Abstract
The objective of our study was to study which is the most accurate specimen for histological diagnosis of prosthetic joint infections (pseudocapsule or interface membrane). This is a prospective study including hip revision arthroplasties performed from January 2007 to June 2009. Specimens from pseudocapsule and from interface membrane were obtained from each patient. The histology was considered positive for infection when ≥5 neutrophils per high-power field ( × 40) were found. Definitive diagnosis of infection was considered when ≥2 cultures were positive for the same microorganism. According to the definition of infection, patients were classified in two groups: (A) patients with aseptic loosening in whom cultures obtained during surgery were negative and (B) patients with prosthetic joint infection. A total of 69 revisions were included in the study; 57 were classified in group A and 12 in group B. In group B, the percentage of positive interface membrane histology was significantly higher than the percentage of positive pseudocapsule histology (83 vs 42%, P=0.04, Fisher's exact test). The results suggest that periprosthetic interface membrane is the best specimen for the histological diagnosis of prosthetic joint infection.
Similar content being viewed by others
Main
Infection after total joint arthroplasty is a challenging problem.1 Microorganisms colonizing the implant surface are associated with prosthesis loosening. Cultures and polymorphonuclear leukocytes count from periprosthetic tissue are the gold standard for the diagnosis of prosthetic joint infections.2 The specificity and sensitivity of histology has never been 100%3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21 and this may be for different reasons.5, 12, 22, 23 False-positive results of histology could be because culture and histological specimens are taken from different areas.5, 12, 22 False-negative results could be attributed to: (1) low virulent microorganisms like Staphylococcus epidermidis6, 7, 22, 24, 25 or Propionibacterium spp26, 27 that do not stimulate neutrophile infiltration, (2) bacteriological contamination of the specimen obtained for culture12 or (3) the cut-off point (number of neutrophils per field) to establish the diagnosis of infection.2, 4, 5, 10, 13, 28, 29, 30 Another possibility for inconsistencies in the histological results could be the type of specimen submitted to the laboratory. The majority of investigators obtain specimens from pseudocapsule, synovial surface, interface membrane and any tissue area suspected of infection.6, 7, 8, 12, 15, 16, 22 The objective of our study was to study which is the most accurate specimen for histological diagnosis of prosthetic joint infection.
Materials and methods
Prospective study including hip revision arthroplasties performed in our hospital from January 2007 to June 2009.
Histological Protocol
Specimens from pseudocapsule and interface membrane were obtained for each patient. The pseudocapsule specimens studied were obtained from the part in contact with the neck of the prosthesis. The surface of the pseudocapsule that faces the joint cavity was identified and the sections were taken perpendicular to it. These surfaces were histologically identified in each specimen examined. Interface membranes from the femoral stem and from the acetabular cup were taken. The specimens for paraffin histology sections were formalin-fixed and paraffin-embedded before hematoxylin-eosin staining. The pathologists of our hospital used the Mirras' criteria (adapted by Feldman).2, 13 The histology was considered positive for infection when ≥5 neutrophils per high-power field ( × 40) in at least five separate microscopic fields were found. The study was performed in paraffin sections and not in frozen sections avoiding histological technical bias.
Microbiology
The specimens for the microbiological study were always taken before the administration of antibiotic prophylaxis. At the time of implant removal, at least five periprosthetic specimens from different sites were submitted to the laboratory for culture. Liquid samples were aspirated from the operative site using a sterile syringe and immediately inoculated into blood culture flasks (Bactec 9400, Becton Dickinson Diagnostic Instruments, Sparks, MD, USA) and incubated for 5 days. Positive flasks were sub-cultured in aerobic and anaerobic agar media. Swab cultures were obtained by rubbing a sterile swab (Deltalab, invasive sterile eurotube collection swab with Stuart transport medium, Rubí, Catalonia, Spain) over the tissue area, bone or fluid suspected of infection. Solid tissue samples from pseudocapsule, periprosthetic membranes or tissue suspected to be infected were immediately placed into a separate sterile universal bottle. Solid tissue and swabs were cultured in aerobic and anaerobic agar media and in thioglicolate broth enriched with vitamin K and hemin and incubated for 10 days. Positive cultures were sent for identification and sensitivity testing.
Patient Classification
Preoperative diagnosis of aseptic loosening was made when the patient had pain, erythrocyte sedimentation rate <30 mm/h and a serum concentration of C-reactive protein <1.3 mg per 100 ml, radiological signs of loosening, Technetium99m methylene diphosphonate scintigraphy and the Tecnetium99m hexamethylpropylene-amineoxine-labelled leukocytes scintigraphy were negative for infection. In these patients revision was performed using one stage exchange.
Preoperative diagnosis of septic loosening was made when the patient had pain in the hip and/or fistula, erythrocyte sedimentation rate >30 mm/h and serum concentration of C-reactive protein >1.3 mg per 100 ml, radiological signs of loosening, Technetium99m methylene diphosphonate scintigraphy and the Tecnetium99m hexamethylpropylene-amineoxine-labelled leukocytes scintigraphy were positive for infection and when a culture of synovial fluid obtained by joint aspiration was positive. In these patients, revision was performed using a two stage exchange.
Definitive diagnosis of infection was considered when ≥2 intraoperative cultures were positive for the same microorganism or when there was pus surrounding the prosthesis.31 Patients with ≤1 intraoperative positive culture were classified as non-infected.
Patients included in the study were classified in two groups:
Group A: patients submitted to hip revision arthroplasty because of a preoperative diagnosis of an aseptic loosening in whom the definitive diagnosis was as non-infected.
Group B: patients submitted to hip revision arthroplasty because of a preoperative diagnosis of a septic loosening in whom the definitive diagnosis was confirmed as infection.
Patients who underwent hip revision arthroplasty because of periprosthetic fracture4, 12, 15 and patients with a preoperative diagnosis of aseptic loosening and a definitive diagnosis of infection were excluded for the study.6
Statistical Analysis
The specificity (true negatives/false positives + true negatives), sensitivity (true positives/false negatives + true positives), positive predictive value (true positives/true positives + false positives) and negative predictive value (true negatives/true negatives + false negatives) of Mirras' criteria were evaluated. For comparison of proportions, a Fisher's exact test was applied and the differences were considered significant when P<0.05.
Results
During the study period, a total of 69 revisions hip arthroplasties were included; 57 were classified in group A and 12 in group B. The mean age was 65 years (range 45–85 years), 34 were women and 35 were men. The results of interface membrane, pseudocapsule histology and microbiology from group A and B are shown in Table 1.
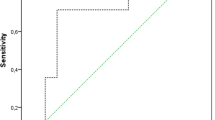
The sensitivity, specificity, positive and negative predictive value of interface membrane histology were 83, 98, 91 and 96%, respectively (Table 2) and of pseudocapsule histology were 42, 98, 83 and 83%, respectively (Table 3). In group B, the percentage of positive interface membrane histology (Figure 1) was significantly higher than the percentage of positive pseudocapsule histology (83 vs 42%, P=0.04, Fisher's exact test).
The types of specimens used for the histological study in previous articles that evaluate the usefulness of histology in prosthetic loosening are summarized in Table 4.
Discussion
Histology has been considered one of the gold standards for the diagnosis of prosthetic joint infection,2, 4, 18, 29 however, a low sensitivity has been observed by several authors.3, 6, 7, 8, 9, 11, 15, 21 These inconsistencies could be attributed to the type of patients included in each study,6, 7, 8 the microbiological19, 29, 32 or histological criteria applied for the diagnosis of infection2, 4, 5, 28, 29, 30 or the different specimens (interface membrane or pseudocapsule) submitted for the analysis.4 Reviewing the literature (Table 4), there is a lot of variability in the specimen submitted for histological evaluation. Some investigators did not obtain interface membrane5, 18, 33, 34 and others did not define the type of specimen analyzed.10, 13, 21 It is generally accepted that there is no important differences between tissue specimens.28, 29, 35 To our knowledge, this is the first study comparing the results of the histology in two different specimens (interface membrane and pseudocapsule). The interface membrane had a higher sensitivity and predictive values than pseudocapsule. In fact, the proportion of infected patients with positive interface membrane was significantly higher than those with positive pseudocapsule (83 vs 42%, P=0.04). Using only pseudocapsule, 7 out of 12 infected patients would not have been correctly diagnosed. Previously, Athanasou et al4 suggested that more florid inflammation was generally found in femoral interface membrane than in joint pseudocapsule, however, this information was not quantified. A possible reasons for our results could be the presence of fibrosis (Figure 2) in pseudocapsule that makes difficult the neutrophil infiltration7 and the fact that the major bacterial biofilm is found between implant and bone.
This photomicrograph is a paraffin section from pseudocapsule without neutrophil infiltration from the same patient showed in Figure 1. Below the synovial surface (head of black arrow), a dense fibrous tissue with mature collagen fibers and ordered fibroblasts is shown.
Recently, there are a group of investigators29, 30, 32, 37, 38 that have used only membranes (not pseudocapsule) and have proposed a histopathological consensus classification for a standardized evaluation of the periprosthetic tissues. Our results support the selection of the interface membrane as a reference tissue for histological classification.
Although frozen section gives surgeons intraoperative information about the diagnosis, our study was performed on paraffin sections to avoid histological technical bias. It has been described that frozen sections have inferior quality than paraffin ones.10, 19, 32 For instance, Tohtz et al32 described a 19% of discrepancies (in 14 out of 64 cases) between frozen section and paraffin sections.32
The main drawback of our study was the low number of infected patients included. However, this study had enough statistical power to reveal differences between interface membrane and pseudocapsule specimens. Patients who underwent hip revision arthroplasty because of periprosthetic fracture were not included since it is a cause of false-positive histology results.4, 12, 15 Patients with a preoperative diagnosis of aseptic loosening and a definitive diagnosis of infection were also not included since in our experience,6 the sensitivity of the histology (using Mirras' criteria) in this group of patients is low.
In conclusion, our results suggest that the best specimen of periprosthetic soft tissue for histological diagnosis of the infection in a total hip revision arthroplasty is the periprosthetic interface membrane.
References
Bauer TW, Parvizi J, Kobayashi N, et al. Diagnosis of periprosthetic infection. J Bone Joint Surg Am 2006;88:869–882.
Feldman DS, Lonner JH, Desai P, et al. The role of intraoperative frozen sections in revision total joint arthroplasty. J Bone Joint Surg Am 1995;77:1807–1813.
Abdul-Karim FW, McGinnis MG, Kraay M, et al. Frozen section biopsy assessment for the presence of polymorphonuclear leukocytes in patients undergoing revision of arthroplasties. Mod Pathol 1998;11:427–431.
Athanasou NA, Pandey R, de SR, et al. Diagnosis of infection by frozen section during revision arthroplasty. J Bone Joint Surg Br 1995;77:28–33.
Banit DM, Kaufer H, Hartford JM . Intraoperative frozen section analysis in revision total joint arthroplasty. Clin Orthop Relat Res 2002;401:230–238.
Bori G, Soriano A, Garcia S, et al. Low sensitivity of histology to predict the presence of microorganisms in suspected aseptic loosening of a joint prosthesis. Mod Pathol 2006;19:874–877.
Bori G, Soriano A, Garcia S, et al. Usefulness of histological analysis for predicting the presence of microorganisms at the time of reimplantation after hip resection arthroplasty for the treatment of infection. J Bone Joint Surg Am 2007;89:1232–1237.
la Valle CJ, Bogner E, Desai P, et al. Analysis of frozen sections of intraoperative specimens obtained at the time of reoperation after hip or knee resection arthroplasty for the treatment of infection. J Bone Joint Surg Am 1999;81:684–689.
Fehring TK, McAlister Jr JA . Frozen histologic section as a guide to sepsis in revision joint arthroplasty. Clin Orthop Relat Res 1994;304:229–237.
Frances BA, Martinez FM, Cebrian Parra JL, et al. Diagnosis of infection in hip and knee revision surgery: intraoperative frozen section analysis. Int Orthop 2007;31:33–37.
Ko PS, Ip D, Chow KP, et al. The role of intraoperative frozen section in decision making in revision hip and knee arthroplasties in a local community hospital. J Arthroplasty 2005;20:189–195.
Lonner JH, Desai P, Dicesare PE, et al. The reliability of analysis of intraoperative frozen sections for identifying active infection during revision hip or knee arthroplasty. J Bone Joint Surg Am 1996;78:1553–1558.
Mirra JM, Amstutz HC, Matos M, et al. The pathology of the joint tissues and its clinical relevance in prosthesis failure. Clin Orthop Relat Res 1976;117:221–240.
Mirra JM, Marder RA, Amstutz HC . The pathology of failed total joint arthroplasty. Clin Orthop Relat Res 1982;170:175–183.
Musso AD, Mohanty K, Spencer-Jones R . Role of frozen section histology in diagnosis of infection during revision arthroplasty. Postgrad Med J 2003;79:590–593.
Nuñez LV, Buttaro MA, Morandi A, et al. Frozen sections of samples taken intraoperatively for diagnosis of infection in revision hip surgery. Acta Orthop 2007;78:226–230.
Pace TB, Jeray KJ, Latham Jr JT . Synovial tissue examination by frozen section as an indicator of infection in hip and knee arthroplasty in community hospitals. J Arthroplasty 1997;12:64–69.
Pons M, Angles F, Sanchez C, et al. Infected total hip arthroplasty--the value of intraoperative histology. Int Orthop 1999;23:34–36.
Spangehl MJ, Masri BA, O'Connell JX, et al. Prospective analysis of preoperative and intraoperative investigations for the diagnosis of infection at the sites of two hundred and two revision total hip arthroplasties. J Bone Joint Surg Am 1999;81:672–683.
Wong YC, Lee QJ, Wai YL, et al. Intraoperative frozen section for detecting active infection in failed hip and knee arthroplasties. J Arthroplasty 2005;20:1015–1020.
Kanner WA, Saleh KJ, Frierson Jr HF . Reassessment of the usefulness of frozen section analysis for hip and knee joint revisions. Am J Clin Pathol 2008;130:363–368.
Bori G, Soriano A, Garcia S, et al. Neutrophils in frozen section and type of microorganism isolated at the time of resection arthroplasty for the treatment of infection. Arch Orthop Trauma Surg 2009;129:591–595.
Athanasou NA, Pandey R, de SR, et al. The role of intraoperative frozen sections in revision total joint arthroplasty. J Bone Joint Surg Am 1997;79:1433–1434.
Tunney MM, Patrick S, Curran MD, et al. Detection of prosthetic hip infection at revision arthroplasty by immunofluorescence microscopy and PCR amplification of the bacterial 16S rRNA gene. J Clin Microbiol 1999;37:3281–3290.
Savarino L, Baldini N, Tarabusi C, et al. Diagnosis of infection after total hip replacement. J Biomed Mater Res B Appl Biomater 2004;70:139–145.
Zeller V, Ghorbani A, Strady C, et al. Propionibacterium acnes: an agent of prosthetic joint infection and colonization. J Infect 2007;55:119–124.
Zappe B, Graf S, Ochsner PE, et al. Propionibacterium spp. in prosthetic joint infections: a diagnostic challenge. Arch Orthop Trauma Surg 2008;128:1039–1046.
Pandey R, Drakoulakis E, Athanasou NA . An assessment of the histological criteria used to diagnose infection in hip revision arthroplasty tissues. J Clin Pathol 1999;52:118–123.
Morawietz L, Classen RA, Schroder JH, et al. Proposal for a histopathological consensus classification of the periprosthetic interface membrane. J Clin Pathol 2006;59:591–597.
Morawietz L, Tiddens O, Mueller M, et al. Twenty-three neutrophil granulocytes in 10 high-power fields is the best histopathological threshold to differentiate between aseptic and septic endoprosthesis loosening. Histopathology 2009;54:847–853.
Leone JM, Hanssen AD . Management of infection at the site of a total knee arthroplasty. J Bone Joint Surg Am 2005;87:2335–2348.
Tohtz SW, Muller M, Morawietz L, et al. Validity of frozen sections for analysis of periprosthetic loosening membranes. Clin Orthop Relat Res 2009;468:762–768.
Schinsky MF, la Valle CJ, Sporer SM, et al. Perioperative testing for joint infection in patients undergoing revision total hip arthroplasty. J Bone Joint Surg Am 2008;90:1869–1875.
la Valle CJ, Sporer SM, Jacobs JJ, et al. Preoperative testing for sepsis before revision total knee arthroplasty. J Arthroplasty 2007;22:90–93.
Pandey R, Berendt AR, Athanasou NA . Histological and microbiological findings in non-infected and infected revision arthroplasty tissues. The OSIRIS Collaborative Study Group. Oxford Skeletal Infection Research and Intervention Service. Arch Orthop Trauma Surg 2000;120:570–574.
Nilsdotter-Augustinsson A, Briheim G, Herder A, et al. Inflammatory response in 85 patients with loosened hip prostheses: a prospective study comparing inflammatory markers in patients with aseptic and septic prosthetic loosening. Acta Orthop 2007;78:629–639.
Muller M, Morawietz L, Hasart O, et al. Diagnosis of periprosthetic infection following total hip arthroplasty—evaluation of the diagnostic values of pre- and intraoperative parameters and the associated strategy to preoperatively select patients with a high probability of joint infection. J Orthop Surg 2008;3:31.
Muller M, Morawietz L, Hasart O, et al. Histopathological diagnosis of periprosthetic joint infection following total hip arthroplasty: use of a standardized classification system of the periprosthetic interface membrane. Orthopade 2009;38:1087–1096.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bori, G., Muñoz-Mahamud, E., Garcia, S. et al. Interface membrane is the best sample for histological study to diagnose prosthetic joint infection. Mod Pathol 24, 579–584 (2011). https://doi.org/10.1038/modpathol.2010.219
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2010.219
Keywords
This article is cited by
-
Usefulness of histology for predicting infection at the time of hip and knee revision in patients with rheumatoid arthritis
Archives of Orthopaedic and Trauma Surgery (2021)
-
Alteration of the RANKL/RANK/OPG System in Periprosthetic Osteolysis with Septic Loosening
Inflammation (2016)
-
Investigation of neutrophilic peptides in periprosthetic tissue by matrix-assisted laser desorption ionisation time-of-flight imaging mass spectrometry
International Orthopaedics (2015)
-
Comparison of bacterial results from conventional cultures of the periprosthetic membrane and the synovial or pseudocapsule during hip revision arthroplasty
Archives of Orthopaedic and Trauma Surgery (2014)