Tregs) population in chronic lymphocytic leukemia patients and CD4 and CD8 characterization. Single-cell suspensions from chronic lymphocytic leukemia were stained with a combination of 14 antibodies and a viable dye as described in Materials and methods. (a) Lymphocytes were identified based on their forward- and side-scatter properties. Subsequently, dead cells were excluded through the use of a viability dye. CD45 and CD3 were used to identify T cells (CD45+CD3+) among the previously selected viable lymphocytes. CD4 T cells and CD8 T cells were identified as uniquely expressing CD4 or CD8 antigens. Conventional Tregs were defined as CD4 T cells co-expressing CD25 and transcription factor forkhead box P3 (FOXP3). CD127 expression was measured in FOXP3-expressing cells. CD25− Tregs were defined as CD4+FOXP3+CD25− T cells. CD8 Tregs were defined as CD8+CD25+FOXP3+ T cells. In addition to Tregs memory and naïve compartment of CD4 and CD8 was described. The graphs display the percentages (the mean percentage values ±s.e.m. are indicated by the bars) of naïve vs memory sub-population CD4 T cells (b) and CD8 T cells (c) in healthy donors (black circle) and chronic lymphocytic leukemia (gray square). (d) A probability state model constructed with GemStone (Verity Software House) was applied to CD4 T cells and CD8 T cells from healthy donors and from chronic lymphocytic leukemia. For these displays, the data were gated on light scatter, viability, and expression of CD45, CD3, and either CD4 or CD8 as described earlier. The y-axis is relative fluorescence intensity, whereas the x-axis displays staged progression from naïve to memory (CM, EM) and effector (EC) compartments. The width of each stage (naïve, EM, CM, EC) indicates the percentage of cells falling into these categories. The width of the bands corresponds to the variability of the data as the cells progress. These graphs reveal the same proportions of memory and naïve subsets as in the previous figures, although here it is possible to visualize relative intensity of marker expression along with putative transitions among these populations.
Cell Sorting of Tregs
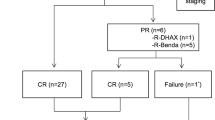
PBMCs were isolated by density gradient centrifugation over LSM. Cells were stained with the following antibodies: CD3, CD4, CD25, CCR7, and CD39. According to Baecher-Allan et al,30, 31 CD4+CD25high is an appropriate gate for sorting viable Tregs without using FOXP3 staining. Three populations were sorted using a FACS Aria flow cytometer (Becton Dickinson): CD4+CD25− (Teffec), CD4+CD25high (Treg), and CD4+CD25highCD39+CCR7+ (TregDP) (Figure 3c). Subsequently, autologous CD3−HLA-DR+ cells were sorted from gamma-irradiated PBMCs (4000 Rad) to use as antigen-presenting cells (APCs).
CFSE Labeling and Treg Suppression Assay
Treg-mediated suppression assay was performed accordingly to Venken et al.32 CD4+CD25− cells (Teffec) were labeled using 2.5 μM CFSE (Cell trace CFSE cell proliferation kit, #C34554, Invitrogen) in PBS for 10 min at 37 °C. Cells were subsequently washed with RPMI supplemented with 10% heat-inactivated human AB serum (Sigma-Aldrich, St Louis, MO) and 1 × antibiotic and anti-mycotic solution (Invitrogen). For the suppression assay, 50 000 Teffec cells were incubated with 50 000 APCs and differing amounts (where Teffec:Treg=1:0, 1:1, 1:0.2) of various sorted Treg cell subsets in a 96-well flat bottom cell culture plate. Cultures were stimulated with mouse anti-human-CD3 antibody (Clone Okt-3, eBioscience) for 72 h at 37 °C in a humidified CO2 chamber. Dilution of CFSE stain was read using an LSRII Flow cytometer (BD Biosciences) and data were analyzed using the FlowJo software (Treestar). Suppressive capacity of Treg toward Teffec cells was expressed as the relative inhibition of the percentage of CFSE-low cells according to the following formula; [100 × (1−(y/x))], where x=percentage of CFSE-low cells in Teffec alone culture and y=percentage of CFSE-low cells in Teffec:Treg culture32 (Figure 3d).
Statistical Analysis
Data obtained with cells from one donor were considered as one experiment (n). Statistical analysis performed on the results included the calculation of mean, s.e., and P-values by use of a multiple comparison test (two-way ANOVA test) or Mann–Whitney test (non-parametric t-test). Correlations between parameters were calculated using the Spearman's correlation, and Spearman's r factor was reported. The significance level was set at P=0.05, and the P-values were given for each series of experiments.
Results
Assessment of CD4+ and CD8+ T-Cell Subsets
The initial analysis of these data was carried out to determine whether there were differences in the frequencies of CD8+ and CD4+ T cells in patients with chronic lymphocytic leukemia compared with healthy donors. Among T cells, the percentage of CD4+ cells was slightly lower in chronic lymphocytic leukemia patients compared with healthy donors but did not reach statistical significance: 47.4±3.8% vs 58.5±3.9% (P=0.08). The percentage of CD8+ T cells in chronic lymphocytic leukemia and healthy donors was similar: 31.4±1.3% in chronic lymphocytic leukemia vs 36.1±3.7% in healthy donors (P=0.2). The CD4 to CD8 ratio was similar in both groups: 2.23±0.4 in chronic lymphocytic leukemia and 2.1±0.2 in healthy donors (P=0.84; data not shown). Double-negative CD4−CD8− T cells were significantly increased in the chronic lymphocytic leukemia; 19.6±11% compared with 4.3±3.6% in healthy donors (P<0.0001).
Among CD4+ and CD8+ T cells, the proportions of naïve, EC, CM and EM cells (as described in Materials and methods) were measured (Figures 1b–d). The frequency of naïve CD4+ population was increased in chronic lymphocytic leukemia, representing 34.4±4.1% vs 24.4±3.6% in healthy donors (P=0.06; Figure 1b), whereas the proportion of naïve CD8+ was unchanged: 45.4±4% in chronic lymphocytic leukemia vs 38.2±3.5% in healthy donors (P=0.27; Figure 1c). A lower frequency of CD4+ ECs was observed in blood from chronic lymphocytic leukemia patients compared with healthy donors (8.8±2.1% vs 16.8±3.6%, P=0.03), but the proportion of CD8+ ECs was unchanged. By contrast, the frequency of CM CD4+ T cells was higher in chronic lymphocytic leukemia compared with healthy donors (11.8±2.4% vs 5.9±1.1%, P=0.05) and the frequency of CM CD8+ T cells was lower in chronic lymphocytic leukemia compared with healthy donors (0.3±0.09% vs 2.2±0.5%, P=0.0001; Figure 1c). Among both CD8+ T cells and CD4+ T cells, the proportion of EM cells was unchanged.
Tregs and Treg Memory and Naïve Sub-populations
The percentage of natural (viable CD45+CD3+CD8−CD4+CD25highFOXP3+) Treg cells was significantly higher in chronic lymphocytic leukemia patients compared with healthy donors (12.8±1.3% vs 5.4±0.4%, P<0.0001; Figure 2a). Flow cytometric analysis confirmed that the majority of Tregs in healthy donors was CD45RA− (90.6±1.7%), whereas in chronic lymphocytic leukemia patients, Treg cells were found in both CD45RA− and CD45RA+ populations. In chronic lymphocytic leukemia, naïve Treg cells were significantly expanded compared with healthy donors (43.5±4.7% vs 11.9±1.4%, P<0.0001; Figure 2b). Among the CD45RA− populations, Treg cells identified as EM (CD45RA−CCR7−CD27+) were decreased in chronic lymphocytic leukemia compared with healthy donors (37.4±4.4% vs 77.7±1.2%, P<0.0001; Figure 2c). The frequency of CM (CD45RA−CCR7+CD27+) Treg was unchanged (8.6±1.3% in chronic lymphocytic leukemia vs 5±0.7% in healthy donors, P=0.62; Figure 2d). The proportion of effector Treg cells was reduced in chronic lymphocytic leukemia compared with healthy donors (1.7±0.4% vs 7.6±1.1%, P<0.0001; Figure 2e).
Conventional T regulatory (Tregs), memory vs naïve subtypes and expression of activation markers in healthy donors and chronic lymphocytic leukemia. Cells were stained as described in Materials and methods and analysis was performed to identify conventional Tregs. (a) Percentages and the mean percentage values (±s.e.m.) of CD4 Tregs in healthy donors (black) and chronic lymphocytic leukemia (gray). (b) Percentages and the mean percentage values (±s.e.m.) of naïve Tregs in healthy donors (black) and chronic lymphocytic leukemia (gray) identified as CD45RA+ cells among Tregs. (c) Percentages and the mean percentage values (±s.e.m.) of effector memory (EM) Tregs identified as CD27+CCR7− cells among Tregs in healthy donors (black) and chronic lymphocytic leukemia (gray). (d) Percentages and the mean percentage values (±s.e.m.) of central memory (CM) Tregs identified as CD27+CCR7+ cells among Tregs in healthy donors (black) and chronic lymphocytic leukemia (gray). (e) Percentages and the mean percentage values (±s.e.m.) of effector Tregs identified as CD27−CCR7− cells among Tregs in healthy donors (black) and chronic lymphocytic leukemia (gray). (f) Percentages and the mean percentage values (±s.e.m.) of Tregs expressing activation markers CD38, CD39, CD103, CD127, and HLA-DR were measured in healthy donors (black) and chronic lymphocytic leukemia (gray).
High-Resolution Immunophenotyping of Treg Cells
To further characterize the phenotype of natural (viable CD45+CD3+CD8−CD4+CD25highFOXP3+) Treg cells present in chronic lymphocytic leukemia and healthy donors, the cell surface expressions of HLA-DR, CD38, CD103, and CD39 were measured (Figure 2f). The frequencies of Tregs expressing CD38, HLA-DR, or CD103 were not significantly different between healthy donors and chronic lymphocytic leukemia. Nevertheless, another activation marker, CD39, was increased in Tregs from chronic lymphocytic leukemia patients compared with healthy donors (66.5±5% and 49.1±5.9%, respectively, P=0.01). In healthy donors, natural Tregs are CD127low (Figure 1b),11 but CD127 expression in chronic lymphocytic leukemia Tregs was increased (27.8±3.1% in chronic lymphocytic leukemia vs 8.2±1.1% in healthy donors, P<0.0001).
In addition to examining expression of activation markers in the overall Treg population, a combination of these activation markers was examined. In chronic lymphocytic leukemia, a significant increase of the double-positive CD39+ CCR7+ Treg population was observed compared with healthy donors (37.8±5% and 4.1±0.7%, respectively, P<0.001). Consequently, the double-negative Treg population was lower in chronic lymphocytic leukemia than in healthy donors (32.9±4.3% and 48.8±5.6%, respectively, P<0.001). Figure 3 shows representative dot plots of the expression of CD39 vs CCR7 in a healthy donor (Figure 3a) and in a chronic lymphocytic leukemia (Figure 3b). In chronic lymphocytic leukemia, the dual-positive CD39+CCR7+ Tregs were primarily CD45RA+: 86.5±3.5% compared with 5.9±2% in healthy donors (P<0.001).
Co-expression of CD39 and CCR7 in conventional T regulatory (Tregs) in healthy donors and chronic lymphocytic leukemia and autologous Treg-mediated suppression of polyclonal T-cell responses from healthy donors and chronic lymphocytic leukemia. Conventional Tregs were identified after staining as described earlier. Expression of the activation markers CD39 and CCR7 were measured. (a) Representative dot plot of CD39 and CCR7 co-expression pattern on conventional Tregs in a healthy donor (left panel) and chronic lymphocytic leukemia (right panel). (b) Histograms of the mean percentages (±s.e.m.) of Tregs expressing these markers in healthy donors (black) and chronic lymphocytic leukemia (gray). (c) Tregs were isolated using flow cytometric sorting as described earlier. Expression of CD25 and CD4 were used to identify Treg cells in both healthy donors and in chronic lymphocytic leukemia. A representative dot plot of CD39 and CCR7 expression pattern in a healthy donor (upper panel) and chronic lymphocytic leukemia (lower panel). (d) Suppressive capacity of Tregs toward responder cells (Teffec) was expressed as relative inhibition of the percentage of CSFE-low cells.
The same activation markers were studied among the memory/naïve Treg sub-populations (Table 3). A different pattern of activation was observed among the Treg in chronic lymphocytic leukemia patients: naïve Treg expressed more CD38, CD39, CD127, and HLA-DR compared with healthy donors (two- to threefold increase, P<0.0001). In the CM Treg sub-population, HLA-DR expression was significantly decreased in chronic lymphocytic leukemia patients (P<0.0001). In the EM Treg sub-population, CD127 and HLA-DR expression was lower in chronic lymphocytic leukemia patients compared with healthy donors; conversely, CD38 expression was higher in chronic lymphocytic leukemia compared with healthy donors. Finally, in the effector Treg sub-population, HLA-DR expression was significantly decreased in chronic lymphocytic leukemia patients (P=0.006), and CD38 was also decreased (P=0.003).
Analysis of Treg-Mediated Suppression of Polyclonal T-Cell Responses
To evaluate the in vitro suppressive capacity of Tregs toward responder Teffec cells, CD4+CD25high T cells (Treg) and CD4+CD25− T cells (Teffec) were sorted from seven healthy donors and five chronic lymphocytic leukemia patients (Figure 3c). Subsequently, the sorted cells were used to setup an autologous coculture assay as described in Venken et al.32 Fifty thousand CFSE-labeled CD4+CD25 T cells (responder cells (Teffec)) were cocultured with varying amounts of CD4+CD25+ T cells (Treg; ratio 1:0, 1:0.2, and 1:1) and stimulated with soluble anti-CD3 antibody in the presence of 105 irradiated autologous CD3−HLA-DR+PBMCs. To determine the undivided peak fluorescence (Figure 3d), CFSE-labeled CD4+CD25 T cells (Teffec) were also cultured in the absence of anti-CD3 antibody (Figure 3d, unstimulated). Cells were subsequently analyzed for CFSE by flow cytometry. In healthy donors, CD4+CD25+ Treg cells suppressed the proliferation of autologous responder cells in coculture in a dose-dependent manner, the mean relative inhibition for Teffec/Treg ratio 1:1 was 22±7.1% for healthy donors. Among the chronic lymphocytic leukemia patients the mean suppression at a 1:1 Tresp/Treg ratio was 16.4±2%. The difference between the mean suppression in healthy donors and in chronic lymphocytic leukemia for Teffec/Treg ratio 1:1 was not significant (P=0.43). In healthy donors, there are virtually no CD39+CCR7+ Tregs, thus, we were not able to sort this specific population for the proliferation assay experiment, and it was impossible to perform this control. In chronic lymphocytic leukemia, the relative inhibition of CD39+CCR7+ Treg was measured as performed for total Treg, and was compared with the suppression obtained by the total Treg population in chronic lymphocytic leukemia. A trend to slightly less suppression was observed in this Treg sub-population compared with the total Treg population in chronic lymphocytic leukemia (1:1 mean suppression=12.5±1.2%, (P=0.59)). Comparing the mean suppression of CD39+CCR7+ Treg with total Treg in healthy donors, showed a trend to a lower suppressive capacity, 12.5±1.2%, vs 22±7.1%, but did not reach significance (P=0.24).
PSM of CD4+ and CD8+ T-Cell Subsets in Healthy Donors and Chronic Lymphocytic Leukemia
Understanding the relationship of multiple markers to each other using bivariate plots and Boolean gating is difficult, particularly when attempting to evaluate 15-color immunophenotyping. To better understand these data, probability state models were constructed for CD4+ and CD8+ T cells in healthy donors and in chronic lymphocytic leukemia (Figure 1d). The use of these models emphasized the difference in the relative intensity of each marker in all populations from healthy donors and chronic lymphocytic leukemia, allowing an understanding of the behavior of each marker at through the progression to maturation. These models display intensity and frequency as a continuum for each marker studied to show the progression of CD4+ or CD8+ T cells from naïve to memory and ECs. The discrimination between memory and naïve population was performed according to the gating described in Materials and methods. Figure 1d shows a comparison of the Ag-dependent partitioning of events as determined by CD45RA, CD197, and CD27 marker downregulations in both CD4+ T cells (left panels and CD8+ T cells right panels) using data from a single donor. For CD4+ T cells, the healthy donor's naïve, CM, EM, and EC fractions were 24.9%, 5.6%, 61%, and 8.8%, respectively. The chronic lymphocytic leukemia fractions were 13%, 10%, 67.3%, and 9.7%, respectively. For CD8+ T cells, the healthy donor's naïve, CM, EM, and EC fractions were 37.6%, 3.7%, 53.6%, and 5.1%, respectively. The chronic lymphocytic leukemia fractions were 36.2%, 1.9%, 52.4%, and 10.6%, respectively. The chronic lymphocytic leukemia patient had decreased naïve and CM phases as well as increased EM and EC phases compared with the healthy donor patient.
PSM of Tregs Cells in Healthy Donors and Chronic Lymphocytic Leukemia
To simplify and better understand the complex relationship of marker expressions among Treg populations, PSMs were designed for Treg cells as described in a previous section (Figure 4a). An increase in the proportion of naïve Treg cells was observed in chronic lymphocytic leukemia patients compared with healthy donors. Activation markers such as CD39, CD38, and HLA-DR presented a higher relative intensity in chronic lymphocytic leukemia patients compared with healthy donors (Figures 4b–d). CD25 and CD127 presented a different pattern of expression in the EM Treg compartment (Figure 4e).
Probability state modeling of T regulatory (Treg) populations in healthy donors and chronic lymphocytic leukemia. Probability model of activation markers expression in conventional Tregs in a healthy donor (left panel) and chronic lymphocytic leukemia (right panel). For these models, the data were gated on light scatter, viability, and expression of CD45, CD3, CD4, CD25high, and FOXP3 as described earlier. The y-axis is relative fluorescence intensity, whereas the x-axis displays staged progression from naïve to memory and effector populations. The width of each stage (naïve, CM, EM, EC) indicates the percentage of cells falling into these categories. The width of the bands corresponds to the variability of the data as the cells progress. These graphs reveal the coordinate expression patterns of memory and naïve markers (a) as well as activation markers through the transitions (b, c and d). Panel e reveals the expression of all markers among the conventional Treg cells in a coordinated manner, with intensities of all markers revealed through the transitional steps.
FOXP3 Expression in CD4+CD25− T Cells in Chronic Lymphocytic Leukemia Patients
During the evaluation of the numbers of Treg cells in healthy donors and in chronic lymphocytic leukemia patients, it was noted that among the CD4+ T-cell population (Figure 1a) there was a cell population expressing FOXP3 but not CD25 (CD4+FOXP3+CD25−). The percentage of these CD25− FOXP3+ was significantly increased in chronic lymphocytic leukemia patients compared with healthy donors (4±1% vs 1.45±0.1%, P=0.0015; Figure 5a). As for natural Tregs, the proportion of naïve, EC, CM and EM cells was determined for the CD4+FOXP3+CD25− cells in chronic lymphocytic leukemia (Figure 5b). In chronic lymphocytic leukemia patients, 29.9±4.5% of CD4+FOXP3+CD25− cells were naïve, but the majority of these CD4+FOXP3+CD25− cells did not express CD45RA (70.1±4.5%). Among CD4+FOXP3+CD25− cells, EM cells were predominant (57.8±5.4%), followed by CM (9.3±1.4%), and ECs (2.9±0.6%).
CD4+CD25−Tregs and CD8 Tregs, their memory vs naïve subtypes, and their activation status in healthy donors and chronic lymphocytic leukemia. Cells were stained with antibodies and analysis was performed to identify CD25−Tregs and CD8 Tregs as described earlier. (a) The graphs display the percentages and the mean percentage values (±s.e.m.) of CD25−Tregs in healthy donors (black) and chronic lymphocytic leukemia (gray). (b) The graphs show the percentages and the mean percentage values (±s.e.m.) of central memory (CM) CD25−Tregs (identified as CD27+CCR7+ cells among CD45RA−CD25−Tregs), of effector memory (EM) CD25−Tregs (identified as CD27+CCR7− cells among CD45RA−CD25−Tregs), of effector CD25−Tregs (identified as CD27−CCR7− cells among CD45RA−CD25−Tregs), and naïve CD25−Tregs (identified as cells among CD25−Tregs). (c) The graphs display the mean percentage values (±s.e.m.) of CD25−Tregs expressing activation markers CD38, CD39, CD103, CD127, and HLA-DR in healthy donors (black) and chronic lymphocytic leukemia (gray). (d) The graphs represent the percentages and the lines indicate the mean percentage value (±s.e.m.) of CD8 Tregs in healthy donors (black) and chronic lymphocytic leukemia (gray). (e) The graphs show the percentages and the lines indicate the mean percentage value (±s.e.m.) of CM CD8 Tregs (identified as CD27+CCR7+ cells among CD45RA−CD8 Tregs), of effector memory (EM) CD8 Tregs (identified as CD27+CCR7− cells among CD45RA−CD8 Tregs), of effector CD8 Tregs (identified as CD27−CCR7− cells among CD45RA−CD8 Tregs), and naïve CD8 Tregs (identified as CD45RA+ cells among CD8 Tregs).
A trend toward a higher expression of CD127 among the CD4+FOXP3+CD25− cells was observed in chronic lymphocytic leukemia patients compared with healthy donors (24.2±3.4% in chronic lymphocytic leukemia vs 3±0.4% in healthy donors (P<0.001)) and lower expressions of the activation marker HLA-DR was observed compared with healthy donors (52±3.4% in healthy donors vs 32.6±4.8% in chronic lymphocytic leukemia, P<0.001; Figure 5c). No significant differences were observed between healthy donors and chronic lymphocytic leukemia for the expression of CD103, CD39, and CD38 in CD4+FOXP3+CD25− cells.
FOXP3 Expression in CD8+CD25+ T Cells in Chronic Lymphocytic Leukemia Patients
Within the CD8+ T-cell population, a cell population expressing FOXP3 and CD25 (FOXP3+CD25+) was identified. The percentage of these CD8+FOXP3+CD25+ cells was significantly increased in chronic lymphocytic leukemia patients compared with healthy donors (11.2±2.1% vs 0.4±0.08%, respectively, P<0.0001; Figure 5d). The proportion of CD8+FOXP3+CD25+ cells defined as naïve, EC, CM, and EM cells was determined for chronic lymphocytic leukemia, but not for healthy donors, as there were not sufficient numbers of cell with this phenotype in the latter for this task (Figure 5e). The majority of CD8+FOXP3+CD25+cells in chronic lymphocytic leukemia were naïve, showing expression of CD45RA+ (76.4±4.1%). Approximately equal proportions of CM cells (11.3±2.9%) and EM (10.4±2.3%) were observed among CD8+FOXP3+CD25+ cells. Effector cells represented 1.9±0.7% of the CD8+FOXP3+CD25+cells. Determination of naïve and memory sub-populations of CD8+FOXP3+CD25+cells in healthy individuals was not possible due to the extremely low percentage of these cells found in healthy donors.
Correlation of Immunophenotypes with Prognostic Markers
The frequencies of Tregs and of the various Treg subsets were analyzed for their correlation with known prognostic markers. Previous studies have reported that a combination of CD38 and ZAP-70 is the best predictor of disease progression.33, 34, 35 Using the Spearman's correlation, we found that both CD45RA+ Treg and CD8 Treg were significantly inversely correlated with combined CD38 and ZAP-70 expression (Spearman's r=−0.55 (P=0.02) and Spearman's r=−0.58 (P=0.01), respectively). Using the Mann–Whitney test, we compared the mean of these two populations in two groups CD38−/ZAP70− and CD38+/ZAP70+, and it was found that the frequency of CD45RA+ Tregs and CD8+ Tregs was significantly different. CD45RA+ Treg cells were lower in CD38+/ZAP70+ group; 41±6.9% vs 60±5.3% in CD38−/ZAP70− (P=0.02). CD8 Treg cells were also lower in CD38+/ZAP70+ group; 6.7±2.1% vs 17.7±3% in CD38−/ZAP70− (P=0.02). We did not observe any other significant correlation between the various Treg phenotypes and the combination of predictors of disease progression.
Discussion
T-regulatory cells can be identified in a number of different ways. Bright expression of CD25 alone on CD4 T cells or in concert with low CD127 expression or expression of FOXP3 are the most common methods of identification of Tregs. Among the reports of Tregs in chronic lymphocytic leukemia, only Giannopoulos et al10 used FOXP3 as a component of Treg identification, yet all found an increase in the frequency of these cells in chronic lymphocytic leukemia. In concordance with these studies we found an increase in the frequency of Tregs in the peripheral circulation compared with age-matched healthy donors. The literature is divided on whether the frequency of Tregs in chronic lymphocytic leukemia correlates with prognostic markers such as CD38, ZAP-70, or IgVH mutational status, and it remains unclear why these discrepancies occur. Several studies did find a correlation between the frequency of Tregs and clinical stage,6, 10 but we found that the frequency of total CD4+ Tregs did not significantly correlate with prognostic markers. We found instead that specific sub-populations of Tregs, CD4+CD45RA+ Tregs, and CD8+ Tregs did show a correlation. These findings strongly suggest that elucidating the complex immunophenotypes of Tregs found in chronic lymphocytic leukemia is necessary to understand their role in this disease progression.
We observed a significant increase of CD4−CD8− T cells in patients with chronic lymphocytic leukemia, these cells could be immature T cells, and could reflect the change on T-cell function induced by the presence of chronic lymphocytic leukemia cells. In addition to immature T cells, these double-negative T cells could be iNKT cells, or γδ T cells. Further experiments would be needed to determinate further the nature of these cells.
The expression of FOXP3 as a specific marker of Tregs cells is controversial regarding whether it is sufficient for a suppressor phenotype.36 Recent data supports the concept that transient expression of FOXP3 does not confer suppressive activity but permanent expression does.12 The current data demonstrate that CD4+CD25−FOXP3+ and CD8+CD25highFOXP3+ populations were significantly increased in chronic lymphocytic leukemia patients compared with healthy donors. Unfortunately there is no way to know whether this FOXP3 expression is transient or permanent. Furthermore, as these cells could only be identified through the use of intracellular staining for FOXP3, they could not be sorted as viable cells and thus there is no way of definitively establishing their suppressive function. Both CD4+CD25−FOXP3+ as well as CD8+CD25+FOXP3+ Tregs have previously been described37, 38, 39 and it is within reason to think these subsets may have suppressive functions. If these populations are indeed suppressive, this suggests that previous studies have underestimated the frequency of Tregs in chronic lymphocytic leukemia as those studies only identified CD4+CD25+ cells as Tregs.
Within the CD4+CD25highFOXP3+ Tregs there exists a greater complexity of phenotypes than reported to date. Until recently, CD4+CD25+Treg cells have been described using limited markers as belonging to the memory T-cell compartment.13, 14, 15, 16 Valmori et al40 identified a Treg-cell population with naïve phenotype (CCR7+CD45RA+), which they termed natural naïve Treg cells. Several observations have been made by other groups examining the naïve (CD45RA+) vs memory (CD45RO+) phenotype of Tregs population. Among these observations are the findings of: (1) an increase of memory Tregs in older HIV-infected patients,41 (2) an increase of naïve Tregs in younger healthy donors,41 and (3) that the frequency, phenotypic characteristic, and anti-proliferative function were comparable in the young (age<40 years) and the elderly (age>65 years).42, 43 The current data demonstrate that Tregs can readily be classified as naïve, EC, CM, and EM subsets using CD27, CCR7, and CD45RA. The NnTreg population, identified in the current study as viable CD45+CD3+CD8−CD4+CD25+FOXP3highCD45RA+CCR7+CD27+, is increased in the chronic lymphocytic leukemia patients compared with controls. Statistically significant differences between chronic lymphocytic leukemia patients and healthy donors were observed in EM Tregs as well as in effector Tregs using these classifications. The data suggest that simple identification of Tregs as naïve or adaptive may be too superficial to draw meaningful conclusions regarding their function, as these cells lend themselves to further phenotypic compartmentalization as performed for CD4+ T cells as a whole. By using these complex classifications, significant differences are observed in the Treg populations between chronic lymphocytic leukemia patients and healthy donors. The current data show in chronic lymphocytic leukemia patients averaging over 65 years of age, naïve Tregs remain a predominant population, whereas in healthy donors, we showed a paucity of naïve Tregs, consistent with previous reports. Booth et al44 have demonstrated that human Tregs expressing either CD45RA or CD45RO have identical suppressive capacity in healthy individuals, although the former are less proliferative. Interestingly, their data also show that CD45RA Tregs express CXCR4 and preferentially accumulate in the bone marrow.
Within the Treg population, the chronic lymphocytic leukemia patients had patterns of marker expression, other than CD45RA, differing significantly from those in healthy donors, such as increased co-expression of CD39 and CCR7. CD39 has been closely associated with the suppressive activity of Tregs.45 Thus, dual-positive CCR7+CD39+ Tregs were speculated to be a highly suppressive phenotype. In five cases of chronic lymphocytic leukemia, the suppressive capability of the sorted Tregs CD39+CCR7+ was less than the total Tregs from the same donor but this did not reach statistical significance. It was not possible to sort sufficient CD39+CCR7+ Tregs from healthy donors, as virtually none existed. However, compared with total Tregs from healthy individuals, the CD39+CCR7+ Tregs unexpectedly showed a slightly reduced suppressive capability. These CD39+ Tregs might be highly activated but not necessarily highly suppressive. Another observation was an increased expression of CD127 in the Tregs from chronic lymphocytic leukemia. Studies have shown that CD127 has an important role in the proliferation and differentiation of mature T cells, and in vitro experiments show that the expression of CD127 is downregulated following T-cell activation.46, 47 Earlier studies showed that CD127 expression inversely correlates with the suppressive function of Tregs.48 The increase of CD127 could be linked to the naïve phenotype of our chronic lymphocytic leukemia Tregs, as low expression of CD127 is a marker for natural Tregs that have a memory phenotype,7 and the chronic lymphocytic leukemia Tregs have a naïve phenotype. This finding would suggest that care should be taken when using low CD127 expression to define Tregs in these patients, and possibly in patients with other forms of cancer. Taken as a whole, our data indicate that it is possible to delineate many putative subtypes of Tregs cells using widely studied markers.49
In the context of chronic lymphocytic leukemia, as well as other neoplastic diseases, ascribing the regulation of immune responses by Tregs might be a far more complex process than simply measuring CD4+CD25+FOXP3+ cells. Much work remains to validate such speculation by sorting the populations of Tregs identified by the 15-color immunophenotyping and elucidating the function of each. It is hoped that the high-dimensional immunophenotyping of Tregs demonstrating numerous distinct sub-populations presented here will serve as an impetus for such studies.
References
Scrivener S, Goddard RV, Kaminski ER, Prentice AG . Abnormal T-cell function in B-cell chronic lymphocytic leukaemia. Leuk Lymphoma 2003;44:383–389.
Reyes E, Prieto A, Carrion F, et al. Altered pattern of cytokine production by peripheral blood CD2+ cells from B chronic lymphocytic leukemia patients. Am J Hematol 1998;57:93–100.
Dianzani U, Omede P, Marmont F, et al. Expansion of T cells expressing low CD4 or CD8 levels in B-cell chronic lymphocytic leukemia: correlation with disease status and neoplastic phenotype. Blood 1994;83:2198–2205.
Mackus WJ, Frakking FN, Grummels A, et al. Expansion of CMV-specific CD8+CD45RA+CD27− T cells in B-cell chronic lymphocytic leukemia. Blood 2003;102:1057–1063.
Beyer M, Kochanek M, Darabi K, et al. Reduced frequencies and suppressive function of CD4+CD25hi regulatory T cells in patients with chronic lymphocytic leukemia after therapy with fludarabine. Blood 2005;106:2018–2025.
Giannopoulos K, Schmitt M, Wlasiuk P, et al. The high frequency of T regulatory cells in patients with B-cell chronic lymphocytic leukemia is diminished through treatment with thalidomide. Leukemia 2008;22:222–224.
Jak M, Mous R, Remmerswaal EB, et al. Enhanced formation and survival of CD4+ CD25hi Foxp3+ T-cells in chronic lymphocytic leukemia. Leuk Lymphoma 2009;50:788–801.
D'Arena G, Laurenti L, Minervini MM, et al. Regulatory T-cell number is increased in chronic lymphocytic leukemia patients and correlates with progressive disease. Leuk Res 2011;35:363–368.
Deutsch V, Perry C, Polliack A . Expansion of regulatory T cells in B chronic lymphocytic leukemia: enhanced ‘brakes’ on host immunity. Leuk Lymphoma 2009;50:687–688.
Giannopoulos K, Schmitt M, Kowal M, et al. Characterization of regulatory T cells in patients with B-cell chronic lymphocytic leukemia. Oncol Rep 2008;20:677–682.
Banham AH . Cell-surface IL-7 receptor expression facilitates the purification of FOXP3(+) regulatory T cells. Trends Immunol 2006;27:541–544.
Buckner JH, Ziegler SF . Functional analysis of FOXP3. Ann N Y Acad Sci 2008;1143:151–169.
Taams LS, Smith J, Rustin MH, et al. Human anergic/suppressive CD4(+)CD25(+) T cells: a highly differentiated and apoptosis-prone population. Eur J Immunol 2001;31:1122–1131.
Annacker O, Pimenta-Araujo R, Burlen-Defranoux O, et al. CD25+ CD4+ T cells regulate the expansion of peripheral CD4 T cells through the production of IL-10. J Immunol 2001;166:3008–3018.
Thornton AM, Shevach EM . Suppressor effector function of CD4+CD25+ immunoregulatory T cells is antigen nonspecific. J Immunol 2000;164:183–190.
Thornton AM, Shevach EM . CD4+CD25+ immunoregulatory T cells suppress polyclonal T cell activation in vitro by inhibiting interleukin 2 production. J Exp Med 1998;188:287–296.
Wing K, Larsson P, Sandstrom K, et al. CD4+ CD25+ FOXP3+ regulatory T cells from human thymus and cord blood suppress antigen-specific T cell responses. Immunology 2005;115:516–525.
Seddiki N, Santner-Nanan B, Tangye SG, et al. Persistence of naive CD45RA+ regulatory T cells in adult life. Blood 2006;107:2830–2838.
Weiss EM, Schmidt A, Vobis D, et al. Foxp3-mediated suppression of CD95L expression confers resistance to activation-induced cell death in regulatory T cells. J Immunol 2011;187:1684–1691.
Curiel TJ, Coukos G, Zou L, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med 2004;10:942–949.
Ding W, Zent CS . Diagnosis and management of autoimmune complications of chronic lymphocytic leukemia/small lymphocytic lymphoma. Clin Adv Hematol Oncol 2007;5:257–261.
Bagwell B . Probability State Modeling—a new paradigm for cytometric analysis. In: Litwin V and Marder P, (eds). Flow Cytometry in Drug Discovery and Development. John Wiley & Sons: Hoboken, 2009, pp 281–302.
Bagwell CB . Data analysis through modeling. In: Dean PN (ed). Current Protocol in Cytometry. John Wiley & Sons: Hoboken, 2001; Unit 10.7.1–10.7.20.
Bagwell CB . Breaking the dimensionality barrier. Methods Mol Biol 2011;699:31–51.
Damle RN, Wasil T, Fais F, et al. Ig V gene mutation status and CD38 expression as novel prognostic indicators in chronic lymphocytic leukemia. Blood 1999;94:1840–1847.
Hamblin TJ, Davis Z, Gardiner A, Oscier DG, Stevenson FK . Unmutated Ig V(H) genes are associated with a more aggressive form of chronic lymphocytic leukemia. Blood 1999;94:1848–1854.
Ahmed R, Bevan MJ, Reiner SL, Fearon DT . The precursors of memory: models and controversies. Nat Rev Immunol 2009;9:662–668.
Appay V, van Lier RA, Sallusto F, Roederer M . Phenotype and function of human T lymphocyte subsets: consensus and issues. Cytometry A 2008;73:975–983.
Song K, Rabin RL, Hill BJ, et al. Characterization of subsets of CD4+ memory T cells reveals early branched pathways of T cell differentiation in humans. Proc Natl Acad Sci USA 2005;102:7916–7921.
Baecher-Allan C, Brown JA, Freeman GJ, Hafler DA . CD4+CD25+ regulatory cells from human peripheral blood express very high levels of CD25 ex vivo. Novartis Found Symp 2003;252:67–88.
Baecher-Allan C, Viglietta V, Hafler DA . Inhibition of human CD4(+)CD25(+high) regulatory T cell function. J Immunol 2002;169:6210–6217.
Venken K, Thewissen M, Hellings N, et al. A CFSE based assay for measuring CD4+CD25+ regulatory T cell mediated suppression of auto-antigen specific and polyclonal T cell responses. J Immunol Methods 2007;322:1–11.
Hus I, Bojarska-Junak A, Dmoszynska A, et al. ZAP-70 and CD38 expression are independent prognostic factors in patients with B-cell chronic lymphocytic leukaemia and combined analysis improves their predictive value. Folia Histochem Cytobiol 2008;46:147–152.
Hus I, Podhorecka M, Bojarska-Junak A, et al. The clinical significance of ZAP-70 and CD38 expression in B-cell chronic lymphocytic leukaemia. Ann Oncol 2006;17:683–690.
Schroers R, Griesinger F, Trumper L, et al. Combined analysis of ZAP-70 and CD38 expression as a predictor of disease progression in B-cell chronic lymphocytic leukemia. Leukemia 2005;19:750–758.
Feuerer M, Hill JA, Mathis D, Benoist C . Foxp3+ regulatory T cells: differentiation, specification, subphenotypes. Nat Immunol 2009;10:689–695.
Siegmund K, Ruckert B, Ouaked N, et al. Unique phenotype of human tonsillar and in vitro-induced FOXP3+CD8+ T cells. J Immunol 2009;182:2124–2130.
Chaput N, Louafi S, Bardier A, et al. Identification of CD8+CD25+Foxp3+ suppressive T cells in colorectal cancer tissue. Gut 2009;58:520–529.
Zelenay S, Lopes-Carvalho T, Caramalho I, et al. Foxp3+ CD25- CD4 T cells constitute a reservoir of committed regulatory cells that regain CD25 expression upon homeostatic expansion. Proc Natl Acad Sci USA 2005;102:4091–4096.
Valmori D, Merlo A, Souleimanian NE, Hesdorffer CS, Ayyoub M . A peripheral circulating compartment of natural naive CD4 Tregs. J Clin Invest 2005;115:1953–1962.
Tenorio AR, Spritzler J, Martinson J, et al. The effect of aging on T-regulatory cell frequency in HIV infection. Clin Immunol 2009;130:298–303.
Hwang KA, Kim HR, Kang I . Aging and human CD4(+) regulatory T cells. Mech Ageing Dev 2009;130:509–517.
Simone R, Zicca A, Saverino D . The frequency of regulatory CD3+CD8+CD28− CD25+ T lymphocytes in human peripheral blood increases with age. J Leukoc Biol 2008;84:1454–1461.
Booth NJ, McQuaid AJ, Sobande T, et al. Different proliferative potential and migratory characteristics of human CD4+ regulatory T cells that express either CD45RA or CD45RO. J Immunol 2010;184:4317–4326.
Mandapathil M, Lang S, Gorelik E, Whiteside TL . Isolation of functional human regulatory T cells (Treg) from the peripheral blood based on the CD39 expression. J Immunol Methods 2009;346:55–63.
Appasamy PM . Biological and clinical implications of interleukin-7 and lymphopoiesis. Cytokines Cell Mol Ther 1999;5:25–39.
Hofmeister R, Khaled AR, Benbernou N, et al. Interleukin-7: physiological roles and mechanisms of action. Cytokine Growth Factor Rev 1999;10:41–60.
Liu W, Putnam AL, Xu-Yu Z, et al. CD127 expression inversely correlates with FoxP3 and suppressive function of human CD4+ T reg cells. J Exp Med 2006;203:1701–1711.
Shevach EM . From vanilla to 28 flavors: multiple varieties of T regulatory cells. Immunity 2006;25:195–201.
Acknowledgements
We are grateful to Dr. M. Roederer and Dr. P. Chattopadhyay for their generous assistance. This research was supported by the Intramural Research Program of the NHLBI and by the CHI, NIH, Bethesda, MD, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Biancotto, A., Dagur, P., Fuchs, J. et al. Phenotypic complexity of T regulatory subsets in patients with B-chronic lymphocytic leukemia. Mod Pathol 25, 246–259 (2012). https://doi.org/10.1038/modpathol.2011.164
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2011.164
Keywords
This article is cited by
-
BCL-2 expression promotes immunosuppression in chronic lymphocytic leukemia by enhancing regulatory T cell differentiation and cytotoxic T cell exhaustion
Molecular Cancer (2022)
-
T-cells in chronic lymphocytic leukemia: Guardians or drivers of disease?
Leukemia (2020)
-
Immunosuppressive Treg cells acquire the phenotype of effector-T cells in chronic lymphocytic leukemia patients
Journal of Translational Medicine (2018)
-
Impaired B cell immunity in acute myeloid leukemia patients after chemotherapy
Journal of Translational Medicine (2017)
-
Regulatory T cells in chronic lymphocytic leukemia: implication for immunotherapeutic interventions
Tumor Biology (2013)